Abstract
Background
Hepatocellular carcinoma is the most common primary liver malignancy, with the highest incidence in the developing world, including Egypt. Hepatocellular carcinoma is usually diagnosed in the terminal stage of the disease because of the low sensitivity of the available screening tests. During the process of carcinogenesis, the cellular metabolism is altered to allow cancer cells to adapt to the hypoxic environment and therefore increase anabolic synthesis and survival and avoid the apoptotic death signals. These changes in metabolic status can be tracked by metabolomics analysis.
Main body
Metabolomics is a comprehensive approach for identifying metabolic signatures towards the screening, prediction, and earlier diagnosis of hepatocellular carcinoma with greater efficiency than the conventional diagnostic biomarker. The identification of metabolic changes associated with hepatocellular carcinoma is essential to the understanding of disease pathophysiology and enables better monitoring of high-risk individuals. However, due to the complexity of the metabolic pathways associated with hepatocellular carcinoma, the details of these perturbations are still not adequately characterized. The current status of biomarkers for hepatocellular carcinoma and their insufficiencies and metabolic pathways linked to hepatocellular carcinogenesis are briefly addressed in this mini-review. The review focused on the significantly changed metabolites and pathways associated with hepatocellular carcinoma such as phospholipids, bile acids, amino acids, reactive oxygen species metabolism, and the metabolic changes related to energy production in a cancer cell. The review briefly discusses the sensitivity of metabolomics in the prediction and prognosis of hepatocellular carcinoma and the effect of coexisting multiple etiologies of the disease.
Conclusions
Metabolomics profiling is a potentially promising tool for better predicting, diagnosis, and prognosis of hepatocellular carcinoma.
Similar content being viewed by others
Background
Hepatocellular carcinoma and deficiencies in current diagnostic procedures
Hepatocellular carcinoma (HCC) is the third deadliest cancer worldwide, with a 5-year survival rate of about 10% [1, 2]. HCCs are the result of preexisting long-term cirrhosis in 90% of cases, and patients with hepatic cirrhosis are at high risk for developing HCC [1]. HCC has emerged as the fastest-rising cause of cancer-related death in many western countries, including the USA [1, 2], with a more severe and aggressive course in rural areas of Asia and sub-Saharan Africa [3]. Egypt is the first most populated country in the Arab world and the second in Africa, with more than 100 million inhabitants. Egypt has the highest incidence and prevalence of HCV infection rate, a major predisposing factor for HCC development [4, 5]. The lack of early detection of HCC results from the inaccuracy of existing HCC screening markers. Alpha-fetoprotein (AFP) remains the principal tumor marker for HCC with many advantages of being an easy, inexpensive, and reproducible blood test, although its sensitivity and predictive values of HCC range from 25 to 65% [6]. Forty percent of HCC patients have normal levels of AFP, and AFP may be high in HCC-free patients [7,8,9]. Only 20% of HCC patients at an early stage have high levels of AFP [10]. The American Association of Study for Liver Diseases (AASLD) pointed to the unreliability of AFP in accurately screening for HCC and excluded AFP as a diagnostic modality for HCC [7, 8]. To overcome the suboptimal performance of current serum markers, AFP, des-gamma-carboxyprothrombin, and lectin-bound AFP (AFP-L3), glypican-3, osteopontin, and high c-met expression had been hypothesized as alternative markers and had shown additional value [7,8,9].
However, one of the pitfalls of these HCC biomarkers is that clinicians cannot rely on them alone. Studies have shown that even combined with AFP, sensitivity to HCC remains low, in particular for lesions < 3 cm [11, 12]. Current serum markers do not play an essential role in determining prognosis and response to HCC treatment; instead, the Barcelona Clinic Liver Cancer Staging System (BCLC) and Milan criteria are widely used to predict the prognosis for HCC [11, 12]. Serum markers can be used as an adjuvant to monitor the prognosis of HCC, and high levels of AFP predict poor survival in HCC patients treated with liver transplant [11]. The Cancer of the Liver Italian Program (CLIP) score is the most widely used and best validated to monitor the prognosis and recurrence of HCC integrate AFP (> 400 ng/ml) with Child-Pugh class, tumor morphology, and portal vein thrombosis [11, 12].
Despite the magnetic resonance imaging (MRI) and computed tomography (CT) of the liver nowadays offer better accuracy in HCC diagnosis, these diagnostic modalities are still economically expensive and inaccessible to many areas suffering from the high HCC mortality rate [10, 13, 14]. Lastly, the role of liver biopsy in the diagnosis of HCC has been weakened over time as it an invasive procedure that carries the risk of tumor seeding and other serious complication as bleeding and infection. Whereas liver biopsy is a sensitive test in the diagnosis of HCC, it only detects the latter stages of the disease [15, 16]. Thus, it is quite clear that to improve the early detection of HCC, a more accurate screening and diagnostic test are required to overcome the limitation of the current modalities [15]. Biomarkers are biochemical substances that can be measured for the purpose of detecting or predicting physiological or pathological processes in response to various diagnostic or therapeutic procedures [16]. The importance of metabolomics studies and the current status of some potential biomarkers of HCC are discussed in the following sections.
