Abstract
Sodium handling is a key physiological hallmark of renal function. Alterations are generally considered a pathophysiologic event associated with kidney injury, with disturbances in the corticomedullary sodium gradient being indicative of a number of conditions. This experimental protocol review describes the individual steps needed to perform 23Na MRI; allowing accurate monitoring of the renal sodium distribution in a step-by-step experimental protocol for rodents.
This chapter is based upon work from the PARENCHIMA COST Action, a community-driven network funded by the European Cooperation in Science and Technology (COST) program of the European Union, which aims to improve the reproducibility and standardization of renal MRI biomarkers. This experimental protocol chapter is complemented by two separate chapters describing the basic concept and data analysis.
You have full access to this open access chapter, Download protocol PDF
Similar content being viewed by others
Key words
1 Introduction
Sodium is an essential body fluid electrolyte, with serum concentration tightly controlled by the renal proximal and distal tubules, the loop of Henle, and the collecting duct through a complex process of active reabsorption via transport proteins [1]. Electrolyte reabsorption requires large quantities of adenosine triphosphate (ATP), to move ions against the concentration gradient, produced via the mitochondrial tricarboxylic acid (TCA) cycle [1,2,3]. To fuel TCA activity, oxygen is delivered via a network of arterial vessels to the renal system. However, should the renal system undergo injury, for example in acute kidney injury or chronic renal disease, the delivery of oxygen to local tissues may be disrupted, and subsequently the gradient of sodium from the cortex to the medulla impaired [4].
In this chapter we describe the process of undertaking sodium MRI for assessing alterations of the corticomedullary sodium gradient in the kidney of rodents in a step-by-step experimental protocol. We also describe the rationale for acquisition parameter selection, with generic terms, with specific examples for rodent imaging on a small-bore animal MR system (Bruker Biospin, Ettlingen, Germany), and porcine imaging on whole body human MR scanner (General Electric, Waukesha, USA). Finally, we discuss the effects of acute diuretics such as furosemide to demonstrate alterations in renal sodium handling.
This experimental protocol chapter is complemented by two separate chapters describing the basic concept and data analysis, which are part of this book.
This chapter is part of the book Pohlmann A, Niendorf T (eds) (2020) Preclinical MRI of the Kidney—Methods and Protocols. Springer, New York.
2 Materials
2.1 Calibration Phantom Preparation: Rodent
2.1.1 Lab Equipment and Components
-
1.
5 mL Eppendorf tubes.
-
2.
Agarose.
-
3.
5 g Sodium chloride.
-
4.
Microwave oven.
-
5.
Beaker (microwave safe).
-
6.
Deionized water.
2.1.2 Process to Make 4% Agarose Phantoms (Example 60 and 150 mmol/L Phantoms)
-
1.
Weigh 350 mg sodium chloride.
-
2.
Weight 25 g agarose.
-
3.
Add both to a beaker with 100 mL of deionized water and stir until dissolved.
-
4.
Heat solution in a microwave oven in 30 s intervals, until thickened.
-
5.
Pipette 5 mL of solution in to Eppendorf tubes.
-
6.
Repeat for 150 mmol/L phantom , weighing 875 mg sodium chloride for an equivalent volume of water.
-
7.
Leave Eppendorf tubes to cool for 24 h and seal with Parafilm.
2.2 Animals
This experimental protocol is tailored for rats (Wistar, Sprague-Dawley or Lewis) with a body mass of 300–350 g or pigs 20–40 kg.
2.3 Lab Equipment
-
1.
Anesthesia: please refer to the chapter by Kaucsar T et al. “Preparation and Monitoring of Small Animals in Renal MRI” for an in-depth description and discussion of the anesthesia. For nonrecovery experiments urethane solution (Sigma-Aldrich, Steinheim, Germany; 20% in distilled water) can provide anesthesia for several hours with comparatively fewer side effects on renal physiology, which is an important issue.
-
2.
Gases: O2, N2, and compressed air, as well as a gas-mixing system (FMI Föhr Medical Instruments GmbH, Seeheim-Ober Beerbach, Germany) to achieve required changes in the oxygen fraction of inspired gas mixture (FiO2).
-
3.
Device for FiO2 monitoring in gas mixtures: for example, Capnomac AGM-103 (Datex GE, Chalfont St Gils, UK).
-
4.
