Abstract
High-frequency oscillations (HFOs) in the electroencephalography (EEG) have been extensively investigated as a potential biomarker of epileptogenic zones. The understanding of the role of HFOs in epilepsy has been advanced considerably over the past decade, and the use of scalp EEG facilitates recordings of HFOs. HFOs were initially applied in large scale in epilepsy surgery and are now being utilized in other applications. In this review, we summarize applications of HFOs in 3 subtopics: (1) HFOs as biomarkers to evaluate epilepsy treatment outcome; (2) HFOs as biomarkers to measure seizure propensity; (3) HFOs as biomarkers to reflect the pathological severity of epilepsy. Nevertheless, knowledge regarding the above clinical applications of HFOs remains limited at present. Further validation through prospective studies is required for its reliable application in the clinical management of individual epileptic patients.
Similar content being viewed by others
Background
Epilepsy is a chronic neurological disorder characterized by recurrent episodes of spontaneous seizures, affecting nearly 1–2% of the population of the world [1]. Despite the overall favorable prognosis, only a few patients can achieve seizure freedom and epilepsy is still a high risk factor for premature death in the general population. Different clinical approaches including assessment of epilepsy treatment outcome, understanding of seizure susceptibility, and reflection of the severity of pathological injury collectively guide the selection of early intervention in epileptic patients. However, currently there is a lack of biomarker that can be explicitly used for measuring epilepsy severity and activity. Thus, new biomarkers with defined pathophysiological predictions are urgently needed in clinical practice.
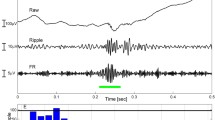
In the past decades, high-frequency oscillations (HFOs), i.e., brain electrical activities at frequencies above 80 Hz, have received much attention. In 1989, Huang and White recorded for the first time high-frequency activities (100–800 Hz) in a metrazol-induced epileptic rat model via subcutaneous needle electrodes [2]. Subsequently, Fisher et al. recorded high-frequency activities in five epileptic patients in 1992 using subdural grid electroencephalography (EEG) [3]. In-depth studies on the relationship between HFOs and epilepsy began in 1999, when recordings using microelectrodes in epileptic rat models and epileptic patients further investigated the mechanisms of HFOs and its relationship with the probable epileptogenic zone (EZ) [4]. Although currently there is no established standard of HFOs, it is generally accepted that HFOs are “spontaneous EEG events (> 80 Hz), having at least four oscillations with sinusoidal-like morphology in the filtered signal (> 80 Hz) with a root mean square amplitude increase of more than 5 times the standard deviation compared to background brain activity” [5]. There are three categories of HFOs based on frequency: ripples (R, 80–250 Hz), fast ripples (FR, 250–500 Hz), and very high-frequency oscillations (> 500 Hz) [6, 7]. HFOs can be detected by scalp electrodes as well as various other intracranial electrodes including microelectrodes with a surface of 0.0013–0.0016 mm2) and macroelectrodes with a surface of 0.5–10.0 mm2.
With subsequent maturity of the technology and more extensive studies in this area, HFOs in EEG are now considered as a potential marker of EZ or seizure onset zone (SOZ) [5, 8]. HFOs are not only detected interictally but can also apparently increase during the preictal or ictal periods [9, 10]. Since invasive intracranial EEG (iEEG) can overcome many physical limits of scalp EEG by recording signals directly from the brain tissue, most insightful findings of HFOs were derived from iEEG in patients with refractory epilepsy, as part of the preoperative evaluation [11]. The electrode contact of iEEG can either be on the cortical surface (electrocorticography, ECoG) or within the cortex and hippocampus. HFOs from ECoG are thought to be novel biomarkers for the localization of epileptic generator [12]. ECoG only detects EEG signals from gyrus surfaces, whereas stereo-electroencephalography (SEEG) is an invasive surgical procedure that enables more accurate neuroelectrophysiological monitoring of deep brain structures [13, 14]. HFOs detected by SEEG are used to identify brain areas from which epileptic seizures originate and enables pre-surgical evaluation [15, 16]. Nevertheless, the scope of iEEG application is greatly limited due to the risks and cost associated with the invasive surgery. In contrast, scalp EEG is widely accepted due to the safety and cost-effectiveness in monitoring the scalp activity of the brain. The recording of HFOs with technical development has unexpectedly revealed high frequencies in the ictal state on scalp EEG recordings [17, 18]. More recent studies have proposed that the scalp EEG can detect both ripples and FR [19,20,21]. Studies have shown that although having small cortical generators, low amplitudes (10–20 μV when measured on the brain surface) and submillimeter and millimeter-scale areas, HFOs are detectable on the scalp with a high signal-to-noise ratio [22, 23]. One additional key issue is that a higher spatial sampling density is necessary for both extracranial and intracranial HFO recordings [24,25,26]. Nonetheless, there are still challenges for detection of scalp HFOs: simultaneous recordings of scalp and intracranial HFOs demonstrated that only 0.1% of intracranial HFOs are visible on scalp EEG recordings [22]. Over the last decade, the clinical applications of HFOs to evaluate epilepsy activity and severity have been investigated [27, 28]. In this review, we discuss the epileptic applications of HFOs by EEG, such as in assessment of treatment outcome, prediction of epileptic seizure and susceptibility to epilepsy, and reflection of pathological severity.
HFOs as a biomarker to evaluate treatment outcome of epilepsy
Evaluating the epilepsy treatment outcome could predict the likelihood of seizure occurrence, and thereby facilitates setting early appropriate interventions to reduce the magnitude and/or frequency of seizures and prevent poor outcomes. Numerous clinical studies and animal experiments using scalp EEG and iEEG have found a strong relationship between HFOs and treatment outcome epilepsy. A study performed simultaneous scalp EEG and iEEG recordings in epilepsy patients and concluded that the widespread HFOs are linked to a poor post-surgical outcome [29]. Evaluation of HFOs before severe seizure attacks enables timely clinical intervention, thereby reducing the seizure recurrence and improving therapy outcomes.
As for pharmacotherapy, either monotherapy (such as levetiracetam, lacosamide and vigabatrin) or mixed anti-epileptic drug (AED) can reduce HFOs [30,31,32,33]. In line with this, a study has reported that HFOs increase with reduction of mixed AEDs as do the seizures, while the spikes are relatively stable [34]. This suggests that HFOs are useful biomarkers for disease activity and more strongly linked to seizures than spikes.
