Abstract
Objectives
Antiphospholipid syndrome (APS) is multisystem autoimmune coagulopathy with antiphospholipid antibodies (aPL) in its ground, manifested as a primary disease (PAPS) or in the setting of other conditions, most commonly systemic lupus erythematosus. The objective of this cross-sectional study was to investigate various cardiac manifestations and their possible relation to aPL type and titer in a Serbian cohort of PAPS patients.
Methods
A total of 360 PAPS patients were analyzed and aPL analysis included detection of anticardiolipin antibodies (aCL: IgG/IgM), anti-ß2glycoprotein I (ß2GPI: IgG/IgM), and lupus anticoagulant (LA). Cardiac manifestations investigated were valvular lesions (comprehending valvular thickening and dysfunction not related to age and pseudoinfective endocarditis), coronary artery disease (CAD) with specific insight for myocardial infarction (MI), chronic cardiomyopathy (CMP), and acute decompensated heart failure (ADHF) as well as pulmonary hypertension (PH) and intracardiac thrombus presence.
Results
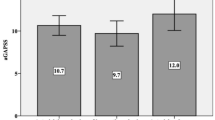
The prevalence of cardiac manifestations overall was 19.6%. There was a strong association between age and the majority of cardiac manifestations, as well as standard atherosclerotic risk factors. aCL IgG–positive patients had a higher prevalence of valvular lesions (p = 0.042). LA presence was significantly related to MI (p = 0.031) and PH (p = 0.044). CMP and ADHF were significantly related to higher titers of aCl IgG (p = 0.033, p = 0.025 respectively). Age and smoking were independent risk predictors for MI in PAPS with meaningful risk for LA positivity (OR 2.567 CI 0.671–9.820 p = 0.168).
Conclusions
Certain cardiac manifestations in PAPS were related to certain aPL type and/or titer levels, imposing confirmation in prospective studies. Preventive actions, comprehending proper anticoagulant/antithrombotic therapy, and intense action against standard atherosclerotic risk factors are of utmost importance in this group of patients.
Key Points • In Serbian patients with primary antiphospholipid syndrome (PAPS), prevalence of non-criteria cardiac manifestations was 19.6% and they were significantly related to certain antiphospholipid antibodies and titers. • Lupus anticoagulant was a meaningful predictor of myocardial infarction, enabling possible risk stratification and proper preventive and therapeutical strategies in this subgroup of PAPS patients. • Patients with high titers of aCL IgG are more prone to acute decompensated heart failure occurence, imposing careful follow-up of these patients • Based on the analysis of the Serbian PAPS cohort, even being non-criterial, cardiology manifestations are significantly present and inclusion of cardiologists in treatment and follow-up of these patients should be implied from the diagnosis establishment. |

Similar content being viewed by others
References
Petri M (2000) Epidemiology of the antiphospholipid antibody syndrome. J Autoimmun 15:145–151. https://doi.org/10.1006/jaut.2000.0409
Hughes GR (1993) The antiphospholipid syndrome: ten years on. Lancet 342:341–344. https://doi.org/10.1016/0140-6736(93)91477-4
Djokovic A, Stojanovich L, Stanisavljevic N, Banicevic S, Smiljanic D, Milovanovic B (2018) Relationship between cerebrovascular and valvular manifestations in a Serbian cohort of patients with antiphospholipid syndrome. Clin Exp Rheumatol 36(5):850–855
Kolitz T, Shiber S, Sharabi I, Winder A, Zandman-Goddard G (2019) Cardiac manifestations of antiphospholipid syndrome with focus on its primary form. Front Immunol 10:941. https://doi.org/10.3389/fimmu.2019.00941
