Abstract
Background
Polycystic ovary syndrome (PCOS) is the most common endocrinologic disorder in reproductive age. Diagnosis is based on clinical, laboratory, and ultrasonography findings. However, the application of ultrasound for the diagnosis of PCOS in overweight and sexually inactive patients may be limited. The purpose of this study was to display the imaging characteristics of intravoxel incoherent motion (IVIM) magnetic resonance imaging (MRI)-derived parameters as Dtrue (slow diffusion coefficient), D* (perfusion-related diffusion), f (perfusion fraction), and apparent diffusion coefficient (ADC) in PCOS.
Results
A total of 43 women, 20 with PCOS (mean age, 24.09 ± 3.92 years) and 23 healthy control (mean age, 23 ± 1.67 years), were included. IVIM MRI-derived parameters of the ovarian stroma were measured by two observers. Mean D* and f values were found to be higher in PCOS patients than in individuals in the control group (p = 0.011 and p = 0.004, respectively). The ADC value was found to be significantly lower in the patient group (p = 0.003). There was no statistically significant difference between two groups in Dtrue (p = 0.742). The interclass correlation analysis of two observers for both groups showed a good-to-excellent agreement. The ROC produced an AUC of 0.521, a sensitivity of 50%, a specificity of 57%, and a cut-off value of 1.48 × 10−3 mm2/s for Dtrue; an AUC of 0.769, a sensitivity of 55%, a specificity of 67%, and a cut-off value of 22.25 × 10−3 mm2/s for D*; an AUC of 0.734, a sensitivity of 55%, a specificity of 62%, and a cut-off value of 20.87% for f; an AUC of 0.893, a sensitivity of 90%, a specificity of 33%, and a cut-off value of 1.37 × 10−3 mm2/s for ADC.
Conclusions
IVIM MRI would be an alternative imaging tool in the diagnosis of PCOS with a good-to-excellent agreement and with acceptable sensitivity and specificity.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Polycystic ovary syndrome (PCOS) is one of the most commonly seen endocrinologic disorders, with a prevalence of 6%–15% in reproductive age[1]. Although the etiology of PCOS is not clarified, it is accepted as a multifactorial with several genetic, metabolic, and endocrine disorders [1]. The defect in secretion or action of the follicle-stimulating hormone (FSH) pathway is suggested to be the reason for impaired dominant follicle selection (1). Furthermore, hypothalamic-pituitary-gonadotropin imbalance causing more remarkable luteinizing hormone (LH) pulse amplitude and frequency lead to an altered LH / FSH ratio that results in follicular arrest [1]. PCOS is suggested to be associated with infertility, psychiatric disorders, and metabolic diseases [2]. Thus, an accurate and certain diagnosis is essential.
PCOS has been defined as a condition of ovulatory disorder, hyperandrogenism, and polycystic appearance of ovaries on ultrasound in a consensus of the Rotterdam ESHRE/ASRM, 2003 [3]. For the diagnosis, 2 of 3 criteria are required with the elimination of other etiologies. Among these three criteria, ultrasonographic evaluation (12 or more follicles with 2–9 mm in diameter per ovary) and/or increase in ovarian volume (larger than 10 ml) is the most challenging component of the diagnosis [4]. Recommendation of ultrasonographic assessment of ovaries based on transvaginal approach [5, 6]. However, the transvaginal approach is contraindicated in virgin patients [5, 6]. And also, it has limited visualization of the ovaries because of the abdominal fat in overweighted patients [5]. Magnetic resonance imaging (MRI) demonstrated that ovarian morphology would be evaluated accurately and offered to be an alternative technique to ultrasound in overweighted and virgin patients [6,7,8,9]. In a study by Yoo et al., MRI is suggested to provide an increased spatial resolution of ovarian morphology with a higher follicle number than that revealed by transabdominal ultrasound [8]. However, functional MRI has not been applied yet. A noninvasive imaging technique not only for characterizing ovarian morphology but also for providing physiological information without using contrast agents is needed for diagnosis or monitoring the response to therapy.