As for surgery, surgical resection of HFO-generating areas led to favorable postoperative seizure freedom [35,36,37]. Wu et al. have reported that intra-operative FR detected in 80% of pediatric epilepsy cases is correlated with the outcome of epilepsy surgery, and complete removal of FR-containing cortex led to postoperative seizure freedom in pediatric patients with mostly extratemporal lesions [38]. Another prospective study in pediatric epilepsy patients showed that incomplete resection of FR-containing cortex predicts postoperative seizures [39]. A retrospective observational study of 123 patients who underwent focal cortical resection indicated that the coupling between high-frequency activities (HFA) and the following slow waves during interictal recording may be a potential predictor for postoperative seizure outcome [40]. Patients with drug-resistant neocortical epilepsy are often faced with greater barriers to localizing epileptogenic focus and making therapeutic plans than those with mesial temporal lobe epilepsy (MTLE) [41]. By retrospectively analyzing ECoG recorded from 54 refractory focal epilepsy patients, van ‘t Klooster and coworkers identified that the specificity of the FR for outcome prediction is better than spikes, and that the post-resection FR may be the strongest predictor for recurrent seizures, especially in patients with a neocortical lesion [42]. In neocortical epilepsy, the resection of brain regions with higher HFO rates in either an interictal [3, 43] or an ictal phase [44, 45] results in post-surgical seizure-free outcomes. The potential value of interictal HFOs deserves special attention, as there is no need to record seizures, which is a time- and labor-consuming process that may increase the risk of complications following secondary generalization after lowering or withdrawal of AEDs.
Secondary epilepsy deriving from multiple clinical disorders with probably different underlying epileptogenic processes, is also related with HFOs in outcomes. Taking tuberous sclerosis complex (TSC) as an example, over 50% of patients with TSC suffer from refractory epilepsy, and epilepsy surgery is frequently used for TSC treatment [46]. TSC is a multisystemic neurocutaneous genetic condition with autosomal dominant inheritance [47]. A study has identified that resection of ictal HFOs can contribute to good surgical outcomes in children with refractory epilepsy secondary to TSC [48].
West syndrome is a severe form of early-onset infantile epilepsy with a high incidence and poor prognosis [49]. The progression and management of West syndrome has been hampered by the lack of reliable prognostic biomarkers until the report of its associations with HFOs both on scalp EEG and iEEG [11, 17, 50, 51]. Kobayashi et al. observed that the scalp HFO rate reduces after the adrenocorticotropic hormone (ACTH) treatment in infants with hypsarrhythmia and West syndrome [52]. A retrospective study in children with West syndrome undergoing short-term drug treatment found that HFOs coupled to 2–3 Hz slow-wave activity increases the seizure incidence in non-refractory epileptic children, compared to those who were refractory [20]. This study also indicated that the HFO rate reduces with drug treatment but shows no difference between responders and non-responders. Iwatani et al. reported that the ictal HFOs on scalp EEG seen during spasms contribute to the identification of EZ in symptomatic West syndrome. In addition, the regions of the maximum augmentation of HFOs at 80–150 Hz are consistent with the neuroimaging findings in 4 children with symptomatic West syndrome, and two of them underwent resection of the area containing HFOs and thus achieved Engel class I [53]. Taken together, for West syndrome, the reduction of HFOs is significantly related to the improvement of treatment outcome, regardless of the medical or surgical intervention. Similar findings have been obtained in a spectrum of pediatric disorders from benign childhood epilepsy with centrotemporal spikes (BECTS) to atypical benign partial epilepsy (ABPE), and to epilepsy with continuous spike-waves during slow-wave sleep (CSWS). A high ratio of ripples per spike has been confirmed in epilepsy with CSWS [21] and the percentage reduction of HFOs after corticosteroids therapy is indicative of a good prognosis [54, 55]. In ABPE, HFOs mirror disease severity and are observed to be more sensitive to methylprednisolone treatment than spikes [56]. Kobayashi et al. proposed that spike-related HFOs in idiopathic partial epilepsy (IPE), including a patient with epilepsy evolving from BECTS to ABPE with CSWS, may indicate whether or not the spikes have a propensity for aggravation [57]. Shibata et al. analyzed spike-associated HFA and its association with spike foci in the EEG of patients with BECTS and Panayiotopoulos syndrome (PS) and found that the proportion of spike-associated HFA was higher in BECTS than in PS [58].
Intractable epilepsy shows a negative impact on the cognitive functioning of children [59, 60]. To investigate the correlation between the number of HFOs and the cognitive outcome, a retrospective study was conducted to analyze the pre-resection ECoG and post-resection ECoG in 20 children with focal refractory epilepsy who received epilepsy surgery [61]. The result showed that HFOs could be used as a biomarker for prediction of cognitive outcome after epilepsy surgery. Similarly, in chronic temporal lobe epilepsy animal models, removal of the FR-generating areas led to the amelioration of cognitive deficits [62]. This evidence supports the predictive potential of HFOs for the cognitive outcome of epilepsy surgery.
In addition, a large number of studies has shown that HFOs correlate with the effect of antiepileptic treatment. It seems that HFOs respond to antiepileptic treatment in a stable and nonspecific manner regardless of the type of treatment. However, a study concluded that tailoring epilepsy surgery can be guided by FRs, but careful assessment of the ECoG is also required, as FR in functionally eloquent areas might not be pathologic [42]. Two meta-analyses based on the existing studies even suggested that the evidence for HFOs as a predictor of surgical outcome is rather weak [63, 64]. In a recent study, the pre-resection of FR-generating regions is not predictive of surgical outcome, while the absence of FR in post-resection ECoG predicted favorable operative outcome [65]. In addition, a prospective multicenter study conducted in chronic SEEG (2 centers) and intra-operative ECoG (1 center) patients showed that prediction is possible at the group rather than the individual level [66]. Consequently, unlike earlier studies, this study inferred that HFOs may be less specific for epileptic tissues. So far, it remains unclear whether HFOs can be utilized to guide treatment or predict the clinical success or failure of therapy, which necessitates the need for more large-scale and longer follow-up studies to assess the reliability of HFOs as a biomarker for outcome prediction.
HFOs as a biomarker to predict seizures and susceptibility to epilepsy
An effective non-invasive biomarker for seizures could identify patients potentially prone to various threats including genetic predisposition and environmental factors [67]. It has been documented that HFOs play a critical role in the prediction of seizures [68].
