Abstract
Background and aims
The relationship between serum amyloid A (SAA) and coronary heart disease (CHD) remains inconsistent, and the correlation of SAA levels and some factors have not been thoroughly evaluated in CHD. The present study assessed the associations of SAA levels and CHD, and the correlation of SAA levels and CRP, fibrinogen, interleukin-6 (IL-6), and HDL-C levels in CHD patient.
Methods
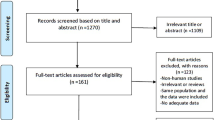
We systematically searched databases of Cochrane Library, PubMed, Embase, and ScienceDirect from their inception to 2018. Pooled standardized mean difference (SMD), correlation coefficient (r), and 95% confidence intervals (CI) were computed using random-effect model.
Result
A total of 26 studies were identified for analysis, involving a total of 6466 CHD cases and 16,184 participants. Compared with the control group, the case group had markedly higher SAA levels (SMD = 0.38, 95% CI 0.21, 0.56). Subgroup analysis manifested that SAA level difference between case group and control group were associated with age, continent, and study type. Moreover, meta-regression model suggested that different continent, sex, and publication year can explain the origin of 52.05%, 50.17%, 28.07% heterogeneity, respectively. By stratified analyses, we further found that the concentration of SAA increased gradually with the aggravation of CHD. Additionally, the meta-analysis of correlation showed that SAA levels were positively related with CRP (r = 0.45, 95% CI 0.19, 0.71), fibrinogen (r = 0.41, 95% CI 0.35, 0.47), and IL-6 (r = 0.48, 95% CI 0.41, 0.54) levels, but negatively linked with HDL-C levels (r = − 0.28, 95% CI − 0.38, − 0.18) in CHD patients.
Conclusion
High levels of SAA are significantly associated with increased risk of CHD, especially for participants aged more than 55 years, subjects from Europe and Asia, or case–control study. Furthermore, we find that SAA concentrations increased with the severity of CHD. Importantly, our study suggests that high levels of SAA might play a role in CHD by increasing CRP, fibrinogen, IL-6 levels, or attenuating HDL-C levels.






Similar content being viewed by others
References
Gaziano TA, Bitton A, Anand S, et al. Growing epidemic of coronary heart disease in low-and middle-income countries. Curr Probl Cardiol. 2010;35:72–115.
Tai ES, Tan CE. Genes, diet and serum lipid concentrations: lessons from ethnically diverse populations and their relevance to coronary heart disease in Asia. Curr Opin Lipidol. 2004;15:5–12.
Vilahur G, Badimon JJ, Bugiardini R, et al. Perspectives: The burden of cardiovascular risk factors and coronary heart disease in Europe and worldwide. Eur Heart J. 2014;16:A7–A11.
Bainey KR, Jugdutt BI. Increased burden of coronary artery disease in South-Asians living in North America. Need for an aggressive management algorithm. Atherosclerosis. 2009;204:1–10.
Galinsky AM, Zelaya CE, Simile C, et al. Health conditions and behaviors of native Hawaiian and Pacific islander persons in the United States, 2014. Vital Health Stat. 2017;3:1–99.
Izadnegahdar M, Mackay M, Lee MK, et al. Sex and ethnic differences in outcomes of acute coronary syndrome and stable angina patients with obstructive coronary artery disease. Circ Cardiovasc Qual Outcomes. 2016;9:S26–S35.
Naidoo DA. Board of Education of the Royal College of Pathologists of, broadsheet: biochemical markers of coronary heart disease. Pathology. 2001;33:329–37.
Overbaugh KJ. Acute coronary syndrome. Am J Nurs. 2009;109:42–52.
Cohen Y, Amir G, Da'As N, et al. Acute myocardial infarction as the presenting symptom of acute myeloblastic leukemia with extreme hyperleukocytosis. Am J Hematol. 2002;71:47–9.
Leow KY, Goh WW, Tan SZ, et al. Variant screening of the serum amyloid A1 gene and functional study of the p.Gly90Asp variant for its role in atherosclerosis. Atherosclerosis. 2013;227:112–7.