Intravoxel incoherent motion (IVIM) MRI is a noninvasive modality that evaluates the tissue diffusion and microcapillary perfusion in separate calculations by a biexponential equation as distinct from diffusion-weighted imaging (DWI), which uses a monoexponential equation [9, 10]. In IVIM MRI, three additional parameters as true or slow diffusion coefficient, perfusion-related (pseudo or rapid) diffusion, and perfusion fraction (f) can be measured [9, 11,12,13]. It has been widely applied in liver pathologies, including hepatosteatosis, liver fibrosis, or in various malignancies such as ovarian, cervical, and breast carcinomas in recent years [14, 15]. As far as we know, IVIM MRI in the assessment of PCOS has not been performed yet. This study aimed to assess IVIM MRI-derived parameters in PCOS and to evaluate the IVIM MRI as a new diagnostic approach.
Methods
Subjects
Ethical approval of this prospective study was obtained from the Ethical Committee of the university hospital, and written informed consent was obtained.
A total of twenty patients who were diagnosed with PCOS according to the revised consensus on diagnostic criteria [3, 4] by a ten years experienced gynecologist and endocrinologist and twenty-three healthy volunteers were included in this study between January 2019 and October 2020. The diagnosis of PCOS was performed according to the presence two criteria of three of the following: (1) ovarian dysfunction (oligo- or anovulation), (2) clinical and/or biochemical signs of hyperandrogenism, and (3) polycystic ovaries (presence of 12 or more follicles in each ovary measuring 2–9 mm) [3, 4].
The inclusion criteria were patients with 17 and 38 years of age. The exclusion criteria were the individuals with any endocrine (diabetes mellitus, hypothyroidism, hyperthyroidism, hyperprolactinemia, adrenal enzyme abnormality, etc.), systemic, and neoplastic disorders were excluded. The patients had ovarian cyst (larger than 3 cm) on transabdominal ultrasound. The patients who had claustrophobia and metallic implants /implantable devices contraindicated to MRI were also excluded.
Demographic and clinical data, including luteinizing hormone (LH), follicle-stimulating hormone (FSH), dehydroepiandrosterone, and dehydroepiandrosterone sulfate (DHEA), free testosterone, free T4, thyroid-stimulating hormone (TSH), glucose, insulin resistance, LH / FSH ratio, were retrieved from the data system.
Transabdominal ultrasound and pelvic MRI were obtained within the first week following the menstruation for all individuals in the control and patient groups. All transabdominal ultrasound evaluations were performed with an Aplio 500 ultrasound system machine (Toshiba Medical Systems, Tokyo, Japan) and a 9 MHz frequency convex array transducer by ten years experienced radiologist.
IVIM MRI examination and analysis
All MRIs were performed on a 1.5 T magnet field scanner (450 W; General Electric Medical Systems, Waukesha, Wisconsin, USA) with a 32-channel phased-array abdominal coil without contrast agent administration. Pelvic images were obtained in the axial plane using a 15 to 20 s breath-hold T2 weighted image and IVIM MRI sequence. Imaging parameters of the T2 weighted images sequence were applied as follows; repetition time 3.1 ms; the echo time 1 ms; flip-angle 58°; bandwidth ± 108 kHz; matrix 192 × 228; FOV 380 mm; the number of excitations 1; slice thickness 5 mm; gap 1 mm. Ten (10) b values (0, 10, 20, 30, 50, 80, 100, 200, 400, 800 s/mm2) were applied during the IVIM MRI sequence. The other parameters were as follows; repetition time 4.2 ms; the echo time 1.4–11 ms; flip-angle 35°; bandwidth ± 55 kHz; matrix 320 × 198; FOV 345 mm; Number of excitations 1; slice thickness 5 mm; gap 1 mm. The average scan time was 5–10 min for T2 weighted image and 5–10 min for IVIM MRI sequence.
