Abstract
Purpose
To verify that lateral trochlear inclination (LTI) measured by the transepicondylar axis can reliably be used to evaluate trochlear dysplasia (TD) on MRI and can serve as an objective indication of trochleoplasty for patients with lateral patellar dislocation (LPD).
Methods
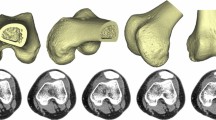
Eighty patients with recurrent LPD and eighty healthy subjects were included. TD, posterior condylar angle (PCA), and LTI measured by the posterior condylar reference line (LTIp), surgical transepicondylar axis (LTIs), and anatomical transepicondylar axis (LTIa) were assessed on MRI. The intraclass correlation coefficient (ICC) and Bland–Altman analysis were performed, the correlations and differences amongst the parameters were identified, and a binary logistic regression model was established.
Results
Each measurement had excellent inter- and intra-observer agreement. The LTIp, LTIs and LTIa were smaller in the study group than in the control group, with mean differences of 9.0°, 7.2° and 7.0°, respectively (P < 0.001). The PCA was larger in patients with LPD than in the control group (P < 0.001). LTIp was associated with PCA in the study group (r = − 0.41, P < 0.001). The pathological values of LTIp, LTIs and LTIa were 11.7°, 15.3° and 17.4°, respectively. LTIs and LTIa were independent risk factors for LPD, with ORs of 7.33 (95% CI [1.06–52.90], P = 0.048) and 10.29 (95% CI [1.38–76.96], P = 0.023), respectively.
Conclusion
The LTI can be reliably measured by MRI, but LTIp could potentially decrease the recorded value from the actual inclination angle. LTIs and LTIa are more appropriate to serve as trochleoplasty indications for patients with LPD, which could help orthopedists with surgical decision-making.
Level of evidence
Level III.





Similar content being viewed by others
Code availability
Not applicable.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- AEA:
-
Anatomical transepicondylar axis
- IQR:
-
Interquartile range
- LOA:
-
Limits of agreement
- LPD:
-
Lateral patellar dislocation
- LTI:
-
Lateral trochlea inclination
- LTL:
-
A line subtended from the cartilaginous surface of the lateral trochlea
- PCA:
-
Posterior condylar angle
- PCRL:
-
Posterior condylar reference line
- SEA:
-
Surgical transepicondylar axis
- TD:
-
Trochlear dysplasia
References
Ahrend MD, Eisenmann T, Herbst M, Gueorguiev B, Keller G, Schmidutz F et al (2022) Increased tibial tubercle-trochlear groove and patellar height indicate a higher risk of recurrent patellar dislocation following medial reefing. Knee Surg Sports Traumatol Arthrosc 30:1404–1413
Balcarek P, Radebold T, Schulz X, Vogel D (2019) Geometry of torsional malalignment syndrome: trochlear dysplasia but not torsion predicts lateral patellar instability. Orthop J Sports Med 7:2325967119829790
Balcarek P, Zimmermann F (2019) Deepening trochleoplasty and medial patellofemoral ligament reconstruction normalize patellotrochlear congruence in severe trochlear dysplasia. Bone Joint J 101-b:325–330
Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA (2000) Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology 216:582–585
Chen J, Huang X, Xu Z, Zhang H, Zhou A, Zhao P et al (2021) Ipsilateral patellofemoral morphological abnormalities are more severe than those of contralateral joints in patients with unilateral patellar dislocation. Knee Surg Sports Traumatol Arthrosc 29:2709–2716
Chen J, Yin B, Yao J, Zhou Y, Zhang H, Zhang J et al (2023) Femoral anteversion measured by the surgical transepicondylar axis is a reliable parameter for evaluating femoral rotational deformities in patients with patellar dislocation. Knee Surg Sports Traumatol Arthrosc 31:3061–3069
D’Ambrosi R, Meena A, Raj A, Ursino N, Hewett TE (2022) Anterior knee pain: state of the art. Sports Med Open 8:98. https://doi.org/10.1186/s40798-022-00488-x
Fitzpatrick CK, Steensen RN, Alvarez O, Holcomb AE, Rullkoetter PJ (2023) Computational comparison of medializing tibial tubercle osteotomy and trochleoplasty in patients with trochlear dysplasia. J Orthop Res 41:1687–1696
Joseph SM, Cheng C, Solomito MJ, Pace JL (2020) Lateral trochlear inclination angle: measurement via a 2-image technique to reliably characterize and quantify trochlear dysplasia. Orthop J Sports Med 8:2325967120958415
Keser S, Savranlar A, Bayar A, Ege A, Turhan E (2008) Is there a relationship between anterior knee pain and femoral trochlear dysplasia? Assessment of lateral trochlear inclination by magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc 16:911–915
Levy BJ, Tanaka MJ, Fulkerson JP (2021) Current concepts regarding patellofemoral trochlear dysplasia. Am J Sports Med 49:1642–1650
Lippacher S, Dejour D, Elsharkawi M, Dornacher D, Ring C, Dreyhaupt J et al (2012) Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images. Am J Sports Med 40:837–843
