Abstract
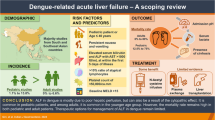
Dengue or breakbone fever is one of the most important causes of febrile illness in children residing in tropical and subtropical regions. This mosquito-borne viral disease is mediated by the bite of the infected Aedes mosquito. Dengue infection has been expanding rapidly throughout the globe in the past few decades. The virus has hepatotoxic effects. However, the pathophysiology of liver involvement in dengue is still not entirely clear. The reported clinical spectrum of dengue hepatitis ranges from mild asymptomatic elevation in transaminaselevels to acute liver failure in children. This review focuses on hepatic manifestation, the pathogenesis of liver injury, and treatment option of the effects of dengue on the liver in the pediatric population.
Similar content being viewed by others
Introduction
Dengue is nowadays become one of the most critical public health problems. It is the most rapidly spreading mosquito-borne disease in the world. Globally, there are 100 million dengue cases identified every year. Around two billion population are at risk in tropical and subtropical countries [1]. Furthermore, 60% of the world’s population is predicted to be at risk of getting dengue by 2080 [2]. Dengue virus infection may remain asymptomatic or result in a wide range of clinical manifestations. Symptomatic dengue infection is a systemic and robust disease that includes severe and non-severe clinical manifestations [3].
After the incubation period, the illness begins very quickly. The disease manifested by three phases — febrile, critical, and recovery in moderate to severe cases. The severity of the disease usually only be apparent around defervescence, i.e., during the transition of the febrile to the afebrile phase due to its dynamic nature. This stage often coincides with the onset of the critical phase.
Unusual clinical pictures of dengue fever have become more evident in recent years. Hepatic dysfunction is a well-known feature of dengue infection, despite the liver not being a primary target organ. Liver involvement may be characterized by acute hepatitis, right hypochondriac pain, hepatomegaly, jaundice, and raised aminotransferase levels [4, 5]. In addition, liver dysfunction resulting from dengue infection can be a direct viral effect on liver cells or an adverse consequence of dysregulated host immune response against the virus [6].
Dengue virus
Dengue is caused by dengue viruses (DEN-V) of the Flaviviridae family and the genus Flavivirus. There are four distinct serotypes of the virus that cause dengue (DENV-1, DENV-2, DENV-3, and DENV-4) [6].
Dengue virus infection
The illness begins abruptly after the incubation period. In moderate to severe disease, this disease is followed by three phases: febrile, critical, and recovery. High level of viremia involves different organs specially the liver and brain, and the liver is the commonest organ to be involved in severe dengue.
Mosquito-to-human transmission
Primarily, the Aedes aegypti mosquito is responsible for transmitting the virus from mosquito to human. The virus spread to humans through bites of infected female mosquitoes. After feeding on a DENV-infected person, the virus replicates in the mosquito midgut before disseminating to secondary tissues, including the salivary glands. The extrinsic incubation period (EIP) is when it takes from ingesting the virus to actual transmission to a new host. For example, if the ambient temperature remains 25–28 °C, the EIP takes about 8–12 days [7,8,9]. Variations in the extrinsic incubation period are also influenced by the magnitude of daily temperature fluctuations [10, 11], virus genotype [12], and initial viral concentration [13]. Once infectious, the mosquito can transmit the virus for lifelong.
Human-to-mosquito transmission
Mosquitoes can become infected from people with viremia with DENV who has asymptomatic dengue infection or pre-symptomatic and even asymptomatic [14]. Human-to-mosquito transmission can occur up to 2 days before someone shows symptoms of the illness [8, 14], up to 2 days after the fever has resolved [15]. Therefore, the risk of mosquito infection is strongly associated with high viremia and high fever in the patient. Most people are viremic for about 4–5 days, but viremia can persist for 12 days [16].
Case definition
According to the World Health Organization (WHO) 1997 classification, dengue has been traditionally classified into dengue fever (DF), dengue hemorrhagic fever (DHF), and dengue shock syndrome (DSS) [17, 18].