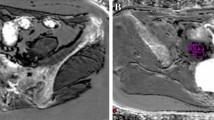
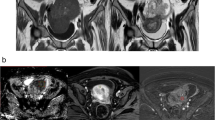
All the MRI examinations were assessed by two radiologists with at least 8 years of experience blinded to patient information. IVIM MRI images were automatically processed on the device, and IVIM MRI-derived parameters [Dtrue, D*, f, and apparent diffusion coefficient (ADC) maps] were produced. All the measurements were performed on a workstation (Advantage Workstation, General Electric Medical Systems, Waukesha, Wisconsin, USA). During the evaluation, an axial T2 weighted image was used to differentiate ovarian stroma from follicles to evaluate the number of ovarian follicles and ovarian volume (Fig. 1). Copied two round regions of interest (ROI) with 2–3 mm2 were placed manually within each ovarian stroma in the IVIM MRI sequence (Fig. 1). The mean Dtrue, D*, f, and ADC values were calculated by averaging the four measurements (two ROIs for left and two ROIs for right ovaries) for both observers. The mean values of IVIM MRI-derived parameters were recorded as average measurements of both observers.
a 20-year-old girl with polycystic ovary syndrome. a–c Axial T2 weighted images (fast imaging employing steady-state acquisition) sequence shows peripheral ovarian follicle and central stoma in the left ovary (a), two regions of interest (ROI) replaced in the ovarian stroma in a single-shot echo-planar diffusion-weighted image (b = 800 s/mm2) (b) and apparent diffusion coefficient (ADC) map (mm.2/s (c), corresponding IVIM MRI sequence that used for derived parameters (d)
Diffusion-weighted and intravoxel incoherent motion magnetic resonance imaging
DWI is a single-shot echoplanar imaging sequence with a long time to echo value with a motion-probing gradient pulse used to reduce the signal intensity of moving water molecules [16].
The magnitude of the water diffusion was described by the ADC. S0 is the baseline signal intensity (b = 0) recorded before the image acquisition, and the Sb is a signal intensity at a prescribed b value. Therefore, the signal intensity of different tissue decreases at different rates defined by their baseline signal intensity, ADC, and the b values [16]. IVIM MRI sequence is established on a bi-compartment model, which was first presented by Le Bihan et al. [9, 11]. According to this model, the increased signal in DWI was originated from the motion of water molecules in different compartments such as extracellular, intracellular, and intravascular space or perfusion [17]. Differentiating the motion of water molecules in intravascular space from diffusion in the extravascular space is presented by the methodology of IVIM imaging [16]. Sb is the signal at a diffusion weighting with a specific b value, and S0 is the signal intensity at baseline.
Dtrue showed the apparent diffusivity of water and is affected by an increment of density in cellular structure [9, 18, 19]. D* or pseudo-diffusion coefficient indicates intravascular blood flow velocity and perfusion fraction (f) shows blood volume, which reflects the capillary perfusion [19]. Thus, a lower D* or f value indicates impaired capillary perfusion. In lower b-values, the intravoxel spin dephasing caused by the pseudorandom blood flow in the presence of diffusion gradient will promote more signal attenuation. During the following phase of the signal decay, the attenuation was mainly the result of the diffusion of water molecules because the blood signal would be suppressed to the higher diffusion gradients [20].
Statistical analysis
Normally distributed data are described as mean ± SD. Non-normally distributed data (free testosterone, free T4, and TSH) are presented as medians with interquartile range (interquartile range, IQR 25–75). Differences between two groups in IVIM MRI-derived parameters and laboratory findings were evaluated using an independent sample t test or Mann–Whitney U test. Laboratory findings were assessed with respect to IVIM-derived parameters using the Pearson or the Spearman correlation tests. All variables were analyzed for normality using Shapiro–Wilk tests, and a p-value of < 0.05 was considered a statistically significant difference. Statistical analyses were done using SPSS (SPSS 20, Chicago, Illinois, USA).
Interclass correlation coefficient (ICC) was assessed by a two-way mixed model. Both observers measured at 2 points of each ovary (4 ROI measurements for each patient). ICC (95% confidence interval [CI]) values of average measurements were obtained by the mean rating of 2 measurements for each observer. An ICC coefficient value higher than 0.8 indicates excellent agreement, 0.8–0.6 substantial agreement, 0.6–0.4 moderate agreement, and lower than 0.4 poor agreement [21]. Receiver operating characteristic (ROC) curve analyses were performed to determine the optimal cut-off values for each covariate (D, D*, f, and ADC).