Yang RZ, Lee MJ, Hu H, et al. Acute-phase serum amyloid A: aninflammatory adipokine and potential link between obesity and its metabolic complications. Plos Med. 2006;3:e287.
Bremer AA, Devaraj S, Afify A, et al. Adipose tissue dysregulation in patients with metabolic syndrome. J Clin Endocrinol Metab. 2011;96:E1782–1788.
Wearn JG, Suagee JK, Crisman MV, et al. Effects of the insulin sensitizing drug, pioglitazone, and lipopolysaccharide administration on markers of systemic inflammation and clinical parameters in horses. Vet Immunol Immunopathol. 2012;145:42–9.
Fain JN. Release of interleukins and other inflammatory cytokines by human adipose tissue is enhanced in obesity and primarily due to the nonfat cells. Vitam Horm. 2006;74:443–77.
Li B, Luo BB, Qin WD, et al. Bidirectional effect of serum amyloid A on plaque stability. Int J Cardiol. 2014;174:179–83.
Song C, Hsu K, Yamen E, et al. Serum amyloid A induction of cytokines in monocytes/macrophages and lymphocytes. Atherosclerosis. 2009;207:374–83.
Li B, Dong Z, Liu H, et al. Serum amyloid A stimulates lipoprotein-associated phospholipase A2 expression in vitro and in vivo. Atherosclerosis. 2013;228:370–9.
Galis ZS, Sukhova GK, Lark MW, et al. Increased expression of matrix metallo proteinase and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J Clin Investig. 1994;94:2493–503.
Uhlar CM, Whitehead AS. Serum amyloid A, the major vertebrate acute-phase reactant. Eur J Biochem. 1999;265:501–23.
Chiba T, Han CY, Vaisar T, et al. Serum amyloid A3 does not contribute to circulating SAA levels. J Lipid Res. 2009;50:1353–62.
Bulut M, Keles N, Caliskan Z, et al. Is the presence of AA amyloidosis associated with impaired coronary flow reserve. Atherosclerosis. 2016;251:389–95.
Sukhova GK, Schonbeck U, Rabkin E, et al. Evidence for increased collagenolysis by interstitial collagenases-1 and-3 in vulnerable human atheromatous plaques. Circulation. 1999;99:2503–9.
Ridker PM, Hennekens CH, Buring JE, et al. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342:836–43.
Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Johnson BD, Kip KE, Marroquin OC, et al. Serum amyloid A as a predictor of coronary artery disease and cardiovascular outcome in women: the national heart, lung, and blood institute-sponsored women’s ischemia syndrome evaluation (WISE). Circulation. 2004;109:726–32.
Liu TLG, Li L, Korantzopoulos P. Association between C-reactive protein and recurren ceofatrial fibrillation after successful electrical cardioversion: a meta-analysis. J Am Coll Cardiol. 2007;49:1642–8.
Liu T, Li L, Korantzopoulos P, et al. Meta-analysis of association between C-reactive protein and immediate success of electrical cardioversion in persistent atrial fibrillation. Am J Cardiol. 2008;101:1749–52.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
Ekkekakis P. Honey, I shrunk the pooled SMD! Guide to critical appraisal of systematic reviews and meta-analyses using the cochrane review on exercise for depression as example. Ment Health Phys Act. 2015;8:21–36.
Bonett DG. Meta-analytic interval estimation for standardized and unstandardized mean differences. Psychol Methods. 2009;14:225–38.
Miyazak IT, Chiuve S, Sacks FM, et al. Plasma pentraxin 3 levels do not predict coronary events but reflect metabolic disorders in patients with coronary artery disease in the CARE trial. PLoS ONE. 2014;9:e94073.
Jousilahti P, Salomaa V, Rasi V, et al. The association of C-reactive protein, serum amyloid a and fibrinogen with prevalent coronary heart disease—baseline findings of the PAIS project. Atherosclerosis. 2001;156:451–6.
Delanghe JR, Langlois MR, Bacquer DD, et al. Discriminative value of serum amyloid A and other acute-phase proteins for coronary heart disease. Atherosclerosis. 2002;160:471–6.
Song C, Shen Y, Yamen E, et al. Serum amyloid A may potentiate prothrombotic and proinflammatory events in acute coronary syndromes. Atherosclerosis. 2009;202:596–604.
