Abstract
Background
The United States has been grappling with the opioid epidemic, which has resulted in over 75,000 opioid-related deaths between April 2020 and 2021. Evidence-based pharmaceutical interventions (buprenorphine, methadone, and naltrexone) are available to reduce opioid-related overdoses and deaths. However, adoption of these medications for opioid use disorder has been stifled due to individual- and system-level barriers. External facilitation is an evidence-based implementation intervention that has been used to increase access to medication for opioid use disorder (MOUD), but the implementation costs of external facilitation have not been assessed. We sought to measure the facility-level direct costs of implementing an external facilitation intervention for MOUD to provide decision makers with estimates of the resources needed to implement this evidence-based program.
Methods
We performed a cost analysis of the pre-implementation and implementation phases, including an itemization of external facilitation team and local site labor costs. We used labor estimates from the Bureau of Labor and Statistics, and sensitivity analyses were performed using labor estimates from the Veterans Health Administration (VHA) Financial Management System general ledger data.
Results
The average total costs for implementing an external facilitation intervention for MOUD per site was $18,847 (SD 6717) and ranged between $11,320 and $31,592. This translates to approximately $48 per patient with OUD. Sites with more encounters and participants with higher salaries in attendance had higher costs. This was driven mostly by the labor involved in planning and implementation activities. The average total cost of the pre-implementation and implementation activities were $1031 and $17,816 per site, respectively. In the sensitivity analysis, costs for VHA were higher than BLS estimates likely due to higher wages.
Conclusions
Implementing external facilitation to increase MOUD prescribing may be affordable depending on the payer’s budget constraints. Our study reported that there were variations in the time invested at each phase of implementation and the number and type of participants involved with implementing an external facilitation intervention. Participant composition played an important role in total implementation costs, and decision makers will need to identify the most efficient and optimal number of stakeholders to involve in their implementation plans.
Similar content being viewed by others
Introduction
Over the last two decades, the United States (U.S.) has been grappling with the opioid epidemic, which has been further exacerbated by the coronavirus disease 2019 (COVID-19) [1]. From April 2020 to April 2021, there were 75,673 opioid-related deaths reported, an increase of 35% from the prior year [2, 3]. Evidence-based interventions to reduce opioid-related overdoses and deaths are available, such as medication treatment for opioid use disorder (MOUD) [4,5,6,7,8,9,10]. MOUD, which includes formulations of methadone, buprenorphine, and naltrexone, are evidence-based pharmaceutical therapies that are effective at reducing illicit use and improving patient outcomes associated with opioid use disorder (OUD) [10,11,12,13,14,15,16,17,18,19,20,21,22]. However, access to MOUD has been limited due to stigma, federal laws requiring providers to acquire additional specialized training, and concerns about time allocation among others [23,24,25,26].
The Veterans Health Administration (VHA), which is a part of the U.S. Department of Veterans Affairs (VA), has made progress to improve access to and prescribing of MOUD through the implementation of innovative programs [27]. One such intervention is Advancing Pharmacological Treatments for Opioid Use Disorder (ADaPT-OUD), an implementation study that was designed to examine an external facilitation intervention to reduce barriers to the provision of MOUD [28]. External facilitation is an evidence-based implementation intervention and differs from national, top-down VHA efforts by empowering local clinical teams, building on local resources and strengths, tailoring strategies to specific facility-level barriers, and promoting sustained attention to implementation [29,30,31,32]. Recent studies have reported improvements in MOUD prescribing through ADaPT-OUD [33, 34]. Gustavson and colleagues reported that seven out of eight VHA facilities that participated in ADaPT-OUD had improvements in the proportion of patients with OUD who received MOUD at the 6-month follow-up [34]. Hagedorn and colleagues reported that VHA facilities that engaged in external facilitation through ADaPT-OUD had significantly increased the proportion of patients with OUD who received MOUD from 18% at baseline to 30% at the 12-month follow-up [33]. Based in part on the success of this trial, the VHA implemented an initiative using an external facilitation intervention to improve access to MOUD in primary care, mental health, and pain clinical environments nationwide [35,36,37].
Having established the effectiveness of external facilitation in this setting, it is critical to perform an accompanying cost analysis to inform stakeholders who are considering implementing this evidence-based intervention [38]. Estimating the cost of the actual implementation piece of the intervention is a necessary but often overlooked exercise when performing a cost analysis of an evidence-based intervention. Without proper understanding of the costs associated with implementing an evidence-based intervention, decision makers will face uncertainty and may decline to invest in the strategy. Hence, it is necessary to itemize the costs of implementing an external facilitation intervention so that decision makers are informed about its impact on their budget. Studies on the cost of implementing evidence-based programs are increasing in the literature, thereby providing stakeholders with some estimates of the resources needed to properly implement evidence-based programs [38,39,40,41]. However, to date, there have been no formal evaluations on the cost of implementing an external facilitation strategy for MOUD. To address this issue, we performed a cost analysis of implementing an external facilitation program to increase MOUD in VHA.
Methods
Design
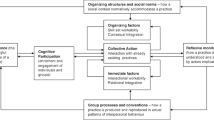
A cost analysis using micro-costing methods was performed to assess the cost of implementing ADaPT-OUD at eight VA sites [42]. Figure 1 illustrates the implementation phases for the ADaPT-OUD intervention with additional details provided in a previous publication [28]. Costs were captured for activities during the pre-site visit, on-site visit, and facilitation that took place after the on-site visit.
External facilitation team (EF)
The external facilitation (EF) team collaborated with internal implementation teams from the 8 sites that participated in ADaPT-OUD. The EF team consisted of 8 members: 4 psychologists, 3 research associates, and 1 physician-scientist.
Local staff (LS)
Local non-research staff consisted of 2 groups: internal implementation teams (IIT) and other training participants (OTP).