Main text
Metabolomics as a cancer biomarker discovery tool
Metabolomics is the comprehensive identification of all small metabolites of less than 1.5 kDa in molecular weight in a tissue sample. A metabolomics study can be carried on varieties of samples such as plasma, serum, urine, feces, tumor cells, and normal tissue. Two analytical platforms are used in the metabolomics field, the nuclear magnetic resonance (NMR) spectroscopy and the mass spectrometry (MS) coupled with different separation instruments, such as the liquid chromatography (LC), the gas chromatography (GC), and the capillary electrophoresis. These advanced tools can detect metabolites of a diverse array of carbohydrates, lipids, amino acids, and nucleotides [16]. Metabolomics platforms are thus considered translationally optimal methods with a strong potential for clinical implementation as they facilitate rapid identification of diagnostic and prognostic markers and drug target pathways in the new drug discovery researches [17].
Metabolomics screening studies are commonly designed to identify potential biomarkers of cancer [18,19,20,21,22,23]. As chronic liver cirrhosis and HCC usually disrupt the normal metabolic pathways [24, 25], metabolomics that detects changes in the metabolic pathways related to carcinogenesis would serve in discovering new HCC biomarkers [15, 26]. Numerous published HCC metabolomics studies demonstrated the pathways involved in hepatic carcinogenesis and detected metabolites with potential use as biomarkers for HCC and cirrhosis [27, 28]. Among these pathways are the metabolic pathway of amino acid, glycerophospholipid, bile acid, acylcarnitine, oxidative stress, and β-oxidation of fatty acids [16, 26].
Significant metabolic changes in cancer cell
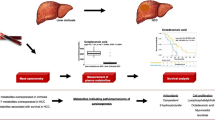
Biochemical knowledge and understanding of tumor metabolism are critical for detecting metabolic markers for any cancer. In cancer cells, glycolysis in a tumor becomes the source of substrates for the pentose-phosphate pathway for nucleotide synthesis instead of providing energy in the form of adenosine triphosphate (ATP). As a result, the proliferation and growth of the tumor cells occur at the expense of energy generation [29, 30]. The Warburg phenomenon (Fig. 1) describes how glycolysis ends with lactate production and secretion, although in the aerobic state and the recycling of NADH to NAD+, cellular carbon loss occurs upon lactate release [32, 33]. Thus, disruption of the tricarboxylic acid (TCA) cycle enzymes shifts glucose carbon towards the pentose-phosphate pathway, which produces ribose for nucleotides and anabolic synthesis [34]. It also produces NADPH for reductive biosynthesis necessary for glutathione, nucleotides, methylation reactions, glycerol synthesis, and complex lipids [35]. The hypoxic tumor with a low-nutrient microenvironment drives the cellular metabolism towards alternate carbon sources such as lactate acetate and lipids to maintain energy production and anabolic synthesis [36,37,38]. With the disruption of the TCA cycle, the mitochondrial function upregulates towards anabolic biosynthesis and the de novo fatty acid biosynthesis [39, 40]. The carbon from the catabolism of glutamine is imported into the mitochondria and used to maintain mitochondrial membrane potential [41] and for the anabolic synthesis of proteins and nucleotides [42].
Warburg effect in cancer cell metabolism: Glycolysis terminates with lactate production and secretion despite the presence of oxygen. TCA cycle enzymes shift glucose carbon towards the pentose-phosphate pathway, which produces ribose for nucleotides and NADPH for reductive biosynthesis; the hexosamine pathway to maintain glutathione levels, and methylation reactions, and glycerol synthesis for the production of complex lipids. GLUT glucose transporter, MCT monocarboxylate transporter, MPC mitochondrial pyruvate carrier, glucose-6P glucose-6-phosphate, fructose-6P fructose-6-phosphate, fructose-1,6-biP fructose-1,6-bisphosphate, DHAP dihydroxyacetone-phosphate, GA3P glyceraldehyde-3-phosphate, 3PG 3-phosphoglycerate, acetyl-CoA acetyl coenzyme-A, α-KG α-ketoglutarate, Succ-CoA succinyl-CoA, OAA oxaloacetate, NAD+ oxidized nicotinamide adenine dinucleotide, NADH, H+ reduced nicotinamide adenine dinucleotide. With modification from [31]
Metabolomics in the study of hepatocellular carcinoma
HCC-induced metabolic disturbances include fatty acid oxidation and ketone biosynthesis, citric acid cycle, phospholipid and sphingolipid metabolism, and amino acid and bile acid metabolism [43]. The initiation and development of tumors are associated with tremendous metabolic change that requires large amounts of energy and substrates for the biosynthesis of different cellular components such as nucleotide and lipid and protein [44]. Liver cirrhosis is a pathological process that results from chronic liver injury and is characterized by hepatocyte regeneration nodules and peripheral fibrosis. Liver cirrhosis usually precedes the development of HCC and is considered as a precancerous risk factor as most HCCs are associated with liver cirrhosis [45].