Results
A total of 43 females, 20 patients diagnosed with PCOS, and 23 healthy controls, were included in this study. There was no significant difference between the two groups in terms of the patient age: 24.09 ± 3.92 years (ranges: 18–31 years) vs. 23 ± 1.67 years (ranges: 21–26 years) (p = 0.239). Body mass index was higher in patient group (28.41 ± 7.14 vs.22.14 ± 2.69 kg/m2, p = 0.001). Demographic details with blood tests and ovarian morphologic characteristics are provided (Table 1). Blood tests showed PCOS patients had increased hormone levels compared to the control group. LH, DHEAS, free testosterone, TSH, insulin resistance and LH/FSH ratio were significantly higher in PCOS patients compared with the control group (p = 0.008, p < 0.0001, p < 0.0001, p = 0.048, p = 0.018, p = 0.013, respectively). There was no significant difference between the two groups in terms of the FSH, free T4, and glucose (p = 0.873, p = 613, and p = 605, respectively). The mean follicle count and ovarian volume for single ovary were calculated as 20.84 ± 3.61 and 13.41 ± 3.15 cm3 in PCOS group and 7.97 ± 2.82 and 8.05 ± 2.20 cm3 in control group (p < 0.0001, p < 0.0001, respectively).
The mean D* and f values in patient group (patient group: D*; 27.88 ± 9.21 × 10 − 3 10−3 mm2/s, f; 23.15 ± 3.56%, control group: D*; 19.85 ± 10.52 × 10−3 mm2/s, f; 18,74 ± 5,61%) were significantly higher (p = 0.011 and p = 0.004, respectively). The ADC value was significantly lower in patient group compared to the control group (ADC; 1.23 ± 0.26 × 10 − 3 mm2/s, ADC; 1.42 ± 0.06 × 10−3 mm2/s, p = 0.003). There was no statistically significant difference in terms of Dtrue (p = 0.742). IVIM MRI-derived parameters of bilateral ovaries in PCOS patients and controls are shown in Table 1. There was no statistically significant correlation between laboratory findings and IVIM MRI parameters in both groups (Table 2).
The interclass correlation analysis of two observers for both groups showed a good-to-excellent agreement for Dtrue, D*, f, ADC values (Table 3). The interobserver agreement was for Dtrue: 0.844 (95% CI = 0.612–0.938), for D*: 0.891 (95% CI = 0.725–0.957), for f: 0.711 (95% CI = 0.257–0.887), for ADC: 0.820(95% CI = 0.583–0.923) in PCOS group, respectively. And also the interobserver agreement was for Dtrue: 0.907 (95% CI = 0.780–0.961), for D*: 0.915 (95% CI = 0.798–0.964), for f: 0.964 (95% CI = 0.915–0.985), for ADC: 0.853 (95% CI = − 0.139–0.967) in control group, respectively.
ROC curves were developed for each covariate (D, D*, f, ADC) (Table 4). The ROC produced an AUC of 0.521 (ranges, 0.341–0.701), a sensitivity of 50%, a specificity of 57%, and a cut-off value of 1.48 × 10−3 mm2/s for Dtrue; an AUC of 0.769 (ranges, 0.625–0.914), a sensitivity of 55%, a specificity of 67%, and a cut-off value of 22.25 × 10−3 mm2/s for D*; an AUC of 0.734 (ranges, 0.584–0.896), a sensitivity of 55%, a specificity of 62%, and a cut-off value of 20.87% for f; an AUC of 0.893 (ranges, 0.774–1.013), a sensitivity of 90%, a specificity of 33%, and a cut-off value of 1.37 × 10−3 mm2/s for ADC. Positive and negative predictive values are 53% and 58% for Dtrue, 61% and 64% for D*, 58% and 63% for f, 62% and 86% for ADC, respectively.
Discussion
DW-MRI and ADC values are mentioned to have the potential of imaging biomarkers in Diffusion-Weighted Magnetic Resonance Imaging as a Cancer Biomarker: Consensus and Recommendations, 2009 [22]. Monoexponential DWI has been applied in various ovarian pathology, including ovarian tumors [23,24,25]. ADC measurement in gynecological disorders has been usually performed either in the evaluation of malignant tumors or in response to therapy. However, ADC assessment of PCOS is scarce [26, 27]. The study by Samancı et al. assessed ovarian stroma by monoexponential DWI and demonstrated significantly lower stromal ADC values in PCOS patients [27]. Similar findings were also revealed in a study by Deveer et al. [26]. In concordance with the results of the study by Deveer et al. and Samancı et al. [26, 27], we found decreased stromal ADC value in PCOS patients.
