Abstract
Background
Ewing’s sarcoma is categorized as small round cell aggressive tumor which commonly occurs in bone and soft tissue. Primary renal Ewing’s sarcoma is an extremely rare entity and accounts for less than 1% of renal masses. It is characterized by a very aggressive course, with very few reported cases in the literature. Primary renal Ewing’s sarcoma is indistinguishable from renal cell carcinoma on anatomical imaging and therefore need histopathological correlation for confirmation. The positron emission tomography (PET) fused with computed tomography (CT) helps in the evaluation of disease, for staging and metastatic workup.
Case presentation
We present a case of 48-year-old lady who presented to urology department with difficulty in passing urine for 5 months associated with pain in the right flank region. She had an episode of haematuria 5 months back. Contrast enhanced CT showed a large lobulated heterogeneously enhancing right retroperitoneal mass in renal fossa. Histopathological examination and immunohistochemistry were suggestive of Ewing’s sarcoma. The PET/CT revealed FDG avid right renal mass with lymph nodal and skeletal metastasis.
Conclusions
Ewing’s sarcoma being aggressive tumour usually present with bone, liver and lung metastasis along with lymph nodal metastasis at time of diagnosis. The 18 F FDG PET/CT helps in diagnosis, staging, appropriate treatment planning, restaging, response evaluation and prognostication of Ewing’s sarcoma.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Ewing’s sarcoma is typically a bone or soft tissue, round cell sarcoma of primitive neuroectodermal origin. It rarely occurs as a primary renal neoplasm [1] and exhibits highly aggressive biological behaviour [2]. Fewer than 150 cases are reported till date [3] and most patients are young adults in the age group of 20 to 40 years with rare paediatric case reports. Primary Renal Ewing’s sarcoma is highly malignant, grows rapidly, and metastasizes early to the lung, bone and lymph node. We present a case of 48-year-old female patient with primary renal Ewing’s sarcoma who was referred for 18F FDG PET CT to our department of nuclear medicine for staging of disease.
Case presentation
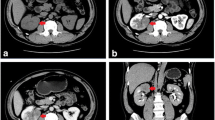
A 48-year-old female presented to the urology department with difficulty in passing urine for 5 months associated with pain in the right flank region. She had an episode of haematuria 5 months back. The pain was intermittent in nature, with no acute exacerbations. She underwent contrast enhanced CT (CECT) abdomen which showed a large lobulated heterogeneously enhancing retroperitoneal mass lesion which had completely replaced the right kidney. It also showed multiple areas of internal necrosis and haemorrhage without any fat component or calcifications. The mass was extending superiorly with scalloping of the inferior surface of the right lobe of the liver with focal loss of fat planes. Medially it was crossing the midline, abutting the aorta more than,, renal vein, posteriorly extending up to the posterior abdominal wall and anteriorly abutting the antropyloric region of the stomach, duodenum and pancreatic head. Multiple large veins, including the right renal vein, left common iliac and infrahepatic part of IVC show thrombosis. The findings were suggestive of renal cell carcinoma. The renal scan using 99mTc ethylene dicysteine (EC) was done to check the functional status of the right kidney and there was non-visualization of the right kidney during the study course and in delayed images suggestive of non-functional status of the kidney (Fig. 1). The patient was referred to our department of nuclear medicine for 18F FDG PET CT for staging of disease. The 18F FDG PET CT (Fig. 2) showed FDG avid ill-defined large mass (~ 14.8 × 18.7 × 20.6 cm, SUVmax 17.6) arising from the right kidney abutting the liver with anterior displacement, medially it is crossing the midline abutting the aorta, corresponding renal vein superior mesenteric and inferior mesenteric artery, posteriorly extending up to posterior abdominal wall and anteriorly abutting antro-pylori region of stomach, duodenum and pancreatic head. Multiple FDG avid lytic lesions were noted in the sternum (~ SUVmax 4.2), multiple ribs bilaterally, bilateral scapulae, multiple vertebrae, sacrum, bilateral pelvic bone, bilateral humeri and femora. FDG avid discrete pleural deposits (~ SUVmax 4.1) were noted in bilateral lungs. The histopathology of the renal mass was done and it showed sheets of monomorphous population of tumour cells which were small to medium in size with amounts of eosinophilic cytoplasm, round nuclei and fine granular chromatin. Immunohistochemistry markers including NFX-2.2, FLI-1, CD-99, Synaptophysin were positive (Fig. 3) and Ki 67 proliferation index was 70–80%. The histopathological findings were consistent with Ewing’s sarcoma.