HFOs could reflect a predisposition to epileptic seizures in animal models. Bragin et al. observed the occurrence of late spontaneous seizures from weeks to months after the detection of FR in three kainic acid-treated rats, and found that all the chronic epileptic rats with HFOs developed recurrent spontaneous seizures. The initial HFO activity was detected after status epilepticus where the first spontaneous seizure occurred, and as time passed, seizure frequency increased [69]. Subsequently, they recorded HFOs a lateral fluid percussion injury model within 2 weeks from the trauma and found that the intracranially recorded HFOs are linked with spontaneous seizure [70]. Besides, they defined a novel pattern of paroxysmal EEG activity as “repetitive HFOs and spikes”, which was proved to predict susceptibility to post-traumatic epilepsy [70, 71]. Levesque et al. found that the interictal spikes with FR in CA3 region are the best predictors for seizure occurrence in status epilepticus rats [30]. Overall, these findings suggest that seizure prediction is possible with the use of HFOs in animal models.
Studies have shown that HFOs occur before clinical spasticity and that clinical epileptic seizures may be triggered by HFOs [50]. In a prospective cohort of children with a first unprovoked seizure, HFOs can predict the development of chronic epilepsy, whereas epileptic spikes fail to determine if the patients would develop epilepsy [72]. Worrell et al. found that an increase in HFA within 20 min before the onset of neocortical seizure predict 62% of seizures in patients with neocortical epilepsy [73]. Subsequently, accumulating evidence has indicated variable changes in the HFO rate prior to seizure onset in focal epilepsy [74,75,76,77]. In addition, in pediatric drug-resistant focal epilepsy, the scalp HFO rate is correlated with seizure frequency and thus epilepsy severity, but not with spike rates, in the individual patient; and the higher the HFO rate, the higher the seizure frequency [78, 79]. These studies provide evidence of identifying periods of increased seizure onset probability and clarifying mechanisms of seizure generation in epilepsy.
Focal cortical dysplasia (FCD) is a localized malformation of brain cortical development that causes epilepsy in nearly 30% of patients, and HFOs are generally found in FCD [80]. The HFO rate is higher in patients with FCD type II lesions than in those with type I lesions. The type II lesions are more likely to cause epilepsy with an earlier seizure onset and a greater seizure frequency [81]. Sato et al. analyzed the correlation between spike-related HFOs and post-spike slow-wave power in SOZ during both interictal and preictal periods in 10 pediatric patients with FCD type II. Their results suggest that the relative power reduction of post-spike slow waves to spike-related HFOs correlates with seizure initiation, therefore may contribute to seizure prediction [82].
The duration of medication in BECTS is difficult to determine in the clinical setting since long-term exposure to anticonvulsants may cause side effects such as attention deficits, aggressiveness, nervousness, and sleep disorders [83, 84], while no-treatment or premature discontinuation of treatment could induce seizures, injury or death [85]. Although spikes are being studied as a predictor for seizure attack in BECTS, they can remain detectable even years after the last seizure [50, 86]. A prospective study attempted to test spike ripples as a reliable biomarker to predict seizure risk and they ultimately found that ripples co-occurring with epileptiform discharges predict seizure risk in BECTS better than spikes, regardless of the medication status [87]. Another study showed that the absence of ripples on top of rolandic spikes predicts a likelihood of children to develop benign rolandic epilepsy rather than atypical rolandic epilepsy [79]. Such results provide further evidence for spike ripples as a noninvasive biomarker for predicting the seizure risk of BECTS and facilitating therapeutic stratification, medication guidance, and assessment of relapse risk.
To summarize, HFOs could be considered as a tool to predict seizure occurrence and susceptibility to epilepsy. These findings are inspiring and compelling but large-scale prospective trials are still required to understand the effectiveness of HFOs for the prediction of seizures and detection of epilepsy susceptibility.
HFOs as a biomarker to mirror pathological severity
HFOs can also reflect the severity of pathological injury. The pathological alterations linked with neuronal loss and synaptic reorganization may contribute to the generation of FR [88, 89]. Cepeda et al. have reported that enhanced GABAergic synaptic activity is correlated with interictal FR in the epileptic zone and hyperactivity of GABAergic interneurons is observed in areas with HFOs, suggesting that GABAergic interneurons play a role in the generation of pathological HFOs [90, 91]. The above research all supports the correlation between HFOs and pathology. Generally, radiologically revealed lesions have a predictive value for the surgical outcome [92]. However, for some patients, even in the presence of pathology injury, the general imaging examination including computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) could not reveal any abnormalities, which hinders pre-operative evaluation. Fortunately, studies have determined a strong association between HFOs and radiological lesions such as severe hippocampal damage. HFOs have been recorded ipsilateral to the side of hippocampal sclerosis (HS) in patients with MTLE, and they do not propagate contralaterally in 10 of 11 (91%) patients. Accordingly, the ictal HFOs in the medial temporal lobe are direct electrophysiological evidence for HS [9]. A recent study in a MTLE model further suggested that changes in HFO generation, associated with progressive neuronal loss in the hippocampus, occur as the disease progresses [93]. The rate of interictal HFO has a negative correlation with the electrical stimulus thresholds, supporting the notion that hyperexcitability and HFOs may share common mechanisms [94, 95]. A subsequent study investigated the close relationship between ictal HFOs and hyperexcitability with regard to surgical outcomes. They found that related to cortical hyperexcitability, the proportion of ictal HFOs among resected channels is significantly higher in patients with Engel Class I/II outcomes than in those achieving III/IV outcomes. In addition, a significantly larger percentage of channels with ictal HFOs was found among channels with radiological lesions compared with those without radiological lesions (P < 0.001); likewise, the percentage of channels with ictal HFOs is higher among those meeting the condition of hyperexcitability than those that did not (P < 0.001) [96]. In addition, for other diseases such as FCD, the HFO rate not only varies with different pathologies but also helps define the extent of pathology in epileptogenic dysplastic tissues [80, 81].
Studies have validated the association between HFOs and epileptic networks [29, 97,98,99,100]. Fahoum et al. investigated the brain regions involved in HFOs by combining EEG and functional MRI, and concluded that a higher rate of epileptic ripples is related to a more active pathologic cortical-thalamocortical network [101]. From these findings it becomes evident that HFOs are a good indicator for the severity of pathological injury, which largely broadens its application spectrum.