Alteration in the metabolic process from carbohydrate metabolism to lipid and amino acid metabolism was associated with increases in the severity of inflammation in cirrhosis by different metabolites such as D-glucose and D-mannitol. These metabolites were also observed in the early precancerous changes in HCC, which account for the relationship between chronic inflammation and HCC pathogenesis [46]. Several metabolomics studies have associated imbalances of the branched-chain amino acids (BCAA) valine, isoleucine, and leucine metabolism at the beginning of HCC. Significant variations of glutamic acid, citric acid, lactic acid, phenylalanine, tyrosine, tryptophan, and aspartate are also related to the carcinogenesis of HCC [47,48,49].
Significantly changed metabolites and pathways in HCC
Glycerophospholipids
Liver cirrhosis and HCC are associated with a profound change in the metabolism of fatty acids. Glycerophosphocholine, phosphatidylcholine, choline, and phosphorylethanolamine increased significantly in HCC compared to cirrhosis. An increase in phosphatidylcholine in the low-grade HCC compared to cirrhosis indicated possible deregulation of glycerophospholipid metabolism in the early development of HCC [28]. These phospholipids also exhibited a direct, positive relationship to tumor burden. The finding of a higher level of phosphatidylcholine, a component of the plasma membrane, reflects the increased demand for plasma membrane synthesis by the growing tumor [16].
Lysophospholipids, free fatty acids, and acylcarnitines
Several HCC metabolomics studies detected significant variations in lysophosphatidylcholines (LPC) [50,51,52,53,54]. Other lipids are significantly altered in HCC and cirrhosis such as free fatty acids (FFA), very-long-chain fatty acids, and acylcarnitines [25, 55]. Downregulated LPCs (14:0), LPC (20:3), LPC (22:6), very-long-chain fatty acids (24:0), and FFA (24:1) were observed, and all of these metabolites show a trend of being lower in HCC than cirrhosis [50]. LPC glycerophospholipids are the building blocks of the cell membranes. The increase in these metabolites indicates the metabolic demand of the growing malignant tumor. LPCs are also major lipids bound to human albumin [55]. As decreased serum albumin is a manifestation of liver cirrhosis and liver cancer, thus, elevations of systemic LPCs might be due to the lack of albumin binding sites resulting in increased circulating levels of these metabolites [56]. The previous metabolomics study reported a decrease in the level of acylcarnitines and bile acids in HCC against cirrhosis with a more significant decrease as tumor burden increased. Stage II and III HCC had a reduced concentration of these metabolites compared with stage 1 of disease metabolites [53]. The downregulation of these lipids metabolomics profile in HCC compared to cirrhosis reflects the cancer Warburg effect with a metabolic shift from the TCA cycle and mitochondrial β-oxidation to more reliance on glycolysis for energy production [57]. To bear β-oxidation in the mitochondrial matrix, the free fatty acid acyl-CoA has to react with cytosolic carnitine via the CPT shuttle system to form acylcarnitines. Acylcarnitines can penetrate the inner mitochondrial membrane to allow CPT enzymes to liberate fatty acyl-CoA allowing β-oxidation to ensue. The decrease in acylcarnitines concentration in HCC in relation to cirrhosis suggests a decrease in CPT1-mediated formation of these compounds from FFA and carnitine [57].
Sphingolipids
The upregulation of signaling molecules, sphingosine, and sphingosine-1-phosphate (S1P) stimulate the progression of many cancers, and metabolomics identified sphingosine as a typically upregulated metabolite in HCC compared to cirrhosis [58,59,60]. Sphingosine is produced via acid ceramidase activity on ceramide. Ceramides have apoptotic effects, whereas S1P is an anti-apoptotic and angiogenic molecule [61].
This cellular turnover control mechanism is known as the sphingosine rheostat, and acid ceramidase is a modulator of cell death homeostasis. Higher S1P in HCC may also reflect an increased sphingosine kinase activity. The anti-tumor effect of the selective S1P kinase inhibitor was observed in HCC xenografts suggesting that S1P may act as a promoter of HCC progression. Thus, increase acid ceramidase activity results in increased sphingosine and may lead to increased production of a large amount of S1P via sphingosine kinase that promotes a microenvironment favorable to HCC initiation [62].