Decreased ADC values in malignant tumors are suggested to be related to a combination of increased cellularity and higher extracellular space tortuosity, all contributing to the reduced motion of water [23]. It is suggested that decreased ADC value is associated with increased stromal collagen and vascular endothelial growth factor (VEGF), which plays an important role in the neovasculature formation in tumor stroma [28]. Ma et al. also observed significant negative correlations of ADC with the VEGF expression and grade in prostate cancer [29]. Huang et al. also found a negative correlation between VEGF expression and the ADC values of hepatocellular carcinoma [30]. In another study, it was demonstrated that the diffusion of water molecules is also restricted by extracellular components, such as collagen fibers and extracellular matrix [31]. On the other hand, overexpressed VEGF, which is linked to increased permeability of thecal blood vessels, angiogenesis, and connective tissue stroma generation in the ovarian stroma of PCOS, has been reported [32]. Moreover, Papachroni et al. revealed that increased distribution of collagen type IV in the polycystic ovary tissue induces cystogenesis [33]. The main principle of the monoexponential model of DWI is the quantification of Brownian motion which reflects the diffusion motion of water molecules in tissues [34]. In this model, obtained ADC information reflects both diffusion motion of water molecules and capillary perfusion of the microcirculatory network [10, 34,35,36]. This limitation could be overcome by the IVIM MRI, which separates molecular diffusion and microcirculatory perfusion-related diffusion, assessing the motion of the water in non-exchanging intravascular and extravascular compartments [10]. In IVIM MRI, both D* and f reflect the perfusion in the capillary network and the blood volume in the tissue. A diminished D* or f value is meaningful for diminished capillary perfusion and blood volume [11, 37]. In our study, we revealed higher D*, f with reduced ADC values in patients with PCOS than healthy controls. However, we found no significant difference between patient and control groups in comparison with Dtrue. Although we did not assess the cellular mechanism of PCOS, we suggest that decreased ADC values with increased IVIM MRI-derived perfusion parameters (D* and f values) would be explained increased extracellular matrix, angiogenesis, and vascularization. This was also mentioned in various Doppler ultrasound studies performed on PCOS patients [38,39,40]. Battaglia et al. showed increased vascularization and high pulsatility index with a typical decreased resistive index in the ovarian stroma [39]. Lam et al. also demonstrated lower resistive index and pulsatility index in two-dimensional Doppler and higher vascularization flow index and vascularization index in three-dimensional power Doppler in patients with PCOS [40]. Our study is the only study that assessed IVIM MRI-derived parameters in patients with PCOS. Moreover, Panchal et al. [41] suggested that elevated LH level increases stromal vascularization by stimulating neoangiogenesis in patients with PCOS. Increased ovarian fibrosis was demonstrated in androgen-induced PCOS rats [42]. Cıracı et al. [43] also showed the increased stromal stiffness by real-time ultrasound elastography in patients with PCOS. In this study, they found an increased strain ratio which showed moderate positive correlations with ovarian volume and follicle count. However, we found no significant difference in terms of Dtrue between the two groups. In liver fibrosis, decreased Dtrue value with perfusion parameters (D* and f values) was found compared to the healthy liver, which is negatively correlated with the severity of hepatic fibrosis [44, 45]. However, they found no significant difference in terms of Dtrue in further studies [20, 46]. The result of our study may be caused by the variation of the disease, such as the peripheral or general cystic patterns of PCOS and different ages of fibrosis. Differences in treatment, complex and multifactorial pathogenesis (polycystic ovarian morphology, hyperandrogenemia, insulin resistance, obesity, etc.) suggest the multifactorial nature, including genetic, environmental components, and heterogeneity of the syndrome [47].