Challenges in the application of HFOs as a clinical tool
HFOs however have not been widely applied in routine clinical practice [27]. There are several barriers that hinder the use of HFOs in clinical practice. First, the identification of HFOs is challenging. Currently, there is no universal definition of HFOs. Visual inspection of HFOs is still the gold standard, which is a very time-consuming process [102] and prone to subjectivity [103, 104] and poor reproducibility. To address this problem, several groups have developed automated HFO-detection algorithms, many of which have been confirmed with sufficient accuracy and increased processing rate [105]. Second, each channel is analyzed independently, either manually or through automated means [106]. This unbiased approach may induce an increased risk of mistaking non-brain electrical activity for HFOs, known as “false HFOs”. Removing muscle artifacts improves the specificity of HFOs to a certain extent [107, 108]. Third, how to distinguish physiological HFOs from pathological HFOs remains a conundrum [109]. Some studies have indicated that the pathophysiological HFOs are more likely to co-occur with epileptiform spikes, whereas pathological HFOs often occur without spikes or outside SOZ [110]. Besides, the pathophysiological HFOs are found to be coupled with different phases of sleep slow waves: they typically appear before the peak of negative half-waves of the sleep slow waves, while physiological HFOs frequently occur after this peak [111,112,113,114]. Moreover, they have different interactions with slow-wave activities: the spectral frequency bands of pathological HFOs are more likely to be higher than physiological HFOs [115]. In spite of the above difficulties, the evidence in support of the role of HFOs in activity and severity of epilepsy is steadily accruing (Table 1).
Conclusions
The present review summarizes current knowledge on the roles of HFOs in the activity and severity of epilepsy. Although pieces of evidence on this topic are still very limited, both iEEG and scalp EEG evidence points to the value of HFOs in assessing treatment outcome, measuring pathological severity and predicting susceptibility to epilepsy. Among these, the contribution of scalp HFOs to epilepsy is informative, but we cannot ignore the existing controversy on the reliability of scalp HFOs. Most of the current research on scalp EEG signals focuses on the international 10–20 system, which has shortcomings such as the low spatial and temporal resolution. With the emergence of dense-array EEG technologies, more accurate electrical source imaging has become available. Moreover, integrating multi-modal neuroimaging data is warranted for greater clinical application. In the future, more technical and methodological advances for HFOs analysis and more high-quality prospective cohort studies and randomized controlled trials are needed to draw firmer conclusions in this field.
Availability of data and materials
Not applicable.
Abbreviations
- ABPE:
-
Atypical benign partial epilepsy
- ACTH:
-
Adrenocorticotropic hormone
- AED:
-
Anti-epileptic drug
- BECTS:
-
Benign childhood epilepsy with centrotemporal spikes
- CSWS:
-
Continuous spike-waves during slow-wave sleep
- CT:
-
Computed tomography
- EEG:
-
Electroencephalography
- ECoG:
-
Electrocorticography
- EZ:
-
Epileptogenic zone
- FCD:
-
Focal cortical dysplasia
- FR:
-
Fast ripples
- HFA:
-
High-frequency activities
- HFOs:
-
High-frequency oscillations
- HS:
-
Hippocampal sclerosis
- iEEG:
-
Intracranial EEG
- IPE:
-
Idiopathic partial epilepsy
- MRI:
-
Magnetic resonance imaging
- MTLE:
-
Mesial temporal lobe epilepsy
- PET:
-
Positron emission tomography
- PS:
-
Panayiotopoulos syndrome
- R:
-
Ripples
- SEEG:
-
Stereo-electroencephalography
- SOZ:
-
Seizure onset zone
- TSC:
-
Tuberous sclerosis complex
References
Bell G, Sander J. The epidemiology of epilepsy: the size of the problem. Seizure. 2001;10:306–14 quiz 315-306.
Huang CM, White LE Jr. High-frequency components in epileptiform EEG. J Neurosci Methods. 1989;30:197–201.
Fisher RS, Webber WR, Lesser RP, Arroyo S, Uematsu S. High-frequency EEG activity at the start of seizures. J Clin Neurophysiol. 1992;9:441–8.
Bragin A, Engel J Jr, Wilson CL, Fried I, Mathern GW. Hippocampal and entorhinal cortex high-frequency oscillations (100--500 Hz) in human epileptic brain and in kainic acid--treated rats with chronic seizures. Epilepsia. 1999;40:127–37.
Jacobs J, Staba R, Asano E, Otsubo H, Wu JY, Zijlmans M, et al. High-frequency oscillations (HFOs) in clinical epilepsy. Prog Neurobiol. 2012;98:302–15.
Brázdil M, Pail M, Halámek J, Plešinger F, Cimbálník J, Roman R, et al. Very high-frequency oscillations: novel biomarkers of the epileptogenic zone. Ann Neurol. 2017;82:299–310.
Bragin A, Engel J Jr, Wilson CL, Fried I, Buzsáki G. High-frequency oscillations in human brain. Hippocampus. 1999;9:137–42.
Cotic M, Zalay OC, Chinvarun Y, del Campo M, Carlen PL, Bardakjian BL. Mapping the coherence of ictal high frequency oscillations in human extratemporal lobe epilepsy. Epilepsia. 2015;56:393–402.
Usui N, Terada K, Baba K, Matsuda K, Nakamura F, Usui K, et al. Clinical significance of ictal high frequency oscillations in medial temporal lobe epilepsy. Clin Neurophysiol. 2011;122:1693–700.
Sato Y, Doesburg SM, Wong SM, Ochi A, Otsubo H. Dynamic preictal relations in FCD type II: potential for early seizure detection in focal epilepsy. Epilepsy Res. 2015;110:26–31.
Akiyama T, Otsubo H, Ochi A, Ishiguro T, Kadokura G, Ramachandrannair R, et al. Focal cortical high-frequency oscillations trigger epileptic spasms: confirmation by digital video subdural EEG. Clin Neurophysiol. 2005;116:2819–25.
Jacobs J, LeVan P, Chander R, Hall J, Dubeau F, Gotman J. Interictal high-frequency oscillations (80-500 Hz) are an indicator of seizure onset areas independent of spikes in the human epileptic brain. Epilepsia. 2008;49:1893–907.
Gonzalez-Martinez J, Bulacio J, Alexopoulos A, Jehi L, Bingaman W, Najm I. Stereoelectroencephalography in the “difficult to localize” refractory focal epilepsy: early experience from a north American epilepsy center. Epilepsia. 2013;54:323–30.
Podkorytova I, Hoes K, Lega B. Stereo-encephalography versus subdural electrodes for seizure localization. Neurosurg Clin N Am. 2016;27:97–109.