Bile acids
Bile acids are synthesized in the liver and play a central role in fatty acid digestion and absorption. Increase bile acid levels in HCC could be due to obstruction of the bile duct by HCC invasion that interferes with their transfer to the small intestine resulting in insufficient digestion and absorption of fats and accumulation of bile acids and lipids in the hepatic tumor [63]. The majority of metabolomics studies which compared HCC to cirrhosis did not detect any significant bile acid expression. However, a decreasing tendency was observed for all bile acid metabolites, with a significant negative correlation between these bile acid levels and tumor growth has been observed [51, 52]. Bile acid downregulation in HCC may reflect a metabolic shift from β-oxidation and reduction in the de novo bile acid production caused by the obliteration of healthy hepatocytes during chronic liver disease [60].
Oxidative stress and metabolism
Metabolomics studies have revealed the pathways of reactive oxygen species, and the γ-glutamyl peptides are significantly associated with HCC. A metabolomics study of HCV and HBV viral hepatitis, liver cirrhosis, and HCV-associated HCC patients revealed notably significant variations in γ-glutamyl expression among these groups [64]. No differences in γ-glutamyl peptides expression were observed between HCC and cirrhosis. On the other hand, HCC and cirrhosis showed significant alterations in the expression of γ-glutamyl compared to either viral hepatitis or normal healthy controls [64].
γ-Glutamyl peptides are precursors of glutathione, the main antioxidant compound primarily synthesized in the liver. An increase in γ-glutamyl peptides in HCC and cirrhosis indicates oxidative stress and liver dysfunction, secondary to the increased demands for these precursors to combat this deteriorating process [65, 66]. γ-Glutamyl peptides are produced in a free form by the action of gamma-glutamyl transpeptidase (GGT) on glutathione. GGT is an enzyme marker for liver disease and used to assess the severity of liver dysfunction. Excessive breakdown of glutathione may explain the relative increase in γ-glutamyl peptide level in cirrhosis and the impaired oxidative stress neutralization commonly observed in HCC [65, 66].
Amino acid metabolites
The expression profiles of amino acids in HCC and advanced liver cirrhosis showed significant increases in the amino acids valine, glutamine, and glutamate in HCC relative to cirrhosis and a decrease in the amino acid lactate, alanine, leucine, glutamate, and glutamine in HCC versus cirrhosis [28]. The increased amino acids in HCC relative to cirrhosis are consistent in many studies associating elevated amino acids and the enzymes responsible for their production in the process of carcinogenesis [67,68,69,70]. In one large-scale metabolomics analysis of 60 cancer cell lines, glycine consistently upregulated in cancer cells [67]. Amino acids are glycolytic enzyme activators, and serine acts as an activator of pyruvate kinase M2 [71], a cancer isoform of the glycolytic enzyme pyruvate kinase responsible for the conversion of phosphoenolpyruvic acid (PEP) to pyruvate. Serine, glycine, and aspartate are significantly upregulated metabolites in HCC compared to cirrhosis [72]. Analysis of HBV-associated HCC showed a strong upregulation of serine, alanine, glycine, cysteine, aspartic acid, methionine, tyrosine, tryptophan, and phenylalanine. The upregulation of such amino acids in HCC could be due to their turnover in rapidly dividing tumor cells along with impaired amino acid utilization [72].
Etiological metabolomics differences
HCC is associated with various etiologies such as viral hepatitis, alcoholic cirrhosis, non-alcoholic fatty liver disease, and other environmental toxic etiology [56]. Most of the metabolomics studies focused on the metabolomics signature of a single etiology. Such an approach ignores the difference in the metabolomics expression pattern of numerous etiologies when coexisting with HCC. The metabolomics expression patterns of HCV cirrhosis-associated HCC and HBV cirrhosis-associated HCC revealed a reduction in LPC expression in HBV cirrhosis-associated HCC patients than the HCV-associated HCC. In cirrhosis, a significant elevation of bile acids, bilirubin and biliverdin, acylcarnitines, and downregulation of glycerophospholipids was also observed. Such findings suggested that these metabolites could serve as markers for the insult that triggers cirrhosis. The trend of progressive downregulation of LPCs from viral hepatitis to cirrhosis until it reaches its lowest level with the development of HCC may indicate a substantial cell death that occurs during cirrhosis. These changes result in diminished LPCs levels, followed by a subsequent massive consumption of residual LPCs by the growing HCC that further exhausts the LPC reservoir [54]. At the molecular and cellular levels, the downregulation of LPCs in HCC may reflect their anti-tumor effect, the ability to induce apoptosis, their anti-invasive effects, and sensitization of the malignant cells to various anti-cancer drugs [54].
