Abstract
Background
The etiology of systemic lupus erythematosus is complex and incurable. A large number of systematic reviews have studied the risk factors of it. Mendelian randomization is an analytical method that uses genetic data as tool variables to evaluate the causal relationship between exposure and outcome.
Objective
To review the systematic reviews and Mendelian randomization studies that focused on the risk factors of systemic lupus erythematosus and shed light on the development of treatments for its prevention and intervention.
Methods
From inception to January 2022, we systematically searched MEDLINE (via PubMed) and Embase for related systematic reviews and Mendelian randomization studies. Extract relevant main data for studies that meet inclusion criteria. The quality of systematic reviews was assessed by using Assessment of Multiple Systematic Reviews 2 (AMSTAR-2). Finally, the risk factors are scored comprehensively according to the results’ quantity, quality, and consistency.
Results
Our study involved 64 systematic reviews and 12 Mendelian randomization studies. The results of systematic reviews showed that diseases (endometriosis, atopic dermatitis, allergic rhinitis), lifestyle (smoking, drinking, vaccination), and gene polymorphism influenced the incidence of systemic lupus erythematosus. The results of Mendelian randomization studies identified the role of disease (periodontitis, celiac disease), trace elements (selenium, iron), cytokines (growth differentiation factor 15), and gut microbiome in the pathogenesis of systemic lupus erythematosus.
Conclusion
We should pay attention to preventing and treating systemic lupus erythematosus in patients with endometriosis, celiac disease, and periodontitis. Take appropriate dietary supplements to increase serum iron and selenium levels to reduce the risk of systemic lupus erythematosus. There should be no excessive intervention in lifestyles such as smoking and drinking.
Similar content being viewed by others
Introduction
Systemic lupus erythematosus (SLE) is a chronic inflammatory autoimmune and multi-systemic disease that is characterized by the production of autoantibodies and tissue deposition of immune complexes. The clinical manifestations range from slight fatigue and joint pain to severe, catastrophic organ damage [1]. Owing to sex, age, ethnicity, time, and environmental exposures the global prevalence of SLE varies widely, with the highest estimates of the prevalence of 241 cases per 100,000 persons in North America and the lowest in Northern Australia [2]. Mortality in patients with SLE is 2–3 times higher than in the general population, and the most common causes are infectious diseases and cardiovascular disease [3].
Despite years of study, the etiology of SLE is still unclear. As reported previously, the development of SLE was associated with hormonal, immunomodulatory, environmental, and genetic factors [4]. Some studies further reported that allergic diseases and hormone-related diseases may be associated with the incidence of SLE; for example, the incidence of SLE in patients with endometriosis is higher than that in controls [5].
Lifestyle may be associated with the incidence of SLE, and its intervention is indispensable in the prevention and treatment of SLE. Studies linked the incidence of SLE to environmental factors, such as silica exposure, smoking and drinking, infection, and vaccination [6]. Evidence from systematic reviews (SRs) suggests that endometriosis, allergic rhinitis, atopic dermatitis, smoking, and vaccination are associated with an increased incidence of SLE.
Gene polymorphism plays an important role in elucidating the susceptibility to diseases and the diversity in the clinical manifestations of the diseases. Single Nucleotide Polymorphism (SNP) is the most common DNA sequence variation in a population. Several studies have shown the key role of SNP in the development of SLE. For example, SNP leads to abnormal T-cell function [4]. And it is known that the risk A allele of SNP (PPP2CA rs7704116) [7] is known to be one of the reasons for the increased incidence of SLE.
Clinical observational studies can only show that the disease and risk factors are related, but it is difficult to make causal inferences. The correlation is likely to be a “false correlation” caused by a variety of confounding factors, and the existence of reverse causality cannot be ignored. Mendelian randomization (MR) study is an analytical method used to evaluate the causal relationship between observable exposure or risk factors and clinical-related results [8]. The core of it is to use genetic data and take genetic variables as instrumental variables, which can effectively overcome the bias caused by confounding. In genetic correlation, the direction of causality is determined, which avoids the interference of reverse causality and thus provides more compelling evidence. At present, there is no research to comprehensively summarize the risk factors of SLE from SR and MR evidence.
In this paper, the reported risk factors of SLE are reviewed and summarized from the perspectives of disease, lifestyle, gene polymorphism, and evidence from MR, to better understand the etiology and provide better medical advice for disease management for the whole population.
Method
Search strategy
We searched MEDLINE (via PubMed), Embase from inception to January 27, 2022, by using the keywords “Risk factor” “Systemic lupus erythematosus”, “Systematic review”, “Meta-analysis”, “Mendelian randomization study” with no restriction on language. For complete search strategies, see “Appendix A” section.
Study selection
All retrieved studies were imported into Zotero (6.0.9), and duplicate studies were removed. Two independent reviewers (X-YX, QC) screened the title and abstract of the article. After cross-checking, the 2 reviewers further independently assessed the full text of the eligible studies. Disagreements about the inclusion of qualified studies were resolved through discussion. If they cannot be resolved, the third reviewer (HZ) would make the final decision.