DF | Fever with at least two features: ocular pain, headache, muscle or joint pains, cutaneous rash, bleeding manifestations, and reduced leukocyte count |
DHF | Fever, thrombocytopenia (≤ 100 × 109/L), bleeding manifestations, and evidence of plasma leakage |
DSS | DHF with tachycardia or low pulse pressure (< 20 mmHg) or hypotension (systolic blood pressure < 90 mmHg) |
The modified categorization of WHO in 2009 includes dengue with or without warning signs or severe dengue [19].
Dengue | Fever and two of these as follows: nausea, vomiting, skin rash, body ache, leukopenia, or any warning sign Warning signs include abdominal pain or the presence of tenderness, persistent vomiting, clinical evidence of fluid accumulation like effusions and ascites, bleeding, lassitude or restiveness, liver enlargement, or rise in hematocrit (≥ 20%) with a rapid reduction in thrombocyte count (< 50,000/mm3) |
Severe dengue | Evidence of severe plasma leakage, bleeding, and organ impairment. Organ impairment includes hepatic involvement in the form of transaminases elevated beyond 1000 IU/L and central nervous system manifestations like alteration in sensorium or cardiac or other organ involvement |
Pathophysiology
The liver is the most widely affected organ in fatal dengue cases. Hepatitis is the most common feature [20]. The pathophysiology of liver impairment in dengue virus infection is still not clear. Liver damage in dengue is postulated to occur either due to direct viral toxicity or dysregulated immunologic injury in response to the virus [21]. Hepatocytes and Kupffer cells are primary targets for DENV infection, demonstrated by biopsies and autopsies of fatal cases [22]. Dengue viral antigens were found in hepatocytes and Kupffer cells by immune histochemistry assays and in situ hybridization and dengue viral nucleic acid in hepatocytes by PCR [23]. Viral entry into hepatocytes and Kupffer cells was mediated by phagocytosis and receptor-mediated endocytosis. The E protein has a role in the attachment of the virus [24]. The cell infected by a virus requires essentially viral entry and a conducive environment for the invader to grow inside the host cell. This property is influenced by viral strain, serotype, and cell type.
After dengue virus entry, two phases occur in Kupffer cells. First, in vitro studies demonstrated that infected Kupffer cells underwent apoptosis via nitric oxide and interferon (INF) alpha production and, a few hours later, via interleukin (IL) 6 and tumor necrosis factor (TNF) alpha-mediated pathways. Identification of the negative strand viral RNA in hepatocytes suggested that viral replication occurred within hepatocytes [20].
In vitro studies showed that the dengue virus hijacked the cellular lipid metabolism pathway for replication. Viral replication was modulated by serotype as well as cell type. HepG2 hepatoma cells were shown to be more vulnerable to infectivity with a higher viral replication rate. That is why children are more susceptible to severe dengue, as most of their hepatocytes are in the G2 phase [25]. The outcome of dengue virus infection of hepatocytes was apoptosis via different pathways, including transcription factor NF-KB activation, endoplasmic reticulum stress-triggered p38 dependent, and transcription factor CCAAT-enhancer-binding protein homologous protein-mediated apoptosis [26].
Different immune responses in dengue virus infections may contribute to varying degrees of liverimpairment. TNF alpha, IL-2, IL-6, and IL-8 levels increase in early dengue infection and reach peak levels in the initial 3 days. IL-5 and IL-10 increase subsequently [27]. IL-17 and IL-10 were associated with liver injury, and IL-17 was significantly associated with transaminase levels [21]. Higher levels of IFN gamma-induced protein-10 and IL-10 correlated with increased aspartate transaminase (AST) and painful hepatomegaly in children [28]. Liver cells from fatal dengue infection cases demonstrated increased Toll-like receptor (TLR)-2, TLR-3, IL-6, and granzyme B with inducible nitric oxide synthases, IL-18, and transforming growth factor-β, which may contribute to liver injury [29]. Pathogenesis of hepatic injury in dengue is believed to be primarily a T-cell-mediated process involving interaction between antibodies and the endothelium and a concomitant cytokine storm.
