Abstract
Purpose
To determine the differences in anatomic parameters between ipsilateral dislocated knees and contralateral non-dislocated knees in patients with unilateral patellar dislocation and to identify any variations in ipsilateral knees contributing to contralateral anatomic abnormalities.
Methods
A total of 82 patients with unilateral patellar dislocation from 2016 to 2019 were retrospectively evaluated. Bilateral anatomic factors, including the tibial tubercle to trochlear groove (TT-TG) distance, lower limb rotational deformities, trochlear dysplasia, patella tilt, and patellar height, were assessed by CT.
Results
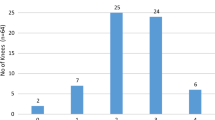
The study included 46 patients (32 females and 14 males, mean age ± SD 20.5 ± 6.8). The interobserver reliability of each parameter showed excellent agreement. The ipsilateral TT-TG distance (P = 0.004), patella tilt (P = 0.001), and patellar height (P = 0.01) were greater in the ipsilateral knees than in the contralateral knees. The lateral trochlea inclination (LTI) in the contralateral knees was larger than that in the ipsilateral knees (P = 0.022). There was a significant difference in the distribution of trochlear dysplasia of Dejour between the ipsilateral knees (dislocated side) and the contralateral knees (P = 0.036). However, bilateral femoral and/or tibial torsion, and bilateral knee joint rotation did not differ significantly. Binary logistic regression showed that only ipsilateral LTI revealed significant ORs of 8.83 (P = 0.016) and 7.64 (P = 0.018) with regard to contralateral abnormal tibial torsion and LTI, respectively.
Conclusion
In patients with unilateral patellar dislocation, the ipsilateral TT-TG distance, patella tilt, and patellar height values were larger in the ipsilateral knees than in the contralateral knees, and trochlear dysplasia was more severe in the ipsilateral joints. The risks of contralateral pathological tibial torsion and LTI were 8.8- and 7.6-fold higher, respectively, in patients with abnormal ipsilateral LTI.
Level of evidence
Level IV.




Similar content being viewed by others
References
Balcarek P, Oberthür S, Hopfensitz S, Frosch S, Walde TA, Wachowski MM et al (2014) Which patellae are likely to redislocate? Knee Surg Sports Traumatol Arthrosc 22:2308–2314
Bayhan IA, Kirat A, Alpay Y, Ozkul B, Kargin D (2018) Tibial tubercle-trochlear groove distance and angle are higher in children with patellar instability. Knee Surg Sports Traumatol Arthrosc 26:3566–3571
Brady JM, Rosencrans AS, Shubin Stein BE (2018) Use of TT-PCL versus TT-TG. Curr Rev Musculoskelet Med 11:261–265
Brady JM, Sullivan JP, Nguyen J, Mintz D, Green DW, Strickland S et al (2017) The tibial tubercle-to-trochlear groove distance is reliable in the setting of trochlear dysplasia, and superior to the tibial tubercle-to-posterior cruciate ligament distance when evaluating coronal malalignment in patellofemoral instability. Arthroscopy 33:2026–2034
Carlson VR, Boden BP, Shen A, Jackson JN, Yao L, Sheehan FT (2017) The tibial tubercle-trochlear groove distance is greater in patients with patellofemoral pain: implications for the origin of pain and clinical interventions. Am J Sports Med 45:1110–1116
Christensen TC, Sanders TL, Pareek A, Mohan R, Dahm DL, Krych AJ (2017) Risk factors and time to recurrent ipsilateral and contralateral patellar dislocations. Am J Sports Med 45:2105–2110
Dagneaux L, Bin Abd Razak HR, Laumonerie P, Faizhan A, LiArno S, Wellings P et al (2021) Bony asymmetry in patellofemoral morphology and risk factors of instability are mostly clinically negligible. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06413-7
Demehri S, Thawait GK, Williams AA, Kompel A, Elias JJ, Carrino JA et al (2014) Imaging characteristics of contralateral asymptomatic patellofemoral joints in patients with unilateral instability. Radiology 273:821–830
Erickson BJ, Nguyen J, Gasik K, Gruber S, Brady J, Shubin Stein BE (2019) Isolated medial patellofemoral ligament reconstruction for patellar instability regardless of tibial tubercle-trochlear groove distance and patellar height: outcomes at 1 and 2 years. Am J Sports Med 47:1331–1337