Sensitivity and specificity of metabolomics in HCC diagnosis
In a metabolomics profile analysis, the biostatistician primarily applies several complicated statistical tests, for example, the principal component analysis, orthogonal projection to latent structures, the random forest machine-learning algorithm, or receiver operating characteristic (ROC) curve class prediction analyses. The reported sensitivity, specificity, and area under the curve values reflect the accuracy of metabolomics in distinguishing HCC from other conditions. Compared with AFP, metabolomics had been regarded as a highly accurate diagnostic method, with a clear demarcation between HCC patients and healthy controls or cirrhosis with greater class prediction power [16]. The potential standardization of metabolomics as a high-throughput clinical diagnostic platform with a big data biomarker would avoid the drew backs of depending on a single metabolite alteration that might not have the proper sensitivity and specificity for diagnosing HCC [56].
Limitation of the result achieved from the metabolomics studies
The metabolomics challenges are primarily concerned with the following aspects. (1) Technical limitations due to a large number of metabolites exceeding single-analysis processing capability [16]. (2) Since metabolomics data analysis typically depends on big data, studies with a small database may lead to false-negative or false-positive results [16]. (3) Despite the alteration in the metabolites generally encountered in HCC metabolomic studies, yet a uniform consensus regarding the shifts of the involved metabolite expression in HCC versus cirrhosis had not been achieved, not need to mention sometimes shows contradictory expression patterns [27, 28, 51, 54]. (4) The marked variation in demographic and clinical characteristic in these metabolomics studies, for example, the mass index, how HCC was diagnosed and staged, whether staged according to the Barcelona staging criteria, or the TNM classification, or imaging and histopathology, MELD scores for HCC, and the Child-Pugh for HCC or cirrhosis. Lack of control of such parameters in these studies is likely contributed to the conflicting universal metabolomics alterations in HCC versus cirrhosis among these studies and further confounded the interpretation of these metabolomics trends [50, 53, 60, 73, 74]. (5) The lack of stress on HCC versus cirrhosis comparison rather than focusing on the metabolomics profile differences between HCC versus healthy control [27, 28, 50,51,52,53,54, 60, 64, 75]. These comparisons explain the altered pathways during hepato-carcinogenesis; nevertheless, the majority of primary liver cancer occurs in preexisting cirrhosis. Thus, the metabolomics comparison between HCC and cirrhosis is more clinically instructive and potentially translational [27, 60].
Conclusions
Metabolomics is a powerful analytical tool that can be applied to identify sensitive and specific biomarkers for HCC in a noninvasive way at the early stage and to evaluate the efficacy of treatment and prognosis. The translational applicability of metabolomics is highlighted by its capability to process high volumes of patient specimens and interpret metabolic expression profiles through robust, validated, and automated software [16]. New biomarker discovery in HCC is still a complicated issue because of the inhomogeneity of the clinical symptoms of cancer and the different pathological changes that could result from potential morbid factors, such as cirrhosis, chronic inflammation, and fatty liver disease. High-throughput metabolomics approaches have transformed the HCC approach and allowed many metabolites to be examined simultaneously, thus providing valuable information for HCC biomarker discovery. Furthermore, metabolomics has significantly increased and enabled the recording of early biochemical changes occurring at different stages of the disease and, therefore, increases the opportunities to detect predictive biomarkers for early interventions [57].
Metabolomics can provide an inclusive metabolic profile of the therapeutic response and prognosis to various therapeutic modalities used to treat HCC, such as conventional chemotherapy, target therapy by small molecule inhibitors, and the natural products used in alternative medicine. These can predict the response and risk of tumor recurrence [15, 76]. As technological advances have brought metabolomics into the spotlight, metabolomics holds promise as a novel disease screening and diagnostic modality that, through characterization of a patient’s global metabolic profile, can be a more sophisticated and comprehensive manner to accurately predict the presence of disease [16].
Availability of data and materials
Partially available.