Internal implementation teams (IIT)
The IIT was a small group consisting of key stakeholders (e.g., facility leaders and clinicians across specialty substance use disorder [SUD] and general health care environments) who were actively involved in leading local facilitation efforts, joined cross-site and monthly facilitation calls, and were interviewed as part of the pre-implementation needs assessment. IIT members attended didactic trainings, participated in monthly coaching calls, and completed any implementation activities during their regularly paid clinical time.
Other training participants (OTP)
The OTP was a large group composed of LS who attended didactic trainings at their sites. They were a more passive audience compared to IIT.
Pre-implementation phase
The pre-implementation or planning phase was defined as the date from when the first labor-driven activity occurred (i.e., preparing resources for site visits, pre-site visit interviews) until the day before the on-site visit which varied across the eight sites. Pre-implementation activities included conducting local needs assessment for each site by interviewing local leaders and clinicians from substance use disorder clinics and other clinic settings (e.g., primary care, general mental health, pain management) that may be involved in increasing access to MOUD. Rapid qualitative analysis was performed to identify facilitators and barriers to prescribing MOUD, and a facility summary report was prepared which was discussed with the local facilitation team during the on-site visit [34, 43, 44]. The external facilitators shared a list of potential topics for face-to-face education (e.g., X-waiver training, treating OUD with buprenorphine and naltrexone, setting up a buprenorphine clinic) with each site. The IIT then selected trainings for their upcoming visit. Other pre-implementation activities by external facilitators included preparing resource materials for on-site trainings and drafting facility-specific action plans.
Implementation phase
We defined the implementation phase as the first day of the on-site visit until the last labor-driven activity (e.g., cross-site collaborative calls, post-site visit interviews) at each site. The EF team shared the facility summary report with the IIT during the on-site facility visits, which lasted between one and two days. Goals and strategies were identified and developed, and MOUD-related educational resources were provided and targeted at the broader clinical audience. Each facility was offered buprenorphine X-waiver certification education by the EF team and 7 of 8 facilities elected to receive this training [45]. X-wavier trainings were credentialed by the American Academy of Addiction Psychiatry and consisted of “half and half” trainings: 4 h of face-to-face case studies, discussions, and lectures led by the on-site external facilitator followed by 4 h of structured web-based curricular content completed at a separate time without the facilitator [46, 47]. Aside from X-waiver trainings, all other trainings (e.g., Introduction to Provider Education and Patient Tracking Resources, Site Report Review, Action Planning) ranged in length from 0.5 to 1.75 h. While training agendas were tailored to individual sites, some aspects of the site visit agenda were standardized. The 2 lead external facilitators, in collaboration with the IIT, developed action plans for each site. These plans provided the guiding goals and action steps for the remainder of the implementation phase. Facility visits were followed by continued external facilitation, including 12 monthly coaching calls, quarterly cross-site community of practice meetings, quarterly site-level feedback reports including key metrics (e.g., MOUD/OUD ratio, number of waivered prescribers, number of patients prescribed buprenorphine in the last six months, and number of patients with a diagnosis of OUD not receiving MOUD), and quarterly newsletters.
Data collection
For the pre-implementation and implementations phases, data collection for each site was done by the EF team to account for time spent on implementation activities by IITs, OTPs, and external facilitators. Sign-in sheets were collected at on-site trainings to capture the number of unique attendees along with the date and record of the training time, and names and occupations of OTPs. The three external facilitators who were most involved, self-reported the time spent on activities with each VA site using tracking logs. Tracking forms and definitions were adapted from a VHA-based implementation facilitation guide [48]. These tracking logs recorded the activities of implementation and the amount of time spent on each activity. Adhering to the facilitation guide, activities less than 15 min were not tracked. All data were entered into Excel spreadsheets and categorized according to activity type (e.g., preparation time, one-on-one or group interactions), communication mode (e.g., phone, email, video), and facilitation activities (e.g., assessment, planning, stakeholder engagement, coaching calls, individual consultation, education, program marketing, problem identification, and problem-solving) [48]. Administrative data were collected for pre and post-implementation interviews, including interviewee roles, dates, and duration of interviews. Finally, records from monthly facilitation and cross-site calls were collected and categorized by date, attendee occupation, and estimated length of calls (recorded in 0.25-h increments).
Costs data
Costs of external facilitation activities were categorized into two phases: pre-implementation (or planning) and implementation. Labor costs were estimated based on the wage rate and hours invested in implementation. The wage tables came from two sources: (1) Bureau of Labor and Statistics (BLS) and (2) VHA Financial Management System (FMS) general ledger data were used. Wages based on the BLS provided a national average that would be more generalizable to non-VHA institutions. VHA FMS general ledger contains data on VHA labor and includes the number of hours worked, the average cost per hour of work, and the occupation type (using the Budget Occupation Code) [49, 50]. BLS data did not include fringe benefits; hence, we performed additional analyses by adding a 30% fringe benefit to the wage rates based on budget guidance from VA [51]. The VHA FMS data included fringe, so we calculated the hourly rate to determine unadjusted costs. Both wage rates were used to calculate the costs of LS (i.e., IIT and OTP) and EF teams.
EF teams traveled to sites to conduct face-to-face facilitation, and travel costs were captured as part of the total costs and were collected from the VHA’s travel and expense management system. External facilitators’ travel itinerary and receipts were used to group travel costs into two categories: lodging and incidentals (e.g., hotel taxes, lodging, meals, tips, and baggage fees), and transportation (e.g., airline flight, gasoline, public transportation, car rental, taxi, and app-based ride hailing).