A represents the maximum intensity projection image of PET/CT scan showing a large area of tracer uptake in the right side of abdomen with focal tracer uptake in bilateral thoracic region and multiple areas in visualized axial and appendicular skeleton. B and C reveal the axial and coronal PET/CT and corresponding CT image showing enlarged right kidney with lobulated large mass with necrotic areas showing increased FDG uptake in the PET. D PET/CT and corresponding CT showing FDG avid lytic lesions in sternum, multiple cervical and dorsolumbar vertebrae. E arrows represent FDG avid bilateral pleural deposits with right pleural effusion. F arrows represent FDG avid retroperitoneal lymph nodes
As the histopathological findings were suggestive of Ewing’s Sarcoma, the patient’s treatment changed from surgical management (as previously planned) to medical management. However, the patient succumbed to the disease before treatment could be initiated.
Discussion
Ewing’s sarcoma rarely presents as primary kidney tumor [4]. The clinical features are usually non-specific such as flank or abdominal pain, hematuria or palpable mass. No specific features are seen in imaging and thus it is impossible to differentiate renal Ewing’s from much more prevalent RCC by imaging alone. RCC and sarcomas can have a similar heterogeneous appearance with areas of necrosis, hemorrhage, and calcification. [5]. Primary renal sarcomas are diagnosed on imaging only after exclusion of renal metastatic involvement from a primary sarcoma, secondary renal involvement from a retroperitoneal sarcoma, and ruling out sarcomatoid renal cell carcinoma. However, definitive diagnosis of renal Ewing’s is solely by post- or pre-operative biopsy [6].
Ewing’s sarcoma being the aggressive tumor with chances of early metastasis and can have bone, liver and lung metastasis along with lymph nodal metastasis at time of diagnosis [7].
18F FDG PET/CT has shown to help to localize the primary sarcoma, its extension, metastasis specially the bony and pulmonary metastasis and to check the response to standard treatment available [8]. It also allows the detection of progression or regression and recurrence of disease prior to anatomic imaging [8, 9].
Conventional imaging can assess the local resectability of tumor, however for distant metastasis, conventional imaging (including CT, MRI etc.) can diagnose only 70% of the cases [10]. Thus PET/CT helps in detection of disease involvement of tissue even before the anatomical changes occurs. The PET/CT has 63–8% sensitivity and 75–100% specificity for detecting metastasis and recurrence in renal tumors. These findings are similar for different variants of renal tumor. The patients with localized disease have a 5-year disease free survival rate of about 45–55% [11]; however the prognosis is even worse in patients with metastatic disease, with overall cure rate of 20% only. The main challenge is the proper diagnosis and timely management.
Conclusions
Primary renal Ewing’s sarcoma is rare disease in adults which can be kept as primary differentials. Because of non-specific clinical features, it is difficult to differentiate Ewing’s sarcoma from RCC on imaging. Patients usually present with bone, liver and lung metastasis along with lymph nodal metastasis at time of diagnosis. The final diagnosis is made by histopathology and immunohistochemistry. The 18F FDG-PET/ CT can be used for evaluating the primary, metastatic disease, and in evaluating response to the chemotherapy.
Availability of data and materials
The dataset used and/or analysed during the current study available from the corresponding author on the reasonable request.