Liu X, Ji G, Wang X, Kang H, Wang F (2017) CT-based morphological analysis of the posterior femoral condyle in patients with trochlear dysplasia. Knee 24:231–236
Meissburger V, Rougereau G, Langlais T, Boisrenoult P, Pujol N (2022) The severity of patellar and trochlear dysplasia are correlated. Knee Surg Sports Traumatol Arthrosc 30:3438–3443
Nacey NC, Fox MG, Luce BN, Boatman DM, Diduch DR (2020) Assessing femoral trochlear morphologic features on cross-sectional imaging before trochleoplasty: Dejour classification versus quantitative measurement. AJR Am J Roentgenol 215:458–464
Nelitz M, Lippacher S, Reichel H, Dornacher D (2014) Evaluation of trochlear dysplasia using MRI: correlation between the classification system of Dejour and objective parameters of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 22:120–127
Ng J, Broomfield J, Barbosa F, Bhangoo N, Geutjens G (2023) Low re-dislocation rate following Bereiter trochleoplasty for recurrent patellar instability with severe trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 31:2494–2499
Pace JL, Cheng C, Joseph SM, Solomito MJ (2020) Effect of trochlear dysplasia on commonly used radiographic parameters to assess patellar instability. Orthop J Sports Med 8:2325967120938760
Paiva M, Blønd L, Hölmich P, Steensen RN, Diederichs G, Feller JA et al (2018) Quality assessment of radiological measurements of trochlear dysplasia; a literature review. Knee Surg Sports Traumatol Arthrosc 26:746–755
Pruneski J, O’Mara L, Perrone GS, Kiapour AM (2022) Changes in anatomic risk factors for patellar instability during skeletal growth and maturation. Am J Sports Med 50:2424–2432
Roger J, Lustig S, Cerciello S, Bruno CF, Neyret P, Servien E (2019) Short lateral posterior condyle is associated with trochlea dysplasia and patellar dislocation. Knee Surg Sports Traumatol Arthrosc 27:731–739
Saccomanno MF, Maggini E, Vaisitti N, Pianelli A, Grava G, Cattaneo S et al (2023) Sulcus angle, trochlear depth, and Dejour’s classification can be reliably applied to evaluate trochlear dysplasia: a systematic review of radiological measurements. Arthroscopy 39:549–568
Tanaka MJ, Sodhi A, Wadhavkar I, Kane K, Velasquez Hammerle MV, Mangudi Varadarajan K et al (2023) Redefining trochlear dysplasia: normal thresholds vary by measurement technique, landmarks, and sex. Am J Sports Med 51:1202–1210
Uimonen M, Ponkilainen V, Hirvinen S, Mattila VM, Kask G, Nurmi H et al (2021) The risk of osteochondral fracture after patellar dislocation is related to patellofemoral anatomy. Knee Surg Sports Traumatol Arthrosc 29:4241–4250
Xu Z, Song Y, Deng R, Ye J, Wang X, Wang H et al (2023) CT and MRI measurements of tibial tubercle lateralization in patients with patellar dislocation were not equivalent but could be interchangeable. Knee Surg Sports Traumatol Arthrosc 31:349–357
Yang G, Dai Y, Dong C, Kang H, Niu J, Lin W et al (2020) Distal femoral morphological dysplasia is correlated with increased femoral torsion in patients with trochlear dysplasia and patellar instability. Bone Joint J 102-b:868–873
Yang G, Dai Y, Dong C, Niu Y, Kang H, Wang F (2023) Two-type classification system for femoral trochlear dysplasia in recurrent patellar instability based on three-dimensional morphology. Knee Surg Sports Traumatol Arthrosc 31:1790–1797
Zhao P, Chen J, Feng Y, Tan H, Yin B, Zhang H et al (2022) Tibial tubercle to trochlear groove distance measured by posterior condylar reference line on MRI can over-evaluate lateralization deformity of tibial tubercle in patients with recurrent patellar dislocation. J Clin Med 11:5072
Zimmermann F, Milinkovic DD, Balcarek P (2021) Outcomes after deepening trochleoplasty and concomitant realignment in patients with severe trochlear dysplasia with chronic patellofemoral pain: results at 2-year follow-up. Orthop J Sports Med 9:23259671211010404
Funding
The authors did not receive support from any organisation for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection was performed by JC, XL and QL, supervised by YF. Statistical analysis was conducted by JC. The first draft of the manuscript was written by JC and modified by ZX and LW. JZ, AZ and ZQ provided theoretical supports and revised the manuscript. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare they have no financial interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University. (Number: 2022-K36).
Consent to participate
The informed consent was waived by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, J., Li, X., Feng, Y. et al. Lateral trochlear inclination measured by the transepicondylar axis holds potential for evaluating trochlear dysplasia in patients with lateral patellar dislocation. Knee Surg Sports Traumatol Arthrosc 31, 5611–5620 (2023). https://doi.org/10.1007/s00167-023-07614-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07614-6