Change history
21 August 2021
A Correction to this paper has been published: https://doi.org/10.1186/s43066-021-00139-y
Abbreviations
- AFP:
-
Alpha-fetoprotein
- AASLD:
-
American Association for the Study of Liver Diseases
- ATP:
-
Adenosine triphosphate
- BCAA:
-
Branched-chain amino acid
- BCLC:
-
Barcelona Clinic Liver Cancer
- CLIP:
-
Cancer of the Liver Italian Program
- CPT:
-
Carnitine palmitoyltransferase
- CT:
-
Computed tomography
- ESAL:
-
European Association for the Study of the Liver
- FFA:
-
Free fatty acids
- GC:
-
Gas chromatography
- GGT:
-
Gamma-glutamyl transpeptidase
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- MELD:
-
Model for end-stage liver disease
- MS:
-
Mass spectrometry
- NADPH:
-
Nicotinamide adenine dinucleotide phosphate
- NHC:
-
Normal healthy control
- NMR:
-
Nuclear magnetic resonance
- PEP:
-
Phosphoenolpyruvic acid
- S1P:
-
Sphingosine-1-phosphate
- ROC:
-
Receiver operating characteristic
- TCA:
-
Tricarboxylic acid
- TNM:
-
(T) tumor, (N) nodes, (M) metastases
References
El-Serag HB, Davila JA (2011) Surveillance for hepatocellular carcinoma: in whom and how? Therap Adv Gastroenterol 4(1):5–10
El-Serag HB, Mason AC (1999) Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med 340(10):745–750
Kew MC (2013) Epidemiology of hepatocellular carcinoma in sub-Saharan Africa. Ann Hepatol 12(2):173–182
El-Serag HB, Kanwal F (2014) Epidemiology of hepatocellular carcinoma in the United States: where are we? Where do we go? Hepatology 60(5):1767–1775
Rashed WM et al (2020) Hepatocellular carcinoma (HCC) in Egypt: a comprehensive overview. J Egypt Natl Canc Inst 32(1):5
Gupta S (2003) Test characteristics of خ±-fetoprotein for detecting hepatocellular carcinoma in patients with hepatitis C. Ann Intern Med 139(1):46
Khalil A et al (2011) Plasma osteopontin level as a diagnostic marker of hepatocellular carcinoma in patients with radiological evidence of focal hepatic lesions. Tumori 99(1):100–107
Kondo S et al (2013) Clinical impact of c-Met expression and its gene amplification in hepatocellular carcinoma. Int J Clin Oncol 18(2):207–213
Xiao WK et al (2014) Prognostic significance of glypican-3 in hepatocellular carcinoma: a meta-analysis. BMC Cancer 14:104
Wild CP, Hall AJ (2000) Primary prevention of hepatocellular carcinoma in developing countries. Mutat Res/Rev Mutat Res 462(2-3):381–393
Berry K, Ioannou GN (2013) Serum alpha-fetoprotein level independently predicts posttransplant survival in patients with hepatocellular carcinoma. Liver Transpl 19(6):634–645
Liu PH et al (2016) Prognosis of hepatocellular carcinoma: assessment of eleven staging systems. J Hepatol 64(3):601–608
Venook AP et al (2010) The incidence and epidemiology of hepatocellular carcinoma: a global and regional perspective. Oncologist 15(S4):5–13
Harris PS et al (2019) Hepatocellular carcinoma surveillance: an evidence-based approach. World J Gastroenterol 25(13):1550–1559
Guo W et al (2018) Deciphering hepatocellular carcinoma through metabolomics: from biomarker discovery to therapy evaluation. Cancer Manag Res 10:715–734
Beyoglu D, Idle JR (2020) Metabolomic and lipidomic biomarkers for premalignant liver disease diagnosis and therapy. Metabolites 10(2):50
Xu Q, Schaefer WH (2012) Overview of metabolomics basics, in predictive approaches in drug discovery and development. Wiley, pp 79–137. https://doi.org/10.1002/9781118230275.ch4
Lok AS et al (2010) Des-gamma-carboxy prothrombin and alpha-fetoprotein as biomarkers for the early detection of hepatocellular carcinoma. Gastroenterology 138(2):493–502
Marshall A et al (2013) Global gene expression profiling reveals SPINK1 as a potential hepatocellular carcinoma marker. PLoS One 8(3):e59459
Pleguezuelo M et al (2010) Proteomic analysis for developing new biomarkers of hepatocellular carcinoma. World J Hepatol 2(3):127–135
Rodrigues RR, Barry CT (2011) Gene pathway analysis of hepatocellular carcinoma genomic expression datasets. J Surg Res 170(1):e85–e92
Shang S et al (2012) Identification of osteopontin as a novel marker for early hepatocellular carcinoma. Hepatology (Baltimore, Md.) 55(2):483–490
Woo HG et al (2011) Exploring genomic profiles of hepatocellular carcinoma. Mol Carcinog 50(4):235–243
Mitra V, Metcalf J (2009) Metabolic functions of the liver. Anaesth Intensive Care Med 10(7):334–335
Nguyen P et al (2008) Liver lipid metabolism. Journal of Animal Physiology and Animal Nutrition 92(3):272–283
