Abstract
Purpose
The high flow nasal cannula (HFNC) has recently been proposed to support infants with respiratory syncytial virus (RSV)-related respiratory distress. However, in this disease, no physiologic data are currently available on the effects of this device. We assessed the capacity of HFNC to generate positive airway pressure, as well as the resulting effects on breathing pattern and respiratory effort.
Methods
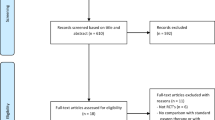
Twenty-one infants less than 6 months old with acute RSV bronchiolitis were studied prospectively in the pediatric intensive care unit of a university hospital. Pharyngeal pressure (PP) and esophageal pressure (Pes) were measured simultaneously at four increasing flows of 1, 4, 6 and 7 L/min delivered through HFNC.
Results
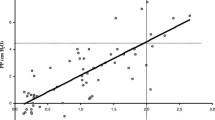
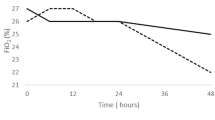
The PP was correlated with flow rate (r = 0.65, p ≤ 0.0001), reaching mean and end-expiratory values of, respectively, 4 (95% CI 3–5) cmH2O and 6.5 (95% CI 5–8) cmH2O at 7 L/min. A flow ≥2 L/kg/min was associated with the generation of a mean pharyngeal pressure ≥4 cmH2O with a sensitivity of 67 %, a specificity of 96 %, a positive predictive value of 75 %, and a negative predictive value of 94.5%. Only flows ≥6 L/min provided positive PP throughout the respiratory cycle. From baseline to maximal flow rate, breathing frequency (p < 0.01), T i/T tot (p < 0.05), Pes swing (p < 0.05) and PTPesinsp/min (p < 0.01), an index of respiratory effort, were reduced.
Conclusions
HFNC with a flow rate equal to or above 2 L/kg/min generated a clinically relevant PP, with improved breathing pattern and rapid unloading of respiratory muscles, in young infants with acute RSV bronchiolitis.



Similar content being viewed by others
References
American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis (2006) Diagnosis and management of bronchiolitis. Pediatrics 118:1774–1793
Welliver RC (2003) Review of epidemiology and clinical risk factors for severe respiratory syncytial virus (RSV) infection. J Pediatr 143:S112–S117
Hammer J, Numa A, Newth CJ (1997) Acute respiratory distress syndrome caused by respiratory syncytial virus. Pediatr Pulmonol 23:176–183
Essouri S, Durand P, Chevret L, Balu L, Devictor D, Fauroux B, Tissières P (2011) Optimal level of nasal continuous positive airway pressure in severe viral bronchiolitis. Intensive Care Med 37:2002–2007
Stokes GM, Milner AD, Groggins RC (1981) Work of breathing, intra-thoracic pressure and clinical findings in a group of babies with bronchiolitis. Acta Paediatr Scand 70:689–694
Cambonie G, Milési C, Jaber S, Amsallem F, Barbotte E, Picaud JC, Matecki S (2008) Nasal continuous positive airway pressure decreases respiratory muscles overload in young infants with severe acute viral bronchiolitis. Intensive Care Med 34:1865–1872
Muller NL, Bryan AC (1979) Chest wall mechanics and respiratory muscles in infants. Pediatr Clin N Am 26:503–516
Beasley JM, Jones SE (1981) Continuous positive airway pressure in bronchiolitis. Br Med J (Clin Res Ed) 283:1506–1508
Thia LP, McKenzie SA, Blyth TP, Minasian CC, Kozlowska WJ, Carr SB (2008) Randomised controlled trial of nasal continuous positive airways pressure (CPAP) in bronchiolitis. Arch Dis Child 93:45–47
Javouhey E, Barats A, Richard N, Stamm D, Floret D (2008) Non-invasive ventilation as primary ventilatory support for infants with severe bronchiolitis. Intensive Care Med 34:1608–1614
