Abstract
Introduction and hyposthesis
Obstetric anal sphincter injuries (OASIs) that are missed at delivery can have long-term consequences. OASIs that are under-classified at delivery are likely to be inadequately repaired, resulting in a persistent anal sphincter defect.
We aimed to identify women who have persistent defects on endoanal ultrasound, inconsistent with the original diagnosis, and compare the effect on St Mark’s incontinence scores (SMIS). We also aimed to look for changes in numbers of under-classification over time.
Methods
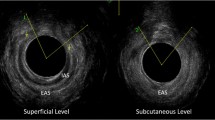
Records of women attending a perineal clinic who had endoanal ultrasound from 2012 to 2020 were reviewed. Women who had a modified Starck score implying a defect greater than the classification [indicated by the depth of external anal sphincter or internal anal sphincter (IAS) defect] at delivery were identified.
Results
A total of 1056 women with a diagnosis of 3a or 3b tears were included. Of these, 120 (11.36%) were found to have a defect greater than the original diagnosis and therefore were incorrectly classified at delivery.
Women who had a 3b tear diagnosed at delivery, but had an IAS defect, had a significantly higher SMIS (p < 0.01). When comparing two 4-year periods, there was a significant improvement in the diagnosis of IAS tears.
Conclusion
Some women with OASIs that have under-classified OASIs are associated with worse anorectal symptoms. This is likely because of an incomplete repair. Some improvement in diagnosis of IAS tears has been noted. We propose improved training in OASIs can help reduce the number of incorrectly classified tears and improve repair.



Similar content being viewed by others
References
Royal College of Obstetrics and Gynaecology. Management of third and fourth degree perineal tears. Greentop guideline number 29 2015.
Sultan AH. Editorial: obstetrical perineal injury and anal incontinence. AVMA Medical & Legal Journal. 1999;5:193–6. https://doi.org/10.1177/135626229900500601.
Roper JC, Sultan AH, Thakar R. Diagnosis of perineal trauma: getting it right first time. Br J Midwifery. 2020;28:710–7. https://doi.org/10.12968/bjom.2020.28.10.710.
Andrews V, Sultan AH, Thakar R, Jones PW. Occult anal sphincter injuries—myth or reality? BJOG. 2006;113:195–200. https://doi.org/10.1111/j.1471-0528.2006.00799.x.
Sioutis D, Thakar R, Sultan AH. Overdiagnosis and rising rate of obstetric anal sphincter injuries (OASIS): time for reappraisal. Ultrasound Obstet Gynecol. 2017;50:642–7. https://doi.org/10.1002/uog.17306.
Sultan AH, Monga A, Lee J, Emmanuel A, Norton C, Santoro G, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female anorectal dysfunction. Int Urogynecol J. 2017;28:5–31. https://doi.org/10.1007/s00192-016-3140-3.
Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI. Anal-sphincter disruption during vaginal delivery. N Engl J Med. 1993;329:1905–11. https://doi.org/10.1056/NEJM199312233292601.
Taithongchai A, Veiga SI, Sultan AH, Thakar R. The consequences of undiagnosed obstetric anal sphincter injuries (OASIS) following vaginal delivery. Int Urogynecol J. 2019. https://doi.org/10.1007/s00192-019-04033-5.
Andrews V, Shelmeridine S, Sultan AH, Thakar R. Anal and urinary incontinence 4 years after a vaginal delivery. Int Urogynecol J. 2013;24:55–60. https://doi.org/10.1007/s00192-012-1835-7.
Ramage L, Yen C, Qiu S, Simillis C, Kontovounisios C, Tan E, et al. Does a missed obstetric anal sphincter injury at time of delivery affect short-term functional outcome? The Annals of The Royal College of Surgeons of England. 2018;100:26–32. https://doi.org/10.1308/rcsann.2017.0140.
Starck M, Bohe M, Valentin L. Results of endosonographic imaging of the anal sphincter 2–7 days after primary repair of third- or fourth-degree obstetric sphincter tears: Endosonographic imaging after anal sphincter tear repair. Ultrasound Obstet Gynecol. 2003;22:609–15. https://doi.org/10.1002/uog.920.
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA. Prospective comparison of faecal incontinence grading systems. Gut. 1999;44:77–80. https://doi.org/10.1136/gut.44.1.77.
Norderval S, Markskog A, Røssaak K, Vonen B. Correlation between anal sphincter defects and anal incontinence following obstetric sphincter tears: assessment using scoring systems for sonographic classification of defects. Ultrasound Obstet Gynecol. 2008;31:78–84. https://doi.org/10.1002/uog.5155.
Andrews V, Thakar R, Sultan AH. Structured hands-on training in repair of obstetric anal sphincter injuries (OASIS): an audit of clinical practice. Int Urogynecol J. 2009;20:193–9. https://doi.org/10.1007/s00192-008-0756-y.
Andrews V, Thankar R, Sultan AH, Kettle C. Can hands-on perineal repair courses affect clinical practice? Br J Midwifery. 2005;13:562–6. https://doi.org/10.12968/bjom.2005.13.9.19625.