Analysis
Records containing information from sign-in sheets at on-site visits, interview logs, call attendance sheets, and external facilitators’ tracking reports were merged into an Excel file. These were categorized into various activities (e.g., calls, trainings, and interviews), which were further divided into subcategories (e.g., monthly facilitation calls, cross-site collaborative calls, X-waiver trainings, and pre-implementation interviews). We rounded the time spent on each activity to the nearest quarter hour. Each participant identified themselves according to their occupation or role on the sign-in sheets from the trainings. In the base-case analysis, wages for these occupations were derived from the 2020 BLS national database. Hourly wages were calculated using a formula (annual salary divided by 2080 h). Wage rates were categorized into the following: < $30 per hour, $30 to < $60 per hour, $60 to < $90 per hour, and $90 or greater per hour. Labor costs were totaled by multiplying the hourly wage of each employee by the time spent on an activity. Additional personnel labor costs were adjusted by adding 30% for fringe benefits. We presented the total costs of planning and implementation and the averaged total costs by sites including standard deviations (SD). We estimated the costs per patient (data on the number of patients with OUD at each site was based on our previous clustered, randomized-controlled trial) [33], costs per participant, and costs per encounter. We also estimated the total hours dedicated to planning and implementation and the average total hours by site including the standard deviations. A sensitivity analysis was conducted using the VHA FMS salary database to compare how total costs differed from the BLS.
Results
Overall summary (base-case analysis)
In the base-case, the average total costs for implementation-related activities per site was $18,847 (SD 6717) and ranged between $11,320 and $31,592 (Table 1 and Additional file 1: Table S1). The average total costs for a patient with OUD was $48 across all sites (minimum: $19, maximum: $173 per patient). For LS, a majority of the costs were due to implementation training activities [average cost per site = $11,456 (SD 7199)] followed by post-site visit activities (e.g., post-implementation interviews, cross-site collaborative calls) [average cost per site = $3052 (SD 1475)] and pre-implementation activities (e.g., pre-implementation interviews, site visit planning) [average cost per site = $396 (SD 67)] (Table 2). The average number of hours per site dedicated from LS to attend trainings was 145 h (SD 83), which was followed by post-site visit activities [average number of hours = 41 h (SD 18)] and pre-implementation activities [average number of hours = 5 h (SD 1)]. The average number of unique attendees per site at meetings, interviews, and trainings were 13, 14, and 28 attendees, respectively (Table 3).
Overall, most of the participants were physicians followed by EF members, service chiefs, nurse practitioners, nurses, other healthcare professions, psychologists, physician assistants, and social workers (Table 3). Additionally, a majority of participants had a wage rate of $90 or greater per hour (average number per site = 16) followed by a wage rate of $30 to $60 per hour (average number per site = 13), $60 to $90 per hour (average number per site = 4), and less than $30 per hour (average number per site = 4).
Sites with more encounters and participants with higher salaries (e.g., physicians, chiefs of staff) in attendance had higher costs. This was driven mostly by the labor involved in planning and implementation activities. For instance, Site 3 had 299 encounters with 57 unique participants; a large proportion of participants were physicians (40%) with wage rates that were $90 per hour or more (54%) (Table 1). This combination resulted in a total site-specific cost of $31,592. In contrast, Site 2 had 207 encounters with 24 unique participants that included mostly service chiefs (21%) and other healthcare professionals (17%) with wage rates of $90 or more per hour (38%) and $30 to $60 per hour (29%), respectively (Table 3). This resulted in a total site-specific cost of $11,320 (Tables 1 and 4). The average total costs per participant and per encounter were $664 and $102, respectively, across all sites (see Additional file 1: Table S1).
Overall, more time and greater costs occurred in the implementation phase compared to the planning phase across all sites. External facilitators accrued 589 total hours in the implementation phase across all sites resulting in a cost of $26,462. In the planning phase, EF accrued 100 h resulting in a cost of $5077. Similarly, LS at each of the 8 sites had greater efforts in the implementation phase with 1493 total hours across all sites resulting in an implementation phase cost of $116,068 in contrast to the pre-implementation phase where LS contributed 39 total hours across sites resulting in a cost of $3170 (Table 4).
Pre-implementation/planning phase
The average total cost of the pre-implementation phase activities was $1031 per site and ranged between $737 and $1365 (Table 4, Fig. 2). The average time invested in pre-implementation activities was 17 h per site and ranged between 13 (Site 3) and 23 h (Site 1) (Fig. 2). As the number of hours increased, the total costs also increased (see Additional file 1: Fig. S1). These costs were based on the EF team’s time conducting local needs assessment and the time dedicated by IITs. EF and IIT engaged in more pre-implementation activities at Site 1 (17 and 5 h, respectively) versus Site 3 (8 and 5 h, respectively). More time was spent on sites 1 and 2 (17 and 16 h, respectively) by the EF team as more time was expended on developing materials, which were then used for the remaining sites (see Table 4). Overall, the EF team had more variability in hours and costs across sites ranging from 8 to 17 h and $312 to $878 in costs than IIT (4 to 6 h, $303 to $511). Two external facilitators (A and B) engaged in more planning activities than other external facilitators (see Additional file 1: Table S2) because they were the only team members who traveled to sites where they led trainings with OTPs and met with IITs.
The average number of pre-implementation interviews was 9 per site and ranged from 7 to 11 interviews (Table 5). The average total cost per site of pre-implementation interviews for IITs was $396 (SD 67) and ranged from $303 to $511. The average time spent by LS for interviews per site was 5 h (SD 1) and ranged from 4 to 6 h. More than half of the EF team conducted pre-implementation interviews (see Additional file 1: Table S2). Differences in the site-specific costs for interviews were attributed to the occupation of interviewees and interviewers rather than the number or duration of interviews.
Implementation phase
The average cost of the implementation phase activities was $17,816 per site and ranged between $10,288 and $30,855 (Table 4, Fig. 2). The average time invested in implementation activities (e.g., trainings, monthly and cross-site facilitation calls) was 260 h per site and ranged from 182 to 380 h (Fig. 2). Similar to the pre-implementation phase, we observed an increase in costs when the hours invested were increased (see Additional file 1: Fig. S1). The index date for implementation was the first day of the site visit and the EF team spent 2 days with local site leaders, clinicians, and staff. There was a lot of heterogeneity in amount of time spent in each implementation phase activity across all sites. For example, Site 3 had the most attendees (n = 178) at trainings with 286 total hours contributing to its training costs of $25,064 (Table 5). Conversely, Site 2 had the least attendees (n = 25) with 40 total hours contributing to its training costs of $2594. Additionally, Site 3 had the most attendees at X-waiver trainings (n = 38) at 152 h which added $12,975 in training costs (Table 5), whereas Site 7 did not spend any time on X-waiver training.
