Abstract
When mimicking epileptic processes in a laboratory setting, it is important to understand the differences between experimental models of seizures and epilepsy. Because human epilepsy is defined by the appearance of multiple spontaneous recurrent seizures, the induction of a single acute seizure without recurrence does not constitute an adequate epilepsy model. Animal models of epilepsy might be useful for various tasks. They allow for the investigation of pathophysiological mechanisms of the disease, the evaluation, or the development of new antiepileptic treatments, and the study of the consequences of recurrent seizures and neurological and psychiatric comorbidities. Although clinical relevance is always an issue, the development of models of pediatric epilepsies is particularly challenging due to the existence of several key differences in the dynamics of human and rodent brain maturation. Another important consideration in modeling pediatric epilepsy is that “children are not little adults,” and therefore a mere application of models of adult epilepsies to the immature specimens is irrelevant. Herein, we review the models of pediatric epilepsy. First, we illustrate the differences between models of pediatric epilepsy and models of the adulthood consequences of a precipitating insult in early life. Next, we focus on new animal models of specific forms of epilepsies that occur in the developing brain. We conclude by emphasizing the deficiencies in the existing animal models and the need for several new models.
Similar content being viewed by others
Introduction
Epilepsy is suspected when there is a repetition of seizures. The causes and clinical spectrums of epilepsy in children are extremely wide ranging. Worldwide, it is estimated that 10.5 million children ˂15 years of age have active epilepsy and constitute approximately 25 % of the global epilepsy population [1]. Several classifications of the seizures (symptoms) and the epilepsy syndromes have been refined in time to have a common vocabulary [2–5]. The classifications provide a fundamental framework for organizing and differentiating the epilepsies. The epilepsy syndromes are distinctive disorders identifiable on the basis of the typical age onset, specific electroencephalographic (EEG) characteristics, seizure types, and often other features that when taken together permit a specific diagnosis. They also have become the focus of treatment trials and genetic, neuropsychological, and neuroimaging investigations, and have implications for treatment and prognosis. Two-thirds of children can be assigned to specific syndromes early after clinical evaluation and appropriate investigations (EEG and/or neuroimaging) [6, 7]. Of the remaining percentage, approximately 30 % will be assigned to a more specific category within 2 years [8]. Approximately 20 to 30 % of patients with epilepsy have refractory epilepsy (i.e., seizures that persist, despite accurate diagnosis and carefully monitored treatment with antiepileptic drugs) [9]. Knowledge of the pathophysiology of childhood epilepsy has considerably increased with improvement of both neuroimaging and genetic techniques. However, our understanding of the causes and the reasons why specific syndromes appear with precise age-relatedness is still very limited.
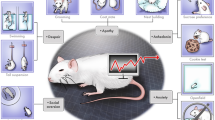
The use of animal models in experimental studies is responsible for much of our knowledge of epilepsy. These animal models can be categorized into models of seizures and models of epilepsy. Because human epilepsy is defined by the appearance of multiple spontaneous, recurrent seizures, models involving the induction of acute seizure activity alone, without subsequent chronic seizures, should be regarded as models for seizures per se, and not specifically epilepsy. Animal models of epilepsy are useful for a variety of tasks; they allow for the investigation of pathophysiological mechanisms, the evaluation and development of new antiepileptic treatment, and the study of the consequences of conditions that may be concurrent with epilepsy (cognitive consequences and/or comorbidities) [10–12].
Despite the tremendous value of animal models, the myriad differences between the human and animal brain make the decision of which paradigm to use a critical one. Moreover, when studying seizures in the developing brain, several differences between the rates of maturation are well-recognized, and making exact equivalences in developmental milestones between species is a multi-dimensional task. As a result, no single animal model is likely to faithfully reproduce every aspect of a human epilepsy syndrome.
In this review, we provide an overview of the animal models that focus on pediatric epilepsy. First we address the need for models and then discuss select models that are used to study the long-term (i.e., adult) consequences of pediatric insults. Finally, we describe the new animal models of childhood epilepsy.
The Need for Models
Given the wide diversity of epilepsy types that present at different developmental ages, certain clinical questions must be considered to identify the models that are needed. Animal models of pediatric epilepsy should permit the study of epilepsy syndromes with high incidences. In addition, there is an impetus to understand epilepsy with refractory seizures and/or cognitive impairments. Finally, despite the low incidence of some epilepsy syndromes in children (such as epileptic encephalopathies), the development of models of these low-incidence syndromes would prove valuable in furthering our understanding of refractoriness and the behavioral/cognitive consequences that present significant challenges in clinical practice. To illustrate the current need for animal models of pediatric epilepsies, Fig. 1 lists the pediatric epilepsy syndromes according to their incidences and consequences.
Graph with the main pediatric epilepsy syndromes according to their incidences and consequences. In blue, the epilepsy syndromes with available animal models. In red, the epilepsy syndromes with needed animal models. CAE = childhood absence epilepsy; IGE = idiopathic generalized epilepsies; Sd = syndrome; TSC = tuberous sclerosis complex
In 2004, a workshop was organized to address the need for pediatric epilepsy models [13]. This gathering stressed the need for models in 2 categories of epilepsy that are of particular concern, because of their intractability to treatment and association with cognitive decline. The epileptic encephalopathies are the first group; they entail age-specific seizure onset, refractoriness to medical treatment, and progressive cognitive deterioration. The second group of epilepsy identified to be in need of animal models is the refractory partial epilepsies.
Figure 1 illustrates the need for new models of pediatric epilepsy. New animal models should meet the following, previously suggested criteria [14]: 1) the animal model should exhibit electrophysiological correlates/patterns similar to those observed in the human condition; 2) the etiologies should be similar (e.g., genetic predisposition or injury); 3) the proposed animal model should be scaled to (or reflect) human age when the epilepsy syndrome is age-specific; 4) the animal model should display similar pathologies when the human condition has specific pathological changes (e.g., cortical dysplasia); 5) the condition being modeled should respond similarly to antiepileptic drugs; and 6) the behavioral characteristics (short- or long-term behavioral changes) should reflect behavioral manifestations observed in humans. We will also use these criteria in the description of various animal models that are discussed here.
Injury to the Immature Brain to Induce Epileptogenesis
The term epileptogenesis applies to a variety of progressive biochemical, anatomic, and physiological changes that lead to spontaneous recurrent seizures. Spontaneous seizures develop after a “silent” period, which may last between several days and several months [15]. Whether cell injury to the immature brain is required to induce epileptogenesis remains an active topic of debate [16, 17]. The majority of existing experimental models of epileptogenesis focus on insults in early life that precipitate epileptogenic insults and their long-term consequences. The existence of the latent period is a major challenge for modeling pediatric epileptogenesis. The underlying mechanisms leading to epilepsy within a specific window of early ontogenic development are difficult to model because laboratory rodents progress from neonates to adults in a few weeks (rats and mice are considered adults at 45–50 days) rather than many years, as is the case for humans; therefore, by the time spontaneous seizures occur, the animal has passed through several developmental stages. It should be stated that none of the models using initial injury to induce epileptogenesis can be considered as models of pediatric epilepsy because they all report the occurrence of spontaneous recurrent seizures during adulthood. However, post-precipitating insult models are important for exploring the mechanisms of early-life epileptogenesis and the development of evidence-based therapeutic strategies to prevent epileptogenesis after injuries that occur during childhood.
Different types of injury and/or prolonged seizures have been used to induce epileptogenesis with the goal of mimicking human conditions (Table 1). Hyperthermic seizures induced in postnatal day 10 or 11 (P10-P11) rat pups are used to mimic prolonged febrile seizure [18]. Hypoxic-ischemic brain insults can also be induced in rat pups to model hypoxic-ischemic encephalopathy, which is a prominent cause of mortality in neonates and morbidities, including epilepsy, in children [19]. Animal models involving hypoxia in P7 to P10 rats have been used to study both acute neonatal seizures and the subsequent development of epilepsy [20, 21]. Status epilepticus (SE) induced by pilocarpine is used in rats from P14 to adulthood to induce significant epileptogenesis and resulting spontaneous seizures [22, 23].
Hyperthermic Seizures Induced in P10 to P11 Rat Pups
Using various methods to induce hyperthermia, this model aims to mimic prolonged febrile seizures. The most studied mechanism to induce hyperthermia is the use of heated airstream on P10 to P11 rats [18]. No evidence of hippocampal neuronal loss (using Nissl stain counting methods) have been found [24], but hyperexcitability in brain slices and an increase in seizure susceptibility have been reported [25]. More recently, spontaneous recurrent seizures have been recorded using concurrent hippocampal and cortical EEG video EEG monitoring [26, 27].
Hypoxia at P7 to P10 in Rats
After unilateral carotid ligation to induce hypoxia at P7, it has been reported that 56 % of rats developed spontaneous recurrent seizures. But all rats with a cerebral infarct developed spontaneous epileptiform discharges and recurrent seizures (100 %), whereas no spontaneous epileptiform discharges or seizures were detected in the rats without infarcts. Spontaneous epileptiform discharges were initially lateralized to ipsilateral neocortex but became bilateral with time. The severity and frequency of the spontaneous behavioral and electrographic seizures progressively increased with time [20].
Using global hypoxia for 15 minutes in P10 rats, seizures are induced during the neonatal period leading to recurrent spontaneous seizures in adulthood. The latent period was shorter than previously reported in the other models (2–3 weeks). A progressive intensification of seizure activity was suggested by the increased seizure frequency and duration [21].