Pathology
A notable spectrum of histological changes has been noted in the liver in dengue virus infection. This comprises micro vesicular fatty change, necrosis of hepatocyte, Kupffer cells hyperplasia and destruction, Councilman bodies, and mononuclear cell infiltrates at the portal tract. Hepatocyte injury including necrotic changes usually involves the midzone area followed by the centrilobular area which may be the preferred target zone of dengue virus [22].
Clinical and biochemical profile of liver involvement
Liver involvement in acute dengue infection is frequently observed. Varying degrees of liver involvement are seen. The clinical spectrum of liver injury in children manifests as either hepatomegaly, asymptomatic elevation in transaminase levels, mild icteric hepatitis, or acute liver failure. Among the clinical features of hepatic involvement, hepatomegaly is the commonest among children. The frequency of hepatomegaly in children ranges from 12 to 80% [30,31,32,33,34]. Clinical jaundice has been detected in 0.95–60% [30,31,32,33,34] in various series among the pediatric population. Hyperbilirubinemia has been also noted though most of them are adult series [35, 36].
Elevation of liver transaminases commonly occurs during childhood dengue infection. Table 1 shows published pediatric literature describing liver abnormalities with dengue fever.
In most of the studies, AST is more remarkable than ALT. The meaning of this trend is still not clear. The AST released from damaged myocytes during dengue infection could be a possible mechanism. AST has various sources, including the heart, striated muscle, and erythrocytes, including the liver, but ALT primarily is hepatic in origin. Increased transaminase levels during the first week of infection usually decrease to average within 3 weeks [37]. The mean levels of AST ranged from 78 U/L [30] to 415 U/L [39] and ALT from 52 U/L [30] to 253 U/L [39] in pediatric age groups in different studies. A more than tenfold increase of transaminases level has been found in the severe dengue group compared to DF with or without the warning sign group [34, 39]. Various studies revealed an increased risk of liver injury with increasing severity of DF [30, 34, 39]. A large pediatric study of 372 children showed 38.7% of children had liver injuries. Among them, only 4.8% had ALT/AST > 1000 IU/L for defining severe dengue according to WHO guidelines [30]. More studies are needed to establish different cut-off values for ALT and AST for predicting severe disease. Liver injury is more common in boys [30, 40].
Coagulation abnormalities have been demonstrated in very few pediatric literature. However, prolonged PT (INR > 1.5) was found in 20% of cases, and it was significantly higher in severe dengue [34]. Hypoalbuminemia has also been seen in children, ranging from 66 to 79% [32, 34, 39].
Acute liver failure and dengue fever
Dengue-related liver failure in children is more frequent. Incidence is much higher than that of adults. The reported incidence of pediatric dengue-associated ALF has shown 14%, 18.5%, and 34.3% in different studies from India and Thailand [38, 41, 42]. The presentation of liver failure can be varied, either classical presentation of dengue with hepatitis and severe dengue or less classical dengue characteristics [22]. Mortality rate is also high which ranges from 50 to 68.3% [42,43,44]. A study from India reported 13.7% (14/102) of children developed dengue-related ALF. Nine of 11 (82%) children of severe hepatitis developed ALF either at presentation or during the hospital course. Also, < 5% of cases developed liver failure in the mild to moderate hepatitis group. The presence of severe hepatitis at presentation was a significant predictor for ALF development on binary logistic regression, p < 0.001 [38]. A large retrospective study comprising 2311 serologically confirmed adolescent and adult dengue patients showed model for end-stage liver disease (MELD) score ≥ 15 was associated with ALF from dengue-induced severe hepatitis. Deterioration of liver function and international normalized ratio (INR) ≥ 1.5 were the most significant factor of mortality related to dengue [45].