Lamarche F, Job A, Deman P, Bhattacharjee M, Hoffmann D, Gallazzini-Crépin C, et al. Correlation of FDG-PET hypometabolism and SEEG epileptogenicity mapping in patients with drug-resistant focal epilepsy. Epilepsia. 2016;57:2045–55.
Shi J, Lacuey N, Lhatoo S. Surgical outcome of MRI-negative refractory extratemporal lobe epilepsy. Epilepsy Res. 2017;133:103–8.
Kobayashi K, Oka M, Akiyama T, Inoue T, Abiru K, Ogino T, et al. Very fast rhythmic activity on scalp EEG associated with epileptic spasms. Epilepsia. 2004;45:488–96.
Kobayashi K, Inoue T, Watanabe Y, Oka M, Endoh F, Yoshinaga H, et al. Spectral analysis of EEG gamma rhythms associated with tonic seizures in Lennox-Gastaut syndrome. Epilepsy Res. 2009;86:15–22.
Bernardo D, Nariai H, Hussain S, Sankar R, Salamon N, Krueger D, et al. Visual and semi-automatic non-invasive detection of interictal fast ripples: a potential biomarker of epilepsy in children with tuberous sclerosis complex. Clin Neurophysiol. 2018;129:1458–66.
Bernardo D, Nariai H, Hussain SA, Sankar R, Wu JY. Interictal scalp fast ripple occurrence and high frequency oscillation slow wave coupling in epileptic spasms. Clin Neurophysiol. 2020;131:1433–43.
Ohuchi Y, Akiyama T, Matsuhashi M, Kobayashi K. High-frequency oscillations in a spectrum of pediatric epilepsies characterized by sleep-activated spikes in scalp EEG. Clin Neurophysiol. 2019;130:1971–80.
Zelmann R, Lina JM, Schulze-Bonhage A, Gotman J, Jacobs J. Scalp EEG is not a blur: it can see high frequency oscillations although their generators are small. Brain Topogr. 2014;27:683–704.
Burnos S, Fedele T, Schmid O, Krayenbühl N, Sarnthein J. Detectability of the somatosensory evoked high frequency oscillation (HFO) co-recorded by scalp EEG and ECoG under propofol. NeuroImage Clin. 2016;10:318–25.
Kuhnke N, Schwind J, Dümpelmann M, Mader M, Schulze-Bonhage A, Jacobs J. High frequency oscillations in the ripple band (80-250 Hz) in scalp EEG: higher density of electrodes allows for better localization of the seizure onset zone. Brain Topogr. 2018;31:1059–72.
Boran E, Ramantani G, Krayenbühl N, Schreiber M, König K, Fedele T, et al. High-density ECoG improves the detection of high frequency oscillations that predict seizure outcome. Clin Neurophysiol. 2019;130:1882–8.
Zweiphenning W, van Diessen E, Aarnoutse EJ, Leijten FSS, van Rijen PC, Braun KPJ, et al. The resolution revolution: comparing spikes and high frequency oscillations in high-density and standard intra-operative electrocorticography of the same patient. Clin Neurophysiol. 2020;131:1040–3.
Frauscher B, Bartolomei F, Kobayashi K, Cimbalnik J, van’t Klooster M, Rampp S, et al. High-frequency oscillations: the state of clinical research. Epilepsia. 2017;58:1316–29.
Jacobs J, Zijlmans M. HFO to measure seizure propensity and improve prognostication in patients with epilepsy. Epilepsy Curr. 2020;20:338–47.
Kuhnke N, Klus C, Dümpelmann M, Schulze-Bonhage A, Jacobs J. Simultaneously recorded intracranial and scalp high frequency oscillations help identify patients with poor postsurgical seizure outcome. Clin Neurophysiol. 2019;130:128–37.
Levesque M, Behr C, Avoli M. The anti-ictogenic effects of levetiracetam are mirrored by interictal spiking and high-frequency oscillation changes in a model of temporal lobe epilepsy. Seizure. 2015;25:18–25.
Behr C, Lévesque M, Ragsdale D, Avoli M. Lacosamide modulates interictal spiking and high-frequency oscillations in a model of mesial temporal lobe epilepsy. Epilepsy Res. 2015;115:8–16.
Frost JD Jr, Le JT, Lee CL, Ballester-Rosado C, Hrachovy RA, Swann JW. Vigabatrin therapy implicates neocortical high frequency oscillations in an animal model of infantile spasms. Neurobiol Dis. 2015;82:1–11.
Lanzone J, Boscarino M, Ricci L, Insola A, Tombini M, Di Lazzaro V, et al. The effects of antiepileptic drugs on high-frequency oscillations in somatosensory evoked potentials. Clin Neurophysiol. 2020;131:1917–24.
Zijlmans M, Jacobs J, Zelmann R, Dubeau F, Gotman J. High-frequency oscillations mirror disease activity in patients with epilepsy. Neurology. 2009;72:979–86.
Fedele T, van’t Klooster M, Burnos S, Zweiphenning W, van Klink N, Leijten F, et al. Automatic detection of high frequency oscillations during epilepsy surgery predicts seizure outcome. Clin Neurophysiol. 2016;127:3066–74.
Fedele T, Ramantani G, Burnos S, Hilfiker P, Curio G, Grunwald T, et al. Prediction of seizure outcome improved by fast ripples detected in low-noise intraoperative corticogram. Clin Neurophysiol. 2017;128:1220–6.
Haegelen C, Perucca P, Châtillon CE, Andrade-Valença L, Zelmann R, Jacobs J, et al. High-frequency oscillations, extent of surgical resection, and surgical outcome in drug-resistant focal epilepsy. Epilepsia. 2013;54:848–57.
Wu JY, Sankar R, Lerner JT, Matsumoto JH, Vinters HV, Mathern GW. Removing interictal fast ripples on electrocorticography linked with seizure freedom in children. Neurology. 2010;75:1686–94.
Hussain SA, Mathern GW, Sankar R, Wu JY. Prospective and “live” fast ripple detection and localization in the operating room: impact on epilepsy surgery outcomes in children. Epilepsy Res. 2016;127:344–51.
Motoi H, Miyakoshi M, Abel T, Jeong J, Nakai Y, Sugiura A, et al. Phase-amplitude coupling between interictal high-frequency activity and slow waves in epilepsy surgery. Epilepsia. 2018;59:1954–65.