Okeahialam NA, Thakar R, Sultan AH. Effect of a subsequent pregnancy on anal sphincter integrity and function after obstetric anal sphincter injury (OASI). Int Urogynecol J. 2021;32:1719–26. https://doi.org/10.1007/s00192-020-04607-8.
Ali-Masri H, Hassan S, Ismail K, Zimmo K, Zimmo M, Fosse E, et al. Enhancing recognition of obstetric anal sphincter injuries in six maternity units in Palestine: an interventional quality improvement study. BMJ Open. 2018;8:e020983. https://doi.org/10.1136/bmjopen-2017-020983.
Roper JC, Amber N, Wan OYK, Sultan AH, Thakar R. Review of available national guidelines for obstetric anal sphincter injury. Int Urogynecol J. 2020;31:2247–59. https://doi.org/10.1007/s00192-020-04464-5.
Sultan AH, Kettle C. Diagnosis of perineal trauma. Perineal and Anal Sphincter Trauma, Springer; 2007, p. 13–20.
Keighley MRB, Perston Y, Bradshaw E, Hayes J, Keighley DM, Webb S. The social, psychological, emotional morbidity and adjustment techniques for women with anal incontinence following obstetric anal sphincter injury: use of a word picture to identify a hidden syndrome. BMC Pregnancy Childbirth. 2016;16:275. https://doi.org/10.1186/s12884-016-1065-y.
Rao SSC. Pathophysiology of adult fecal incontinence. Gastroenterology. 2004;126:S14–22. https://doi.org/10.1053/j.gastro.2003.10.013.
Daly JO, Thakar R, Sultan AH, Van-Delft K. Diagnosis of obstetric anal sphincter injuries: time for re-appraisal of training. International Urogycology Journal and Pelvic Floor Dysfunction Conference: 37th Annual Meeting of the International Urogynecological Association, IUGA 2012., Brisbane, Australia: 2012, p. pp S63-s64.
Capanna F, Haslinger C, Wisser J. Accuracy of clinical diagnosis of anal sphincter defect: clinical evaluation vs 3D-transperineal ultrasound (3D-TPUS). Minerva Ginecol. 2020. https://doi.org/10.23736/S0026-4784.20.04562-1.
Cafaro D, Sturiale A, Donati E, Bordonaro M, Fabiani B, Naldini G. Underdiagnosis and the rising rate of obstetric anal sphincter injuries. The role of three-dimensional ultrasound evaluation. Techniques in Coloproctology. Conference: 8th National Congress of the Italian Society of Colorectal Surgery., vol. 24, Italy: Springer; 2020, p. 363–4.
Berg MR, Sahlin Y. Anal incontinence and unrecognized anal sphincter injuries after vaginal delivery– a cross-sectional study in Norway. BMC Womens Health. 2020;20:131. https://doi.org/10.1186/s12905-020-00989-5.
Keighley M, Webb S, Hayes J. Too many cases of anal incontinence (AI) from obstetric anal sphincter injuries (OASIS) are due to missed third and fourth degree tears. Association of Coloproctology of Great Britain and Ireland Annual Meeting, ACPGBI 2017, UK: Blackwell Publishing Ltd; 2017, p. 12.
Walsh KA, Grivell RM. Use of endoanal ultrasound for reducing the risk of complications related to anal sphincter injury after vaginal birth. Cochrane Database Syst Rev 2015:CD010826. https://doi.org/10.1002/14651858.CD010826.pub2.
Faltin DL, Boulvain M, Floris LA, Irion O. Diagnosis of anal sphincter tears to prevent fecal incontinence: a randomized controlled trial. Obstet Gynecol. 2005;106:6–13. https://doi.org/10.1097/01.AOG.0000165273.68486.95.
Wong KW, Thakar R, Sultan AH, Andrews V. Can transperineal ultrasound improve the diagnosis of obstetric anal sphincter injuries? 2019 world congress of the Royal College of Obstretriscians and Gynaecologists, RCOG 2019., UK: Blackwell Publishing Ltd; 2019, p. 229.
Starck M, Bohe M, Fortling B, Valentin L. Endosonography of the anal sphincter in women of different ages and parity. Ultrasound Obstet Gynecol. 2005;25:169–76. https://doi.org/10.1002/uog.1818.
Acknowledgments
I thank Paul Bassett for his help with the statistics. This project has been presented at IUGA 45th Virtual Annual Meeting 29 August–4 September 2020.
Author information
Authors and Affiliations
Contributions
Roper: Data collection, manuscript writing.
Thakar: Manuscript editing.
Sultan: Manuscript editing.
Corresponding author
Ethics declarations
Financial disclaimer/conflicts of interest
None.
Ethical approval
not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roper, J.C., Thakar, R. & Sultan, A.H. Under-classified obstetric anal sphincter injuries. Int Urogynecol J 33, 1473–1479 (2022). https://doi.org/10.1007/s00192-021-05051-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-05051-y