After visiting each site, the external facilitators met separately with LS for monthly facilitation calls and quarterly cross-site collaboration calls for one year. Across all 8 sites, monthly and cross-site calls had 286 and 31 LS encounters, respectively. During the implementation phase, Sites 1 and 2 had the most staff encounters with 63 and 54 documented encounters in the monthly facilitation calls, respectively, and 7 and 10 documented encounters on the cross-site collaboration calls, respectively (Table 5). The number of post-site visit meetings was greater for Sites 1 and 2 because their on-site trainings occurred earlier in the project allowing them more opportunities to join cross-site facilitation calls.
Based on documented hours, external facilitators spent an average of 74 h per site during implementation ranging from 62 and 87 h. The average cost of EF’s effort per site was $3308 (SD 648) (Table 4).
Travel costs were based on two members (A and B) from the EF team who traveled to each site. Costs were grouped by (1) lodging and incidentals and (2) travel (Table 6). Variations in costs were attributed to the time when flight and hotel reservation were booked relative to the visit date and locality rates at different destinations.
Sensitivity analysis
In the sensitivity analysis using VHA FMS wage table, most of the staff at each of the 8 sites were in the $90 + per hour (average number per site = 15), followed by $60–$90 per hour (average number per site = 9), $30 to $60 per hour (average number per site = 7), less than $30 per hour (average number per site = 0) (see Additional file 1: Table S3). Similarly, when using the BLS wage table, many of the staff at each site were in the $90 or greater per hour wage category (average number per site = 16). Yet variation appeared in other wage categories as many of the staff were in the $30 to $60 per hour (average number per site = 13) category, followed by less than $30 per hour (average number per site = 4), and $60 to $90 per hour (average number per site = 4) categories (Table 3). Wage rates categories showed differences in total costs in the VHA FMS and BLS scales. VHA FMS totals costs were higher in the $90 + ($157,910 vs $122,715) and $60 to $90 categories ($40,010 vs $17,075) compared to BLS wage table. However, BLS totals costs were higher in the lower wage categories of $30 to $60 ($42,489 vs $32,231) and less than $30 categories ($13,780 vs $12,995) compared to the VHA FMS wage table (see Additional file 1: Fig. S2). Additional sensitivity analyses of higher salary costs in the VHA FMS wage table compared to the BLS wage table are presented in Additional file 1: Tables S2, S4, and S5.
Discussion
This was the first study to measure the facility-level direct costs of implementing an external facilitation intervention for MOUD. Our study reported that implementation costs of an external facilitation program to improve MOUD prescribing at VHA were mainly driven by labor costs. Moreover, these costs were influenced by variations in the time invested at each phase of implementation and the number and type of participants involved with implementing an external facilitation intervention. These findings provide salient accounting information for decision makers who are planning to implement a similar intervention at their medical facilities.
There are few studies that have evaluated the implementation costs of external facilitation. Ritchie and colleagues performed an assessment to capture the costs associated with facilitation of primary care mental health integration (PCMHI) at VHA regional networks [52]. The authors reported that the cost of implementation facilitation varied between $258,127 and $263,490 over a 28-month period. Labor costs of participants, excluding the EF team, comprised of 84 to 88% of the total direct costs. Our study findings were similar in that the labor costs of participants (excluding the EF) comprised 79% of the total implementation costs. However, this varied across sites and ranged from 57 to 90% of the total direct costs. Given that the study by Ritchie and colleagues was done at the regional network level and lasted two years, it was difficult to draw comparisons in terms of costs with our own implementation facilitation. However, the similarity in the proportion of labor that involved participants other than the external facilitation team supports the idea that local participation is a major driver of costs.
Each site had different needs, which are reflected by the heterogeneity of the time invested across the implementation key activities. Some sites required more X-waiver trainings (e.g., Site 3), while others did not invest time into this activity (e.g., Site 7). As more time was invested in each site, total costs increased (see Additional file 1: Fig. S1). These variations highlight the demand for flexible targeting of external facilitation based on the site’s needs, which will impact the costs of implementation. By providing the costs and key activities for each site, we have allowed stakeholders to make an informative decision on implementing an external facilitation program at their centers.
We opted to include the average total implementation cost per site alongside the cost per patient to provide stakeholders with varying perspectives of the cost estimates. Cost analyses such as the budget impact analysis summarize the cost of adopting evidence-based practice at the patient level (e.g., cost per patient, cost per member per month) [53]. This is done to provide a convenient method to scale up the intervention. However, with implementation interventions such as external facilitation, the target is a system-wide effort designed to change the practice culture to impact the patient. Hence, summarizing the overall implementation costs per site makes rational sense given the context of the intervention’s target and goals. Moreover, scalability will depend on the number of patients with OUD; as the number increases, there may be more demand to scale up operations. It is also important to mention that the Drug Enforcement Agency has recently eliminated the need for an X-waiver [54], which could improve access to MOUD patients with OUD. It is unclear how this would impact future costs, but it is an element that stakeholders and decision makers will need to incorporate.
The implementation intervention ended prior to the coronavirus disease 2019 (COVID-19) pandemic and site trainings were held in-person and without travel restrictions. This report has important implications for external facilitation amid travel restrictions due to COVID-19. External facilitation has been performed using both in-person and virtual interactions. However, with the advent of COVID-19 travel restrictions and a move toward more virtual spaces for employment and employee engagement, there could be limitations to the ability to perform in-person external facilitation. Virtual mediums may be a possible alternative to perform such work. Hartmann and colleagues provide guidance on transitioning to a fully virtual external facilitation program, which involves overarching (e.g., pilot testing, adopting a model, prioritizing metacognition) and practical principles (e.g., planning, real-time communication, relationship building, stakeholder engagement, and construction of a virtual room) [55]. However, it’s unclear whether external facilitation functions as well in a virtual space. It may benefit other institutions with limited resources for travel to investigate the effectiveness of virtual versus in-person external facilitation.