Jobst BC, Cascino GD. Resective epilepsy surgery for drug-resistant focal epilepsy: a review. JAMA. 2015;313:285–93.
van’t Klooster MA, van Klink NE, Leijten FS, Zelmann R, Gebbink TA, Gosselaar PH, et al. Residual fast ripples in the intraoperative corticogram predict epilepsy surgery outcome. Neurology. 2015;85:120–8.
Cho JR, Koo DL, Joo EY, Seo DW, Hong SC, Jiruska P, et al. Resection of individually identified high-rate high-frequency oscillations region is associated with favorable outcome in neocortical epilepsy. Epilepsia. 2014;55:1872–83.
Ochi A, Otsubo H, Donner EJ, Elliott I, Iwata R, Funaki T, et al. Dynamic changes of ictal high-frequency oscillations in neocortical epilepsy: using multiple band frequency analysis. Epilepsia. 2007;48:286–96.
Modur PN, Zhang S, Vitaz TW. Ictal high-frequency oscillations in neocortical epilepsy: implications for seizure localization and surgical resection. Epilepsia. 2011;52:1792–801.
Curatolo P, Nabbout R, Lagae L, Aronica E, Ferreira J, Feucht M, et al. Management of epilepsy associated with tuberous sclerosis complex: updated clinical recommendations. Eur J Paediatr Neurol. 2018;22:738–48.
Ebrahimi-Fakhari D, Mann L, Poryo M, Graf N, von Kries R, Heinrich B, et al. Correction to: Incidence of tuberous sclerosis and age at first diagnosis: new data and emerging trends from a national, prospective surveillance study. Orphanet J Rare Dis. 2019;14:106.
Fujiwara H, Leach J, Greiner H, Holland-Bouley K, Rose D, Arthur T, et al. Resection of ictal high frequency oscillations is associated with favorable surgical outcome in pediatric drug resistant epilepsy secondary to tuberous sclerosis complex. Epilepsy Res. 2016;126:90–7.
Pavone P, Striano P, Falsaperla R, Pavone L, Ruggieri M. Infantile spasms syndrome, West syndrome and related phenotypes: what we know in 2013. Brain Dev. 2014;36:739–51.
Nariai H, Nagasawa T, Juhász C, Sood S, Chugani HT, Asano E. Statistical mapping of ictal high-frequency oscillations in epileptic spasms. Epilepsia. 2011;52:63–74.
Walker LE, Janigro D, Heinemann U, Riikonen R, Bernard C, Patel M. WONOEP appraisal: molecular and cellular biomarkers for epilepsy. Epilepsia. 2016;57:1354–62.
Kobayashi K, Akiyama T, Oka M, Endoh F, Yoshinaga H. A storm of fast (40-150Hz) oscillations during hypsarrhythmia in West syndrome. Ann Neurol. 2015;77:58–67.
Iwatani Y, Kagitani-Shimono K, Tominaga K, Okinaga T, Kishima H, Kato A, et al. Ictal high-frequency oscillations on scalp EEG recordings in symptomatic West syndrome. Epilepsy Res. 2012;102:60–70.
Cao D, Chen Y, Liao J, Nariai H, Li L, Zhu Y, et al. Scalp EEG high frequency oscillations as a biomarker of treatment response in epileptic encephalopathy with continuous spike-and-wave during sleep (CSWS). Seizure. 2019;71:151–7.
Gong P, Xue J, Qian P, Yang H, Liu X, Cai L, et al. Scalp-recorded high-frequency oscillations in childhood epileptic encephalopathy with continuous spike-and-wave during sleep with different etiologies. Brain Dev. 2018;40:299–310.
Qian P, Li H, Xue J, Yang Z. Scalp-recorded high-frequency oscillations in atypical benign partial epilepsy. Clin Neurophysiol. 2016;127:3306–13.
Kobayashi K, Yoshinaga H, Toda Y, Inoue T, Oka M, Ohtsuka Y. High-frequency oscillations in idiopathic partial epilepsy of childhood. Epilepsia. 2011;52:1812–9.
Shibata T, Yoshinaga H, Akiyama T, Kobayashi K. A study on spike focus dependence of high-frequency activity in idiopathic focal epilepsy in childhood. Epilepsia Open. 2016;1:121–9.
Van Schooneveld MM, Braun KP. Cognitive outcome after epilepsy surgery in children. Brain Dev. 2013;35:721–9.
Elliott IM, Lach L, Smith ML. I just want to be normal: a qualitative study exploring how children and adolescents view the impact of intractable epilepsy on their quality of life. Epilepsy Behav. 2005;7:664–78.
Sun D, van’t Klooster M, van Schooneveld M, Zweiphenning W, van Klink N, Ferrier C, et al. High frequency oscillations relate to cognitive improvement after epilepsy surgery in children. Clin Neurophysiol. 2020;131:1134–41.
Ewell LA, Fischer KB, Leibold C, Leutgeb S, Leutgeb JK. The impact of pathological high-frequency oscillations on hippocampal network activity in rats with chronic epilepsy. Elife. 2019;8:e42148.
Höller Y, Kutil R, Klaffenböck L, Thomschewski A, Höller P, Bathke A, et al. High-frequency oscillations in epilepsy and surgical outcome. A meta-analysis. Front Hum Neurosci. 2015;9:574.
Gloss D, Nevitt SJ, Staba R. The role of high-frequency oscillations in epilepsy surgery planning. Cochrane Database Syst Rev. 2017;10:Cd010235.
van’t Klooster MA, van Klink NEC, Zweiphenning W, Leijten FSS, Zelmann R, Ferrier CH, et al. Tailoring epilepsy surgery with fast ripples in the intraoperative electrocorticogram. Ann Neurol. 2017;81:664–76.
Jacobs J, Wu J, Perucca P, Zelmann R, Mader M, Dubeau F, et al. Removing high-frequency oscillations: a prospective multicenter study on seizure outcome. Neurology. 2018;91:e1040–52.
Engel J Jr. Biomarkers in epilepsy: introduction. Biomark Med. 2011;5:537–44.
Modur P, Miocinovic S. Interictal high-frequency oscillations (HFOs) as predictors of high frequency and conventional seizure onset zones. Epileptic Disord. 2015;17:413–24.
Bragin A, Wilson CL, Almajano J, Mody I, Engel J Jr. High-frequency oscillations after status epilepticus: epileptogenesis and seizure genesis. Epilepsia. 2004;45:1017–23.