Inclusion: (1) SR of risk factors related to the incidence of SLE; (2) SR of autoimmune diseases including SLE; (3) MR study of SLE. Exclusion: (1) review; (2) case report; (3) original clinical research; (4) autoimmune-related but not related to SLE or related to SLE but lacking corresponding data; (5) discoid lupus erythematosus; (6) lupus nephritis; (7) drug-induced lupus erythematosus.
Data extraction
Two researchers independently extracted data according to predetermined extraction criteria. The following information was extracted from papers on disease and lifestyle, and some papers did not contain all information: Study ID, risk factor, outcome (relative risk or odds ratio of a risk factor to SLE, 95% confidence interval, and P-value), type of study design (cohort, case–control, or cross-sectional), presence or absence of sensitivity and subgroup analyses, publication bias, and quality assessment tools (Table 1).
MR studies extracted the following: Study ID, number of SNP, and main results (Table 2). Studies of genetic polymorphism were divided into four categories: risk factors, protective factors, contradictory factors, and unrelated factors. The following information was extracted: study ID, gene and SNP, and major significant results (Table 3).
Assessment of methodological quality
Assessment of Multiple Systematic Reviews 2 (AMSTAR-2) is a tool to assess the quality of included SRs. There were 16 items, including 7 critical items (items 2, 4, 7, 9, 11, 13, 15) and 9 non-critical items. Each item was evaluated as ‘‘yes’’ (a positive result), ‘‘partial yes’’ (partial adherence to the standard), and ‘‘no’’ (no information is provided to rate an item) according to adherence to the standard. Based on these items, SR was divided into four grades: high, moderate, low, and critically low [9]. This review evaluates SRs with risk factors related to disease and lifestyle (“Appendix B” section).
Determination of the magnitude of risk factors
SR and MR Studies were scored and the magnitude was determined according to the number of studies on risk factors, the average score of AMSTAR-2, the consistency of results from different studies, the consistency of results from different methods and sensitivity tests, and finally summarize the risk factors and magnitude of SLE (Fig. 1).
Risk Factors for SLE and the consensus on the magnitude. Abbreviations: SLE, systemic lupus erythematosus. SR, systematic review. MR, Mendelian randomization. AMSTAR-2, Assessment of Multiple Systematic Reviews 2. TNF-α, tumor necrosis factor-α. TNFAIP3, Tumor necrosis factor-α-induced protein 3. TNFSF4, Tumor necrosis factor ligand superfamily member 4. IL, Interleukin. HLA, Human leukocyte antigen. IRF5, Interferon regulatory factor 5. STAT4, Signal transducer and activator of transcription 4. ITGAM, Integrin Subunit Alpha M. Annotation: Determination on the magnitude for the risk factors: a systematic reviews: based on a consensus after considering the evidence from (i). The number of literature, (ii). The average score of AMSTAR-2 (no score added for e critically low, 1 score for low, 3 scores for moderate, and 5 scores for high quality), and iii. The consistency of the results (1 score for factors with a number of ≥ 3 and consistent results, inconsistent results with a number of ≥ 2 minus 1 score). b Mendelian randomization: based on a consensus after considering the evidence from (i). The number of literature, (ii). The consistency of results (2 scores if the results of inverse variance weighted, weighted median, and MR Egger are consistent, otherwise no score), and (iii). Sensitivity tests (no horizontal pleiotropy is counted as 1 score, otherwise no score). If the risk factors involved both SR and MR studies, the scores were added if the results were consistent and subtracted if the results were not consistent. Score the SR and MR studies according to the above criteria and label low, medium, and high after the score (“low” for scores 1 and 2, “medium” for scores 3 and 4, and “high” for 5 and above.), and finally summarize the risk factors and related magnitude of SLE
Results
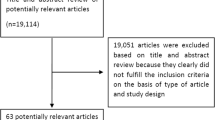
A total of 594 articles were retrieved on SRs of risk factors. After removing duplicates, 493 articles remained. After screening the title and abstract, 119 articles remained. 64 articles were finally included after reading the full text. One study was related to the worldwide incidence of SLE, 3 were related to disease, 10 were related to lifestyle, and 50 were related to gene polymorphism. In the study of gene polymorphism, 19 genes or SNPs were risk factors.
A total of 45 MR studies related to risk factors were retrieved. After removing duplicates, 31 articles remained, and 12 were finally included in our review. Among them, 2 were related to disease, 5 were related to lifestyle, 2 were related to cytokine, 2 were related to trace elements, and 1 was related to gut microbiome (Fig. 2).