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA et al (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32:1114–1121
Franciozi CE, Ambra LF, Albertoni LJ, Debieux P, Rezende FC, Oliveira MA et al (2017) Increased femoral anteversion influence over surgically treated recurrent patellar instability patients. Arthroscopy 33:633–640
Franciozi CE, Ambra LF, Albertoni LJB, Debieux P, Granata GSM Jr, Kubota MS et al (2019) Anteromedial tibial tubercle osteotomy improves results of medial patellofemoral ligament reconstruction for recurrent patellar instability in patients with tibial tuberosity-trochlear groove distance of 17 to 20 mm. Arthroscopy 35:566–574
Gravesen KS, Kallemose T, Blønd L, Troelsen A, Barfod KW (2018) High incidence of acute and recurrent patellar dislocations: a retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg Sports Traumatol Arthrosc 26:1204–1209
Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA (2019) Factors associated with an increased risk of recurrence after a first-time patellar dislocation: a systematic review and meta-analysis. Am J Sports Med 48:2552–2562
Kaiser P, Konschake M, Loth F, Plaikner M, Attal R, Liebensteiner M et al (2020) Derotational femoral osteotomy changes patella tilt, patella engagement and tibial tuberosity trochlear groove distance. Knee Surg Sports Traumatol Arthrosc 28:926–933
Kaiser P, Loth F, Attal R, Kummann M, Schuster P, Riechelmann F et al (2020) Static patella tilt and axial engagement in knee extension are mainly influenced by knee torsion, the tibial tubercle-trochlear groove distance (TTTG), and trochlear dysplasia but not by femoral or tibial torsion. Knee Surg Sports Traumatol Arthrosc 28:952–959
Kaiser P, Schmoelz W, Schoettle P, Zwierzina M, Heinrichs C, Attal R (2017) Increased internal femoral torsion can be regarded as a risk factor for patellar instability - A biomechanical study. Clin Biomech (Bristol, Avon) 47:103–109
Kuroda Y, Matsushita T, Matsumoto T, Kawakami Y, Kurosaka M, Kuroda R (2014) Bilateral medial patellofemoral ligament reconstruction in high-level athletes. Knee Surg Sports Traumatol Arthrosc 22:2465–2469
Levy BJ, Tanaka MJ, Fulkerson JP (2020) Current concepts regarding patellofemoral trochlear dysplasia. Am J Sports Med. https://doi.org/10.1177/0363546520958423363546520958423
Lin KM, James EW, Aitchison AH, Schlichte LM, Wang G, Green DW (2021) Increased tibiofemoral rotation on MRI with increasing clinical severity of patellar instability. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06382-x
Lippacher S, Dejour D, Elsharkawi M, Dornacher D, Ring C, Dreyhaupt J et al (2012) Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images. Am J Sports Med 40:837–843
Marcacci M, Zaffagnini S, Iacono F, Visani A, Petitto A, Neri NP (1995) Results in the treatment of recurrent dislocation of the patella after 30 years’ follow-up. Knee Surg Sports Traumatol Arthrosc 3:163–166
Nelitz M, Lippacher S, Reichel H, Dornacher D (2014) Evaluation of trochlear dysplasia using MRI: correlation between the classification system of Dejour and objective parameters of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 22:120–127
Paiva M, Blønd L, Hölmich P, Steensen RN, Diederichs G, Feller JA et al (2018) Quality assessment of radiological measurements of trochlear dysplasia; a literature review. Knee Surg Sports Traumatol Arthrosc 26:746–755
Parikh SN, Lykissas MG, Gkiatas I (2018) Predicting risk of recurrent patellar dislocation. Curr Rev Musculoskelet Med 11:253–260
Rebolledo BJ, Nam D, Cross MB, Green DW, Sculco TP (2012) Familial association of femoral trochlear dysplasia with recurrent bilateral patellar dislocation. Orthopedics 35:e574-579
Sanders TL, Pareek A, Hewett TE, Stuart MJ, Dahm DL, Krych AJ (2018) High rate of recurrent patellar dislocation in skeletally immature patients: a long-term population-based study. Knee Surg Sports Traumatol Arthrosc 26:1037–1043