Wang DX, Liu H, Yan LR, et al. The relationship between serum amyloid A and apolipoprotein A–I in high-density lipoprotein isolated from patients with coronary heart disease. Chin Med J. 2013;126:3656–61.
Xie X, Ma YT, Yang YN, et al. Genetic polymorphisms of serum amyloid A1 and coronary artery disease risk. Tissue Antigens. 2015;85:168–76.
Bilginer Y, Ozaltin F, Basaran C, et al. Evaluation of intima media thickness of the common and internal carotid arteries with inflammatory markers in familial Mediterranean fever as possible predictors for atherosclerosis. Rheumatol Int. 2008;28:1211–6.
Backer JD, Mak R, Bacquer DD, et al. Parameters of inflammation and infection in a community based case-control study of coronary heart disease. Atherosclerosis. 2002;160:457–63.
Liu K, Tang Q, Zhu X, et al. IL-37 increased in patients with acute coronary syndrome and associated with a worse clinical outcome after ST-segment elevation acute myocardial infarction. Clin Chim Acta. 2017;468:140–4.
Song CJ. SAA induction of TNF in PBMC from patients with coronary artery disease. Heart Lung Circ. 2007;16:S170.
Alwaili K, Bailey D, Awan Z, et al. The HDL proteome in acute coronary syndromes shifts to an inflammatory profile. Biochim Biophys Acta. 2012;1821:405–15.
Omicron HB, Thomas GN, Bosch JA, et al. Evaluation of 9 biomarkers for predicting 10-year cardiovascular risk in patients undergoing coronary angiography: findings from the Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Int J Cardiol. 2013;168:2609–15.
Chen GL, Liu LW, Xie S, et al. High-density lipoprotein associated factors apoA-I and serum amyloid A in Chinese non-diabetic patients with coronary heart disease. Chin Med J. 2010;123:658–63.
Zairis MN, Adamopoulou EN, Manousakis SJ, et al. Outcome in acute coronary syndromes, the impact of hs C-reactive protein and other inflammatory biomarkers on long-term cardiovascular mortality in patients with acute coronary syndromes. Atherosclerosis. 2007;194:397–402.
Pussinen PJ, Sarna S, Puolakkainen M, et al. The balance of serum matrix metalloproteinase-8 and its tissue inhibitor in acute coronary syndrome and its recurrence. Int J Cardiol. 2013;167:362–8.
Eren E, Ellidag HY, Akar Y, et al. No association between vitamin D levels and inflammation markers in patients with acute coronary syndrome. Adv Med Sci. 2015;60:89–93.
Buffon A, Liuzzo G, Biasucci LM, et al. Preprocedural serum levels of C-reactive protein predict early complications and late restenosis after coronary angioplasty. J Am Coll Cardiol. 1999;34:1512–21.
Stefano DR, Bello DV, Barsotti MC, et al. Inflammatory markers and cardiac function in acute coronary syndrome: difference in ST-segment elevation myocardial infarction (STEMI) and in non-STEMI models. Biomed Pharmacother. 2009;63:773–80.
Korita I, Bulo A, Langlois MR, et al. Serum amyloid A is independently related to apolipoprotein A–I but not to HDL-cholesterol in patients with angina pectoris. Clin Biochem. 2013;46:1660–3.
Ehlers R, Buttcher E, Eltzschig HK, et al. Correlation between ST-T-segment changes with markers of hemostasis in patients with acute coronary syndromes. Cardiology. 2002;98:40–5.
Rott D, Leibowitz D, Yeheskel Z, et al. The relationship of plasminogen activator inhibitor-1 levels to the ST deviation pattern of acute myocardial infarction. Cardiology. 2009;112:56–9.
Cabala M, Gajdosz R. The role of serum amyloid A in the early diagnosis of acute coronary syndrome. Przegl Lek. 2005;62:13–6.
Mezaki T, Matsubara T, Hori T, et al. Plasma levels of soluble thrombomodulin, C-reactive protein, and serum amyloid A protein in the atherosclerotic coronary circulation. Jpn Heart J. 2003;44:601–12.