ALF due to paracetamol overdose is common. There have been enormous pieces of evidence that the metabolism of paracetamol is reduced in patients with hepatitis [46]. WHO guideline discourages other nonsteroidal anti-inflammatory drugs (ibuprofen or antipyretics) in DF [19]. Dengue can mimic ALF. It needs to be considered in the differential diagnosis of ALF and cerebral malaria in endemic areas. Dengue can also cause worsening of chronic liver disease, being the critical component of acute on chronic liver failure (ACLF) [47].
Management of dengue-associated ALF is mainly supportive. However, no specific treatment was rigorously demonstrated. Intravenous (IV) N-acetylcysteine (NAC) was proposed as a potential treatment for dengue-associated ALF. The exact mechanism of action of NAC in non-paracetamol-induced ALF was not precise. It was hypothesized to improve oxygen delivery to the tissue [48]. Few reports of NAC use among children showed clinical improvement [49, 50]. However, it was unclear whether improvement was due to the natural disease course.
High volume plasma (HVP) exchange is a promising option in ALF and ACLF as it supports hepatocyte function and eliminates cytokine storms. But the outcome is not satisfactory in the case of dengue-associated liver failure. For example, only two of five patients with dengue-related ALF survived and underwent HVP exchange [51].
Liver transplantation becomes a complex proposal instead of hemodynamic instability, bleeding manifestation, and organ failure seen during dengue infection. A recent case report demonstrated a successful living donor liver transplant (LDLT) in a 29-year-old woman with dengue-related ALF and shock [52].
Conclusion
Dengue has an extended spectrum of clinical manifestations and becomes challenging for clinicians to treat the condition. Liver dysfunction in dengue infection is more common in children than adults. Liver injury becomes more notable when the disease progresses into a more severe form. Careful monitoring and early detection of patients with severe dengue are essential for appropriate and timely medical intervention to reduce the fatal outcome. Supportive treatment is usually required to manage this group of patients. Cautious use of drugs is mandatory, which may worsen liver damage.
Availability of data and materials
Not applicable.
References
Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, Moyes CL et al (2013) The global distribution and burden of dengue. Nature 496:504–7. https://doi.org/10.1038/nature12060
Messina JP, Brady OJ, Golding N, Kraemer MUG, Wint GRW, Ray SE et al (2019) The current and future global distribution andpopulation at risk of dengue. Nat Microbiol. 4:1508–15. https://doi.org/10.1038/s41564-019-0476-8
Rigau-Pérez JG, Clark GG, Gubler DJ, Reiter P, Sanders EJ, Vorndam AV (1998) Dengue and dengue haemorrhagic fever. Lancet 352:971–77. https://doi.org/10.1016/s0140-6736(97)12483-7
Ray A, Sarker D, Chakraborty S, Chaudhuri J, Ghosh P, Chakraborty S (2013) Profile of hepatic involvement by dengue virus in dengue infected children. N Am JMed Sci 5:480–85. https://doi.org/10.4103/1947-2714.117313
Kittigul L, Pitakarnjanakul P, Sujirarat D, Siripanichgon K (2007) The differences of clinical manifestations and laboratory findings in children and adults with dengue virus infection. J ClinVirol 39:76–81. https://doi.org/10.1016/J.JCV.2007.04.006
Westaway EG, Brinton MA, GaidamovichSYa MC, Igarashi A, Kääriäinen L, Lvov DK et al (1985) Flaviviridae. Intervirology 24:183–92. https://doi.org/10.1159/000149642
