Abstract
Background
Prosthetic valve thrombosis (PVT) is serious complication of valvular replacement surgery, and increased levels of anticardiolipin antibodies (aCL) are associated with thrombosis. The aim of this study was to evaluate the role of aCL in the development of PVT.
Patients and methods
We studied the aCL IgM and IgG levels in 114 patients with PVT and 80 healthy patients with prosthetic valves without PVT or a history of thrombosis. All patients underwent detailed transthoracic, transesophageal echocardiographic and clinical examinations. Blood samples were obtained after transesophageal echocardiography. Tests were repeated 12 weeks apart in patients with aCL IgM or IgG positivity.
Results
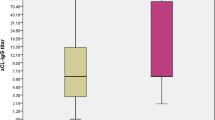
The mean age, sex, presence of atrial fibrillation and cardiovascular risk factors, elapsed time after surgery, and prosthetic valve type and location were similar between patients with PVT and those without. Ineffective anticoagulation was significantly higher among patients with PVT (p < 0.001). The aCL IgM values were significantly higher and positive (> 40 MPL) in the PVT group compared with the control group (10.58 ± 15.90 MPL to 3.70 ± 2.30 MPL, p < 0.001; 7.0 to 0 %, p = 0.016, respectively). The aCL IgG values were significantly higher and positive (> 40 GPL) in the PVT group compared with the control group (12.04 ± 17.58 GPL to 3.83 ± 2.56 GPL, p < 0.001 and 7.9 to 0 %, p = 0.01, respectively). According to international consensus documents, 16 patients had antiphospholipid syndrome. Ineffective anticoagulation and aCL IgM and IgG positivity were independent predictors of PVT in logistic regression analysis (multivariate r2= 0.648; p < 0.001, OR= 21.405, 95 %CI= 8.201–55.872; p = 0.008, OR= 1.322, %95CI= 1.076–1.626; p = 0.005, OR= 1.288, 95 %CI= 1.079–1.538).
Conclusion
Since the presence of aCL IgM and IgG positivity may cause a tendency toward PVT, these values should be examined in all patients with PVT.
Zusammenfassung
Hintergrund
Die Thrombose der Herzklappenprothese (“prosthetic valve thrombosis”, PVT) ist eine ernste Komplikation der Klappenersatzchirurgie, mit einer solchen Thrombose gehen erhöhte Werte für Anticardiolipin-Antikörper (aCL) einher. Ziel der vorliegenden Studie ist es, die Rolle von aCL bei der Entstehung einer PVT zu bestimmen.
Patienten und Methoden
Es wurden aCL-IgM und -IgG bei 114 Patienten mit PVT und 80 gesunden Patienten mit Klappenprothesen ohne PVT und ohne Thrombose in der Anamnese bestimmt. Bei sämtlichen Patienten wurden eine ausführliche transthorakale und transösophageale Echokardiographie sowie eine klinische Untersuchung durchgeführt. Nach der transösophagealen Echokardiographie wurden Blutproben entnommen. Bei Patienten mit positivem aCL-IgM und -IgG wurden die Untersuchungen nach 12 Wochen wiederholt.
Ergebnisse
Das Durchschnittsalter, Geschlecht, Vorliegen eines Vorhofflimmerns und kardiovaskulärer Risikofaktoren, Zeit seit der Operation, Art der Klappenprothese und ihre Lokalisation waren für Patienten mit und für Patienten ohne PVT ähnlich. Eine ineffektive Antikoagulation war bei Patienten mit PVT signifikant häufiger (p < 0,001). Der Wert für aCL-IgM war in der PVT-Gruppe im Vergleich zu den Kontrollen signifikant höher (10,58 ± 15,90 Standard-IgM-aCL-Einheiten, MPL bzw. 3,70 ± 2,30 MPL; p < 0,001; 7,0 % bzw. 0 %; p = 0,016) und positiv (> 40 MPL). Der Wert für aCL-IgG war in der PVT-Gruppe im Vergleich zu den Kontrollen signifikant höher (12,04 ± 17,58 Standard-IgG-aCL-Einheiten, GPL bzw. 3,83 ± 2,56 GPL; p < 0,001 und 7,9 % bzw. 0 %; p = 0,01) und positiv (> 40 GPL). Gemäß den Kriterien des internationalen Konsensuspapiers lag bei 16 Patienten ein Antiphospholipidsyndrom vor. Eine infeffektive Antikoagulation sowie positive Werte für aCL-IgM und -IgG waren unabhängige Prädiktoren einer PVT in der logistischen Regressionsanalyse (multivariates r2= 0,648; p < 0,001; OR= 21,405; 95%-KI= 8,201–55,872; p = 0,008; OR= 1,322; 95%-KI= 1,076–1,626; p = 0,005; OR= 1,288; 95%-KI= 1,079–1,538).