Finally, our study involved 5 diseases (endometriosis, atopic dermatitis, allergic rhinitis, celiac disease, periodontitis), 9 lifestyles (smoking, drinking, vaccination, silicone breast implants, helicobacter Pylori infection, immigration, Vitamin D, coffee consumption, statins), 2 cytokines (circulating adiponectin, growth differentiation factor 15), 2 trace elements (selenium, iron), the gut microbiome (Bacillales, Coprobacter, Lachnospira, Actinobacteria, Bacilli, Lactobacillales, and Eggerthella), and more than 10 gene polymorphisms (Table 4).
Risk factors
Disease
Endometriosis
One SR and meta-analysis including cohort studies and case–control studies in the study of endometriosis [5] (OR for case–control studies 1.36, 95% CI 1.07–1.73, P = 0.010; RR for cohort studies 1.74, 95% CI 1.10–2.77, P = 0.020), and show the prevalence of SLE in patients with endometriosis was higher than that in the control group. It was rated moderate quality by AMSTAR-2.
Endometriosis is an estrogen-dependent disorder, and the increase in estrogen level can aggravate or induce SLE by suppressing cellular immunity and increasing the formation of autoantibodies [10].
Atopic dermatitis
Atopic dermatitis is associated with an increased risk of cardiovascular, neurological, and autoimmune disease. Meta-analysis showed participants who had atopic dermatitis were at an increased risk of SLE [11] (OR 1.46, 95% CI 1.05–2.04, P = 0.020). The result of AMSTAR-2 was critically low quality.
Allergic rhinitis
Patients with allergic rhinitis had a higher risk of SLE than individuals without [12] (OR 1.36, 95% CI 1.08–1.72, P = 0.009). The result of AMSTAR-2 was critically low quality.
The pathogenesis of atopic dermatitis, allergic rhinitis, and autoimmune disorders was similar and related to the increase of inflammatory mediators and immune dysregulation [13]. The up-regulation of Th2 activity and the increase of IgE production during the development of the disease may be the triggers for SLE in the future.
Lifestyle
Smoking and drinking
Previous studies showed that moderate drinking reduced the risk of SLE, and smoking increased it [6]. The main mechanisms include the anti-inflammatory mechanism related to alcohol consumption [14], including lower levels of C-reactive protein and fibrinogen in plasma, and Cigarette-related pro-inflammatory mechanisms including an increase in plasma C-reactive protein, oxidative stress, and apoptosis. The effects of drinking status and smoking consumption on chemokine/cytokine concentrations in healthy female nurses in the United States in 2020 and 2021 showed that moderate drinking was related to lower stem cell factor levels [15]. The current smoking status was related to the decrease of B-lymphocyte stimulator and interleukin-10 (IL-10) [16].
An SR of drinking indicated that moderate alcohol consumption might be a protective factor (OR 0.71, 95% CI 0.55–0.93, P = 0.012), while light and heavy alcohol consumption were not related to the risk of SLE [17].
We included four SRs related to smoking from 2004 to 2020. The first [18] pointed out that the current smoking status was correlated with the development of SLE (OR 1.50, 95% CI 1.09–2.08), but there was no correlation among former smokers (OR 0.98, 95% CI 0.75–1.27). The second showed consistent results on the impact of current smoking, but when analyzing non-smokers and former smokers, different regions showed inconsistent results [19]. The third stated that smoking was not only a risk factor for SLE but also hampered disease treatment by reducing the curative effect of belimumab [20]. Therefore, it was suggested that smoking cessation should be the first task in the prevention and treatment of SLE, which was supported in the fourth SR [21].
Vaccination
Vaccination can stimulate antigens to produce a specific immune response, so it is considered the pathogenic factor of SLE. One SR with 12 studies showed that vaccination significantly increased the risk of SLE (RR 1.50, 95% CI 1.05–2.12, P = 0.024) [22]. The results of subgroup analysis and sensitivity analysis both supported this conclusion.
Silicone breast implants
Autoimmune diseases caused by silicone breast implantation have long been a concern, but the SR results seemed to be reassuring. There was no evidence that silicone breast implantation was associated with connective tissue and autoimmune diseases, including SLE (RR 0.65, 95% CI 0.35–1.23) [23].
Helicobacter pylori infection
The molecular simulation, activation of polyclonal lymphocytes, and cell damage produced by Helicobacter pylori may be risk factors for autoimmune diseases. One SR published in 2020 showed that Helicobacter pylori infection was not related to SLE susceptibility (OR 0.97, 95% CI 0.76–1.23, P = 0.820), but its strains (H. pylori cagA positive strains) might be associated with a higher risk of autoimmune diseases (OR 2.65, 95% CI 1.52–4.64, P = 0.001) [24].
Immigrant
It was believed that environmental factors have made a great contribution to its incidence. Based on the findings of five population studies, the incidence of SLE was the highest among immigrants from Africa, Iraq, and South Asia, especially among women and successive immigrant descendants [25]. Assuming that “immigration” is a risk factor for people in the appeal area, the impact of environmental and lifestyle changes behind immigration on the incidence of SLE cannot be ignored.