Tjaden NB, Thomas SN, Fischer D, Beierkuhnlein C (2013) Extrinsic incubation period of dengue: knowledge, backlog, and applications of temperature dependence. PLoSNegl Trop Dis 7:e2207. https://doi.org/10.1371/jounal.pntd.0002207
Siler JF, Hall MW,. Hitchens AP. Dengue: its history, epidemiology, mechanism of transmission, etiology, clinical manifestations, immunity and prevention. Philipp J Sci1926;29: 1-304 Publisher: Manila, Record number: 19261000360
Watts DM, Burke DS, Harrison BA, Whitmire RE, Nisalak A (1987) Effect of temperature on the vector efficiency of Aedesaegypti for dengue 2 virus. Am J Trop Med Hyg 36:143–52. https://doi.org/10.4296/ajtmh.1987.36.143
Carrington LB, Armijos MV, Lambrechts L, Scott TW (2013) Fluctuations at low mean temperatures accelerate dengue virus transmission byAedesaegypti. PLoSNegl Trop Dis 7:e2190
Lambrechts L, Paaijmans KP, Fansiri T, Carrington LB, Kramer LD, Thomas LB et al (2011) Impact of daily temperature fluctuations on dengue virus transmission by Aedesaegypti. ProcNatlAcadSci U S A 108:7460–65. https://doi.org/10.1073/pnas.1101377108
Anderson JR, Rico-Hesse R (2006) Aedesaegyptivectorial capacity is determined by the infecting genotype of dengue virus. Am J Trop Med Hyg 75:886–92 (PMID: 17123982)
Ye YH, Carrasco AM, Frentiu FD, Chenoweth SF, Beebe NW, Hurk AF et al (2015) Wolbachia reduces the transmission potential of dengue-infected Aedesaegypti. PLoSNegl Trop Dis 9:e0003894. https://doi.org/10.1371/journal.pntd.0003894
Duong V, Lambrechts L, Paul RE, Ly S, Lay RS, Long KC et al (2015) Asymptomatic humans transmit dengue virus to mosquitoes. ProcNatlAcadSci USA 112:14688–93. https://doi.org/10.1073/pnas.1508114112
Nguyen NM, Kien DTH, Tuan TV, Quyen NTH, Tran CNB, Vo Thi L et al (2013) Host and viral features of human dengue cases shape the population of infected and infectious Aedesaegypti mosquitoes. Proc Natl Acad Sci U S A 110:9072–7. https://doi.org/10.1073/pnas.1303395110
Gubler DJ, Suharyono W, Tan R, Abidin M, Sie A et al (1981) Viraemia in patients with naturally acquired dengue infection. Bull World Health Organ 59:623–30 (PMID: 6976230)
WHO. Dengue hemorrhagic fever: diagnosis, treatment, prevention and control, Geneva, 1997. Available from: URL:http://www.who.int/csr/resources/publications/dengue/Denguepublication/en/
Lee LK, Gan VC, Lee VJ, Tan AS, Leo YS, Lye DC (2012) Clinical relevance and discriminatory value of elevated liver aminotransferase levels for dengue severity. PLoSNegl Trop Dis. 6:e1676. https://doi.org/10.1371/journal.pntd.0001676
WHO. Dengue: guidelines for diagnosis, treatment, prevention and control, Geneva, 2009.
Póvoa TF, Alves AMB, Oliveira CAB, Nuovo GJ, Chagas VLA, Paes MV (2014) The pathology of severe dengue in multiple organs of human fatal cases: histopathology, ultrastructure and virus replication. PloS one 9:e83386
Fernando S, Wijewickrama A, Gomes L, Punchihewa CT, Madusanka SDP, Dissanayake H et al (2016) Patterns and causes of liver involvement in acute dengue infection. BMC Infect Dis. 16:319. https://doi.org/10.1186/s12879-016-1656-2
Samanta J, Sharma V (2015) Dengue and its effect on liver. World J clin cases 16(3):125–31. https://doi.org/10.12998/wjcc.v3.I2.125
Jessie K, Fong MY, Devi S, Lam SK, Wong KT (2004) Localization of dengue virus in naturally infected human tissues, by immunohistochemistry and in situ hybridization. J Infect Dis. 189:1411–8. https://doi.org/10.1086/383043