Schlussfolgerung
Da das Vorliegen positiver Werte für aCL-IgM und -IgG möglicherweise eine Neigung zur PVT bedingt, sollte dieser Wert bei allen Patienten mit PVT untersucht werden.


Similar content being viewed by others
References
Wilson WA, Gharavi AE, Koike T et al (1999) International consensus statement on preliminary classification criteria for definite antiphospholipid syndrome: report of an international workshop. Arthritis Rheum 42:1309–1311
Miyakis S, Lockshin MD, Atsumi T et al (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4:295–306
McNeil HP, Simpson RJ, Chesterman CN et al (1990) Anti-phospholipid antibodies are directed against a complex antigen that includes a lipid-binding inhibitor of coagulation: beta 2-glycoprotein I (apolipoprotein H). Proc Natl Acad Sci U S A 87:4120–4124
Galli M, Comfurius P, Maassen C et al (1990) Anticardiolipin antibodies (ACA) directed not to cardiolipin but to a plasma protein cofactor. Lancet 335:1544–1547
Ozkan M, Gündüz S, Biteker M et al (2013) Comparison of different TEE-guided thrombolytic regimens for prosthetic valve thrombosis: the TROIA trial. JACC Cardiovasc Imaging 6:206–216
Özkan M, Kaymaz C, Kırma C et al (2000) Intravenous thrombolytic treatment of mechanical prosthetic valve thrombosis: a study using serial transesophageal echocardiography. J Am Coll Cardiol 35:1881–1889
Tincani A, Allegri F, Sanmarco M et al (2001) Anticardiolipin antibody assay: a methodological analysis for a better consensus in routine determinations: a cooperative project of the European Antiphospholipid Forum. Thromb Haemost 86:575–583
Brandt JT, Barna LK, Triplett DA (1995) Laboratory identification of lupus anticoagulants: results of the Second International Workshop for Identification of Lupus Anticoagulants. Thromb Haemost 74:1597–1603
Pengo V, Biasiolo A, Pegoraro C et al (2005) Antibody profiles for the diagnosis of antiphospholipid syndrome. Thromb Haemost 93:1147–1152
Tarr T, Lakos G, Bhattoa HP et al (2007) Analysis of risk factors for the development of thrombotic complications in antiphospholipid antibody positive lupus patients. Lupus 16:39–45
Ruffatti A, Tonello M, Del Ross T et al (2006) Antibody profile and clinical course in primary antiphospholipid syndrome with pregnancy morbidity. Thromb Haemost 96:337–341
The APASS Writing Committee (2004) Antiphospholipid antibodies and subsequent thrombo-occlusiveevents in patients with ischemic stroke. JAMA 291:576–584
Schulman S, Svenungsson E, Granqvist S (1998) Duration of anticoagulation study group. Anticardiolipin antibodies predict early recurrence of thromboembolism and death among patients with venous thromboembolism following anticoagulant therapy. Am J Med 104:332–338
Groot PG de, Lutters B, Derksen RH et al (2005) Lupus anticoagulants and the risk of a first episode of deep venous thrombosis. J Thromb Haemost 3:1993–1997
Petri M (2002) Epidemiology of systemic lupus erythematosus. Best Pract Res Clin Rheumatol 16:847–858
Shi W, Krilis SA, Chong BH et al (1990) Prevalence of lupus anticoagulant and anticardiolipin antibodies in a healthy population. Aust N Z J Med 20:231–236
Crowther MA, Wisloff F (2005) Evidence based treatment of the antiphospholipid syndrome II: optimal anticoagulant therapy for thrombosis. Thromb Res 115:3–8
Kearon C, Gent M, Hirsh J et al (1999) A comparison of three months of anticoagulation with extended anticoagulation for a first episode of idiopathic venous thromboembolism. N Engl J Med 340:901–907
Kearon C, Ginsberg JS, Kovacs MJ et al (2003) Comparison of low-intensity warfarin therapy with conventional- intensity warfarin therapy for long-term prevention of recurrent venous thromboembolism. N Engl J Med 349:631–639
Rosove MH, Brewer PM (1992) Antiphospholipid thrombosis: clinical course after the first thrombotic event in 70 patients. Ann Intern Med 117:303–308
Khamashta MA, Cuadrado MJ, Mujic F et al (1995) The management of thrombosis in the antiphospholipid-antibody syndrome. N Engl J Med 332:993–997
Compliance with ethical guidelines
Conflict of interest. A.C. Aykan, T. Gökdeniz, M. Kalçık, M.A. Astarcıoğlu, S. Gündüz, S. Karakoyun, M.O. Gürsoy, A.E. Oğuz, E. Ertürk, B. Çakal, Z. Bayram, and M. Özkan state that there are no conflicts of interest. All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aykan, A., Gökdeniz, T., Kalçık, M. et al. Role of anticardiolipin antibodies in the pathogenesis of prosthetic valve thrombosis. Herz 40, 528–533 (2015). https://doi.org/10.1007/s00059-013-4038-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-013-4038-1