Bertolaccini ML, Khamashta MA, Hughes GR (2005) Diagnosis of antiphospholipid syndrome. Nat Clin Pract Rheumatol 1:40–46. https://doi.org/10.1038/ncprheum0017
Denas G, Jose SP, Bracco A, Zoppellaro G, Pengo V (2015) Antiphospholipid syndrome and the heart: a case series and literature review. Autoimmun Rev 14(3):214–222. https://doi.org/10.1016/j.autrev.2014.11.003
de Souza AW, Silva NP, de Carvalho JF, D’Almeida V, Noguti MA, El S (2007) Impact of hypertension and hyperhomocystenemia on arterial thrombosis in primary antiphospholipid syndrome. Lupus 16:782–787. https://doi.org/10.1177/0961203307081847
Zuily S, Huttin O, Mohamed S, Marie PY, Selton-Suty C, Wahl D (2013) Valvular heart disease in antiphospholipid syndrome. Curr Rheumatol Rep 15:320. https://doi.org/10.1007/s11926-013-0320-8
Cervera R, Piette JC, Font J, Khamashta MA, Shoenfeld Y, Camps MT et al (2002) Antiphospholipid syndrome: clinical and immunologic manifestations and patterns of disease expression in a cohort of 1,000 patients. Arthritis Rheum 46:1019–1027. https://doi.org/10.1002/art.10187
Erkan D, Asherson RA, Espinosa G (2003) Long term outcome of catastrophic antiphospholipid syndrome survivors. Ann Rheum Dis 62:530–533. https://doi.org/10.1136/ard.62.6.530
Narshi CB, Giles IP, Rahman A (2011) The endothelium: an interface between autoimmunity and atherosclerosis in systemic lupus erythematosus? Lupus 20:5–13. https://doi.org/10.1177/0961203310382429
Volkov I, Seguro L, Leon EP, Kovács L, Roggenbuck D, Schierack P et al (2020) Profiles of criteria and non-criteria anti-phospholipid autoantibodies are associated with clinical phenotypes of the antiphospholipid syndrome. Auto Immun Highlights 11(1):8. https://doi.org/10.1186/s13317-020-00131-3
Sciascia S, Amigo MC, Roccatello D, Khamashta M (2017) Diagnosing antiphospholipid syndrome: ‘extra-criteria’ manifestations and technical advances. Nat Rev Rheumatol 13(9):548–560. https://doi.org/10.1038/nrrheum.2017.124
Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R et al (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4:295–306. https://doi.org/10.1111/j.1538-7836.2006.01753.x
Cervera R. CAPS Registry Project Group (2010) Catastrophic antiphospholipid syndrome (CAPS): update from the “CAPS Registry.” Lupus 19:412–418. https://doi.org/10.1177/0961203309361353
Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T et al (2000) Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30:633. https://doi.org/10.1086/313753
Tektonidou MG, Andreoli L, Limper M, Amoura Z, Cervera R, Costedoat-Chalumeau N et al (2019) EULAR recommendations for the management of antiphospholipid syndrome in adults. Ann Rheum Dis 78(10):1296–1304. https://doi.org/10.1136/annrheumdis-2019-215213
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K et al (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23(7):685–713. https://doi.org/10.1016/j.echo.2010.05.010
Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A et al (2015) 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J 46(4):903–975. https://doi.org/10.1093/eurheartj/ehv317
Pengo V, Tripodi A, Reber G, Rand JH, Ortel TL, Galli M et al (2009) Subcommittee on lupus anticoagulant/antiphospholipid antibody of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis. Update of the guidelines for lupus anticoagulant detection. J Thromb Haemost 7:1737–1740. https://doi.org/10.1111/j.1538-7836.2009.03555.x
Ruiz-Irastorza G, Crowther M, Branch W, Khamashta MA (2010) Antiphospholipid syndrome. Lancet 376:1498–1509. https://doi.org/10.1016/S0140-6736(10)60709-X