Harb TS, Zareba W, Moss AJ, et al. Association of C-reactive protein and serum amyloid A with recurrent coronary events in stable patients after healing of acute myocardial infarction. Am J Cardiol. 2002;89:216–21.
Rached F, Lhomme M, Camont L, et al. Defective functionality of small, dense HDL3 subpopulations in ST segment elevation myocardial infarction: relevance of enrichment in lysophosphatidylcholine, phosphatidic acid and serum amyloid A. Biochim Biophys Acta. 2015;1851:1254–61.
Hoffmeister A, Rothenbacher D, Khuseyinova N, et al. Plasminogen levels and risk of coronary artery disease. Am J Cardiol. 2002;90:1168–70.
Ogasawara K, Mashiba S, Wada Y, et al. A serum amyloid A and LDL complex as a new prognostic marker in stable coronary artery disease. Atherosclerosis. 2004;174:349–56.
Xie X, Ma YT, Yang YN, et al. Polymorphisms in the SAA1/2 gene are associated with carotid intima media thickness in healthy han Chinese subjects: the cardiovascular risk survey. PLoS ONE. 2010;5:e13997.
Artl A, Marsche G, Lestavel S, et al. Role of serum amyloid A during metabolism of acute-phase HDL by macrophages. Arterioscler Thromb Vasc Biol. 2000;20:763–72.
Santoso A, Kaniawati M, Bakri S, et al. Secretory phospholipase A2 is associated with the odds of acute coronary syndromes through elevation of serum amyloid-A. Protein Int J Angiol. 2013;22:49–544.
Winckers K, Cate HT, Hackeng TM. The role of tissue factor pathway inhibitor in atherosclerosis and arterial thrombosis. Blood Rev. 2013;27:119–32.
Sjöholm K, Lundgren M, Olsson M, et al. Association of serum amyloid A levels with adipocyte size and serum levels of adipokines: differences between men and women. Cytokine. 2009;48:260–6.
AlBadr A, We J, Mehta P, et al. Inflammatory biomark Il-6 predicts heart failure in women with signs and symptoms of ischemia and no obstructive coronary artery disease: findings from the Nhlbi-Sponsored Women's Ischemic Syndrome Evaluation (Wise) Study. JACC. 2016;67:1313.
Werba JP, Veglia F, Amato M, et al. Patients with a history of stable or unstable coronary heart disease have different acute phase responses to an inflammatory stimulus. Atherosclerosis. 2008;196:835–40.
Gomma AH, Hirschfield GM, Gallimore JR, et al. Preprocedural inflammatory markers do not predict restenosis after successful coronary stenting. Am Heart J. 2004;147:1071–7.
Haverkate F, Thompson G, Pyke SD, et al. Production of C-reactive protein and risk of coronary events in stable and unstable angina. European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. Lancet. 1997;349:462–6.
Zhang T, Wang Z, Xiao W. A meta-analysis of interleukin-6 -572G%3eC polymorphism and coronary heart disease susceptibility. Cardiol J. 2017;24:107–10.
Papageorgiou N, Briasoulis A, Hatzis G, et al. Coronary artery atherosclerosis in hypertensive patients: the role of fibrinogen genetic variability. Rev Esp Cardiol (Engl Ed). 2017;70:34–41.
Filep JG, Kebir D. Serum amyloid A as a marker and mediator of acute coronary syndromes. Future Cardiol. 2008;4:495–504.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (Grant no. 81570786 to K. Y. Chen; 81770295 to Y.L.).
Author information
Authors and Affiliations
Contributions
JLZ designed the study and developed the retrieval strategy. JLZ and KYC screened the literature. JLZ and SFW extracted the data from the literature. JLZ, KYC, and SFW conducted the meta-analysis and wrote the manuscript. JLZ and YL performed the revised process of paper. All authors read and approved the final draft.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they do not have anything to disclose regarding conflict of interest with respect to this manuscript.
Additional information
Responsible Editor: John Di Battista.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, J., Lu, Y., Wang, S. et al. Association between serum amyloid A levels and coronary heart disease: a systematic review and meta-analysis of 26 studies. Inflamm. Res. 69, 331–345 (2020). https://doi.org/10.1007/s00011-020-01325-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-020-01325-1