Bragin A, Li L, Almajano J, Alvarado-Rojas C, Reid A, Staba R, et al. Pathologic electrographic changes after experimental traumatic brain injury. Epilepsia. 2016;57:735–45.
Reid AY, Bragin A, Giza CC, Staba RJ, Engel J Jr. The progression of electrophysiologic abnormalities during epileptogenesis after experimental traumatic brain injury. Epilepsia. 2016;57:1558–67.
Klotz KA, Sag Y, Schönberger J, Jacobs J. Scalp ripples can predict development of epilepsy after first unprovoked seizure in childhood. Ann Neurol. 2021;89:134–42.
Worrell GA, Parish L, Cranstoun SD, Jonas R, Baltuch G, Litt B. High-frequency oscillations and seizure generation in neocortical epilepsy. Brain. 2004;127:1496–506.
Jacobs J, Zelmann R, Jirsch J, Chander R, Dubeau CE, Gotman J. High frequency oscillations (80-500 Hz) in the preictal period in patients with focal seizures. Epilepsia. 2009;50:1780–92.
Zijlmans M, Jacobs J, Kahn YU, Zelmann R, Dubeau F, Gotman J. Ictal and interictal high frequency oscillations in patients with focal epilepsy. Clin Neurophysiol. 2011;122:664–71.
Malinowska U, Bergey GK, Harezlak J, Jouny CC. Identification of seizure onset zone and preictal state based on characteristics of high frequency oscillations. Clin Neurophysiol. 2015;126:1505–13.
Khosravani H, Mehrotra N, Rigby M, Hader WJ, Pinnegar CR, Pillay N, et al. Spatial localization and time-dependant changes of electrographic high frequency oscillations in human temporal lobe epilepsy. Epilepsia. 2009;50:605–16.
Boran E, Sarnthein J, Krayenbühl N, Ramantani G, Fedele T. High-frequency oscillations in scalp EEG mirror seizure frequency in pediatric focal epilepsy. Sci Rep. 2019;9:16560.
van Klink NE, van’t Klooster MA, Leijten FS, Jacobs J, Braun KP, Zijlmans M. Ripples on rolandic spikes: a marker of epilepsy severity. Epilepsia. 2016;57:1179–89.
Ferrari-Marinho T, Perucca P, Mok K, Olivier A, Hall J, Dubeau F, et al. Pathologic substrates of focal epilepsy influence the generation of high-frequency oscillations. Epilepsia. 2015;56:592–8.
Kerber K, LeVan P, Dümpelmann M, Fauser S, Korinthenberg R, Schulze-Bonhage A, et al. High frequency oscillations mirror disease activity in patients with focal cortical dysplasia. Epilepsia. 2013;54:1428–36.
Sato Y, Doesburg SM, Wong SM, Boelman C, Ochi A, Otsubo H. Preictal surrender of post-spike slow waves to spike-related high-frequency oscillations (80-200 Hz) is associated with seizure initiation. Epilepsia. 2014;55:1399–405.
Halma E, de Louw AJ, Klinkenberg S, Aldenkamp AP, IJff DM, Majoie M. Behavioral side-effects of levetiracetam in children with epilepsy: a systematic review. Seizure. 2014;23:685–91.
Mellish LC, Dunkley C, Ferrie CD, Pal DK. Antiepileptic drug treatment of rolandic epilepsy and Panayiotopoulos syndrome: clinical practice survey and clinical trial feasibility. Arch Dis Child. 2015;100:62–7.
Doumlele K, Friedman D, Buchhalter J, Donner EJ, Louik J, Devinsky O. Sudden unexpected death in epilepsy among patients with benign childhood epilepsy with centrotemporal spikes. JAMA Neurol. 2017;74:645–9.
Bouma PA, Bovenkerk AC, Westendorp RG, Brouwer OF. The course of benign partial epilepsy of childhood with centrotemporal spikes: a meta-analysis. Neurology. 1997;48:430–7.
Kramer MA, Ostrowski LM, Song DY, Thorn EL, Stoyell SM, Parnes M, et al. Scalp recorded spike ripples predict seizure risk in childhood epilepsy better than spikes. Brain. 2019;142:1296–309.
Ogren J, Wilson C, Bragin A, Lin J, Salamon N, Dutton R, et al. Three-dimensional surface maps link local atrophy and fast ripples in human epileptic hippocampus. Ann Neurol. 2009;66:783–91.
Staba R, Frighetto L, Behnke E, Mathern G, Fields T, Bragin A, et al. Increased fast ripple to ripple ratios correlate with reduced hippocampal volumes and neuron loss in temporal lobe epilepsy patients. Epilepsia. 2007;48:2130–8.
Cepeda C, Levinson S, Nariai H, Yazon V, Tran C, Barry J, et al. Pathological high frequency oscillations associate with increased GABA synaptic activity in pediatric epilepsy surgery patients. Neurobiol Dis. 2020;134:104618.
Cepeda C, Wu J. Special issue: basic mechanisms of pediatric epilepsy. CNS Neurosci Ther. 2015;21:71–3.
Téllez-Zenteno JF, Hernández Ronquillo L, Moien-Afshari F, Wiebe S. Surgical outcomes in lesional and non-lesional epilepsy: a systematic review and meta-analysis. Epilepsy Res. 2010;89:310–8.
Behr C, Lévesque M, Stroh T, Avoli M. Time-dependent evolution of seizures in a model of mesial temporal lobe epilepsy. Neurobiol Dis. 2017;106:205–13.
Jacobs J, Zijlmans M, Zelmann R, Olivier A, Hall J, Gotman J, et al. Value of electrical stimulation and high frequency oscillations (80-500 Hz) in identifying epileptogenic areas during intracranial EEG recordings. Epilepsia. 2010;51:573–82.
Jacobs J, Zijlmans M, Zelmann R, Chatillon CE, Hall J, Olivier A, et al. High-frequency electroencephalographic oscillations correlate with outcome of epilepsy surgery. Ann Neurol. 2010;67:209–20.
Leung H, Zhu C, Chan D, Poon W, Shi L, Mok V, et al. Ictal high-frequency oscillations and hyperexcitability in refractory epilepsy. Clin Neurophysiol. 2015;126:2049–57.
Zweiphenning W, van’t Klooster M, van Diessen E, van Klink N, Huiskamp G, Gebbink T, et al. High frequency oscillations and high frequency functional network characteristics in the intraoperative electrocorticogram in epilepsy. NeuroImage Clin. 2016;12:928–39.