Status Epilepticus Induced by Pilocarpine in Rats from P14 to Adulthood
In the lithium-pilocarpine model of SE, it has been shown that a significant level of SE-induced cell injury is observed at P14. In 2- and 3-week-old pups, the cell injuries are mainly observed in CA1. At P21, the injuries to the hilus and CA3 reached an adult-like pattern, whereas amygdalar neuronal cell injuries increased progressively with age [22]. Lithium-pilocarpine SE induced at P14 results in significant epileptogenesis with spontaneous recurrent seizure in approximately 10 to 20 % of rats [22, 28]. When SE is induced at P21 or P28, the percentage of animals with spontaneous recurrent seizures is close to the rate of epileptic animals generated by the same SE model in adult rats [29]. To evaluate the role of inflammation, which is a component of febrile seizure in children [30], we recently conducted a study using a double hit injury (status epilepticus pluse systemic inflammation). We found that inflammation increased epileptogenesis when combined with SE in the immature brain [28].
Neonatal Epileptic Encephalopathies with Suppression Burst
Neonatal epileptic encephalopathies with suppression burst (SB) are a rare group of neonatal epilepsies characterized by an onset of seizures in the first months of life with SB in EEG recordings. This specific pattern is described as generalized, multifocal, high-voltage, and with spikes and sharp wave complexes alternating with periods of suppression of electrical activity. Two syndromes have been described: 1) early infantile epileptic encephalopathy (EIEE) and 2) early myoclonic encephalopathy (EME) [31]. In EIEE with SB, seizures start within the first 10 days of life. The seizure types are variable, but epileptic spasms are the most frequent type. Later, generalized tonic-clonic seizures may occur. The children become inactive and hypotonic when the seizures begin. Moreover, there is an absence of psychomotor development and the appearance of neurological symptoms. EME is also associated with early infancy onset, an SB EEG pattern, a variety of seizure types, and poor psychomotor outcome. The 2 syndromes are now classified in the group of epileptic encephalopathies. The prominent erratic myoclonia observed in EME is not present in EIEE, and spasms and tonic seizures predominate in EIEE. The etiologies are also different. Metabolic etiologies predominate in EME, whereas malformative etiologies predominate in EIEE. A family with an autosomal recessive form of EME enabled the identification of a missense mutation in the gene encoding the mitochondrial glutamate/proton “symporter” GC1 [32]. The identification of mutant GC1 as an etiology of EME also emphasizes the importance of the mitochondrial component of glutamate metabolism in normal brain function.
An interesting study has reported seizures in P5 to P7 rats that are associated with EEG abnormalities similar to those observed in suppression burst [33]. The aim of the study was to examine the consequences of dysfunction of the glutamate transport on electrographic patterns of the immature rat. Pharmacological inhibition of the glutamate transporters with DL-threo-beta-benzyloxyaspartate resulted in the occurrence of bilateral recurrent bursts, consisting of a slow deflection followed by fast spiking activity and alternating with periods in which detectable activity was absent. These paroxysmal bursts occurred at a regular rate. In about half of the animals, the bursts were associated with myoclonic startles. Moreover, long-lasting rhythmic delta–theta oscillatory activities were also recorded and could occasionally be associated with behavioral manifestations such as crawling, tonic postures of 1 or 2 limbs, freezing-like postures, and hypermotoric activity. The authors concluded that partial seizures that are best characterized by rhythmic slow oscillations in 1 territory of the brain are most likely due to poor axonal myelination.
The use of threo-beta-benzyloxyaspartate to modify glutamate transport has several advantages: threo-beta-benzyloxyaspartate is a nontransportable inhibitor and, as such, does not induce artificial transmitter release through hetero exchange and does not act as a partial agonist of glutamate receptors (these properties were demonstrated with electrophysiological recordings and binding assays) [34]. They demonstrated the role of glutamate receptor activation in the generation of the EEG pattern by modifying the frequency and duration of activation by administering the N-Methyl-D-aspartate (NMDA) antagonist ketamine or the α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) antagonist NBQX [33].
This pattern has not been previously described in other animal models of epilepsy during the neonatal period. The cortical activity is reminiscent of “suppression burst,” because the EEG pattern is characterized by the occurrence of high-amplitude bursts of spikes, slow waves alternating with almost silent periods, and the absence of normal background activity. This first description suggests that this model should be further explored. It would be interesting to know the consequences of these early changes in terms of behavior/cognition, as well as epileptogenesis.
Infantile Spasms
Infantile spasm (IS) is the most frequent epileptic syndrome in the first year of life. However, its overall incidence is relatively low. IS is characterized by its associated epileptic spasms, psychomotor regression and a specific electroencephalogram (EEG) pattern called hypsarrhythmia. IS is an age-dependent epileptic encephalopathy with various etiologies that exhibit variable courses [35]. There are many etiologies with a wide range of acquired and congenital causes that are categorized as symptomatic (cause known) or cryptogenic (no obvious brain disorder; cause unknown). Children presenting with IS and hypsarrhythmia have a high risk of developing cognitive deterioration [36]. Most of the conventional antiepileptic drugs are ineffective for IS. The epileptic spasms may respond to treatments, such as glucocorticoids, adrenocorticotropic hormone (ACTH), and vigabatrin. The main long-term effects of this epileptic syndrome are the persistence of epilepsy and the cognitive outcome representing a main cause of cognitive deterioration during infancy [36–39].
For many years, the development of an IS model appeared to be a real challenge [13]. Recently, several new infantile spasm models have been published, creating new hope for better understanding of the underlying mechanisms of IS. Six animal models can be considered appropriate (Table 2). Four of these models are chemically induced, and 2 are based on genetically modified mice. These models permit a representation of the etiological spectrum that is observed in children with IS. The models that are induced by endogenous and exogenous toxins or stress hormones represent acquired causes, whereas genetic causes are represented by Ts65Dn mice, which are a model of Down syndrome or the Aristaless-related homeobox (ARX) model.
Models of Acquired Causes of IS
There are 4 models of IS that represent the different causes of IS: 1) the corticotropin-releasing hormone (CRH) model, 2) the NMDA model, 3) the tetrodotoxin model, and 4) the multiple-hit model.
The Corticotropin-Releasing Hormone Model
This model derives from the hypothesis that the stress hormones ACTH and the glucocorticoids ameliorate infantile spasms [40]. CRH release is increased by stress. The model has been induced by intraperitoneal or intracerebroventricular administration of CRH [41]. CRH administration during the second week of life in rats caused severe seizures by inhibiting the hypothalamic–pituitary–adrenal axis. The semiology of the seizures suggests limbic origins. Acute ACTH treatment does not influence seizures induced by exogenous CRH. These observations suggest that ACTH acts to repress infantile spasms by suppressing the level of endogenous CRH [42, 43]. EEG recordings during CRH seizures show rhythmic, sharp activity [41]. These EEG recordings are closer to those observed in limbic seizures than those observed in IS in humans. However, this age-specific model is induced without any brain damage, which permits the analysis of the consequences of the spasms themselves in studies of long-term consequences. Moreover, the CRH model provides pivotal insight into the actions of ACTH and glucocorticoid in brain development and infantile spasms.
The NMDA Model
The NMDA model is induced with intraperitoneal injections of the glutamate receptor agonist NMDA in rat pups between P10 and P15 [44]. This model was originally induced with the injections administered from P12 to P18 [45]. This model is most likely a model of acute seizure with hyperflexion and tonic spasms of the entire body, but the animals return after awhile to normal behavior. The spasms occur in clusters. Ictal EEG shows generalized amplitude reduction, whereas interictal EEG may show, in some animals, large-amplitude, nonsynchronous waves. These electroclinical characteristics fit human IS, even though interictal EEG cannot represent a true hypsarrhythmia. At the same time, the rats lose their righting reflex [44]. Cognitive deficits in the form of impairments in spatial learning and memory appear in adult rats following NMDA-induced seizures in pups [46].
More recently, it has been shown that the spasms start earlier and occur in greater numbers when the rats are prenatally exposed to betamethasone or restraint stress [47, 48]. This pretreatment was chosen by the authors of these studies to mimic prenatal stress by altering the hypothalamic–pituitary–adrenal axis. Similar to the human condition, chronic pre-treatment ACTH treatment or chronic pretreatment with methylprednisolone at the time of spasms significantly reduces the number of spasms and significantly increases the latency of spasm onset. Moreover, pretreatment with vigabatrin, but not rapamycin, suppresses the spasms [48]. Significant behavioral changes occur following the start of spasms. The betamethasone/NMDA model satisfies some of the infantile spasm criteria for seizure semiology: age specificity, EEG changes, pharmacological profile, and cognitive deficits. Owing to the lack of structural brain damage or lesions in the betamethasone/NMDA model, some investigators have proposed this model as one of cryptogenic infantile spasms [49]. The NMDA model shares interesting pharmacological response properties with the suppression of epileptic spasm with ACTH, methylprednisolone, or vigabatrin [48].
The Tetrodotoxin Model
Intrahippocampal infusion of tetrodotoxin (TTX) creates recurrent brief spasm-like seizures in P10 to P12 rat pups [50, 51]. These seizures consist of short discharges of fast activity as recorded by EEG. The use of TTX to chronically suppress neural activity during specific developmental windows results in hyperexcitability.
When TTX is injected for 28 days, beginning on P10, initially there is a depression of neuronal activity, followed by EEG abnormalities some time later. Around P21, one third of TTX-treated rats developed flexor or extensor spasms that occur singly or in clusters. The ictal EEG is a generalized slow wave followed by voltage attenuation and then low-voltage fast activity. This pattern is similar to the usual ictal pattern of IS. Recently, it has been shown that high frequency EEG activity occurs throughout ictal events [52]. Interestingly, the interictal EEG pattern has high-voltage, slow waves and multi-spikes. This interictal EEG can be compared to hypsarrhythmia. These electroclinical features continue after the end of the TTX infusion. The spasms give way to prolonged seizures. The TTX model provides convincing evidence for hypsarrhythmia and electrodecrement in an animal model [53]. In this model, the occurrence of spasms is very late in terms of brain maturation. However, this model emphasizes that blocking neuronal activity of a normal brain might result in epileptic spasms. The TTX could also be an interesting tool for understanding the mechanisms by which spasms evolve into other seizure types. The behavioral consequences and efficacy of antiepileptic drugs need to be further studied in this model.