van der Schaar HM, Rust MJ, Chen C, van der Ende-Metselaar H, Wilschut J, Zhuang X et al (2008) Dissecting the cell entry pathway of dengue virus by single-particle tracking in living cells. PLoSPathog 4:e1000244
Phoolcharoen W, Smith DR (2004) Internalization of the dengue virus is cell cycle modulated in HepG2, but not Vero cells. J Med Virol. 74:434–41. https://doi.org/10.1002/jmv.20195
Sreekanth GP, Chuncharunee A, Sirimontaporn A, Panaampon J, Srisawat C, Morchang A et al (2014) Role of ERK1/2 signaling in dengue virus-induced liver injury. Virus Res. 188:15–26. https://doi.org/10.1016/j.virusres.2014.03.025
Chaturvedi UC, Elbishbishi EA, Agarwal R, Raghupathy R, Nagar R, Tandon R et al (1999) Sequential production of cytokines by dengue virus-infected human peripheral blood leukocyte cultures. J Med Virol. 59:335–40. https://doi.org/10.1002/(sici)1096-9071(199911)59:3%3c335:aid-jmv13%3e3.0.co;2-e
Ferreira RA, de Oliveira SA, Gandini M, Ferreira LC, Correa G, Abiraude FM et al (2015) Circulating cytokines and chemokinesassociated with plasma leakage and hepatic dysfunction in Brazilian children with dengue fever. Acta Trop. 149:138–47. https://doi.org/10.1016/j.actatropica.2015.04.023
Pagliari C, Quaresma JA, Fernandes ER, Stegun FW, Brasil RA, de Andrade Jr HF et al (2014) Immunopathogenesis of dengue hemorrhagic fever: contribution to the study of human liver lesions. J Med Virol. 86:1193–7. https://doi.org/10.1002/jmv.23758
Srivastava G, Chhavi N, Goel A (2018) Validation of serum aminotransferases levels to define severe dengue fever in children. Pediatr Gastroenterol Hepatol Nutr 21(4):289–296. https://doi.org/10.5223/pghn.2018.21.4.289
Kulkarni MJ, Sarathi V, Bhalla V, Shivpuri D, Acharya U (2010) Clinicoepidemiological profile of children hospitalized with dengue. Indian J Pediatr 77:1103–7. https://doi.org/10.1007/s12098-010-0202-2
Pires Neto RD, de Sá SL, Pinho SC, Pucci FH, Teófilo CR, Evangelista PD et al (2013) Dengue infection in children and adolescents: clinical profile in a reference hospital in northeast Brazil. Rev Soc Bras Med Trop 46:765–8. https://doi.org/10.1590/0037-8682-1716-2013
Mohan B, Patwari AK, Anand VK (2000) Hepatic dysfunction in childhood dengue infection. J Trop Pediatr 46:40–3. https://doi.org/10.1093/tropej/46.1.40
Jagadishkumar K, Jain P, Manjunath VG, Umesh L (2012) Hepatic involvement in dengue Fever in children. Iran J Pediatr 22:231–6 (PMID: 23056891)
Saha AK, Maitra S, Hazra SCh (2013) Spectrum of hepatic dysfunction in 2012 dengue epidemic in Kolkata West Bengal. Indian J Gastroenterol 32:400–3. https://doi.org/10.1007/s12664-013-0382-6
Kuo CH, Tai DI, Chang-Chien CS, Lan CK, Chiou SS, Liaw YF (1992) Liver biochemical tests and dengue fever. Am J Trop Med Hyg 47:265–70. https://doi.org/10.4269/ajtmh.1992.47.265
Roy A, Sarkar D, Chakraborty S, Chaudhuri J, Ghosh P, Chakraborty S (2013) Profile of hepatic involvement by dengue virus in dengue infected children. N Am J Med Sci 5:480–5. https://doi.org/10.4103/1947-2714.117313
Prasad D, Bhriguvansi A (2020) Clinical profile, liver dysfunction and outcome of dengue infection in children a prospective observational study. Pediatr Infect Dis J 39:97–101. https://doi.org/10.1097/INF.0000000000002519
Rahman MA, Rao KVR, Sravya V (2018) Prediction of severity of dengue infection in children based on hepatic involvement. IOSR Journal of Dental and Medical science 17:44–9. https://doi.org/10.9790/0853-1708014449