Schöttle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J (2005) Trochleaplasty for patellar instability due to trochlear dysplasia: a minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop 76:693–698
Seitlinger G, Ladenhauf HN, Wierer G (2018) What is the chance that a patella dislocation will happen a second time: update on the natural history of a first time patella dislocation in the adolescent. Curr Opin Pediatr 30:65–70
Seitlinger G, Moroder P, Scheurecker G, Hofmann S, Grelsamer RP (2016) The Contribution of Different Femur Segments to Overall Femoral Torsion. Am J Sports Med 44:1796–1800
Stephen JM, Lumpaopong P, Dodds AL, Williams A, Amis AA (2015) The effect of tibial tuberosity medialization and lateralization on patellofemoral joint kinematics, contact mechanics, and stability. Am J Sports Med 43:186–194
Takagi S, Sato T, Watanabe S, Tanifuji O, Mochizuki T, Omori G et al (2018) Alignment in the transverse plane, but not sagittal or coronal plane, affects the risk of recurrent patella dislocation. Knee Surg Sports Traumatol Arthrosc 26:2891–2898
Tokgöz MA, Çavuşoğlu AT, Ayanoğlu T, Elma T, Vural A (2017) Neglected bilateral congenital dislocation of the patella. Eklem Hastalik Cerrahisi 28:128–131
Verhulst FV, van Sambeeck JDP, Olthuis GS, van der Ree J, Koëter S (2020) Patellar height measurements: Insall-Salvati ratio is most reliable method. Knee Surg Sports Traumatol Arthrosc 28:869–875
Xiong R, Chen C, Yin L, Gong X, Luo J, Wang F et al (2018) How Do Axial Scan Orientation Deviations Affect the Measurements of Knee Anatomical Parameters Associated with Patellofemoral Instability? A Simulated Computed Tomography Study. J Knee Surg 31:425–432
Xu Z, Zhang H, Chen J, Mohamed SI, Zhou A (2020) Femoral anteversion is related to tibial tubercle-trochlear groove distance in patients with patellar dislocation. Arthroscopy 36:1114–1120
Xu Z, Zhang H, Fu B, Mohamed SI, Zhang J, Zhou A (2020) Tibial tubercle-roman arch distance: a new measurement of patellar dislocation and indication of tibial tubercle osteotomy. Orthop J Sports Med 8:2325967120914872
Xu Z, Zhang H, Yan W, Qiu M, Zhang J, Zhou A (2021) Validating the role of tibial tubercle-posterior cruciate ligament distance and tibial tubercle-trochlear groove distance measured by magnetic resonance imaging in patients with patellar dislocation: a diagnostic study. Arthroscopy 37:234–242
Yang G, Dai Y, Dong C, Kang H, Niu J, Lin W, et al. (2020) Distal femoral morphological dysplasia is correlated with increased femoral torsion in patients with trochlear dysplasia and patellar instability. Bone Joint J 102-b:868–873
Zhang Z, Zhang H, Song G, Wang X, Zhang J, Zheng T et al (2020) A high-grade J sign is more likely to yield higher postoperative patellar laxity and residual maltracking in patients with recurrent patellar dislocation treated with derotational distal femoral osteotomy. Am J Sports Med 48:117–127
Acknowledgements
None.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by PZ, LY and ZX. The first draft of the manuscript was written by JC, and modified by XH. HZ and AZ provided theoretical supports and retrospectively verify the diagnosis of unilateral patellar dislocation of all patients. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no financial interests.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University. (Number: 2019–228).
Consent to participate
The informed consent was waived by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University in view of the retrospective nature of the study.
Availability of data and material
The data used to support the findings of this study are available from the corresponding author upon request.
Code availability
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, J., Huang, X., Xu, Z. et al. Ipsilateral patellofemoral morphological abnormalities are more severe than those of contralateral joints in patients with unilateral patellar dislocation. Knee Surg Sports Traumatol Arthrosc 29, 2709–2716 (2021). https://doi.org/10.1007/s00167-021-06539-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06539-2