The Multiple Hit Model of IS
The multiple hit model uses severe damage to cortical and subcortical structures on the basis of the theory that IS results from abnormal interactions between cortical areas and subcortical structures, including the brain stem. Doxorubicin is injected into the cerebral ventricles, and lipopolysaccharide is administered intracerebrally in P3 rats. Doxorubicin, an anthracycline chemotherapeutic agent, is used to induce neuronal damage, whereas lipopolysaccharide, a part of bacterial walls that acts as a toll-like receptor 4 agonist, is used to induce inflammation. These initial brain injuries are followed by an intraperitoneal injection of p-chlorophenylalanine at P5 to inhibit tryptophan hydroxylase and block the synthesis of brain serotonin. Serotonin is known to reduce brain excitability. After these 3 hits, the rats begin to exhibit recurrent seizures from P7 to P12. These seizures, such as IS, have clusters of spasms associated with electroencephalographic decrement. After P11 to P12, limbic seizures with running behavior are also observed [54]. The multiple hit model should be considered a model of symptomatic IS that represents the most common etiology of IS in humans [35]. In this model, ACTH did not suppress spasms, whereas vigabatrin had a transient effect on spasms (only at P5). This model may be helpful in evaluating treatments for refractory IS [54]. More recently, new treatments have been evaluated (e.g., rapamycin suppressed spasms dose-dependently and improved visuospatial learning [55], and carisbamate also displayed acute effects on spasms [56]). These findings have helped to create new hypotheses for treatment evaluation in refractory IS.
Models of Genetic Causes of IS
The Down Syndrome Model — Ts65Dn Mice
A mouse model of Down syndrome (Ts65Dn) has been developed to study many aspects of this genetic disorder [57]. Ts65Dn mice exhibit spontaneous spike-wave discharges in EEG recordings without any seizures at baseline [58]. The spike-wave discharges are similar to those induced in normal rats exposed to GABAB receptor agonists [59]. It has also been shown that the Ts65Dn mice overexpress GABAB receptors, which prompted the suggestion that the use of GABAB receptor agonists might increase seizure susceptibility [58]. The administration of baclofen or γ-butyrolactone (the pro-drug of the GABAB agonist γ-hydroxybutyrate) to Ts65Dn mice (1 week to 2 months old) results in clusters of extensor spasms with polyspike-wave bursts and electrodecrement on EEG recording, whereas γ-butyrolactone injected into wild-type mice causes spike-wave discharges and absence seizures [59]. antiepileptic drugs used to treat infantile spasms (ACTH and vigabatrin) improve these epileptic phenomenon, suggesting this model of spasms is pharmacologically reliable [58, 60]. Assessment of the long-term consequences would be interesting. These mice can be considered a model of the genetic causes of infantile spasms because infantile spasms occur in ≤10 % of children with Down syndrome [61]. The major limitation is the absence of spontaneously or chronically occurring infantile spasms. However, the need for GABAB receptor agonist injection suggests that GABAB receptors are involved in the pathogenesis of infantile spasms, at least those associated with Down syndrome. The mechanism by which GABAB receptor alteration causes spasms needs to be further studied. Another limitation is that the induced spasms are observed in 2-month-old mice (late adolescent to adult). Epileptic spasms in humans can be observed after infancy [62, 63] but have not been reported to occur this early in Down syndrome [64].
The Aristaless-Related Homeobox Mutation Model — ARX Spasms Model
Mutations in the ARX gene (OMIM *300382) are associated with a variety of neurological syndromes, including infantile spasms [65]. The ARX gene is 1 of a family of homeobox genes encoding transcription factors required for normal nervous system development. ARX knockout mice exhibit deficient proliferation of several cell types, including GABAergic interneurons [66]. Thus, mice with conditional deletions of ARX from inhibitory interneurons of the cortex have been created. Arx knock-in in these mice reproduces the 23 alanine codons in human ISSX-ARX(GCG)10+7. The pups display twice as many spontaneous spasm-like movements as do wild-type littermates. Arx (GCG)10+7 mice have EEG abnormalities that include sharp spike-slow wave transients followed by attenuation of background activity and an increase in high-frequency background rhythmic activity. These EEG findings are not observed in the older mutants. These mice also have behavior modifications, including abnormally low anxiety and cognitive impairment. Between the ages of 3.5 and 10 weeks, Arx (GCG)10+7 mutants show spontaneous seizures characterized by versive or clonic movements that are associated with generalized attenuation of the EEG background with low-voltage fast activity and followed by generalized high frequency and high-amplitude spikes and polyspikes in different brain areas. The seizures last more than 20 seconds. The ARX spasm model seems to share critical phenotypic features with human IS. Interestingly, the persistence of seizures should allow modeling of the transition from spasms to other types of seizures [67]. There are currently no data on the effect of treatments on this model.
Despite the fact that epileptic spasms are recorded among days, most of the models of IS are induced by injection of various components. The genetic models exhibit spontaneous epileptic spasms. However, the genetic models reflect a small number of the etiologies of IS. An ideal model that recapitulates all aspects of human IS is unlikely, but increases in the number of IS models would permit multiple approaches to further understand the underlying mechanisms of this epileptic encephalopathy.
Cortical Dysplasia
Cortical dysplasia is a frequent cause of medically intractable forms of epilepsy [68]. Abnormalities in neuronal migration (when newly developed neurons fail to reach their proper destinations) result in aberrant brain structures that are often termed cortical dysplasia. Dysplastic cell clusters and/or surrounding structures (neocortex or hippocampus) are often identified as the sites in which epileptic activities are generated, and invasive surgical resections of these “lesions” have been used to control seizures [69–71]. There are several animal models of neuronal migration disorders that can be induced by chemical treatments (e.g., methylazoxymethanol acetate), prenatal irradiation, modifications of cell development genes, or cortical freeze-lesions [72].
Methylazoxymethanol Acetate
In utero exposure of rats to MAM results in reproducible brain abnormalities that include microcephaly, heterotopic cell clusters in the hippocampus and cortex, and abnormally located cell clusters in the periventricular region [73]. Abnormal connectivity between heterotopia clusters and the cortical and hippocampal regions has been shown using tract-tracing methods [74]. The focal abnormalities induced in this model are more than anatomical abnormalities; the surrounding tissue is also abnormal [75], and it has been suggested that this tissue is the initiator/driver of the epileptiform discharge [76].
MAM-induced abnormalities underlie increases in seizure susceptibility during the first periods of life [77–80] and enhance epileptogenesis using a kindling model [78].
Germano et al. [80] first reported the effect of prenatal exposure to MAM on hyperthermic seizures. They found a higher incidence of induced-hyperthermic seizures at P14 and a higher mortality rate. Later, it was shown that prenatal exposure to MAM alone results in spontaneous recurrent seizures in approximately 20 % of animals [81]. In the developing brain, a double hit injury with hyperthermic seizures and MAM results in spontaneous recurrent seizure in a higher percentage of animals [82]. When a “double-hit” combining MAM and pilocarpine is used to induce SE in adult rats, it has been established that prenatal induced cortical development results in more severe post-SE induced epilepsy. MAM pilocarpine rats showed abnormally large cortical pyramidal neurons with neurofilament over-expression, suggesting some similarities with dysplastic neurons in humans [83]. These data show that pre-existing experimental cortical malformations enhance epileptogenesis.
In Utero Irradiation
The use of in utero radiation on postnatal brain structures and its behavioral consequences are dependent on both the timing and the dose of radiation [84–86]. Fetal irradiation can produce a wide range of structural defects, including microcephaly, diffuse cortical dysplasia, neuronal heterotopias, and ectopic pyramidal cells in the hippocampus. Brain dysplasias produced by irradiation with gamma rays at various stages of prenatal development cause different postnatal susceptibility to seizures [79, 87]. This model produces multiple brain abnormalities and seems to share similar properties regarding seizure susceptibility and epileptogenesis with the MAM model.
Focally Induced Lesions
Because MAM produces widespread lesions, some authors have developed a model using unique focal lesions. Focal microgyric lesions can be induced in P1 neonatal rats using a cylindrical 2-mm diameter copper probe that is cooled in liquid nitrogen. The cooled cylinder is brought into contact with the skull overlying the right frontoparietal cortex for 10 seconds (2 mm Anterior-posterior (AP), 2 mm lateral). Freeze lesions are known to result in anatomical and functional changes that lead to cortical hyperexcitability. These changes have been reported to include increased density of thalamic projections to the paramicrogyral cortex [88] and a loss of inhibitory interneurons within the microgyrus [89]. These lesions are also responsible for an increase of NMDA receptor density in the transition zone between the microgyrus and the paramicrogyral cortex and a diffuse decrease in GABA receptor density [90–92].
The cortical dysplasias created by focally induced lesions are responsible for shorter latencies and lower thresholds to seizure in response to hyperthermic seizure model. The electrographic seizure activity lasted longer than that in control groups [72]. The same group examined the effects of focal lesions (induced with the same methods) in combination with hyperthermic seizures induced by a hair dryer. A 20-minute hyperthermic seizure was responsible for limbic seizures and memory deficits during adulthood in 86 % of the animals [93]. The mechanisms by which focal lesions lead to significant temporal lobe epileptogenesis are currently unknown [93]. Once again, this model of focal lesions has allowed the clear establishment of the role of such lesions in epileptogenesis. However, there are currently no spontaneous seizures at an early stage that would permit defining this model as a pediatric epilepsy model.