While there was no ongoing support from the EF team after the implementation phase, the external facilitators built up local teams across sites during the intervention so local staff could perform maintenance past the intervention. Only the planning and implementation phases were accounted for in the costing timeframe. Identifying the time and cost of labor to sustain an implementation intervention could further help inform policymakers and stakeholders.
Our focus with this assessment was on the costs of implementing an external facilitation intervention. We did not focus on the actual medications that are used for MOUD, such as methadone, buprenorphine, and naltrexone. These pharmaceuticals are low-cost evidence-based interventions that would offset the high costs of opioid use disorder and negative health impacts resulting from OUD. Fairley and colleagues performed a cost-effectiveness analysis to assess the value of using MOUD to treat OUD and reported that MOUDs along with naloxone for harm reduction treatment were cost-effective strategies compared to no treatment [56]. Given that the economic burden of the opioid epidemic exceeded $1 trillion dollars, MOUDs are an affordable evidence-based treatment that should be accessible to patient with OUD [57]. Future studies will need to assess the budget impact of using these MOUDs in a real-world setting.
Limitations
Despite our best efforts to capture the major domains of implementation costs associated with external facilitation, there were several limitations to this cost analysis. First, it is probable that LS facilitated implementation activities outside of trainings, interviews, and calls with the EF team that were not accounted for in our cost analysis. Since these were not observed or documented, our estimates may be underestimating the actual costs of implementation. Additionally, some external facilitation activities were not included in the accounting. For example, time spent in transit and non-work social functions (e.g., having dinner) with IITs which were used to discuss and overcome implementation barriers. Second, there is a lack of standard frameworks for the cost analysis of implementation science; hence, we approached this using a traditional economic perspective. Attempts to remedy this are underway and several papers have been published to provide guidance on this issue [40, 58]. Meanwhile, we adopted a direct micro-costing approach to capture implementation costs focusing on the planning and implementation phases [59,60,61]. Micro-costing methods are useful in capturing specific details of activities related to the intervention, but this is dependent on a careful prospective collection of data [42]. Although we did prospectively collect data, multiple participants were needed to collect and input data into our database. Potential for errors and recall bias could impact the overall costs. Alternative methods [62] using the implementation framework by Proctor and colleagues [63] have been developed based on the Time-Driven Activity-Based Costs approach from the business sector [64]. These novel approaches to capturing implementation costs should be considered in future investigations. Next, wage rates for each participant were based on average wage rates from the BLS, which can vary considerably. To address this, we performed a sensitivity analysis using FMS wage rate specific to VHA employees, which resulted in higher implementation costs. This is likely due to the higher wages federal employees incur. According to a systematic review by the Government Accountability Office (GAO-12-564), federal employees made between 4 and 58% more compared to the private sector; however, one study reported that federal employees made 28% less than the private sector [65]. Decision makers will need to validate their wage table to properly account for their labor associated with implementation. Further, we did not capture indirect costs such as the fixed costs of maintaining and operating the facilities. Therefore, our cost estimates are on the lower bound, and decision makers will need to account for the indirect costs when deciding on an implementation plan. Finally, our cost analysis was based in the VHA, which is a large, integrated healthcare system. Stakeholders at VHA may have different incentives compared to non-VHA healthcare systems to implement external facilitation programs, and our findings may not be generalizable to all non-VHA institutions [66]. For example, VHA uses clinical pharmacists differently than other health care systems. While pharmacists fill prescriptions at VHA, they also engage in care management roles [67]. For the current intervention, clinical pharmacists were champions at many of the sites [28, 33]. Moreover, VA does not bill for additional outpatient or ancillary services so the cost benefit to other health care systems might be different. However, there are similarities. This was an external facilitation and the intervention, and the costs associated with it, are applicable to other health care systems. For example, having expert facilitators, champions, and monthly contacts after a site visit can be replicated in other healthcare systems. Thus, large, integrated healthcare systems that are similar to VHA may find our findings informative, particularly if they are planning to implement a similar program at their facility.
Conclusions
External facilitation may be an affordable strategy to help address the opioid epidemic. Increasing access to MOUD would benefit Veterans through improved health outcomes. Participant composition played an important role in total implementation costs, and decision makers will need to identify the most efficient and optimal number of stakeholders to involve in their implementation plans. However, these implementation costs may be considered a necessary trade-off to address the growing morbidity and mortality of the opioid addiction crisis, and decision makers would benefit from this cost analysis to inform their own implementation plans.
Availability of data and materials
The datasets generated and analyzed during the study are not publicly available due to the sensitive nature of cost data but are available from the corresponding author on reasonable request.
Abbreviations
- ADaPT-OUD:
-
Advancing Pharmacological Treatments for Opioid Use Disorder
- BLS:
-
Bureau of Labor and Statistics
- CPT:
-
Current Procedural Terminology
- EF:
-
External facilitation
- FMS:
-
Financial Management System
- IIT:
-
Internal implementation teams
- LS:
-
Local staff
- MOUD:
-
Medication treatment for opioid use disorder
- OEND:
-
Opioid overdose education and naloxone distribution
- OTP:
-
Other training participants
- OUD:
-
Opioid use disorder
- PCMHI:
-
Primary care mental health integration
- SD:
-
Standard deviation
- SUD:
-
Substance use disorder
- VA:
-
U.S. Department of Veterans Affairs
- VHA:
-
Veterans Health Administration
- US:
-
United States
References
Manchikanti L, Singh VM, Staats PS, et al. Fourth wave of opioid (illicit drug) overdose deaths and diminishing access to prescription opioids and interventional techniques: cause and effect. Pain Physician. 2022;25(2):97–124.