Others
The SR about vitamin D showed that vitamin D level was negatively related to SLE disease activity [26]. Although there were some reported risk factors, such as ultraviolet radiation, silica, air pollution, pesticides, heavy metals, and so on [6, 27], they were not covered in this paper due to the lack of SR evaluation.
Gene polymorphism
Gene polymorphism means that the structure or nucleotide sequence of the same gene is not the same in different individuals, which is the variation of alleles. Human gene polymorphism plays an important role in elucidating the susceptibility and tolerance of the human body to disease, the diversity of clinical manifestations of diseases, and the responsiveness to drug treatment.
There are three types of genes related to SLE: genes regulating the function of B cells and T cells, genes regulating interferon (IFN), and genes repairing DNA [28]. The gene polymorphism study of this article mainly includes two aspects of B Cell and T Cell Function-related genes and genes regulating IFN.
B cell and T cell function-related genes
Vitamin D
The vitamin D receptor (VDR) is a member of the nuclear receptor superfamily. By binding to VDR, vitamin D can exert biological functions such as cell proliferation, differentiation, and immune response in the human body, and inhibit the pro-inflammatory activity of Th1 cells and the production of cytokines, such as IL-2, IFN-γ and TNF-α [29].
The polymorphism of the VDR gene was related to SLE, and its polymorphism mainly included the following four types: VDR BsmI(rs1544410), Fok1(rs2228570), ApaI(rs7975232), and TaqI(rs731236). In three studies from 2014 to 2016 [29,30,31], the results showed that the polymorphism of BsmI(rs1544410) and FokI(rs2228570) in the Asian population contributed to the pathogenesis of SLE, but the findings were not replicated in the Caucasian population.
B‑cell lymphocyte kinase
B-cell lymphocyte kinase (BLK), a member of the Src family, is involved in signal transduction downstream of B-cell receptors, B-cell development, differentiation, and signal transduction, and further affects B-cell function [32]. The risk allele variation of BLK may cause changes in the level of BLK protein, which may affect the tolerance mechanism of B cells and induce immune diseases. There was a significant correlation with BLK(rs4840568) (OR 1.32, 95% CI 1.22–1.43, P = 0.010) [33] and BLK(rs13277113) A-type allele (OR 1.36, 95% CI 1.29–1.43, P < 0.001) [34].
Cytotoxic T lymphocyte-associated Antigen-4
Cytotoxic T lymphocyte-associated antigen-4 (CTLA-4), expressed on T cells, is a key down-regulated molecule that inhibits T cell activation and regulates its peripheral tolerance [35]. The relationship between rs231775(+49A/G) polymorphism [35,36,37,38] and SLE was studied, and the conclusions based on different races showed significant heterogeneity. The rs231775(+49A/G) polymorphism mainly contributed to the SLE development in the Asian population.
Tumor necrosis factor-α and related gene
Tumor necrosis factor-α (TNF-α) is a proinflammatory cytokine, which can stimulate the production of cytokines, enhance the expression of adhesion molecules, increase neutrophil activation, and act as a costimulatory factor for T cell activation and antibody production. Its function-related proteins and receptors are actively involved in the pathogenesis of SLE. Five SR-based meta-analyses reported TNF-α promoter-308A/G polymorphism [39,40,41,42,43]. These studies were carried out in the China population, and whether the conclusions could be extended to other populations remained to be verified. There were also a series of genes related to TNF, such as tumor necrosis factor-α-induced protein 3 (TNFAIP3) (rs2230926) [44,45,46,47], tumor necrosis factor ligand superfamily member 4 (TNFSF4) (rs2205960) [48,49,50,51], and tumor necrosis factor receptor-associated factor 1, complement component 5 (TRAF1/ C5)(rs10818488) [52] were also related to SLE susceptibility.
Interleukin
Interleukin (IL), a kind of cytokine produced by many kinds of cells, plays an important role in a series of processes such as the maturation, activation, proliferation, and regulation of immune cells. IL-1 gene polymorphism, including IL-1A-889C/T, IL-1B-31T/C, and IL-1B-511C/T, might be associated with a higher risk of SLE [53], which needed more research to prove. IL-6 polymorphisms, rs1800796 and rs1800795, might be risk factors in the previous studies [54,55,56]. However, one study in 2021 showed that rs1800795 was a protective factor, and rs1800796 was not associated with susceptibility [57], which was inconsistent with results from previous studies. IL-10 gene polymorphism rs1800896 was related to susceptibility [28, 58, 59], while rs1800871 and rs1800872 were not related to susceptibility. Although some of them were different in subgroup analysis, we wrote the report based on the results of the general population. The results of research on IL-18 rs187238 were inconsistent. One study showed that there was no relationship between rs187238 polymorphism and SLE in all populations, including the Chinese population [60]. Another study with hierarchical analysis showed that rs187238 was a risk factor for SLE, especially in the Asian population [61].