A physiological monitoring system that can track the respiration, and which is connected to the MR system such that it can be used to trigger the image acquisition.
2.4 MRI Hardware
The general hardware requirements for renal 1H MRI on mice and rats are described in the chapter by Ramos Delgado P et al. “Hardware Considerations for Preclinical Magnetic Resonance of the Kidney.” The technique described in this chapter has been tailored for a 7 and 3 T MR system (Biospec 94/20, Bruker Biospin, Ettlingen, Germany and MR750, General Electric, Milwaukee, USA), but advice for adaptation to other field strengths is given where necessary. An additional dual or single tuned 1H/23Na surface or volume coil is required, as well as multinuclear capabilities of the MR system.
3 Methods
3.1 MR Protocol Setup
3.1.1 Total Sodium Imaging (BRUKER)
-
1.
Sequence type: 3D gradient echo sequence . This is a standard sequence on Bruker MRI systems. See Notes 1–3 for details.
-
2.
Repetition time (TR): Choose 2.5× greater than the T1 of sodium in free fluid (T1 approx. 70 ms at 7 T).
-
3.
Flip angle (FA): 90°.
-
4.
Echo time (TE): The minimum TE achievable on the system is used to acquire the rapidly decaying signal.
-
5.
Acquisition bandwidth (BW): Use the highest acquisition bandwidth possible to shorten the echo time; however, this will lead to a decrease in SNR. Low SNR may be countered by signal averaging.
-
6.
Respiration trigger: on (per excitation).
-
7.
Geometry: adapt so that animal fits into FOV in L-R direction.
-
8.
Spatial resolution: adapt to the physiological resolution aimed for in the study at hand. Recommend 1 mm × 1 mm in rats.
-
9.
Crushing: Ensure signal is crushed at the end of each readout, to ensure spoiling of latent \( {T}_2^{\ast } \)signal.
3.1.2 Total Sodium Imaging (General Electric)
-
1.
Sequence type: Fidall. This is a research pulse sequence from GE. See Notes 4–6 for sequence details.
-
2.
Calibration can be performed using the inbuilt Bloch–Siegert calibration sequence .
-
3.
Readout type: 3D cones. Waveforms can be generated using code available online (http://www-mrsrl.stanford.edu/~ptgurney/cones.php).
-
4.
Repetition time (TR): Choose 2.5× greater than the T1 of sodium in free fluid (T1 approx. 50 ms at 3 T).
-
5.
Flip angle (FA): Ernst-angle (typically 70–90°).
-
6.
Echo time (TE): The minimum TE achievable on the system is used to acquire the rapidly decaying signal.
-
7.
Acquisition bandwidth (BW): Use the highest acquisition bandwidth possible to shorten TE, however this will lead to a decrease in SNR. Low SNR may be countered by signal averaging.
-
8.
Respiration trigger: on (minimum 6 per excitation).
-
9.
Geometry: adapt so that animal fits into FOV in L-R direction.
-
10.
Crushing: Ensure signal is crushed at the end of each readout, to ensure spoiling of latent \( {T}_2^{\ast } \)signal using crusher gradients.
3.1.3 \( {T}_2^{\ast } \) Mapping (BRUKER)
-
1.
Sequence type: 3D gradient echo sequence . This is a standard sequence on Bruker MRI systems, where it is called “3D gradient echo” (see Note 1 for sequence details).
-
2.
Repetition time (TR): Choose 2.5× greater than the T1 of sodium in free fluid (T1 approx. 70 ms at 7 T).
-
3.
Flip angle (FA): 90°.
-
4.
Echo time (TE): The minimum TE achievable on the system is used to acquire the rapidly decaying signal.
-
5.
Acquisition bandwidth (BW): Use the highest acquisition bandwidth possible to shorten TE, however this will lead to a decrease in SNR. Low SNR may be countered by signal averaging.
-
6.
Geometry: adapt so that animal fits into FOV in L-R direction.
-
7.
Spatial resolution: adapt to the physiological resolution aimed for in the study at hand. Recommend 1 mm × 1 mm in rats.
-
8.
Crushing: Ensure signal is crushed at the end of each readout to ensure spoiling of latent \( {T}_2^{\ast } \) signal using crusher gradients.
-
9.
Repeat acquisition using same prescan parameters with incremented TE, ensuring at least five echo times are collected. We recommended eight echo times: 0.5, 1, 2, 4, 5, 10, 15, and 20 ms.