National Institute on Drug Abuse. Overdose death rates: trends and statistics. National Institute on Drug Abuse; 2021. https://www.drugabuse.gov/drug-topics/trends-statistics/overdose-death-rates. Accessed 8 Feb 2021.
CDC/National Center for Heatlh Statistics. Drug overdose deaths in the U.S. top 100,000 annually. 2021. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm. Accessed 6 Dec 2021.
Binswanger IA, Koester S, Mueller SR, Gardner EM, Goddard K, Glanz JM. Overdose education and naloxone for patients prescribed opioids in primary care: a qualitative study of primary care staff. J Gen Intern Med. 2015;30(12):1837–44. https://doi.org/10.1007/s11606-015-3394-3.
Lott DC, Rhodes J. Opioid overdose and naloxone education in a substance use disorder treatment program. Am J Addict. 2016;25(3):221–6. https://doi.org/10.1111/ajad.12364.
Pauly JB, Vartan CM, Brooks AT. Implementation and evaluation of an opioid overdose education and naloxone distribution (OEND) program at a Veterans Affairs Medical Center. Subst Abuse. 2018:1–17. https://doi.org/10.1080/08897077.2018.1449174.
U.S. Department of Veterans Affairs. Opioid overdose education and naloxone distribution. Office of Research & Development; 2018. https://www.research.va.gov/research_in_action/Opioid-overdose-education-and-naloxone-distribution.cfm. Accessed 12 May 2018.
Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174.
Coffin PO, Behar E, Rowe C, et al. Nonrandomized intervention study of naloxone coprescription for primary care patients receiving long-term opioid therapy for pain. Ann Intern Med. 2016;165(4):245–52. https://doi.org/10.7326/M15-2771.
National Academies of Sciences, Engineering, and Medicine. Medications for opioid use disorder save lives. The National Academies Press; 2019. https://doi.org/10.17226/25310.
Clausen T, Anchersen K, Waal H. Mortality prior to, during and after opioid maintenance treatment (OMT): a national prospective cross-registry study. Drug Alcohol Depend. 2008;94(1–3):151–7. https://doi.org/10.1016/j.drugalcdep.2007.11.003.
Giacomuzzi SM, Ertl M, Kemmler G, Riemer Y, Vigl A. Sublingual buprenorphine and methadone maintenance treatment: a three-year follow-up of quality of life assessment. ScientificWorldJournal. 2005;5:452–68. https://doi.org/10.1100/tsw.2005.52.
Giacomuzzi SM, Riemer Y, Ertl M, et al. Buprenorphine versus methadone maintenance treatment in an ambulant setting: a health-related quality of life assessment. Addict Abingdon Engl. 2003;98(5):693–702. https://doi.org/10.1046/j.1360-0443.2003.00352.x.
Gowing L, Farrell MF, Bornemann R, Sullivan LE, Ali R. Oral substitution treatment of injecting opioid users for prevention of HIV infection. Cochrane Database Syst Rev. 2011;(8):CD004145. https://doi.org/10.1002/14651858.CD004145.pub4.
Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: a cohort study. Ann Intern Med. 2018;169(3):137–45. https://doi.org/10.7326/M17-3107.
Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;(2):CD002207. https://doi.org/10.1002/14651858.CD002207.pub4.
Ponizovsky AM, Grinshpoon A. Quality of life among heroin users on buprenorphine versus methadone maintenance. Am J Drug Alcohol Abuse. 2007;33(5):631–42. https://doi.org/10.1080/00952990701523698.
Ponizovsky AM, Margolis A, Heled L, Rosca P, Radomislensky I, Grinshpoon A. Improved quality of life, clinical, and psychosocial outcomes among heroin-dependent patients on ambulatory buprenorphine maintenance. Subst Use Misuse. 2010;45(1–2):288–313. https://doi.org/10.3109/10826080902873010.
Thomas CP, Fullerton CA, Kim M, et al. Medication-assisted treatment with buprenorphine: assessing the evidence. Psychiatr Serv Wash DC. 2014;65(2):158–70. https://doi.org/10.1176/appi.ps.201300256.
Tkacz J, Volpicelli J, Un H, Ruetsch C. Relationship between buprenorphine adherence and health service utilization and costs among opioid dependent patients. J Subst Abuse Treat. 2014;46(4):456–62. https://doi.org/10.1016/j.jsat.2013.10.014.
Volkow ND, Collins FS. The role of science in addressing the opioid crisis. N Engl J Med. 2017;377(4):391–4. https://doi.org/10.1056/NEJMsr1706626.
Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies–tackling the opioid-overdose epidemic. N Engl J Med. 2014;370(22):2063–6. https://doi.org/10.1056/NEJMp1402780.
Berk J. A good place to start — low-threshold buprenorphine initiation. N Engl J Med. 2020;383(8):701–3. https://doi.org/10.1056/NEJMp2017363.
Poorman E. The number needed to prescribe — what would it take to expand access to buprenorphine? N Engl J Med. 2021;384(19):1783–4. https://doi.org/10.1056/NEJMp2101298.
Hutchinson E, Catlin M, Andrilla CHA, Baldwin LM, Rosenblatt RA. Barriers to primary care physicians prescribing buprenorphine. Ann Fam Med. 2014;12(2):128–33. https://doi.org/10.1370/afm.1595.
Haffajee RL, Bohnert ASB, Lagisetty PA. Policy pathways to address provider workforce barriers to buprenorphine treatment. Am J Prev Med. 2018;54(6 Suppl 3):S230–42. https://doi.org/10.1016/j.amepre.2017.12.022.
Wyse JJ, Gordon AJ, Dobscha SK, et al. Medications for opioid use disorder in the Department of Veterans Affairs (VA) health care system: historical perspective, lessons learned, and next steps. Subst Abuse. 2018;39(2):139–44. https://doi.org/10.1080/08897077.2018.1452327.