Human leukocyte antigen
The frequency change of the human leukocyte antigen (HLA) allele is related to SLE. One study focusing on the relationship between HLA-DRB1 allele polymorphism and SLE susceptibility demonstrated that HLADR3, DR9, and DR15 were risk factors [62]. Another study provided evidence to support HLA-DR3 and HLA-DR15 as the risk factors for SLE, and the study acknowledged the existence of inter-ethnic heterogeneity [63].
Interferon regulatory genes
Interferon regulatory factor 5
Interferon regulatory factor 5 (IRF5) belongs to the transcription factor family that regulates the activity of the immune system. It is expressed in antigen-presenting cells (including dendritic cells, macrophages, and B cells) and monocytes, and it participates in the pathogenesis of SLE by influencing the antigen-presenting cells [64]. IRF5 rs2070197 T allele and rs2004640 C allele were positively associated with the pathogenesis of SLE [65, 66]. Although rs2070197 showed susceptibility to SLE in the general population (OR 2.13, 95% CI 1.86–2.44, P < 0.001), it had no effect in the Asian population [67]. Since this gene is monomorphic in China and Korea, the population in the two countries was not affected by the disease susceptibility caused by this gene polymorphism. It was speculated that it may be caused by the linkage imbalance between regions, and further studies on the specificity of ethnic populations are therefore needed.
STAT4
The signal transducer and activator of transcription 4 (STAT4) is a transcription factor activated by IFN-α signal transduction, and the increase of IFN-α signal transduction is the main pathogenic promotor of SLE. The genetic variation of STAT4 is related to the risk of SLE. Three SRs showed that there was a significant relationship between the STAT4 rs7574865 T allele and the risk of developing SLE, and the OR value was around 1.60 [68,69,70].
MiR-146a
MiR-146a is identified as a negative regulator of natural immunity, which directly inhibits the downstream transactivation of type-I IFN at the molecular level and targets IRF5. There were some contradictions in the results of miR-146a. No association between miR-146a and SLE susceptibility was found in 2015 [71] and 2017 [72], which might be attributed to the small number of included studies. MiR-146a rs57095329 was found to correlate with the risk of SLE in two studies [73, 74], but this correlation was not supported in a recent study [75]; the rs2431697 and susceptibility to SLE were confirmed by two studies [73, 75].
Integrin Subunit Alpha M
Complement dysfunction impairs the ability to clear apoptotic cell fragments, which may stimulate the production of autoantibodies in SLE. The rs1143679 G/A polymorphism in Integrin Subunit Alpha M (ITGAM) severely impaired the phagocytosis of complement-coated particles and was positively associated with the risk of SLE [76], consistent with the findings of two studies in 2011 [77] and 2021 [76].
Evidence from Mendelian randomization study
The evidence from SRs including case–control or cohort studies was meaningful to confirm the correlation between risk factors and SLE development, but it is insufficient to make causal inferences. MR is an analytical method of causal estimation based on epidemiological data. it has been widely used in the medical field in recent years to assess the causal effect between exposure and outcome. We summarized the findings from the included 13 MR studies on SLE below.
Serum selenium, iron, growth differentiation factor 15, and circulating adiponectin
Three MR analyses were performed [78,79,80], showing that the rise in serum selenium (OR 0.85, 95% CI 0.77–0.93, P = 0.001) [78], serum iron (OR 0.79, 95% CI 0.66–0.94) [79] and growth differentiation factor 15 (GDF-15) (OR 0.80, 95% CI 0.68–0.92) [80] were all related to the decrease of SLE risk, which provided the potential causal evidence of the protective effect of selenium, iron and GDF-15 on SLE.
Another study showed that there was no causal relationship between circulating adiponectin levels and SLE (OR 1.38, 95% CI 0.91–1.35, P = 0.130) [81]. The test of reverse causation in the study was also negative, and the several analyses performed also supported this conclusion.
Gut microbiome
Xiang et al. [82] conducted a study on the composition of the gut microbiome (211 gut microbiota), supporting a causal relationship between its positive and negative effects on SLE risk (Table 2). The results of inverse variance weighted, MR Egger, and weighted median methods were slightly different. The levels of Bacillales, Coprobacter, Lachnospira, and Actinobacteria were negatively correlated with the risk of SLE, while Bacilli, Lactobacillales, and Eggerthella might be risk factors for SLE. Although the overlapping in the study samples—a limitation in two-sample MR studies—might affect the robustness of the findings, these findings intrigue thoughts about the development of new treatment modalities, such as probiotics supplements, for the treatment of SLE.
Statins
Recently, an MR used HMGCR inhibition to genetically mimic statins and studied the relationship between the genetic mimicry effect of statins and allergic diseases and immune-related diseases. The results showed that genetic mimicry had little effect on allergic diseases or autoimmune diseases of men or women (OR 0.72, 95% CI 0.33–1.58, P = 0.419) [83].