Ward PS, Thompson CB (2012) Metabolic reprogramming: a cancer hallmark even Warburg did not anticipate. Cancer Cell 21(3):297–308
Gao R et al (2015) Serum metabolomics to identify the liver disease-specific biomarkers for the progression of hepatitis to hepatocellular carcinoma. Sci Rep 5:18175–18175
Yang Y et al (2007) Metabonomic studies of human hepatocellular carcinoma using high-resolution magic-angle spinning 1H NMR spectroscopy in conjunction with multivariate data analysis. J Proteome Res 6(7):2605–2614
Chen XS et al (2016) Anticancer strategies based on the metabolic profile of tumor cells: therapeutic targeting of the Warburg effect. Acta Pharmacol Sin 37(8):1013–1019
Jin LH, Wei C (2014) Role of microRNAs in the Warburg effect and mitochondrial metabolism in cancer. Asian Pac J Cancer Prev 15(17):7015–7019
DeBerardinis RJ, Chandel NS (2020) We need to talk about the Warburg effect. Nat Metab 2(2):127–129
Warburg O (1956) On the origin of cancer cells. Science 123(3191):309–314
Vander Heiden MG, Cantley LC, Thompson CB (2009) Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science 324(5930):1029–1033
King A, Selak MA, Gottlieb E (2006) Succinate dehydrogenase and fumarate hydratase: linking mitochondrial dysfunction and cancer. Oncogene 25(34):4675–4682
Patra KC, Hay N (2014) The pentose phosphate pathway and cancer. Trends Biochem Sci 39(8):347–354
Doherty JR, Cleveland JL (2013) Targeting lactate metabolism for cancer therapeutics. J Clin Invest 123(9):3685–3692
Schug ZT et al (2015) Acetyl-CoA synthetase 2 promotes acetate utilization and maintains cancer cell growth under metabolic stress. Cancer Cell 27(1):57–71
Kamphorst JJ et al (2014) Quantitative analysis of acetyl-CoA production in hypoxic cancer cells reveals substantial contribution from acetate. Cancer Metab 2:23
Ahn CS, Metallo CM (2015) Mitochondria as biosynthetic factories for cancer proliferation. Cancer Metab 3(1):1
Currie E et al (2013) Cellular fatty acid metabolism and cancer. Cell Metab 18(2):153–161
Wise DR, Thompson CB (2010) Glutamine addiction: a new therapeutic target in cancer. Trends Biochem Sci 35(8):427–433
DeBerardinis RJ et al (2007) Beyond aerobic glycolysis: transformed cells can engage in glutamine metabolism that exceeds the requirement for protein and nucleotide synthesis. Proc Natl Acad Sci U S A 104(49):19345–19350
Liu Y et al (2014) NMR and LC/MS-based global metabolomics to identify serum biomarkers differentiating hepatocellular carcinoma from liver cirrhosis. Int J Cancer 135(3):658–668
Minton DR et al (2015) Analyses of the transcriptome and metabolome demonstrate that HIF1alpha mediates altered tumor metabolism in clear cell renal cell carcinoma. PLoS One 10(4):e0120649
Nakayama H, Takayama T (2015) Management before hepatectomy for hepatocellular carcinoma with cirrhosis. World J Hepatol 7(20):2292–2302
Peng B et al (2015) Dynamic metabolic change is indicative of inflammation-induced transformation of hepatic cells. Int J Biochem Cell Biol 66:45–58
Nezami Ranjbar MR et al (2015) GC-MS based plasma metabolomics for identification of candidate biomarkers for hepatocellular carcinoma in Egyptian cohort. PLoS One 10(6):e0127299
Darpolor MM et al (2014) The aspartate metabolism pathway is differentiable in human hepatocellular carcinoma: transcriptomics and (13) C-isotope based metabolomics. NMR Biomed 27(4):381–389
Stepien M et al (2016) Alteration of amino acid and biogenic amine metabolism in hepatobiliary cancers: findings from a prospective cohort study. Int J Cancer 138(2):348–360
Patterson AD et al (2011) Aberrant lipid metabolism in hepatocellular carcinoma revealed by plasma metabolomics and lipid profiling. Cancer Res 71(21):6590–6600
Ressom HW et al (2012) Utilization of metabolomics to identify serum biomarkers for hepatocellular carcinoma in patients with liver cirrhosis. Anal Chim Acta 743:90–100
Wang B et al (2012) Metabonomic profiles discriminate hepatocellular carcinoma from liver cirrhosis by ultraperformance liquid chromatography–mass spectrometry. J Proteome Res 11(2):1217–1227
Xiao JF et al (2012) LC-MS based serum metabolomics for identification of hepatocellular carcinoma biomarkers in Egyptian cohort. J Proteome Res 11(12):5914–5923
Zhou L et al (2012) Serum metabolic profiling study of hepatocellular carcinoma infected with hepatitis B or hepatitis C virus by using liquid chromatography–mass spectrometry. J Proteome Res 11(11):5433–5442