3.1.4 Total Sodium Imaging Agilent)
-
1.
Sequence type: 2D or 3D chemical shift imaging sequence . This is a standard sequence on preclinical MRI and clinical MRI systems. See Notes 7 and 8 for sequence details.
-
2.
Repetition time (TR): Choose 2.5× greater than the T1 of sodium in free fluid (T1 approx. 70 ms at 7 T).
-
3.
Echo time (TE): choose the shortest possible for good signal-to-noise.
-
4.
Flip angle (FA): 90° or according to the Ernst angle.
-
5.
Acquisition bandwidth (BW): Choose BW and NP to ensure sufficient resolution and acquisition time of approximately 2.5 × \( {T}_2^{\ast } \).
3.1.5 Calibration Scans
-
1.
Perform a reference scan with above given parameters using a homogeneous phantom to acquire the receive sensitivity of the RF coils and gradient trajectory (see Note 8).
-
2.
Coregistration of reference and the scans of Subheading 3.1.1–3.1.4.
-
3.
Obtain sensitivity corrected images by the quotient image of both coregistered images concentration.
-
4.
For B1 mapping (double angle method) perform a measurement using a homogeneous phantom and scan parameters reported in Subheading 3.1.1 and flip angles of α1 = 40°, α2 = 80°.
3.2 In Vivo Sodium Imaging
3.2.1 Preparations
-
1.
Anesthetize the animal, obtained venous access (tail vein for rat and ear vein for pig) and transfer it to scanner.
-
2.
Set up the temperature monitoring (rectal probe) and respiratory monitoring (balloon on chest) unit.
-
3.
Fixate the sodium phantoms to the animal near the imaging area.
-
4.
Perform anatomical imaging as described in the chapter by Pohlmann A et al. “Essential Practical Steps for MRI of the Kidney in Experimental Research.”
3.2.2 Baseline Condition
-
1.
Load the 3D GRE sequence , altering the slice orientation to the desired acquisition plane.
-
2.
Triggering: in the monitoring unit set the trigger delay so that the trigger starts at the beginning of the expiratory plateau (no chest motion) and the duration such that it covers the entire expiratory phase, that is, until just before inhalation starts.
-
3.
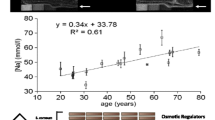
Run the sodium scan. Example images are shown in Fig. 1.
3.2.3 Imaging Furosemide Action
-
1.
Duplicate the sodium scan.
-
2.
Introduction of furosemide: Inject 10 mg/kg furosemide via tail vein catheter and begin image acquisition.
-
3.
Continue to acquire sodium imaging for up to one hour post the introduction of furosemide.
-
4.
A demonstration of the sodium changes that can be expected in pathophysiological scenarios is given in Fig. 2.
3.2.4 \( {T}_2^{\ast } \) Mapping
-
1.
Load the 3D GRE multiecho sequence , altering the slice orientation to the desired acquisition plane.
-
2.
Triggering: in the monitoring unit set the trigger delay so that the trigger starts at the beginning of the expiratory plateau (no chest motion) and the duration such that it covers the entire expiratory phase, that is, until just before inhalation starts.
-
3.
Run the sodium scan.
4 Notes
-
1.
Example 3D gradient echo sequence parameters at 4.7 T: 90° sine/cosine adiabatic pulse, echo-time/repetition-time (TE/TR) of 1.7/60 ms, FOV 12 × 12 × 5–8 cm3, and a matrix of 128 × 128 × 16 with ten scans (20 min scan time).
-
2.
Example 3D gradient echo sequence parameters at 7 T: 90° sine/cosine adiabatic pulse, echo-time/repetition-time (TE/TR) of 1.7/180 ms, FOV 12 × 12 × 5–8 cm3, and a matrix of 128 × 128 × 16 with ten scans (60 min scan time).
-
3.
Example dynamic imaging protocol at 4.7 T: 90° sine/cosine adiabatic pulse, echo-time/repetition-time (TE/TR) of 1.7/60 ms, FOV 12 × 12 × 5–8 cm3, and a matrix of 128 × 128 × 16 with two scans (4 min scan time).
-
4.