Periodontitis, celiac disease, vitamin D, coffee consumption, smoking, and drinking
Four studies on periodontitis [84], vitamin D [85], coffee consumption [86], and alcohol intake [87] were conducted, respectively. The results showed that there might be a causal relationship between periodontal inflammation and SLE (β < 0.01, SE < 0.01, P = 0.046) [84]. Besides, celiac disease also showed a possible causal relationship (β = 0.29, SE = 0.06, P < 0.001) [88]. Vitamin D, coffee consumption, and alcohol intake had no causal relationship with SLE. The common problem of the studies was the insufficient number of SNP and the existence of weak instrumental bias. One study showed that there was no causal relationship between smoking or drinking and the risk of SLE [89]. The analysis results based on the three methods were consistent, and the corresponding tool variables were appropriate.
The aforementioned MR studies adopted the above genetic data from the European population only, which ensured the genetic homogeneity and robustness of the results but limited the generalization of the results to other populations. Therefore, the appeal of causality is worthy of further exploration.
Discussion
Combined evidence from SR and MR showed that endometriosis, atopic dermatitis, allergic rhinitis, periodontitis, and celiac disease were risk factors for SLE. The increased levels of trace elements iron, selenium, and GDF-15 should be protective factors for SLE. Smoking, alcohol consumption, coffee consumption, and vitamin D did not appear to have any effect on the risk of SLE.
Periodontitis and celiac disease should be paid more attention as observed risk factors. Early detection and screening of antibodies in people with these diseases may prevent the follow-up occurrence and development of SLE. More research evidence on the causal relationship between endometriosis, atopic dermatitis, allergic rhinitis, and SLE is needed to further define disease interactions.
Based on the results of MR, serum iron, selenium, GDF-15, gut microbiomes Bacillales, Lachnospira, and Actinobacteria might provide more options for the prevention and treatment of SLE, and relevant clinical trials are needed to verify their protective effects.
The pathogenesis of SLE is related to the reduction of T lymphocytes, the decline of the function of T suppressor cells, and the excessive proliferation of B cells to produce a large number of antibodies. The existing emerging therapies for SLE focus on the T-/B cell costimulatory pathway as a target [90]. The risk factors confirmed by the studies of gene polymorphism included STAT4, IFN-α, and IL-10, suggesting that future research might focus on multi-target and multi-pathway precision therapy, for example, using a combination of B cell activator inhibitor, IFN-α and STAT4 inhibitors, and recombinant human IL-2. The prevention and treatment effect may be achieved by regulating cytokines.
Contrary to the experience of routine care for SLE, smoking, alcohol consumption, coffee consumption, and vitamin D, as shown by the MR studies, were not associated with SLE pathogenesis. This finding might indicate that other confounding factors contribute more to SLE, for example, patients who smoke or overdrink might be under the status of stress, depression, higher frequency of staying up late, or less physical exercise. Such specific lifestyle interventions, such as smoking or overdrinking, may not be emphasized in future medical advice to SLE patients and those at risk for the disease. Instead, more MR analyses should be conducted to rule out the real disease contributors behind the aforementioned unhealthy lifestyles.
Finally, according to the studies of SR and MR, we determined the risk factors and their magnitude based on the quality, quantity, and consistency of the results (Fig. 1). We summed up the most relevant risk factors for SLE. There was only one study of endometriosis, atopic dermatitis, allergic rhinitis, periodontitis, and celiac disease. The quality of evidence of endometriosis and celiac disease was medium (4 scores), periodontitis, atopic dermatitis and allergic rhinitis were all low-quality evidence (1–2 scores), more research is needed to support it in the future. The MR results of smoking and drinking were both negative and the evidence was of high quality. We tend to not correlate with drinking and SLE, so it was not included. There were four SRs on smoking, but the AMSTAR-2 score was very low, and MR did not support it as a risk factor, so smoking was also low-quality evidence (1 score). All research on gene polymorphism came from SR. We summarized the 9 genes with the largest number of literature and the most consistent results, among which the genes related to TNF had the highest score (6 scores), which was high-quality evidence.
However, some limitations in this review or included studies should be noted. First, the search was relatively not comprehensive, we only searched two databases. The types of included studies were limited, including only SRs and MR, without original studies and reviews, and the literature was not up-to-date enough. Second, most of the SR quality assessment scores included in the studies were critically low. Many of the included studies were small in scale and were likely to produce false associations. MR studies of endometriosis, atopic dermatitis, allergic rhinitis, and SLE are also needed to further determine the causal relationship. Finally, there is a lack of official assessment tools for MR quality to confirm the reliability of the evidence.
Conclusion
In short, we should pay attention to preventing and treating SLE in patients with endometriosis, celiac disease, and periodontitis. Take appropriate dietary supplements to increase serum iron and selenium levels to reduce the risk of SLE. There should be no excessive intervention in lifestyle such as smoking and drinking, as it does not affect the incidence of SLE.