Although these models have enabled further understanding of the role and underlying mechanisms of cortical dysplasia in seizure susceptibility/epileptogenesis, they have not resulted in spontaneous seizures before the animals become adults. However, in the majority of patients with focal cortical dysplasia and epilepsy, epilepsy began in the first 5 years of life [94].
Tuberous Sclerosis Complex
Tuberous sclerosis complex (TSC) is an autosomal dominant multisystem disorder characterized by hamartomas in multiple organ systems, including the brain, skin, heart, kidneys, and lung. Central nervous system manifestations include infantile spasms, epilepsy, learning difficulties, and behavioral problems. TSC affects approximately 1 in 7500 individuals worldwide. TSC occurs when inactivating mutations occur in 1 of 2 genes: TSC1 (OMIM #191100) or TSC2 (OMIM #613254). TSC1 codes for the hamartin protein and TSC2 codes for tuberin. Hamartin and tuberin together form a guanosine triphosphatase (GTPase) activating protein complex that inhibits rheb, the GTPase that activates the mammalian Target of Rapamycin (mTOR) [95, 96]. Mutations to either TSC1 or TSC2 disrupt the function of the complex, which explains why mutations to either gene cause the same disease. The mTOR pathway provides an intersection for an intricate network of protein cascades that respond to cellular nutrition, energy levels, and growth-factor stimulation [97]. Because of the pathogenesis of TSC, mTOR inhibitors are interesting drugs for the treatment of TSC.
The Eker rat is the first animal model of TSC. The Eker rat was initially reported to have autosomic dominant renal adenoma and adenocarcinoma [98, 99] (Table 3). Later, the pathogenesis in this strain was linked to a spontaneous inactivating mutation of TSC2 [100]. Typical neuropathological hallmarks of tuberous sclerosis have also been reported with subependymal and subcortical hamartomas as the most prevalent (65 % of the TSC2 mutated rats). No cortical tubers were detected. Meningiomas and pituitary adenomas were also observed in a significant number of animals [101]. Brain abnormalities in the Eker rats increased after the use of irradiation as a second hit. Moreover, a trend for shorter latencies to flurothyl induced-seizures suggests an increase in seizure susceptibility [102]. Although these lesions have some resemblance to the brain lesions occurring in TSC patients, no correlation with a significant clinical phenotype has been reported.
Initial attempts to recapitulate the human TSC phenotype in mice used conventional knockout Tsc1 or Tsc2 mice. Mice homozygous for the loss of Tsc1 or Tsc2 die in mid-embryogenesis of apparent cardiac malformations and liver hypoplasia [103–105], whereas heterozygous animals are viable and develop renal and liver tumors. These mice do not exhibit a clear phenotype of TSC central nervous system involvement, except that altered ultrasonic vocalizations that suggest social abnormalities have been reported in Tsc2+/− mice [106]. In the central nervous system of Tsc2+/− and Tsc1+/− mice, the number of astrocytes is increased, which suggests that hamartin and tuberin are important astrocyte growth regulators [107]. These findings, and the frequent development of astrocytic tumors in patients with TSC, highlight the importance of astrocytes in the involvement of TSCs with the brain. Subsequently, conditional knockout mice with inactive TSC genes in astrocytes have been studied.
The TSC1GFAP conditional knockout mice initially appear to have normal brains. With age, the number of GFAP-positive cells increases along with ectopic neurons within the hippocampus. These mice exhibit seizures by 1 to 2 months, and die by age 4 to 5 months [108]. Pathologically, the brains of these mice exhibit an increased number of astrocytes and neuronal disorganization within the hippocampus. There is no evidence of focal abnormalities resembling tubers. Alterations in glutamate homeostasis secondary to dysfunctional astrocytes have been identified [109]. These findings suggest that induced molecular abnormalities are sufficient to cause seizures independently of the existence of tubers. The use of rapamycin in the TSC1GFAP CKO inhibits the activation of the mTOR pathway, resulting in the prevention of histological abnormalities (astrogliosis, increased brain size, and neuronal disorganization) and prevention of the occurrence of epilepsy when rapamycin treatment is given early (P14). When rapamycin was given after the start of the first seizures (6 weeks), the seizures were suppressed and the survival rates were increased [110].
Similar to TSC1GFAP CKO mice, TSC2GFAP CKO mice exhibit epilepsy, premature death, progressive megalencephaly, diffuse glial proliferation, dispersion of hippocampal pyramidal cells, and decreased astrocytic glutamate transporter expression. However, TSC2GFAP CKO mice have an earlier onset (3 weeks in TSC2GFAP CKO vs 4 weeks in TSC1GFAPCKO) and higher frequency of seizures (30–35 Sz/48 h at 7 weeks in TSC2GFAP CKO vs less than 10Sz/48 h at 7 weeks in TSC1GFAPCKO), and significantly more severe histological abnormalities. The differences between these 2 transgenic mice seem to be correlated with higher levels of mTOR activation in TSC2GFAP CKO mice. These findings can be partially reversed by rapamycin [111].
Knockout mice involving inactivation of TSC1 in neurons (TSC1synapsinCKO mice) have also been generated. TSC1synapsinCKO mice exhibit neuronal hyperexcitability and spontaneous seizures [112, 113]. The TSC1synapsinCKO mice have several neurological abnormalities, such as enlarged and/or dysplastic cortical and hippocampal neurons. Some neurons are ectopic in multiple sites in the cortex and hippocampus. This model replicates several neuropathological features of human TSC brain lesions [113].
These models allow multiple approaches to understand the underlying mechanisms leading to the clinical phenotypes of TSC. They also permit the study of the molecular pathways and preclinical evaluation of mTOR inhibitors.
Rapid Kindling: A Model of Epileptogenesis in the Developing Brain
As previously mentioned, the majority of existing experimental pediatric models of temporal lobe epilepsy focus on early life insults precipitating epileptogenesis and their long-term consequences (i.e., spontaneous recurrent seizures occurring during adulthood). The time between the insult and the appearance of spontaneous seizures is a major challenge for modeling pediatric epileptogenesis; indeed, seizures typically begin to occur after the animals are already adults, because the speed of rodent brain maturation outpaces the evolution of epilepsy. The kindling model affords a reproduction of, and a means to examine, epileptogenesis, despite the fact that kindled animals do not develop spontaneous seizures. Although post-precipitating insult models are hardly amenable for studying epileptogenesis in the developing brain, the use of a kindling model in the developing brain is possible.
The kindling phenomenon consists of the occurrence and progressive development of secondary generalized complex partial seizures in response to repetitive, initially subconvulsive electrical stimulations of limbic structures [114]. Moshe [115] and Moshe and Albala [116] were the first to show that immature rats can be kindled and that the effects of kindling are life-long. In 1985, Eric Lothman introduced a model of epileptogenesis that was based on the kindling phenomenon [117]. Under conditions of conventional kindling, the epileptic state is generally achieved within 1 to 2 weeks. However, by manipulating the parameters of the electrical stimuli applied to the ventral hippocampus of adult rats, Lothman et al. [117] were able to compress the progression to the kindled state to several hours. The feasibility of the model in the immature rat was confirmed by Michelson and Lothman [118], who provided a detailed description of both behavioral and electrographic hallmarks of rapid kindling in immature rats at several ages, including postnatal days 7 (neonatal), 14 (post-neonatal), 21 (pre-adolescent), and 28 (adolescent). This finding created a new opportunity for pediatric epilepsy research; indeed, using the rapid kindling model, epileptogenesis could now be reproduced within a very narrow and specific ontogenic window of interest, thus creating a system usable both for basic research and preclinical development of antiepileptic drugs tailored to specific ages. The latter aspect is particularly important, considering that the control of neuronal excitability and, hence, conceivable mechanisms of epileptogenesis are different between the immature and the adult brain, and evolve as a function of brain maturation. Furthermore, rapid kindling protocols can be used to discern between antiepileptogenic (i.e., interfering with the seizure progression) and antiictogenic (i.e., attenuating the established kindling seizures) effects of candidate antiepileptic drugs [119]. The usefulness of rapid kindling in studying pediatric epileptogenesis is highlighted by experiments involving the modulators of the Na+-K+-2Cl- co-transporter (NKCC1) and the KCNQ2/3 channels.
The Na+-K+-2Cl- Co-Transporter (NKCC1) and the Effects of Bumetanide
In the adult brain, the inhibitory effects of GABA are due to the GABA-A receptor-mediated Cl- influx, which is determined by the Cl- extruding K+-Cl- co-transporter (KCC2) [120]. In contrast, during the very early stages of development (prenatal-early neonatal), Cl- flow is regulated by the inward NKCC1, which increases concentrations of intracellular Cl- [121]. As a result, during early stages of development, the GABA-A receptor-mediated opening of Cl- channels leads to an outward Cl- flow and, thus, to excitation [122]. One of the presumed consequences of GABA acting as an excitatory neurotransmitter early in life is the ineffectiveness of GABAergic antiepileptic drugs [122, 123] on the one hand, and the antiepileptic effects of NKCC1 blockers on the other hand. Indeed, the NKCC1 blocker bumetanide exerted acute anticonvulsant effects in immature animals [123]. Under conditions of rapid kindling applied to immature animals across different ages, bumetanide exerted potent antiepileptogenic effect in all but few neonatal rats, yet it was completely ineffective in pre-adolescent subjects. During the neonatal-to-pre-adolescent transition, bumetanide suppressed kindling progression in approximately one half of animals; this result apparently reflected the completion of the ontogenic shift from the NKCC1 to KCC2 regulation in some animals [124].