Abbreviations
- RCC:
-
Renal cell carcinoma
- CECT:
-
Contrast enhanced computer tomography
- FDG:
-
Fluorodeoxyglucose
- PET/CTP:
-
Positron emission tomography–computed tomography
References
Babapour S, Mohseni I, Piri R, Basi A (2020) Left renal Ewing’s sarcoma: a case study and a review of imaging literature. Radiol Case Rep 15(4):391–395. https://doi.org/10.1016/j.radcr.2020.01.010
Bing Z, Zhang P, Tomaszewski JE, Maclennan GT (2009) Primary Ewing sarcoma/primitive neuroectodermal tumor of the kidney. J Urol 181(3):1341–1342. https://doi.org/10.1016/j.juro.2008.12.029
Zhang S, Li Y, Wang R, Song B (2019) Ewing’s sarcoma/primitive neuroectodermal tumor of the kidney: a case report and literature review. Transl Androl Urol 8(5):562–566. https://doi.org/10.21037/tau.2019.09.46
Tarek N, Said R, Andersen CR, Suki TS, Foglesong J, Herzog CE, Tannir NM, Patel S, Ratan R, Ludwig JA, Daw NC (2020) Primary Ewing Sarcoma/primitive neuroectodermal tumor of the kidney: the MD Anderson cancer center experience. Cancers 12(10):2927. https://doi.org/10.3390/cancers12102927
Risi E, Iacovelli R, Altavilla A, Alesini D, Palazzo A, Mosillo C, Trenta P, Cortesi E (2013) Clinical and pathological features of primary neuroectodermal tumor/Ewing sarcoma of the kidney. Urology 82(2):382–386. https://doi.org/10.1016/j.urology.2013.04.015
Choudhury AR, Jain SG, Reghunath A et al (2022) Primary Ewing’s sarcoma of the kidney: a rare masquerader of renal cell carcinoma on imaging. Egypt J Radiol Nucl Med 53:53. https://doi.org/10.1186/s43055-022-00718-y
Ellinger J, Bastian PJ, Hauser S, Biermann K, Müller SC (2006) Primitive neuroectodermal tumor: rare, highly aggressive differential diagnosis in urologic malignancies. Urology 68(2):257–262. https://doi.org/10.1016/j.urology.2006.02.037
Seth N, Seth I, Bulloch G, Siu AHY, Guo A, Chatterjee R, MacManus M, Donnan L (2022) 18F-FDG PET and PET/CT as a diagnostic method for Ewing sarcoma: a systematic review and meta-analysis. Pediatr Blood Cancer 69(3):e29415. https://doi.org/10.1002/pbc.29415
Huang T, Li F, Yan Z, Ma Y, Xiong F, Cai X, Zhang Q, Liu F, Dong J (2018) Effectiveness of 18F-FDG PET/CT in the diagnosis, staging and recurrence monitoring of Ewing sarcoma family of tumors: a meta-analysis of 23 studies. Medicine 97(48):e13457. https://doi.org/10.1097/MD.0000000000013457
Ozturk H (2015) Peripheral neuroectodermal tumour of the kidney (Ewing’s sarcoma): restaging with (18)F-fluorodeoxyglucose (FDG)-PET/CT. Can Urol Assoc J 9(1–2):E39-44. https://doi.org/10.5489/cuaj.2286
Angel JR, Alfred A, Sakhuja A, Sells RE, Zechlinski JJ (2010) Ewing’s sarcoma of the kidney. Int J Clin Oncol 15(3):314–318. https://doi.org/10.1007/s10147-010-0042-0
Acknowledgements
Not Applicable
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written consent to participate.
Consent for publication
Written consent for publication from study participant.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Singh, M.M., Verma, S., Kakkar, L. et al. Ewing’s sarcoma of the right kidney with multiple metastasis on PET/CT. Egypt J Radiol Nucl Med 54, 2 (2023). https://doi.org/10.1186/s43055-022-00953-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00953-3