The main advantages of the technique are to be noninvasive, are not requiring contrast agents and ionizing radiation, and provide quantitative information, fast and easy to performance into routine practice. In recent years, ovarian morphology has been increasingly evaluated by MRI in several studies [7, 9, 48]. MRI has an advantage for imaging ovaries with high-contrast resolution in adolescents and obese women. Although perfusion MRI was not studied in patients with PCOS, it is mentioned that DWI and MRI perfusion have approximately the same sensitivity and positive impact on operative management [49]. Further studies comparing IVIM MRI-derived perfusion and diffusion parameters with either histopathological findings of perfusion MRI will be useful for elucidating the hypothesis underlying the pathogenesis. Additionally, compared IVIM MRI studies that assess the response to the therapy are required.
Our study has some limitations, including a small sample size and a lack of correlation between IVIM MRI-derived parameters and the factors that play a role in the PCOS mechanism. And also, we did not assess the IVIM MRI-derived parameters of the ovarian stroma in PCOS patients in response to the various treatments. Moreover, the IVIM DWI has its own limitations. Scanner and field intensities, physiological activities of the tissue [50], and motion artifacts may affect the result. Lack of consensus on the number and distribution of b values is the other limitation of the DWI and IVIM MRI techniques. To overcome these limitations, the measurement was revealed from the mean of four ROI values for each observer. Further research correlated with the factors that play a role in the mechanism of PCOS in a larger cohort is required.
Conclusions
In conclusions, our study results showed that values of IVIM-derived parameters of the ovarian stroma are higher in patients with PCOS than in control subjects. IVIM MRI may be a useful imaging tool in diagnosis of PCOS with a good-to-excellent agreement and with an acceptable sensitivity and specificity. It can be revealed routinely and safely without radiation exposure and using a contrast agent. IVIM MRI would be added to image ovaries especially in overweighted and virgin patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MRI:
-
Magnetic resonance imaging
- IVIM:
-
Intravoxel incoherent motion
- PCOS:
-
Polycystic ovary syndrome
- LH:
-
Luteinizing hormone
- FSH:
-
Follicle-stimulating hormone
- DHEA:
-
Dehydroepiandrosterone and dehydroepiandrosterone sulfate
- TSH:
-
Thyroid-stimulating hormone
- D :
-
True diffusion or slow diffusion coefficient
- D*:
-
Pseudo-diffusion or fast diffusion coefficient
- f :
-
Perfusion fraction
- ADC:
-
Apparent diffusion coefficient
- ICC:
-
Interclass correlation coefficient
- ROC:
-
Receiver operating characteristic
References
Rosenfield RL, Ehrmann DA (2016) The Pathogenesis of Polycystic Ovary Syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism. Revisit Endocr Rev 37:467–520
Dumesic DA, Oberfield SE, Stener-Victorin E et al (2015) Scientific statement on the diagnostic criteria, epidemiology, pathophysiology, and molecular genetics of polycystic ovary syndrome. Endocr Rev 36:487–525
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group Revised (2003) Consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril 2004(81):19–25
Dewailly D, Lujan ME, Carmina E et al (2014) Definition and significance of polycystic ovarian morphology: a task force report from the Androgen Excess and Polycystic Ovary Syndrome. Soc Hum Reprod Update 20:334–352
Barber TM, McCarthy MI, Wass JA et al (2006) Obesity and polycystic ovary syndrome. Clin Endocrinol (Oxf) 65:137–145
Barber TM, Alvey C, Greenslade T et al (2010) Patterns of ovarian morphology in polycystic ovary syndrome: a study utilising magnetic resonance imaging. Eur Radiol 20:1207–1213
Nylander M, Frøssing S, Bjerre AH et al (2017) Ovarian morphology in polycystic ovary syndrome: estimates from 2D and 3D ultrasound and magnetic resonance imaging and their correlation to anti-Müllerian hormone. Acta Radiol 58:997–1004