KCNQ2/3 Channels and Effects of Retigabine
KCNQ2/3 (also known as KV7.2/7.3) are potassium channels that mediate M-type K+ currents and play important roles in the regulation of neuronal excitability [125, 126]. Mutations in the genes encoding KNCQ2/3 have been associated with the benign familial neonatal seizures, which rescind during the first month of life [127]. Qiu et al. [128] established that K+ M-current plays critical role in regulating the transition from interictal to ictal bursts in the 0 Mg2+ seizure model in vitro and that this mechanism is particularly important in immature neurons. Retigabine is an antiepileptic drug that exerts anticonvulsant effects through the opening of KCNQ2/3 channels [129]. Comparison of the antiepileptogenic and anticonvulsant effects of retigabine in immature rats subjected to rapid kindling revealed that while the compound was effective across all 3 ages, there was an age-dependent decline in its antiepileptogenic efficacy from post-neonatal to adolescences [130].
The previously described data emphasize the usefulness of the rapid kindling model in evaluating the effectiveness of evidence-based therapeutic interventions in the immature epileptic brain. Key advantages of rapid kindling include the ability to study the epileptic process (as opposed to single acute seizures) during the narrow ontogenic window of interest (as opposed to long-term outcomes of precipitating insults). At the same time, the limitations of the model should be acknowledged and understood when planning preclinical trial studies or examining mechanisms of pediatric epilepsy and epileptogenesis. The most obvious limitation is that rapid kindling is contingent primarily on neuronal plasticity, not neurodegeneration. Therefore, it is suitable neither for studying mechanisms of epilepsy-induced cell death nor for the development of neuroprotective therapeutic interventions. Another serious limitation of the model is that, unlike post-precipitating insult models [131] and conventional kindling (Sutula, 1990), the epileptic state created by repetitive stimulation is not life-long, but it diminishes and disappears within several days after the procedure [132]. Finally, the examination of the anti-epileptogenic effects of candidate therapeutic interventions requires their administration prior to the commencement of the kindling procedure and, thus, limits their therapeutic relevance; this limitation does not apply to studying antiictogenic therapies.
Models of Dravet Syndrome
Dravet syndrome (DS) (OMIM 607208), or severe myoclonic epilepsy, was described by Charlotte Dravet in 1978. This syndrome is characterized by febrile and afebrile, generalized and unilateral clonic or tonic-clonic seizures that occur in the first year of life in an otherwise normal infant. Later, myoclonus, atypical absences, and partial seizures are observed. Developmental delay becomes apparent within the second year of life. DS is a refractory epilepsy syndrome [133, 134]. The onset of seizures is characterized by febrile partial status epilepticus occurring before the age of 1. This first seizure is often considered a febrile seizure, but shortly thereafter, both febrile seizures and seizures without fever occur, leading to diagnosis. SCN1A mutations have been identified as a cause of DS. SCN1A encodes the α-subunit of the Nav1.1 channel. Voltage-gated Na + channels are complexes of an α subunit containing the voltage sensor and ion conducting pore, in association with 1 or 2 β subunits (β1-β4) [135]. Voltage-gated sodium channels (NaV) are critical for initiation of action potentials. Eighty percent of DS patient mutations arise de novo in affected individuals. Approximately 50 % of these mutations result in truncated proteins, which demonstrates haploinsufficiency for SCN1A, and several of the missense mutations in patients with severe myoclonic epilepsy in infancy also appear to cause loss of function [136].
A first animal model of DS has been generated in mice through a targeted deletion of a major exon in the SCN1A gene [137]. Homozygous null Scn1a−/− mice developed ataxia and died around P15, whereas heterozygous Scn1a1/– mice had hyperthermic-induced seizures and spontaneous seizures [137]. A second mouse model has been generated through knock-in of a stop codon into the SCN1A gene (R1407X, in exon 21) [138]. Both models exhibit symptoms that are observed in DS patients (e.g., spontaneous seizure and hyperthermia-induced seizure and ataxia). The appearance of seizures is related to brain maturation in a way that can be extrapolated to humans. In the first model, hyperthermic seizures begin to be observed at P20-P22. Myoclonic seizures followed by generalized seizures are induced by hyperthermia at P20 and later. Spontaneous seizures are also observed in mice older than P32. The interictal recordings permit further illustration of these developmental changes in the seizure susceptibility. Most of the P20-P22 mice have interictal epileptic activity with elevated body temperature, whereas interictal activity was observed at normal temperature in most of the P30-P46 mice [137]. In the second model, the authors reported that homozygous knock-in (Scn1aRX/RX) pups developed recurrent spontaneous seizures at P12. The homozygous pups have tonic-clonic and clonic seizures at P12-P16 that last for 1 to 3 minutes with a 1- to 4-h interval between seizure attacks. They also exhibit rhythmic jerking movements. Furthermore, at p10, Scn1aRX/RX pups developed abnormal and unstable gait. The mean lifetime of the homozygous mice was approximately 16 days. The authors suggested that the movement and gait were responsible for malnutrition that leads to death. In the Scn1aRX/- pups, the seizures started in the third postnatal week. However, some pups exhibited recurrent spontaneous seizures after P18. After P18, sporadic sudden death was also observed in many Scn1aRX/- mice. In this case, the authors did not report any relationship with malnutrition [138]. This hypothesis should be further explored because it might be an interesting model to study Sudden unexpected death in epilepsy (SUDEP) occurring in DS [139].
It is initially unclear why haploinsufficiency of a sodium channel critical for initiation of action potentials should cause seizures. It has been shown that the voltage-dependent activation or inactivation of sodium channels is unchanged [140]. However, the sodium current density in inhibitory interneurons in the hippocampus of NaV1.1 (+/−) and NaV1.1 (−/−) mice leads to a loss of sustained high-frequency firing of action potentials in hippocampal and cortical interneurons [138, 140]. These abnormalities lead to hyperexcitability, which might explain epilepsy in patients with Severe myoclonic epilepsy of infancy (SMEI). Moreover, ataxia observed in these mice may also be due to GABAergic cell-specific loss of sodium current. Recordings of cerebellar Purkinje neurons from mutant mice showed a reduction of sodium currents without any change in the kinetics or voltage dependence of channel activation or inactivation. These changes were responsible for a reduction of the firing rates [141].
As much of our current knowledge of the pathophysiology of epilepsy is derived from the use of animal models; the models can also be helpful in pharmacological investigations. Investigations of antiepileptic drugs could be performed with hyperthermia-induced seizures, as well as spontaneous seizures. For example, it has recently been shown that a ketogenic diet (KD) increases the latency to flurothyl-induced seizure [142]. This study explored the mechanisms of KD using 2 mice models with SCN1A mutations (Dravet syndrome and GEFS+). However, this study might suggest that the mouse model of DS exhibits similar treatment responses to those observed in humans. To date, the efficacy of the KD in DS patients has been examined in several clinical studies [143–145]. These small clinical studies strongly suggest that KD is effective in patients with DS. Further studies are needed to address whether the animal models of DS can predict pharmacological responses, as has been shown in the Genetic Absence Epilepsy Rat from Strasbourg (GAERS) model [146]. A first step to further explore this hypothesis would be to study stiripentol and topiramate, and evaluate their effects on both types of seizures. It would also be interesting to study lamotrigine to identify whether this model may recapitulate the worsening effect observed in humans [147]. The use of the DS model with a deletion of SCN1A is interesting for such a translational approach because more than 300 mutations have been described among patients with DS [136]. Regarding the study of new treatment strategies, the animal model of DS generated with a stop codon could be an interesting tool; it would permit exploration of treatments for the suppression of nonsense mutations. Genetic and biochemical studies have demonstrated that aminoglycoside antibiotics bind a specific site in ribosomal RNA and disturb codon-anticodon recognition at the aminoacyl-tRNA (Transfer RNA) acceptor site. As a result, the ribosome introduces missense mutations and translates through termination codons in bacteria, as well as eukaryotic cells. Aminoglycoside antibiotics are able to disrupt translational fidelity in both species. There are now data showing that the growth of mammalian cells in the presence of an aminoglycoside antibiotic can suppress nonsense mutations [148]. In vitro and in vivo studies have suggested that this strategy may be relevant for human diseases. Suppression of a nonsense mutation in the cystic fibrosis transmembrane conductance regulator gene by growth in gentamicin increased cystic fibrosis transmembrane conductance regulator expression by 10 to 20 % compared to control cells and restored cAMP-activated chloride transport [149, 150]. In a mouse model of Duchenne muscular dystrophy, gentamicin was used to disrupt translational fidelity to phenotypically correct a nonsense mutation [151]. This type of treatment might be used only with mouse models that use a codon stop.
Conclusion
The need for pediatric epilepsy models has been stressed for many years [13]. Ideal models recapitulating all aspects of each pediatric epilepsy syndrome are not to be expected. However, increasing the number of animal models would enable approaches for the various aspects of each syndrome. The models of infantile spasms are a good example. Studies using several models would permit evaluation of the effects of treatment in models mimicking various etiologies.
There are still epilepsy syndromes without any relevant model (e.g., rolandic epilepsy, juvenile myoclonic epilepsy, Lennox-Gastaut syndrome, and Hemiconvulsion-Hemiplegia-Epilepsy). An improvement of our understanding of the various pediatric epilepsy syndromes through more cellular and molecular data using genetic, human tissue, imaging investigations is required to develop new animal models of pediatric epilepsy. Moreover, a better understanding of the relationship between brain development and epilepsy is also a necessity. Finally, we need to improve our knowledge regarding the presence of therapeutic targets in both laboratory rodent and human brains across development to decrease the gap between preclinical data and successful clinical trials.
References
Guerrini R. Epilepsy in children. Lancet 2006;367:499–524.
Berg AT, Berkovic SF, Brodie MJ, al. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia 2010;51:676–685.
Fisher RS, van Emde BW, Blume W, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 2005;46:470–472.
ILAE. Proposal for revised clinical and electroencephalographic classification of epileptic seizures. Epilepsia 1981;22:489–501.
ILAE. Proposal for revised classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia 1989;30:389–399.