Cotic M, Chinvarun Y, del Campo M, Carlen PL, Bardakjian BL. Spatial coherence profiles of ictal high-frequency oscillations correspond to those of Interictal low-frequency oscillations in the ECoG of epileptic patients. IEEE Trans Biomed Eng. 2016;63:76–85.
Bragin A, Wilson CL, Engel J Jr. Chronic epileptogenesis requires development of a network of pathologically interconnected neuron clusters: a hypothesis. Epilepsia. 2000;41(Suppl 6):S144–52.
van Diessen E, Hanemaaijer J, Otte W, Zelmann R, Jacobs J, Jansen F, et al. Are high frequency oscillations associated with altered network topology in partial epilepsy? Neuroimage. 2013;82:564–73.
Fahoum F, Melani F, Andrade-Valenca L, Dubeau F, Gotman J. Epileptic scalp ripples are associated with corticothalamic BOLD changes. Epilepsia. 2014;55:1611–9.
Dümpelmann M, Jacobs J, Kerber K, Schulze-Bonhage A. Automatic 80-250Hz “ripple” high frequency oscillation detection in invasive subdural grid and strip recordings in epilepsy by a radial basis function neural network. Clin Neurophysiol. 2012;123:1721–31.
Spring A, Pittman D, Aghakhani Y, Jirsch J, Pillay N, Bello-Espinosa L, et al. Interrater reliability of visually evaluated high frequency oscillations. Clin Neurophysiol. 2017;128:433–41.
Cimbálník J, Hewitt A, Worrell G, Stead M. The CS algorithm: a novel method for high frequency oscillation detection in EEG. J Neurosci Methods. 2018;293:6–16.
Remakanthakurup Sindhu K, Staba R, Lopour BA. Trends in the use of automated algorithms for the detection of high-frequency oscillations associated with human epilepsy. Epilepsia. 2020;61:1553–69.
Worrell GA, Jerbi K, Kobayashi K, Lina JM, Zelmann R, Le Van Quyen M. Recording and analysis techniques for high-frequency oscillations. Prog Neurobiol. 2012;98:265–78.
Zijlmans M, Worrell G, Dümpelmann M, Stieglitz T, Barborica A, Heers M, et al. How to record high-frequency oscillations in epilepsy: a practical guideline. Epilepsia. 2017;58:1305–15.
Ren S, Gliske SV, Brang D, Stacey WC. Redaction of false high frequency oscillations due to muscle artifact improves specificity to epileptic tissue. Clin Neurophysiol. 2019;130:976–85.
Alkawadri R, Gaspard N, Goncharova I, Spencer D, Gerrard J, Zaveri H, et al. The spatial and signal characteristics of physiologic high frequency oscillations. Epilepsia. 2014;55:1986–95.
Frauscher B, von Ellenrieder N, Zelmann R, Rogers C, Nguyen DK, Kahane P, et al. High-frequency oscillations in the normal human brain. Ann Neurol. 2018;84:374–85.
Frauscher B, von Ellenrieder N, Ferrari-Marinho T, Avoli M, Dubeau F, Gotman J. Facilitation of epileptic activity during sleep is mediated by high amplitude slow waves. Brain. 2015;138:1629–41.
von Ellenrieder N, Frauscher B, Dubeau F, Gotman J. Interaction with slow waves during sleep improves discrimination of physiologic and pathologic high-frequency oscillations (80-500 Hz). Epilepsia. 2016;57:869–78.
Weiss SA, Song I, Leng M, Pastore T, Slezak D, Waldman Z, et al. Ripples have distinct spectral properties and phase-amplitude coupling with slow waves, but indistinct unit firing, in human epileptogenic hippocampus. Front Neurol. 2020;11:174.
Song I, Orosz I, Chervoneva I, Waldman ZJ, Fried I, Wu C, et al. Bimodal coupling of ripples and slower oscillations during sleep in patients with focal epilepsy. Epilepsia. 2017;58:1972–84.
Nonoda Y, Miyakoshi M, Ojeda A, Makeig S, Juhász C, Sood S, et al. Interictal high-frequency oscillations generated by seizure onset and eloquent areas may be differentially coupled with different slow waves. Clin Neurophysiol. 2016;127:2489–99.
Akiyama T, McCoy B, Go CY, Ochi A, Elliott IM, Akiyama M, et al. Focal resection of fast ripples on extraoperative intracranial EEG improves seizure outcome in pediatric epilepsy. Epilepsia. 2011;52:1802–11.
van Klink NEC, Van’t Klooster MA, Zelmann R, Leijten FSS, Ferrier CH, Braun KPJ, et al. High frequency oscillations in intra-operative electrocorticography before and after epilepsy surgery. Clin Neurophysiol. 2014;125:2212–9.
Fedele T, Burnos S, Boran E, Krayenbühl N, Hilfiker P, Grunwald T, et al. Resection of high frequency oscillations predicts seizure outcome in the individual patient. Sci Rep. 2017;7:13836.
Cuello-Oderiz C, von Ellenrieder N, Sankhe R, Olivier A, Hall J, Dubeau F, et al. Value of ictal and interictal epileptiform discharges and high frequency oscillations for delineating the epileptogenic zone in patients with focal cortical dysplasia. Clin Neurophysiol. 2018;129:1311–9.
Acknowledgements
Not applicable.
Funding
This work was supported by grants from the National Key R&D Program of China (2017YFC1307500 to QW), the Capital Health Research and Development of Special Program (2016-1-2011 and 2020-1-2013 to QW), the Beijing-Tianjin-Hebei Cooperative Basic Research Program (H2018206435 to QW), the Beijing Natural Science Foundation (Z200024 to YGW and QW), and the National Natural Science Foundation of China (81801280 to GR, 81601126 to JR).
Author information
Authors and Affiliations
Contributions
QW conceived, designed, and supervised the study. YQS drafted the manuscript. GPR, JCR, and QW critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors gave consent to publication of this review.
Competing interests
Author Qun Wang is the member of the Editorial Board for Acta Epileptologica, who was not involved in the journal’s review of, or decisions related to this manuscript. Other authors declare no conflicts of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sun, Y., Ren, G., Ren, J. et al. High-frequency oscillations detected by electroencephalography as biomarkers to evaluate treatment outcome, mirror pathological severity and predict susceptibility to epilepsy. Acta Epileptologica 3, 29 (2021). https://doi.org/10.1186/s42494-021-00063-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42494-021-00063-z