Availability of data and materials
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- SLE:
-
Systemic lupus erythematosus
- SR:
-
Systematic review
- MR:
-
Mendelian randomization
- SNP:
-
Single nucleotide polymorphism
- AMSTAR-2:
-
Assessment of Multiple Systematic Reviews 2
- IL:
-
Interleukin
- IFN:
-
Interferon
- VDR:
-
Vitamin D receptor
- BLK:
-
B-cell lymphocyte kinase
- CTLA-4:
-
Cytotoxic T lymphocyte-associated antigen-4
- TNF-α:
-
Tumor necrosis factor-α
- TNFAIP3:
-
Tumor necrosis factor-α-induced protein 3
- TNFSF4:
-
Tumor necrosis factor ligand superfamily member 4
- TRAF1/C5:
-
Tumor necrosis factor receptor-associated factor 1: complement component 5
- HLA:
-
Human leukocyte antigen
- IRF5:
-
Interferon regulatory factor 5
- STAT4:
-
Signal transducer and activator of transcription 4
- ITGAM:
-
Integrin Subunit Alpha M
References
Kiriakidou M, Ching CL. Systemic lupus erythematosus. Ann Intern Med. 2020;172:ITC81–96. https://doi.org/10.7326/AITC202006020.
Rees F, Doherty M, Grainge MJ, Lanyon P, Zhang W. The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatology. 2017;56:1945–61. https://doi.org/10.1093/rheumatology/kex260.
Barber MRW, Drenkard C, Falasinnu T, Hoi A, Mak A, Kow NY, Svenungsson E, Peterson J, Clarke AE, Ramsey-Goldman R. Global epidemiology of systemic lupus erythematosus. Nat Rev Rheumatol. 2021;17:515–32. https://doi.org/10.1038/s41584-021-00668-1.
Tsokos GC. Systemic lupus erythematosus. N Engl J Med. 2011. https://doi.org/10.1056/NEJMra1100359.
Shigesi N, Kvaskoff M, Kirtley S, Feng Q, Fang H, Knight JC, Missmer SA, Rahmioglu N, Zondervan KT, Becker CM. The association between endometriosis and autoimmune diseases: a systematic review and meta-analysis. Hum Reprod Update. 2019;25:486–503. https://doi.org/10.1093/humupd/dmz014.
Barbhaiya M, Costenbader KH. Environmental exposures and the development of systemic lupus erythematosus. Curr Opin Rheumatol. 2016;28:497–505. https://doi.org/10.1097/BOR.0000000000000318.
Tan W, Sunahori K, Zhao J, Deng Y, Kaufman KM, Kelly JA, Langefeld CD, Williams AH, Comeau ME, Ziegler JT, et al. Association of PPP2CA polymorphisms with systemic lupus erythematosus susceptibility in multiple ethnic groups. Arthritis Rheum. 2011;63:2755–63. https://doi.org/10.1002/art.30452.
Sekula P, Del Greco MF, Pattaro C, Köttgen A. Mendelian randomization as an approach to assess causality using observational data. J Am Soc Nephrol. 2016;27:3253–65. https://doi.org/10.1681/ASN.2016010098.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. https://doi.org/10.1136/bmj.j4008.
Bereshchenko O, Bruscoli S, Riccardi C. Glucocorticoids, sex hormones, and immunity. Front Immunol. 2018;9:1332. https://doi.org/10.3389/fimmu.2018.01332.
Ponvilawan B, Charoenngam N, Wongtrakul W, Ungprasert P. Association of atopic dermatitis with an increased risk of systemic lupus erythematosus: a systematic review and meta-analysis. J Postgrad Med. 2021;67:139–45. https://doi.org/10.4103/jpgm.JPGM_1270_20.
Wongtrakul W, Charoenngam N, Ponvilawan B, Ungprasert P. Allergic rhinitis and risk of systemic lupus erythematosus: a systematic review and meta-analysis. Int J Rheum Dis. 2020;23:1460–7. https://doi.org/10.1111/1756-185X.13928.
Sin E, Anand P, Frieri M. A link: allergic rhinitis, asthma & systemic lupus erythematosus. Autoimmun Rev. 2016;15:487–91. https://doi.org/10.1016/j.autrev.2016.02.003.
Imhof A, Froehlich M, Brenner H, Boeing H, Pepys MB, Koenig W. Effect of alcohol consumption on systemic markers of inflammation. Lancet. 2001;357:763–7. https://doi.org/10.1016/S0140-6736(00)04170-2.
Hahn J, Leatherwood C, Malspeis S, Liu X, Lu B, Roberts AL, Sparks JA, Karlson EW, Feldman CH, Munroe ME, et al. Associations between daily alcohol consumption and systemic lupus erythematosus-related cytokines and chemokines among US female nurses without SLE. Lupus. 2020;29:976–82. https://doi.org/10.1177/0961203320929427.