Berg AT, Shinnar S, Levy SR, Testa FM. Newly diagnosed epilepsy in children: presentation at diagnosis. Epilepsia 1999;40:445–452.
King M, Newton M, Jackson G, et al. Epileptology of the first-seizure presentation: a clinical, electroencephalographic, and magnetic resonnance imaging study of 300 consecutive patients. Lancet 1998;352:1007–1011.
Berg AT, Shinnar S, Levy SR, Testa FM, Smith-Rapaport S, Beckerman B. How well can epilepsy syndromes be identified at diagnosis? A reassessment 2 years after initial diagnosis. Epilepsia 2000;41:1269–1275.
Picot MC, Baldy-Moulinier M, Daures JP, Dujols P, Crespel A. The prevalence of epilepsy and pharmacoresistant epilepsy in adults: A population-based study in a Western European country. Epilepsia 2008;49:1230–1238.
Stafstrom CE, Sutula TP. Models of epilepsy in the developing and adult brain: implications for neuroprotection. Epilepsy Behav 2005;7(suppl 3):S18-S24.
Jensen FE. Pediatric epilepsy models. Epilepsy Res 2006;68:28–31.
Engel J, Schwartzkroin PA. What should be modeled? In: Pitkanen A, Schwartzkroin PA, Moshe SL, eds. Models of seizures and epilepsy. Amsterdam: Elsevier, 2006:1–14.
Stafstrom CE, Moshe SL, Swann JW, Nehlig A, Jacobs MP, Schwartzkroin PA. Models of pediatric epilepsies: startegies and opportunities. Epilepsia 2006;47:1407–1414.
Sarkisian MR. Overview of the current animal models for human seizure and epileptic disorders. Epilepsy Behav 2001;2:201–216.
Pitkanen A, Kharatishvili I, Karhunen H, et al. Epileptogenesis in experimental models. Epilepsia 2007;48(suppl 2):13–20.
Baram TZ, Jensen FE, Brooks-Kayal A. Does acquired epileptogenesis in the immature brain require neuronal death. Epilepsy Curr 2011;11:21–26.
Dudek FE, Ekstrand JJ, Staley KJ. Is neuronal death necessary for acquired epileptogenesis in the immature brain? Epilepsy Curr 2010;10:95–99.
Dubé C, Baram TZ. Complex febrile seizure-An experimental model in immature rodents. In: Pitkanen A, Schwartzkroin PA, Moshe SL, eds. Models of seizures and epilepsy. Oxford, UK: Elsevier, 2006:333–340.
Wallace SJ. Epilepsy in cerebral palsy. Dev Med Child Neurol 2001;43:713–717.
Kadam SD, White AM, Staley KJ, Dudek FE. Continuous electroencephalographic monitoring with radio-telemetry in a rat model of perinatal hypoxia-ischemia reveals progressive post-stroke epilepsy. J Neurosci 2010;30:404–415.
Rakhade SN, Klein PM, Huynh T, et al. Development of later life spontaneous seizures in a rodent model of hypoxia-induced neonatal seizures. Epilepsia 2011;52:753–765.
Sankar R, Shin DH, Liu H, Mazarati A, Pereira de Vasconcelos, Wasterlain CG. Patterns of status epilepticus-induced neuronal injury during development and long-term consequences. J Neurosci 1998;18:8382–8393.
Raol YS, Budreck EC, Brooks-Kayal AR. Epilepsy after early-life seizures can be independent of hippocampal injury. Ann Neurol 2003;53:503–511.
Toth Z, Yan XX, Haftoglou S, Ribak CE, Baram TZ. Seizure-induced neuronal injury: vulnerability to febrile seizures in an immature rat model. J Neurosci 1998;18:4285–4294.
Bender RA, Dube C, Gonzalez-Vega R, Mina EW, Baram TZ. Mossy fiber plasticity and enhanced hippocampal excitability, without hippocampal cell loss or altered neurogenesis, in an animal model of prolonged febrile seizures. Hippocampus 2003;13:399–412.
Dubé C, Richichi C, Bender RA, Chung G, Litt B, Baram TZ. Temporal lobe epilepsy after experimental prolonged febrile seizures: prospective analysis. Brain 2006;129:911–922.
Dubé C, Ravizza T, Hamamura M, Qinqin Z, Keebaugh A, Fok K et al. Epileptogenesis provked by prolonged exêrimental febrile seizures: mechanisms and biomarkers. J Neurosci 2010;30:7484–7494.
Auvin S, Mazarati A, Shin D, Sankar R. Inflammation enhances epileptogenesis in the developing rat brain. Neurobiol Dis 2010;40:303–310.
Auvin S, Catteau B, Ganga-Zandzou PS, Ythier H. Atypical varicella with palm and sole involvement. Int J Dermatol 2002;41:903–905.
Auvin S, Vallee L. [Febrile seizures: current understanding of pathophysiological mechanisms]. Arch Pediatr 2009;16:450–456.
Ohtahara S, Yamatogi Y. Epileptic encephalopathies in early infancy with suppression-burst. J Clin Neurophysiol 2003;20:398–407.
Molinari F, Raas-Rothschild A, Rio M, et al. Impaired mitochondrial glutamate transport in autosomal recessive neonatal myoclonic epilepsy. Am J Hum Genet 2005;76:334–339.
Milh M, Becq H, Villeneuve N, Ben-Ari Y, Aniksztejn L. Inhibition of glutamate transporters results in a "suppression-burst" pattern and partial seizures in the newborn rat. Epilepsia 2007;48:169–174.
Shimamoto K, Lebrun B, Yasuda-Kamatani Y, et al. DL-threo-beta-benzyloxyaspartate, a potent blocker of excitatory amino acid transporters. Mol Pharmacol 1998;53:195–201.
Watanabe K. West syndrome: etiological and pronosctic aspects. Brain Dev 1998;20:1–8.
Riikonen R. Infantile spasms: therapy and outcome. J Child Neurol 2004;19:401–404.
Rantala H, Putkonen T. Occurrence, outcome, and prognostic factors of infantile spasms and Lennox-Gastaut syndrome. Epilepsia 1999;40:286–289.
Riikonen R. Long-term otucome of West syndrome: a study of adults with a history of infantile spasms. Epilepsia 1996;37:367–372.
Koo B, Hwang PA, Logan WJ. Infantile spasms: outcome and prognostic factors of cryptogenic and symptomatic groups. Neurology 1993;43:2322–2327.
Brunson KL, Eghbal-Ahmadi M, Baram TZ. How do the many etiologies of West syndrome lead to excitability and seizures? The corticotropin releasing hormone excess hypothesis. Brain Dev 2001;23:533–538.
Baram TZ, Schultz L. Corticotropin-releasing hormone is a rapid and potent convulsant in the infant rat. Brain Res Dev Brain Res 1991;61:97–101.
Baram TZ, Schultz L. ACTH does not control neonatal seizures induced by administration of exogenous corticotropin-releasing hormone. Epilepsia 1995;36:174–178.
Brunson KL, Khan N, Eghbal-Ahmadi M, Baram TZ. Corticotropin (ACTH) acts directly on amygdala neurons to down-regulate corticotropin-releasing hormone gene expression. Ann Neurol 2001;49:304–312.
Kabova R, Liptakova S, Slamberova R, Pometlova M, Velisek L. Age-specific N-methyl-D-aspartate-induced seizures: perspectives for the West syndrome model. Epilepsia 1999;40:1357–1369.
Mares P, Velisek L. N-methyl-D-aspartate (NMDA)-induced seizures in developing rats. Brain Res Dev Brain Res 1992;65:185–189.
Stafstrom CE, Sasaki-Adams DM. NMDA-induced seizures in developing rats cause long-term learning impairment and increased seizure susceptibility. Epilepsy Res 2003;53:129–137.
Yum MS, Chachua T, Veliskova J, Velisek L. Prenatal stress promotes development of spasms in infant rats. Epilepsia 2012;53:e46-e49.
Chachua T, Yum MS, Veliskova J, Velisek L. Validation of the rat model of cryptogenic infantile spasms. Epilepsia 2011;52:1666–1677.
Velisek L, Jehle K, Asche S, Veliskova J. Model of infantile spasms induced by N-methyl-D-aspartic acid in prenatally impaired brain. Ann Neurol 2007;61:109–119.
Galvan CD, Hrachovy RA, Smith KL, Swann JW. Blockade of neuronal activity during hippocampal development produces a chronic focal epilepsy in the rat. J Neurosci 2000;20:2904–2916.
Galvan CD, Wenzel JH, Dineley KT, et al. Postsynaptic contributions to hippocampal network hyperexcitability induced by chronic activity blockade in vivo. Eur J Neurosci 2003;18:1861–1872.
Frost JD Jr., Lee CL, Hrachovy RA, Swann JW. High frequency EEG activity associated with ictal events in an animal model of infantile spasms. Epilepsia 2011;52:53–62.
Lee CL, Frost JD Jr., Swann JW, Hrachovy RA. A new animal model of infantile spasms with unprovoked persistent seizures. Epilepsia 2008;49:298–307.
Scantlebury MH, Galanopoulou AS, Chudomelova L, Raffo E, Betancourth D, Moshe SL. A model of symptomatic infantile spasms syndrome. Neurobiol Dis 2010;37:604–612.
Raffo E, Coppola A, Ono T, Briggs SW, Galanopoulou AS. A pulse rapamycin therapy for infantile spasms and associated cognitive decline. Neurobiol Dis 2011;43:322–329.
Ono T, Moshe SL, Galanopoulou AS. Carisbamate acutely suppresses spasms in a rat model of symptomatic infantile spasms. Epilepsia 2011;52:1678–1684.
Galdzicki Z, Siarey RJ. Understanding mental retardation in Down's syndrome using trisomy 16 mouse models. Genes Brain Behav 2003;2:167–178.