Hagedorn H, Kenny M, Gordon AJ, et al. Advancing Pharmacological Treatments for Opioid Use Disorder (ADaPT-OUD): protocol for testing a novel strategy to improve implementation of medication-assisted treatment for veterans with opioid use disorders in low-performing facilities. Addict Sci Clin Pract. 2018;13(1):25. https://doi.org/10.1186/s13722-018-0127-z.
Stetler CB, Legro MW, Rycroft-Malone J, et al. Role of “external facilitation” in implementation of research findings: a qualitative evaluation of facilitation experiences in the Veterans Health Administration. Implement Sci. 2006;1(1):23. https://doi.org/10.1186/1748-5908-1-23.
Hagedorn H, Dieperink E, Dingmann D, et al. Integrating hepatitis prevention services into a substance use disorder clinic. J Subst Abuse Treat. 2007;32(4):391–8. https://doi.org/10.1016/j.jsat.2006.10.004.
Hagedorn HJ, Rettmann N, Dieperink E, Knott A, Landon BE. A training model for implementing hepatitis prevention services in substance use disorder clinics: a qualitative evaluation. J Gen Intern Med. 2015;30(8):1215–21. https://doi.org/10.1007/s11606-015-3317-3.
Kirchner JE, Ritchie MJ, Pitcock JA, Parker LE, Curran GM, Fortney JC. Outcomes of a partnered facilitation strategy to implement primary care-mental health. J Gen Intern Med. 2014;29(Suppl 4):904–12. https://doi.org/10.1007/s11606-014-3027-2.
Hagedorn HJ, Gustavson AM, Ackland PE, et al. Advancing pharmacological treatments for opioid use disorder (ADaPT-OUD): an implementation trial in eight veterans health administration facilities. J Gen Intern Med. 2022;37(14):3594–602. https://doi.org/10.1007/s11606-021-07274-7.
Gustavson AM, Wisdom JP, Kenny ME, et al. Early impacts of a multi-faceted implementation strategy to increase use of medication treatments for opioid use disorder in the Veterans Health Administration. Implement Sci Commun. 2021;2(1):20. https://doi.org/10.1186/s43058-021-00119-8.
Gordon AJ, Drexler K, Hawkins EJ, et al. Stepped Care for Opioid Use Disorder Train the Trainer (SCOUTT) initiative: expanding access to medication treatment for opioid use disorder within Veterans Health Administration facilities. Subst Abuse. 2020;41(3):275–82. https://doi.org/10.1080/08897077.2020.1787299.
Hawkins EJ, Danner AN, Malte CA, et al. Clinical leaders and providers’ perspectives on delivering medications for the treatment of opioid use disorder in Veteran Affairs’ facilities. Addict Sci Clin Pract. 2021;16(1):55. https://doi.org/10.1186/s13722-021-00263-5.
Hawkins EJ, Malte CA, Gordon AJ, et al. Accessibility to medication for opioid use disorder after interventions to improve prescribing among nonaddiction clinics in the US veterans health care system. JAMA Netw Open. 2021;4(12):e2137238. https://doi.org/10.1001/jamanetworkopen.2021.37238.
Wagner TH, Yoon J, Jacobs JC, et al. Estimating costs of an implementation intervention. Med Decis Mak Int J Soc Med Decis Mak. 2020;40(8):959–67. https://doi.org/10.1177/0272989X20960455.
Saldana L, Chamberlain P, Bradford WD, Campbell M, Landsverk J. The cost of implementing new strategies (COINS): a method for mapping implementation resources using the stages of implementation completion. Child Youth Serv Rev. 2014;39:177–82. https://doi.org/10.1016/j.childyouth.2013.10.006.
Eisman AB, Quanbeck A, Bounthavong M, Panattoni L, Glasgow RE. Implementation science issues in understanding, collecting, and using cost estimates: a multi-stakeholder perspective. Implement Sci. 2021;16(1):75. https://doi.org/10.1186/s13012-021-01143-x.
Bowser DM, Henry BF, McCollister KE. Cost analysis in implementation studies of evidence-based practices for mental health and substance use disorders: a systematic review. Implement Sci. 2021;16(1):26. https://doi.org/10.1186/s13012-021-01094-3.
Barnett PG. An improved set of standards for finding cost for cost-effectiveness analysis. Med Care. 2009;47(7 Suppl 1):S82-88. https://doi.org/10.1097/MLR.0b013e31819e1f3f.
Gale RC, Wu J, Erhardt T, et al. Comparison of rapid vs in-depth qualitative analytic methods from a process evaluation of academic detailing in the Veterans Health Administration. Implement Sci. 2019;14(1):11. https://doi.org/10.1186/s13012-019-0853-y.
Hamilton AB, Brunner J, Cain C, et al. Engaging multilevel stakeholders in an implementation trial of evidence-based quality improvement in VA women’s health primary care. Transl Behav Med. 2017;7(3):478–85. https://doi.org/10.1007/s13142-017-0501-5.
Gordon AJ, Kenny M, Dungan M, et al. Are x-waiver trainings enough? Facilitators and barriers to buprenorphine prescribing after x-waiver trainings. Am J Addict. 2022;31(2):152–8. https://doi.org/10.1111/ajad.13260.
American Academy of Addication Psychiatry. American Academy of Addiction Psychiatry - X-Waiver Training. 8 hour and 24 hour X-waiver training. https://www.aaap.org/education/waiver-training/. Accessed 31 Jan 2022.
Providers Clinical Support System. Medication assisted treatment for opioid use disorder overview. Providers Clinical Support System. https://pcssnow.org/medications-for-opioid-use-disorder/. Accessed 7 Feb 2022.
Ritchie MJ, Dollar KM, Miller CJ, et al. Using implementation facilitation to improve care in the Veterans Health Administration (version 2). Veterans Health Adm Qual Enhanc Res Initiat QUERI Team-Based Behav Health. 2017. https://www.queri.research.va.gov/tools/implementation.cfm. Accessed 6 Feb 2023.