Yoo RY, Sirlin CB, Gottschalk M et al (2005) Ovarian imaging by magnetic resonance in obese adolescent girls with polycystic ovary syndrome: a pilot study. Fertil Steril 84:985–995
Le Bihan D, Breton E, Lallemand D et al (1988) Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology 168:497–505
Koh DM, Collins DJ, Orton MR (2011) Intravoxel incoherent motion in body diffusion-weighted MRI: reality and challenges. AJR Am J Roentgenol 196:1351–1361
Le Bihan D, Breton E, Lallemand D et al (1986) MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology 161:401–407
Le Bihan D, Turner R (1992) The capillary network: a link between IVIM and classical perfusion. Magn Reson Med 27:171–178
Le Bihan D, Turner R, Moonen CT et al (1991) Imaging of diffusion and microcirculation with gradient sensitization: design, strategy, and significance. J Magn Reson Imaging 1:7–28
Tao YY, Zhou Y, Wang R et al (2020) Progress of intravoxel incoherent motion diffusion-weighted imaging in liver diseases. World J Clin Cases 8:3164–3176
Manoharan D, Das CJ, Aggarwal A et al (2016) Diffusion weighted imaging in gynecological malignancies—present and future. World J Radiol 8:288–297
Mannelli L, Nougaret S, Vargas HA et al (2015) Advances in diffusion-weighted imaging. Radiol Clin N Am 53:569–581
Dixon WT (1988) Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging: a modest proposal with tremendous potential. Radiology 168:566–567
Le Bihan D (1988) Intravoxel incoherent motion imaging using steady-state free precession. Magn Reson Med 7:346–351
Luciani A, Vignaud A, Cavet M et al (2008) Liver cirrhosis: intravoxel incoherent motion MR imaging-pilot study. Radiology 249:891–899
Lautt WW (1977) Hepatic vasculature: a conceptual review. Gastroenterology 73:1163–1169
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Padhani AR, Liu G, Koh DM et al (2009) Diffusion-weighted magnetic resonance imaging as a cancer biomarker: consensus and recommendations. Neoplasia 11:102–125
He M, Song Y, Li H et al (2020) Histogram analysis comparison of monoexponential, advanced diffusion-weighted imaging, and dynamic contrast-enhanced MRI for differentiating borderline from malignant epithelial ovarian tumors. J Magn Reson Imaging 52:257–268
Xiao Z, Tang Z, Zhang J et al (2020) Whole-tumor histogram analysis of monoexponential and advanced diffusion-weighted imaging for sinonasal malignant tumors: correlations with histopathologic features. J Magn Reson Imaging 51:273–285
Ding Y, Tan Q, Mao W et al (2019) Differentiating between malignant and benign renal tumors: Do IVIM and diffusion kurtosis imaging perform better than DWI? Eur Radiol 29:6930–6939
Deveer M, Deveer R, Cullu N et al. The added value of diffusion-weighted MRI in diagnosis of polycystic ovary syndrome: a preliminary study. Eur Congr Radiol ECR. https://doi.org/10.1594/ecr2016/B-1326
Samanci C, Alis D, Ustabasioglu FE et al (2017) Apparent diffusion coefficient measurement of ovarian stroma: a potential tool for the diagnosis of polycystic ovary syndrome. Diagn Interv Imaging 98:57–61
Aoyagi T, Shuto K, Okazumi S et al (2012) Apparent diffusion coefficient correlation with oesophageal tumour stroma and angiogenesis. Eur Radiol 22:1172–1177
Ma T, Yang S, Jing H et al (2018) Apparent diffusion coefficients in prostate cancer: correlation with molecular markers Ki-67, HIF-1α and VEGF. NMR Biomed. https://doi.org/10.1002/nbm.3884
Huang Z, Meng X, Xiu J et al (2014) MR imaging in hepatocellular carcinoma: correlations between MRI features and molecular marker VEGF. Med Oncol 31:313
Hauge A, Wegner CS, Gaustad JV et al (2017) Diffusion-weighted MRI-derived ADC values reflect collagen I content in PDX models of uterine cervical cancer. Oncotarget 8:105682–105691
Kamat BR, Brown LF, Manseau EJ et al (1995) Expression of vascular permeability factor/vascular endothelial growth factor by human granulosa and theca lutein cells. Role in corpus luteum development. Am J Pathol 146:157–165