Milési C, Matecki S, Jaber S, Mura T, Jacquot A, Pidoux O, Chautemps N, Novais AR, Combes C, Picaud JC, Cambonie G (2012) 6 cm H2O positive airway pressure versus conventional oxygen therapy in severe viral bronchiolitis: a randomized trial. Pediatr Pulmonol. doi:10.1002/ppul.22533
Surenthiran SS, Wilbraham K, May J, Chant T, Emmerson AJ, Newton VE (2003) Noise levels within the ear and post-nasal space in neonates in intensive care. Arch Dis Child Fetal Neonatal Ed 88:F315–F318
Robertson NJ, McCarthy LS, Hamilton PA, Moss AL (1996) Nasal deformities resulting from flow driver continuous positive airway pressure. Arch Dis Child Fetal Neonatal Ed 75:F209–F212
McKiernan C, Chua LC, Visintainer PF, Allen H (2010) High flow nasal cannulae therapy in infants with bronchiolitis. J Pediatr 156:634–638
Schibler A, Pham TM, Dunster KR, Foster K, Barlow A, Gibbons K, Hough JL (2011) Reduced intubation rates for infants after introduction of high-flow nasal prong oxygen delivery. Intensive Care Med 37:847–852
Dysart K, Miller TL, Wolfson MR, Shaffer TH (2009) Research in high flow therapy: mechanisms of action. Respir Med 103:1400–1405
Kubicka ZJ, Limauro J, Darnall RA (2008) Heated, humidified high-flow nasal cannula therapy: yet another way to deliver continuous positive airway pressure? Pediatrics 121:82–88
Lampland AL, Plumm B, Meyers PA, Worwa CT, Mammel MC (2009) Observational study of humidified high-flow nasal cannula compared with nasal continuous positive airway pressure. J Pediatr 154:177–182
Spence KL, Murphy D, Kilian C, McGonigle R, Kilani RA (2007) High-flow nasal cannula as a device to provide continuous positive airway pressure in infants. J Perinatol 27:772–775
Wilkinson DJ, Andersen CC, Smith K, Holberton J (2008) Pharyngeal pressure with high-flow nasal cannulae in premature infants. J Perinatol 28:42–47
Parke R, McGuinness S, Eccleston M (2009) Nasal high-flow therapy delivers low level positive airway pressure. Br J Anaesth 103:886–890
Dani C, Pratesi S, Migliori C, Bertini G (2009) High flow nasal cannula therapy as respiratory support in the preterm infant. Pediatr Pulmonol 44:629–634
Collett PW, Perry C, Engel LA (1985) Pressure-time product, flow, and oxygen cost of resistive breathing in humans. J Appl Physiol 58:1263–1272
Spentzas T, Minarik M, Patters AB, Vinson B, Stidham G (2009) Children with respiratory distress treated with high-flow nasal cannula. J Intensive Care Med 24:323–328
Vilozni D, Efrati O, Barak A, Yahav Y, Augarten A, Bentur L (2009) Forced inspiratory flow volume curve in healthy young children. Pediatr Pulmonol 44:105–111
Martin RJ, Miller MJ, Siner B, DiFiore JM, Carlo WA (1989) Effects of unilateral nasal occlusion on ventilation and pulmonary resistance in infants. J Appl Physiol 66:2522–2526
Hasan RA, Habib RH (2011) Effects of flow rate and airleak at the nares and mouth opening on positive distending pressure delivery using commercially available high-flow nasal cannula systems: a lung model study. Pediatr Crit Care Med 12:e29–e33
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was carried out in the Pediatric Intensive Care Unit, Hôpital Arnaud de Villeneuve, CHU Montpellier, F-34000 France.
Rights and permissions
About this article
Cite this article
Milési, C., Baleine, J., Matecki, S. et al. Is treatment with a high flow nasal cannula effective in acute viral bronchiolitis? A physiologic study. Intensive Care Med 39, 1088–1094 (2013). https://doi.org/10.1007/s00134-013-2879-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-2879-y