Christensen E et al (1993) Peroxisomal β--oxidation of polyunsaturated long chain fatty acids in human fibroblasts. The polyunsaturated and the saturated long chain fatty acids are retroconverted by the same acyl-CoA oxidase. Scand J Clin Lab Invest 53(sup215):61–74
Wang X, Zhang A, Sun H (2013) Power of metabolomics in diagnosis and biomarker discovery of hepatocellular carcinoma. Hepatology 57(5):2072–2077
Armitage EG, Southam AD (2016) Monitoring cancer prognosis, diagnosis and treatment efficacy using metabolomics and lipidomics. Metabolomics 12:146
Furuya H, Shimizu Y, Kawamori T (2011) Sphingolipids in cancer. Cancer Metastasis Rev 30(3-4):567–576
Ojala PJ et al (2007) Acyl chain-dependent effect of lysophosphatidylcholine on human neutrophils. J Leukoc Biol 82(6):1501–1509
Fitian AI et al (2014) Integrated metabolomic profiling of hepatocellular carcinoma in hepatitis C cirrhosis through GC/MS and UPLC/MS-MS. Liver Int 34(9):1428–1444
Bao M et al (2011) Sphingosine kinase 1 promotes tumour cell migration and invasion via the S1P/EDG1 axis in hepatocellular carcinoma. Liver Int 32(2):331–338
Yang L et al (2013) Sphingosine kinase/sphingosine 1-phosphate (S1P)/S1P receptor axis is involved in liver fibrosis-associated angiogenesis. J Hepatol 59(1):114–123
El-Mir MY et al (2001) Increased levels of typically fetal bile acid species in patients with hepatocellular carcinoma. Clin Sci 100(5):499
Soga T et al (2011) Serum metabolomics reveals γ-glutamyl dipeptides as biomarkers for discrimination among different forms of liver disease. J Hepatol 55(4):896–905
Marra M et al (2011) Molecular targets and oxidative stress biomarkers in hepatocellular carcinoma: an overview. J Transl Med 9:171
Suzuki Y et al (2013) Hepatocellular carcinoma patients with increased oxidative stress levels are prone to recurrence after curative treatment: a prospective case series study using the d-ROM test. J Cancer Res Clin Oncol 139(5):845–852
Jain M et al (2012) Metabolite profiling identifies a key role for glycine in rapid cancer cell proliferation. Science (New York, N.Y.) 336(6084):1040–1044
Locasale JW et al (2011) Phosphoglycerate dehydrogenase diverts glycolytic flux and contributes to oncogenesis. Nature genetics 43(9):869–874
Luo J (2011) Cancer’s sweet tooth for serine. Breast Cancer Res 13(6):317–317
Possemato R et al (2011) Functional genomics reveal that the serine synthesis pathway is essential in breast cancer. Nature 476(7360):346–350
Chaneton B et al (2012) Serine is a natural ligand and allosteric activator of pyruvate kinase M2. Nature 491(7424):458–462
Fitian AI, Cabrera R (2017) Disease monitoring of hepatocellular carcinoma through metabolomics. World J Hepatol 9(1):1–17
Nahon P et al (2012) Identification of serum proton NMR metabolomic fingerprints associated with hepatocellular carcinoma in patients with alcoholic cirrhosis. Clin Cancer Res 18(24):6714–6722
Budhu A et al (2013) Integrated metabolite and gene expression profiles identify lipid biomarkers associated with progression of hepatocellular carcinoma and patient outcomes. Gastroenterology 144(5):1066–1075.e1
Wu F-X et al (2009) Identifying serological biomarkers of hepatocellular carcinoma using surface-enhanced laser desorption/ionization-time-of-flight mass spectroscopy. Cancer Lett 279(2):163–170
Clark P (2016) Serum markers for hepatocellular carcinoma. Clin Liver Dis (Hoboken) 8(2):29–33
Acknowledgements
This review article was written as a part of a project titled “Metabolomics characterization of chronic liver diseases versus hepatocellular carcinoma in Egyptian patients using chromatography-MS for early diagnosis of hepatocellular carcinoma” which is funded by Menofia University.
Funding
No funding was obtained for this review.
Author information
Authors and Affiliations
Contributions
AK: Writing of the manuscript, corresponding author. AF, SG, MH, GG, SA, and MA: searched the literature. MO, HS Conceived the ideas. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised as the authors noticed the following errors in the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khalil, A., Elfert, A., Ghanem, S. et al. The role of metabolomics in hepatocellular carcinoma. Egypt Liver Journal 11, 41 (2021). https://doi.org/10.1186/s43066-021-00085-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-021-00085-9