VA Health Economics Resource Center. Cost of VA staff & labor. https://www.herc.research.va.gov/include/page.asp?id=cost-stf-labor. Accessed 3 Aug 2020.
Barnett PG, Dally SK, Scott WJ. Researchers’ guide to estimating VHA labor costs: FY2000 to FY2022. Dataset. Menlo Park: VA Palo Alto, Health Economics Resource Center; 2023.
U.S. Department of Veterans Affairs, Office of Research & Development. HSR&D Merit Review Award (Parent I01). 2021. https://www.va.gov/files/2022-07/hx-22-001-parent.pdf. Accessed 6 Feb 2023.
Ritchie MJ, Kirchner JE, Townsend JC, Pitcock JA, Dollar KM, Liu CF. Time and organizational cost for facilitating implementation of primary care mental health integration. J Gen Intern Med. 2020;35(4):1001–10. https://doi.org/10.1007/s11606-019-05537-y.
Sullivan SD, Mauskopf JA, Augustovski F, et al. Budget impact analysis-principles of good practice: report of the ISPOR 2012 Budget Impact Analysis Good Practice II Task Force. Value Health J Int Soc Pharmacoeconomics Outcomes Res. 2014;17(1):5–14. https://doi.org/10.1016/j.jval.2013.08.2291.
Substance Abuse and Mental Health Services Administration. Removal of DATA Waiver (X-Waiver) Requirement. 2023. https://www.samhsa.gov/medications-substance-use-disorders/removal-data-waiver-requirement. Accessed 6 Feb 2023.
Hartmann CW, Engle RL, Pimentel CB, et al. Virtual external implementation facilitation: successful methods for remotely engaging groups in quality improvement. Implement Sci Commun. 2021;2(1):66. https://doi.org/10.1186/s43058-021-00168-z.
Fairley M, Humphreys K, Joyce VR, et al. Cost-effectiveness of treatments for opioid use disorder. JAMA Psychiat. 2021;78(7):767–77. https://doi.org/10.1001/jamapsychiatry.2021.0247.
Florence C, Luo F, Rice K. The economic burden of opioid use disorder and fatal opioid overdose in the United States, 2017. Drug Alcohol Depend. 2021;218:108350. https://doi.org/10.1016/j.drugalcdep.2020.108350.
Dopp AR, Kerns SEU, Panattoni L, et al. Translating economic evaluations into financing strategies for implementing evidence-based practices. Implement Sci. 2021;16(1):66. https://doi.org/10.1186/s13012-021-01137-9.
Barnett PG. Review of methods to determine VA health care costs. Med Care. 1999;37(4 Suppl Va):AS9-17.
Frick KD. Micro-costing quantity data collection methods. Med Care. 2009;47(7 Suppl 1):S76–81. https://doi.org/10.1097/MLR.0b013e31819bc064.
Polsky D, Glick H. Costing and cost analysis in randomised trials: caveat emptor. Pharmacoeconomics. 2009;27(3):179–88.
Cidav Z, Mandell D, Pyne J, Beidas R, Curran G, Marcus S. A pragmatic method for costing implementation strategies using time-driven activity-based costing. Implement Sci. 2020;15(1):28. https://doi.org/10.1186/s13012-020-00993-1.
Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8(1):139. https://doi.org/10.1186/1748-5908-8-139.
Kaplan RS, Anderson SR. Time-driven activity-based costing. Harv Bus Rev. 2004. https://hbr.org/2004/11/time-driven-activity-based-costing. Accessed 6 Feb 2023.
U.S. Government Accountability Office. Results of studies on federal pay varied due to differing methodologies. 2012. p. 66. https://www.gao.gov/assets/gao-12-564.pdf. Accessed 7 Mar 2023.
Mahajan A, Madhani P, Chitikeshi S, Selvaganesan P, Russell A, Mahajan P. Advanced data analytics for improved decision-making at a veterans affairs medical center. J Healthc Manag Am Coll Healthc Exec. 2019;64(1):54–62. https://doi.org/10.1097/JHM-D-17-00164.
Giannitrapani KF, Glassman PA, Vang D, et al. Expanding the role of clinical pharmacists on interdisciplinary primary care teams for chronic pain and opioid management. BMC Fam Pract. 2018;19(1):107. https://doi.org/10.1186/s12875-018-0783-9.
Acknowledgements
We would like to thank all of the implementation teams from our intervention facilities. We would also like to thank Adam Chow for helpful guidance on analysis.
Reporting guidelines
The CHEERS checklist is uploaded as an “Additional file”.
Funding
This study was funded by the Veteran Administrations Health Services Research and Development Investigator Initiated Research Project #16–145. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
Author information
Authors and Affiliations
Contributions
HJH conceptualized the study. AJG and HJH obtained funding. HJH, AJG, AMG, PEA, AHSH, BC, SN, and MEK designed the study. HJH, AJG, AMG, PEA, and MEK implemented the study. HJH, AJG, and MEK collected the data. CCG, MB, AE, and AB analyzed the data. CCG and MB wrote the initial draft with all other authors, including AHSH and WM, providing feedback and revisions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by VA Central IRB 16-23.
Consent for publication
We consent to publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Cost per patient, participant, and encounter*. Table S2. Number of encounters by external facilitators per facilitation activity. Table S3. Number of unique participants by wage category per sitea (VHA FMS data). Table S4. Costs of local site clinicians, leadership, and staffa,b (VA FMS Data). Table S5. Costs of external facilitation team (VHA FMS Data). Figure S1. Correlation between total hours and total costs for the Planning and Implementation phases. Figure S2. Total Costs by Wage Rate Categoriesa.
Additional file 2.
CHEERS 2022 Checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Garcia, C.C., Bounthavong, M., Gordon, A.J. et al. Costs of implementing a multi-site facilitation intervention to increase access to medication treatment for opioid use disorder. Implement Sci Commun 4, 91 (2023). https://doi.org/10.1186/s43058-023-00482-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43058-023-00482-8