Cortez MA, Shen L, Wu Y, et al. Infantile spasms and Down syndrome: a new animal model. Pediatr Res 2009;65:499–503.
Snead OC, III, Depaulis A, Vergnes M, Marescaux C. Absence epilepsy: advances in experimental animal models. Adv Neurol 1999;79:253–278.
Cortez MA, Sadeghnia HR, Aleem IS, et al. A new animal model of infantile spasms: ACTH and antiepileptic drug profiles. 2007;A211 Pediatr Res. 2009 May;65(5):499–503.
Stafstrom CE, Konkol RJ. Infantile spasms in children with Down syndrome. Dev Med Child Neurol 1994;36:576–585.
Auvin S, Lamblin MD, Pandit F, Vallee L, Bouvet-Mourcia A. Infantile epileptic encephalopathy with late-onset spasms: report of 19 patients. Epilepsia 2010;51:1290–1296.
Eisermann MM, Ville D, Soufflet C, O et al. Cryptogenic late-onset epileptic spasms: an overlooked syndrome of early childhood? Epilepsia 2006;47:1035–1042.
Eisermann MM, DeLaRaillere A, Dellatolas G, et al. Infantile spasms in Down syndrome — effects of delayed anticonvulsive treatment. Epilepsy Res 2003;55:21–27.
Hirose S, Mitsudome A. X-linked mental retardation and epilepsy: pathogenetic significance of ARX mutations. Brain Dev 2003;25:161–165.
Kitamura K, Yanazawa M, Sugiyama N, et al. Mutation of ARX causes abnormal development of forebrain and testes in mice and X-linked lissencephaly with abnormal genitalia in humans. Nat Genet 2002;32:359–369.
Price MG, Yoo JW, Burgess DL, et al. A triplet repeat expansion genetic mouse model of infantile spasms syndrome, Arx(GCG)10+7, with interneuronopathy, spasms in infancy, persistent seizures, and adult cognitive and behavioral impairment. J Neurosci 2009;29:8752–8763.
Blumcke I, Thom M, Aronica E, et al. The clinicopathologic spectrum of focal cortical dysplasias: a consensus classification proposed by an ad hoc Task Force of the ILAE Diagnostic Methods Commission. Epilepsia 2011;52:158–174.
Hirabayashi S, Binnie CD, Janota I, Polkey CE. Surgical treatment of epilepsy due to cortical dysplasia: clinical and EEG findings. J Neurol Neurosurg Psychiatry 1993;56:765–770.
Francione S, Vigliano P, Tassi L, et al. Surgery for drug resistant partial epilepsy in children with focal cortical dysplasia: anatomical-clinical correlations and neurophysiological data in 10 patients. J Neurol Neurosurg Psychiatry 2003;74:1493–1501.
Russo GL, Tassi L, Cossu M, et al. Focal cortical resection in malformations of cortical development. Epileptic Disord 2003;5(suppl 2):S115-S123.
Scantlebury MH, Ouellet PL, Psarropoulou C, Carmant L. Freeze lesion-induced focal cortical dysplasia predisposes to atypical hyperthermic seizures in the immature rat. Epilepsia 2004;45:592–600.
Baraban SC, Wenzel HJ, Hochman DW, Schwartzkroin PA. Characterization of heterotopic cell clusters in the hippocampus of rats exposed to methylazoxymethanol in utero. Epilepsy Res 2000;39:87–102.
Colacitti C, Sancini G, Franceschetti S, et al. Altered connections between neocortical and heterotopic areas in methylazoxymethanol-treated rat. Epilepsy Res 1998;32:49–62.
Castro PA, Cooper EC, Lowenstein DH, Baraban SC. Hippocampal heterotopia lack functional Kv4.2 potassium channels in the methylazoxymethanol model of cortical malformations and epilepsy. J Neurosci 2001;21:6626–6634.
Tschuluun N, Jurgen WH, Doisy ET, Schwartzkroin PA. Initiation of epileptiform activity in a rat model of periventricular nodular heterotopia. Epilepsia 2011;52:2304–2314.
de Feo MR, Mecarelli O, Ricci GF. Seizure susceptibility in immature rats with micrencephaly induced by prenatal exposure to methylazoxymethanol acetate. Pharmacol Res 1995;31:109–114.
Chevassus-au-Louis N, Ben-Ari Y, Vergnes M. Decreased seizure threshold and more rapid rate of kindling in rats with cortical malformation induced by prenatal treatment with methylazoxymethanol. Brain Res 1998;812:252–255.
Setkowicz Z, Janicka D, Kowalczyk A, Turlej A, Janeczko K. Congenital brain dysplasias of different genesis can differently affect susceptibility to pilocarpine- or kainic acid-induced seizures in the rat. Epilepsy Res 2005;67:123–131.
Germano IM, Zhang YF, Sperber EF, Moshe SL. Neuronal migration disorders increase susceptibility to hyperthermia-induced seizures in developing rats. Epilepsia 1996;37:902–910.
Harrington EP, Moddel G, Najm IM, Baraban SC. Altered glutamate receptor - ctransporter expression and spontaneous seizures in rats exposed to methylazoxymethanol in utero. Epilepsia 2007;48:158–168.
Park KI, Chu K, Jung KH, et al. Role of cortical dysplasia in epileptogenesis following prolonged febrile seizure. Epilepsia 2010;51:1809–1819.
Choi IS, Cho JH, Lee MG, Choi BJ. Pilocarpine-induced seizure susceptibility in rats following prenatal methylazoxymethanol treatment. Biol Pharm Bull 2005;28:1408–1413.
Hicks SP, D'amato CJ. Low dose radiation of the developing brain. Science 1963;141:903–905.
Hossain M, Chetana M, Devi PU. Late effect of prenatal irradiation on the hippocampal histology and brain weight in adult mice. Int J Dev Neurosci 2005;23:307–313.
Roper SN. In utero irradiation of rats as a model of human cerebrocortical dysgenesis: a review. Epilepsy Res 1998;32:63–74.
Setkowicz Z, Majcher K, Janicka D, et al. Brains with different degrees of dysplasia show different patterns of neurodegenerative changes following pilocarpine-induced seizures. Histologic evidence of tissue damage correlated with MRI data. Neurol Res 2006;28:453–460.
Rosen GD, Burstein D, Galaburda AM. Changes in efferent and afferent connectivity in rats with induced cerebrocortical microgyria. J Comp Neurol 2000;418:423–440.
Hablitz JJ, DeFazio T. Excitability changes in freeze-induced neocortical microgyria. Epilepsy Res 1998;32:75–82.
Jacobs KM, Hwang BJ, Prince DA. Focal epileptogenesis in a rat model of polymicrogyria. J Neurophysiol 1999;81:159–173.
Zilles K, Qu MS, Kohling R, Speckmann EJ. Ionotropic glutamate and GABA receptors in human epileptic neocortical tissue: quantitative in vitro receptor autoradiography. Neuroscience 1999;94:1051–1061.
Redecker C, Luhmann HJ, Hagemann G, Fritschy JM, Witte OW. Differential downregulation of GABAA receptor subunits in widespread brain regions in the freeze-lesion model of focal cortical malformations. J Neurosci 2000;20:5045–5053.
Scantlebury MH, Gibbs SA, Foadjo B, Lema P, Psarropoulou C, Carmant L. Febrile seizures in the predisposed brain: a new model of temporal lobe epilepsy. Ann Neurol 2005;58:41–49.
Fauser S, Huppertz HJ, Bast T, et al. Clinical characteristics in focal cortical dysplasia: a retrospective evaluation in a series of 120 patients. Brain 2006;129:1907–1916.
Garami A, Zwartkruis FJ, Nobukuni T, et al. Insulin activation of Rheb, a mediator of mTOR/S6K/4E-BP signaling, is inhibited by TSC1 and 2. Mol Cell 2003;11:1457–1466.
Van Slegtenhorst M, Nellist M, Nagelkerken B, et al. Interaction between hamartin and tuberin, the TSC1 and TSC2 gene products. Hum Mol Genet 1998;7:1053–1057.
Orlova KA, Crino PB. The tuberous sclerosis complex. Ann N Y Acad Sci 2010;1184:87–105.
Eker R. Familial renal adenomas in Wistar rats; a preliminary report. Acta Pathol Microbiol Scand 1954;34:554–562.
Eker R, Mossige J, Johannessen JV, Aars H. Hereditary renal adenomas and adenocarcinomas in rats. Diagn Histopathol 1981;4:99–110.
Yeung RS, Xiao GH, Jin F, Lee WC, Testa JR, Knudson AG. Predisposition to renal carcinoma in the Eker rat is determined by germ-line mutation of the tuberous sclerosis 2 (TSC2) gene. Proc Natl Acad Sci U S A 1994;91:11413–11416.
Yeung RS, Katsetos CD, Klein-Szanto A. Subependymal astrocytic hamartomas in the Eker rat model of tuberous sclerosis. Am J Pathol 1997;151:1477–1486.
Wenzel HJ, Patel LS, Robbins CA, Emmi A, Yeung RS, Schwartzkroin PA. Morphology of cerebral lesions in the Eker rat model of tuberous sclerosis. Acta Neuropathol 2004;108:97–108.
Kwiatkowski DJ, Zhang H, Bandura JL, et al. A mouse model of TSC1 reveals sex-dependent lethality from liver hemangiomas, and up-regulation of p70S6 kinase activity in Tsc1 null cells. Hum Mol Genet 2002;11:525–534.
Kobayashi T, Minowa O, Kuno J, Mitani H, Hino O, Noda T. Renal carcinogenesis, hepatic hemangiomatosis, and embryonic lethality caused by a germ-line Tsc2 mutation in mice. Cancer Res 1999;59:1206–1211.