3D cones sequence parameters at 3 T: TR = 48 ms; TE = 0.5 ms, flip angle = 90°; pulse length 500 μs; receiver bandwidth = 250 kHz; readout length = 30 ms, averages = 10; slice orientation = coronal oblique; FOV = (240 × 240 × 240) mm; matrix size = 60 × 60 × 60 zero-filled to 120 × 120 × 120 (10 min scan time).
-
5.
Example dynamic imaging protocol at 3 T: TR = 48 ms; TE = 0.5 ms, flip angle = 90°; pulse length 500 μs; receiver bandwidth = 250 kHz; readout length = 30 ms, averages = 5; slice orientation = coronal oblique; FOV = (240 × 240 × 240) mm; matrix size = 60 × 60 × 60 zero-filled to 120 × 120 × 120 (5 min scan time).
-
6.
Example 3D radial UTE protocol at 9.4 T: TR = 150 ms; TE = 185 μs; 90° block pulse length of 350 μs; each radial projection was recorded in 6.4 ms of read out time (Tro) using a low acquisition bandwidth of 5 kHz; undersampling factor of 3; number of projections to 4206, nominal anisotropic resolution of (1 × 1 × 4) mm3, and FOV = 64 mm × 64 mm × 64 mm; TR = 50 ms.
-
7.
2D CSI sequence parameters at 9.4 T: Example for a 300 g rat at 9.4 T: TR = 65 ms; TE = 0.65 ms, flip angle = 90°; pulse length 500 μs; receiver bandwidth = 8 kHz; number of points = 256 complex points, averages = 8; slice orientation = axial oblique; FOV = (60 × 60) mm; matrix size = 32 × 32 zero-filled to 64 × 64; 1 slice with 1–2 cm thickness; TA = 67 s (without triggering).
-
8.
Rapid MR-imaging sequences using non-Cartesian sampling are known to be sensitive to gradient hardware imperfections and eddy-current effects that can superimpose acquired data. This is a common problem on preclinical MRI systems which compared with human MRI systems are equipped with approximately 20-fold stronger (740 mT/m maximal gradient amplitude) and 30-fold faster gradient systems (6900 T/m/s gradient slew rate). To overcome this a calibration by measuring the readout trajectory on a phantom should be performed. For further details please see [5].
References
Kiil F (1977) Renal energy metabolism and regulation of sodium reabsorption. Kidney Int 11:153–160
Klahr S, Hamm LL, Hammerman MR, Mandel LJ (2011) Renal metabolism: integrated responses. Compr Physiol. https://doi.org/10.1002/cphy.cp080249
Deng A, Miracle CM, Suarez JM et al (2005) Oxygen consumption in the kidney: effects of nitric oxide synthase isoforms and angiotensin II. Kidney Int 68:723–730
Hansell P, Welch WJ, Blantz RC, Palm F (2013) Determinants of kidney oxygen consumption and their relationship to tissue oxygen tension in diabetes and hypertension. Clin Exp Pharmacol Physiol 40:123–137
Zhang Y, Hetherington HP, Stokely EM et al (1998) A novel k-space trajectory measurement technique. Magn Reson Med 39:999–1004
Acknowledgments
This chapter is based upon work from COST Action PARENCHIMA, supported by European Cooperation in Science and Technology (COST). COST (www.cost.eu) is a funding agency for research and innovation networks. COST Actions help connect research initiatives across Europe and enable scientists to enrich their ideas by sharing them with their peers. This boosts their research, career, and innovation.
PARENCHIMA (renalmri.org) is a community-driven Action in the COST program of the European Union, which unites more than 200 experts in renal MRI from 30 countries with the aim to improve the reproducibility and standardization of renal MRI biomarkers.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2021 The Author(s)
About this protocol
Cite this protocol
Grist, J.T., Hansen, E.S., Zöllner, F.G., Laustsen, C. (2021). Sodium (23Na) MRI of the Kidney: Experimental Protocol. In: Pohlmann, A., Niendorf, T. (eds) Preclinical MRI of the Kidney. Methods in Molecular Biology, vol 2216. Humana, New York, NY. https://doi.org/10.1007/978-1-0716-0978-1_28
Download citation
DOI: https://doi.org/10.1007/978-1-0716-0978-1_28
Published:
Publisher Name: Humana, New York, NY
Print ISBN: 978-1-0716-0977-4
Online ISBN: 978-1-0716-0978-1
eBook Packages: Springer Protocols