Devreese KMJ (2020) How to interpret antiphospholipid laboratory tests. Curr Rheumatol Rep 22(8):38. https://doi.org/10.1007/s11926-020-00916-5
Pengo V, Biasiolo A, Pegoraro C, Cucchini U, Noventa F, Iliceto S (2005) Antibody profiles for the diagnosis of antiphospholipid syndrome. Thromb Haemost 93:1147–1152. https://doi.org/10.1160/TH04-12-0839
Font J, Cervera R (2006) Cardiac manifestations in antiphospholipid syndrome. In: Khamashta MA (ed) Hughes Syndrome. 2nd edn. Singapore Springer pp 41–53
Cervera R, Serrano R, Pons-Estel GJ, Ceberio-Hualde L, Shoenfeld Y, de Ramón E et al (2015) Morbidity and mortality in the antiphospholipid syndrome during a 10-year period: a multicentre prospective study of 1000 patients. Ann Rheum Dis 74:1011–1018. https://doi.org/10.1136/annrheumdis-2013-204838
Djokovic A, Stojanovich L, Kontic M, Stanisavljevic N, Radovanovic S, Marisavljevic D (2014) Association between cardiac manifestations and antiphospholipid antibody type and level in a cohort of Serbian patients with primary and secondary antiphospholipid syndrome. Isr Med Assoc J 16:162–167
Pengo V, Ruffatti A, Legnani C, Gresele P, Barcellona D, Erba N et al (2010) Clinical course of high-risk patients diagnosed with antiphospholipid syndrome. J Thromb Haemost 8(2):237–242. https://doi.org/10.1111/j.1538-7836.2009.03674.x
Stojanovich L, Kontic M, Smiljanic D, Djokovic A, Stamenkovic B, Marisavljevic D (2013) Association between non-thrombotic neurological and cardiac manifestations in patients with antiphospholipid syndrome. Clin Exp Rheumatol 31(2):234–242
Stojanovich L, Djokovic A, Kontic M (2015) Antiphospholipid-mediated thrombosis: interplay between type of antibodies and localisation of lung, and cardiovascular incidences in primary antiphospholipid syndrome. Clin Exp Rheumatol 33(4):531–536
Kelchtermans H, Chayouâ W, de Laat B (2018) The significance of antibodies against domain I of beta-2 glycoprotein I in antiphospholipid syndrome. Semin Thromb Hemost 44(05):458–465. https://doi.org/10.1055/s-0037-1601329
Urbanus RT, Siegerink B, Roest M, Rosendaal FR, de Groot PG, Algra A (2009) Antiphospholipid antibodies and risk of myocardial infarction and ischaemic stroke in young women in the RATIO study: a case-control study. Lancet Neurol 8:998–1005. https://doi.org/10.1016/S1474-4422(09)70239-X
Molhoek JE, de Groot PG, Urbanus RT (2018) The lupus anticoagulant paradox. Semin Thromb Hemost 44(05):445–452. https://doi.org/10.1055/s-0037-1606190
Erkan D, Barbhaiya M, George D, Sammaritano L, Lockshin Md (2010) Moderate versus high-titer persistently anticardiolipin antibody positive patients: are they clinically different and does high-titer anti-beta 2-glycoprotein-I antibody positivity offer additional predictive information? Lupus 19(5):613–619. https://doi.org/10.1177/0961203309355300
Udry S, Latino JO, Belizna C, Perés Wingeyer S, Fernández Romero DS, de Larrañaga G (2019) A high-risk laboratory profile of antiphospholipid antibodies and thrombosis is associated with a large number of extra-criteria manifestations in obstetric antiphospholipid syndrome. Immunol Res 67(6):478–485. https://doi.org/10.1007/s12026-019-09110-x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Djokovic, A., Stojanovich, L., Stanisavljevic, N. et al. Cardiac manifestations in primary antiphospholipid syndrome and their association to antiphospholipid antibodies’ types and titers—cross-sectional study of Serbian cohort. Clin Rheumatol 41, 1447–1455 (2022). https://doi.org/10.1007/s10067-022-06056-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06056-8