Papachroni KK, Piperi C, Levidou G et al (2010) Lysyl oxidase interacts with AGE signalling to modulate collagen synthesis in polycystic ovarian tissue. J Cell Mol Med 14:2460–2469
Taouli B, Koh DM (2010) Diffusion-weighted MR imaging of the liver. Radiology 254:47–66
Bammer R (2003) Basic principles of diffusion-weighted imaging. Eur J Radiol 45:169–184
Lewis S, Dyvorne H, Cui Y et al (2014) Diffusion-weighted imaging of the liver: techniques and applications. Magn Reson Imaging Clin N Am 22:373–395
Wolff D, van Melle JP, Dijkstra H et al (2016) The Fontan circulation and the liver: a magnetic resonance diffusion-weighted imaging study. Int J Cardiol 1(202):595–600
Bozkurt M, Kara Bozkurt D, Kurban D et al (2021) 2-D and 3-D ultrasonographic characteristics of the ovary in women with PCOS and multifollicular ovaries. J Obstet Gynaecol 41:920–926
Battaglia C, Artini PG, D’Ambrogio G et al (1995) The role of color Doppler imaging in the diagnosis of polycystic ovary syndrome. Am J Obstet Gynecol 172:108–113
Lam PM, Johnson IR, Raine-Fenning NJ (2007) Three-dimensional ultrasound features of the polycystic ovary and the effect of different phenotypic expressions on these parameters. Hum Reprod 22:3116–3123
Panchal S, Nagori CB (2012) Baseline scan and ultrasound diagnosis of PCOS. Donald School J Ultrasound Obst Gynecol 6:290–299
Wang D, Wang W, Liang Q et al (2018) DHEA-induced ovarian hyperfibrosis is mediated by TGF-β signaling pathway. J Ovarian Res 10(11):6
Cıracı S, Tan S, Özcan AS et al (2015) Contribution of real-time elastography in diagnosis of polycystic ovary syndrome. Diagn Interv Radiol 21:118–122
Chen C, Wang B, Shi D et al (2014) Initial study of biexponential model of intravoxel incoherent motion magnetic resonance imaging in evaluation of the liver fibrosis. Chin Med J 127:3082–3087
Hu G, Chan Q, Quan X et al (2015) Intravoxel incoherent motion MRI evaluation for the staging of liver fibrosis in a rat model. J Magn Reson Imaging 42:331–339
Wu CH, Ho MC, Jeng YM et al (2015) Assessing hepatic fibrosis: comparing the intravoxel incoherent motion in MRI with acoustic radiation force impulse imaging in US. Eur Radiol 25:3552–3559
Hoeger KM, Dokras A, Piltonen T (2021) Update on PCOS: consequences, challenges, and guiding treatment. J Clin Endocrinol Metab 8(106):e1071–e1083
Brown M, Park AS, Shayya RF et al (2013) Ovarian imaging by magnetic resonance in adolescent girls with polycystic ovary syndrome and age-matched controls. J Magn Reson Imaging 38:689–693
El Ameen NF, Eissawy MG, Mohsen LAMS et al (2020) MR diffusion versus MR perfusion in patients with ovarian tumors: How far could we get? Egypt J Radiol Nucl Med 51:35
Neil JJ, Bretthorst GL (1993) On the use of Bayesian probability theory for analysis of exponential decay data: an example taken from intravoxel incoherent motion experiments. Magn Reson Med 29:642–647
Acknowledgements
Not applicable.
Funding
There was no source of funding.
Author information
Authors and Affiliations
Contributions
SO interpreted all images and wrote discussion section. MBD, MH, MS and BC collected data and wrote introduction as well as Material and Method. AA managed this project and edited manuscript. We confirm that all of us as we are the authors accept the manuscript for submission. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been ethically approved by the ethics committee of Istanbul Medeniyet University (ID Number, 2019/0156). Written informed agreement was obtained from all the cases.
Consent for publication
Written consent to publish this information was obtained from study participants, and proof of consent to publish from study participants can be requested at any time.
Competing interests
The authors have no potential conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ozkok, S., Sorkun, M., Dogan, M.B. et al. Intravoxel incoherent motion magnetic resonance imaging and derived parameters in the assessment for polycystic ovary syndrome. Egypt J Radiol Nucl Med 53, 218 (2022). https://doi.org/10.1186/s43055-022-00905-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00905-x