Vega RM, Phumratanaprapin W, Phonrat B, Dhitavat J, Sutherat M, Choovichian V (2016) Differences inliver impairment between adults and children with dengue infection. Am J Trop Med Hyg 94:1073–9. https://doi.org/10.4269/ajtmh.15-0507
Kumar R, Tripathi P, Tripathi S, Kanodia A, Venkatesh V (2008) Prevalence of dengue infection in north Indian children with acute hepatic failure. Ann Hepatol. 7:59–62 (PMID: 18376367)
Poovorawan Y, Hutagalung Y, Chongsrisawat V, Boudville I, Bock HL (2006) Dengue virus infection: a major cause of acute hepatic failure in Thai children. Ann Trop Paediatr. 26:17–23. https://doi.org/10.1179/146532806X90565
Chongsrisawat V, Hutagalung Y, Poovorawan Y (2009) Liver function test results and outcomes in children with acute liver failure due to dengue infection. Southeast Asian J Trop Med Public Health. 40:47–53 (PMID: 19323033)
Laoprasopwattana K, Jundee P, Pruekprasert P, Geater A (2016) Outcome of severe dengue viral infection-caused acute liver failure in Thai children. J Trop Pead 62:200–5. https://doi.org/10.1093/tropej/fmv099
Teerasarntipan T, Chaiteerakij R, Komolmit P, Tangkijvanich P, Treeprasertsuk S (2020) Acute liver failure and death predictors in patients with dengueinduced severe hepatitis. World J Gastroenterol 26:4983–95. https://doi.org/10.3748/wjg.v26.i33.4983
Maddox JF, Amuzie CJ, Li M, Newport SW, Sparkenbaugh E, Cuff CF et al (2010) Bacterial- and viral-induced inflammation increases sensitivity to acetaminophen hepatotoxicity. J Toxicol Environ Health A 73:58–73. https://doi.org/10.1080/15287390903249057
Jha AK, Nijhawan S, Rai RR, Nepalia S, Jain P, Suchismita A (2013) Etiology, clinical profile, and inhospital mortality of acute-on-chronic liver failure: a prospective study. Indian J Gastroenterol 32:108–14. https://doi.org/10.1007/s12664-012-0295-9
Walsh TS, Hopton P, Philips BJ, Mackenzie SJ, Lee A (1998) The effect of N-acetylcysteine on oxygen transport and uptake in patients with fulminant hepatic failure. Hepatol. 27:1332–40. https://doi.org/10.1002/hep.510270520
Senanayake MP, Jayamanne MD, Kankananarachchi I (2013) N-acetylcysteine in children with acute liver failure complicating dengue viral infection. Ceylon Med J 58:80–2. https://doi.org/10.4038/cmj.v58i2.5684
Lim G, Lee JH (2012) N-acetylcysteine in children with dengue associated liver failure: a case report. J Trop Pediatr 58:409–13. https://doi.org/10.1093/tropej/fmr108
Margabandhu S, Ranjit S, Jayakumar I, Sundaramoorthy C, Janarthanan M, Reddy J (2018) Therapeutic plasma exchange for pediatric nonrenal disease indications and outcomes: a single-center experience. Asian J Transfus Sci. 12:127–35. https://doi.org/10.4103/ajts.AJTS_123_17
Chikkala BR, Pandey Y, Acharya R, Sreekumaer S, Dey R, Agarwal S (2021) Living donor liver transplant for dengue-related acute liver failure: a case report. Exp clin transplant 19:163–6. https://doi.org/10.6002/ect.2020.0217
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Dr. RA, contributed in conceptualization and writing and editing manuscript and finalized the manuscript. Professor. Md. R, contributed in manuscript writing and reviewing the manuscript. Dr. KLN, contributed in conceptualization and writing and editing manuscript
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Yes.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alam, R., Rukunuzzaman, M. & Nahid, K.L. Hepatic involvement in childhood dengue infection. Egypt Liver Journal 13, 45 (2023). https://doi.org/10.1186/s43066-023-00281-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-023-00281-9