Kobayashi T, Minowa O, Sugitani Y, et al. A germ-line Tsc1 mutation causes tumor development and embryonic lethality that are similar, but not identical to, those caused by Tsc2 mutation in mice. Proc Natl Acad Sci U S A 2001;98:8762–8767.
Young DM, Schenk AK, Yang SB, Jan YN, Jan LY. Altered ultrasonic vocalizations in a tuberous sclerosis mouse model of autism. Proc Natl Acad Sci U S A 2010;107:11074–11079.
Uhlmann EJ, Apicelli AJ, Baldwin RL, et al. Heterozygosity for the tuberous sclerosis complex (TSC) gene products results in increased astrocyte numbers and decreased p27-Kip1 expression in TSC2+/− cells. Oncogene 2002;21:4050–4059.
Uhlmann EJ, Wong M, Baldwin RL, et al. Astrocyte-specific TSC1 conditional knockout mice exhibit abnormal neuronal organization and seizures. Ann Neurol 2002;52:285–296.
Wong M, Ess KC, Uhlmann EJ, et al. Impaired glial glutamate transport in a mouse tuberous sclerosis epilepsy model. Ann Neurol 2003;54:251–256.
Zeng LH, Xu L, Gutmann DH, Wong M. Rapamycin prevents epilepsy in a mouse model of tuberous sclerosis complex. Ann Neurol 2008;63:444–453.
Zeng LH, Rensing NR, Zhang B, Gutmann DH, Gambello MJ, Wong M. Tsc2 gene inactivation causes a more severe epilepsy phenotype than Tsc1 inactivation in a mouse model of tuberous sclerosis complex. Hum Mol Genet 2011;20:445–454.
Wang Y, Greenwood JS, Calcagnotto ME, Kirsch HE, Barbaro NM, Baraban SC. Neocortical hyperexcitability in a human case of tuberous sclerosis complex and mice lacking neuronal expression of TSC1. Ann Neurol 2007;61:139–152.
Meikle L, Talos DM, Onda H, et al. A mouse model of tuberous sclerosis: neuronal loss of Tsc1 causes dysplastic and ectopic neurons, reduced myelination, seizure activity, and limited survival. J Neurosci 2007;27:5546–5558.
Racine RJ. Modification of seizure activity by electrical stimulation: cortical areas. Electroencephalogr Clin Neurophysiol 1975;38:1–12.
Moshe SL. The effects of age on the kindling phenomenon. Dev Psychobiol 1981;14:75–81.
Moshe SL, Albala BJ. Kindling in developing rats: persistence of seizures into adulthood. Brain Res 1982;256:67–71.
Lothman EW, Hatlelid JM, Zorumski CF, Conry JA, Moon PF, Perlin JB. Kindling with rapidly recurring hippocampal seizures. Brain Res 1985;360:83–91.
Michelson HB, Lothman EW. An ontogenetic study of kindling using rapidly recurring hippocampal seizures. Brain Res Dev Brain Res 1991;61:79–85.
Sankar R, Auvin S, Kwon Y, Pineda E, Shin D, Mazarati A. Evaluation of development-specific targets for antiepileptogenic therapy using rapid kindling. Epilepsia. 2010 Jul;51 Suppl 3:39–42.
Wang C, Shimizu-Okabe C, Watanabe K, et al. Developmental changes in KCC1, KCC2, and NKCC1 mRNA expressions in the rat brain. Brain Res Dev Brain Res 2002;139:59–66.
Ben-Ari Y. Excitatory actions of gaba during development: the nature of the nurture. Nat Rev Neurosci 2002;3:728–739.
Dzhala VI, Talos DM, Sdrulla DA, et al. NKCC1 transporter facilitates seizures in the developing brain. Nat Med 2005;11:1205–1213.
Dzhala VI, Brumback AC, Staley KJ. Bumetanide enhances phenobarbital efficacy in a neonatal seizure model. Ann Neurol 2008;63:222–235.
Mazarati A, Shin D, Sankar R. Bumetanide inhibits rapid kindling in neonatal rats. Epilepsia 2009;50:2117–2122.
Shah MM, Mistry M, Marsh SJ, Brown DA, Delmas P. Molecular correlates of the M-current in cultured rat hippocampal neurons. J Physiol 2002;544:29–37.
Okada M, Wada K, Kamata A, Murakami T, Zhu G, Kaneko S. Impaired M-current and neuronal excitability. Epilepsia 2002;43(suppl 9):36–38.
Singh NA, Westenskow P, Charlier C, et al. KCNQ2 and KCNQ3 potassium channel genes in benign familial neonatal convulsions: expansion of the functional and mutation spectrum. Brain 2003;126:2726–2737.
Qiu C, Johnson BN, Tallent MK. K + M-current regulates the transition to seizures in immature and adult hippocampus. Epilepsia 2007;48:2047–2058.
Main MJ, Cryan JE, Dupere JR, Cox B, Clare JJ, Burbidge SA. Modulation of KCNQ2/3 potassium channels by the novel anticonvulsant retigabine. Mol Pharmacol 2000;58:253–262.
Mazarati A, Wu J, Shin D, Kwon YS, Sankar R. Antiepileptogenic and antiictogenic effects of retigabine under conditions of rapid kindling: an ontogenic study. Epilepsia 2008;49:1777–1786.
Lothman EW, Bertram EH, III. Epileptogenic effects of status epilepticus. Epilepsia 1993;34(suppl 1):S59-S70.
Lothman EW, Williamson JM. Closely spaced recurrent hippocampal seizures elicit two types of heightened epileptogenesis: a rapidly developing, transient kindling and a slowly developing, enduring kindling. Brain Res 1994;649:71–84.
Dravet C. The core Dravet syndrome phenotype. Epilepsia 2011;52(suppl 2):3–9.
Dravet C, Bureau M, Dalla BB, Guerrini R. Severe myoclonic epilepsy in infancy (Dravet syndrome) 30 years later. Epilepsia 2011;52(suppl 2):1–2.
Catterall WA. Ion channel voltage sensors: structure, function, and pathophysiology. Neuron 2010;67:915–928.
Depienne C, Trouillard O, Saint-Martin C, et al. Spectrum of SCN1A gene mutations associated with Dravet syndrome: analysis of 333 patients. J Med Genet 2009;46:183–191.
Oakley JC, Kalume F, Yu FH, Scheuer T, Catterall WA. Temperature- and age-dependent seizures in a mouse model of severe myoclonic epilepsy in infancy. Proc Natl Acad Sci U S A 2009;106:3994–3999.
Ogiwara I, Miyamoto H, Morita N, et al. Nav1.1 localizes to axons of parvalbumin-positive inhibitory interneurons: a circuit basis for epileptic seizures in mice carrying an Scn1a gene mutation. J Neurosci 2007;27:5903–5914.
Genton P, Velizarova R, Dravet C. Dravet syndrome: the long-term outcome. Epilepsia 2011;52(suppl 2):44–49.
Yu FH, Mantegazza M, Westenbroek RE, et al. Reduced sodium current in GABAergic interneurons in a mouse model of severe myoclonic epilepsy in infancy. Nat Neurosci 2006;9:1142–1149.
Kalume F, Yu FH, Westenbroek RE, Scheuer T, Catterall WA. Reduced sodium current in Purkinje neurons from Nav1.1 mutant mice: implications for ataxia in severe myoclonic epilepsy in infancy. J Neurosci 2007;27:11065–11074.
Dutton SB, Sawyer NT, Kalume F, et al. Protective effect of the ketogenic diet in Scn1a mutant mice. Epilepsia 2011;52:2050–2056.
Caraballo RH, Cersosimo RO, Sakr D, Cresta A, Escobal N, Fejerman N. Ketogenic diet in patients with Dravet syndrome. Epilepsia 2005;46:1539–1544.
Korff C, Laux L, Kelley K, Goldstein J, Koh S, Nordli D Jr. Dravet syndrome (severe myoclonic epilepsy in infancy): a retrospective study of 16 patients. J Child Neurol 2007;22:185–194.
Nabbout R, Copioli C, Chipaux M, et al. Ketogenic diet also benefits Dravet syndrome patients receiving stiripentol: a prospective pilot study. Epilepsia 2011;52:e54-e57.
van Luijtelaar EL, Drinkenburg WH, van Rijn CM, Coenen AM. Rat models of genetic absence epilepsy: what do EEG spike-wave discharges tell us about drug effects? Methods Find Exp Clin Pharmacol 2002;24(suppl D):65–70.
Guerrini R, Dravet C, Genton P, Belmonte A, Kaminska A, Dulac O. Lamotrigine and seizure aggravation in severe myoclonic epilepsy. Epilepsia 1998;39:508–512.
Burke JF, Mogg AE. Suppression of a nonsense mutation in mammalian cells in vivo by the aminoglycoside antibiotics G-418 and paromomycin. Nucleic Acids Res 1985;13:6265–6272.
Howard M, Frizzell RA, Bedwell DM. Aminoglycoside antibiotics restore CFTR function by overcoming premature stop mutations. Nat Med 1996;2:467–469.
Bedwell DM, Kaenjak A, Benos DJ, et al. Suppression of a CFTR premature stop mutation in a bronchial epithelial cell line. Nat Med 1997;3:1280–1284.
Barton-Davis ER, Cordier L, Shoturma DI, Leland SE, Sweeney HL. Aminoglycoside antibiotics restore dystrophin function to skeletal muscles of mdx mice. J Clin Invest 1999;104:375–381.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 347 kb)
Rights and permissions
About this article
Cite this article
Auvin, S., Pineda, E., Shin, D. et al. Novel Animal Models of Pediatric Epilepsy. Neurotherapeutics 9, 245–261 (2012). https://doi.org/10.1007/s13311-012-0119-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-012-0119-8