Hahn J, Leatherwood C, Malspeis S, Liu X, Lu B, Roberts AL, Sparks JA, Karlson EW, Feldman CH, Munroe ME, et al. Associations between smoking and systemic lupus erythematosus-related cytokines and chemokines among US female nurses. Arthritis Care Res. 2021;73:1583–9. https://doi.org/10.1002/acr.24370.
Wang J, Liu J, Pan L, Guo L, Liu C, Yang S. Association between alcohol intake and the risk of systemic lupus erythematosus: a systematic review and meta-analysis. Lupus. 2021;30:725–33. https://doi.org/10.1177/0961203321991918.
Costenbader KH, Kim DJ, Peerzada J, Lockman S, Nobles-Knight D, Petri M, Karlson EW. Cigarette smoking and the risk of systemic lupus erythematosus: a meta-analysis. Arthritis Rheum. 2004;50:849–57. https://doi.org/10.1002/art.20049.
Jiang F, Li S, Jia C. Smoking and the risk of systemic lupus erythematosus: an updated systematic review and cumulative meta-analysis. Clin Rheumatol. 2015;34:1885–92. https://doi.org/10.1007/s10067-015-3008-9.
Parisis D, Bernier C, Chasset F, Arnaud L. Impact of tobacco smoking upon disease risk, activity and therapeutic response in systemic lupus erythematosus: a systematic review and meta-analysis. Autoimmun Rev. 2019;18:102393. https://doi.org/10.1016/j.autrev.2019.102393.
Chua MH, Ng IA, Mike WC, Mak A. Association between cigarette smoking and systemic lupus erythematosus: an updated multivariate Bayesian meta-analysis. J Rheumatol. 2020;47:1514–21. https://doi.org/10.3899/jrheum.190733.
Wang B, Shao X, Wang D, Xu D, Zhang J-A. Vaccinations and risk of systemic lupus erythematosus and rheumatoid arthritis: a systematic review and meta-analysis. Autoimmun Rev. 2017;16:756–65. https://doi.org/10.1016/j.autrev.2017.05.012.
Janowsky EC, Kupper LL, Hulka BS. Meta-analyses of the relation between silicone breast implants and the risk of connective-tissue diseases. N Engl J Med. 2000;342:781–90. https://doi.org/10.1056/NEJM200003163421105.
Youssefi M, Tafaghodi M, Farsiani H, Ghazvini K, Keikha M. Helicobacter pylori infection and autoimmune diseases; is there an association with systemic lupus erythematosus, rheumatoid arthritis, autoimmune atrophy gastritis and autoimmune pancreatitis? A systematic review and meta-analysis study. J Microbiol Immunol Infect. 2021;54:359–69. https://doi.org/10.1016/j.jmii.2020.08.011.
Agrawal M, Shah S, Patel A, Pinotti R, Colombel J-F, Burisch J. Changing epidemiology of immune-mediated inflammatory diseases in immigrants: a systematic review of population-based studies. J Autoimmun. 2019;105:102303. https://doi.org/10.1016/j.jaut.2019.07.002.
Sakthiswary R, Raymond AA. The clinical significance of Vitamin D in systemic lupus erythematosus: a systematic review. PLoS ONE. 2013;8:e55275. https://doi.org/10.1371/journal.pone.0055275.
Parks CG, de Souza Espindola Santos A, Barbhaiya M, Costenbader KH. Understanding the role of environmental factors in the development of systemic lupus erythematosus. Best Pract Res Clin Rheumatol. 2017; 31:306–320. https://doi.org/10.1016/j.berh.2017.09.005.
Yin Q, Wu L-C, Zheng L, Han M-Y, Hu L-Y, Zhao P-P, Bai W-Y, Zhu X-W, Xia J-W, Wang X-B, et al. Comprehensive assessment of the Association between genes on JAK-STAT pathway (IFIH1, TYK2, IL-10) and systemic lupus erythematosus: a meta-analysis. Arch Dermatol Res. 2018;310:711–28. https://doi.org/10.1007/s00403-018-1858-0.
Hu W, Niu G, Lin Y, Chen X, Lin L. Impact of the polymorphism in Vitamin D receptor gene BsmI and the risk of systemic lupus erythematosus: an updated meta-analysis. Clin Rheumatol. 2016;35:927–34. https://doi.org/10.1007/s10067-015-3157-x.
Zhou T-B, Jiang Z-P, Lin Z-J, Su N. Association of Vitamin D receptor gene polymorphism with the risk of systemic lupus erythematosus. J Recept Signal Transduct Res. 2015;35:8–14. https://doi.org/10.3109/10799893.2014.922577.
Xiong J, He Z, Zeng X, Zhang Y, Hu Z. Association of Vitamin D receptor gene polymorphisms with systemic lupus erythematosus: a meta-analysis. Clin Exp Rheumatol. 2014;32:174–81.
Zhang X, Mei D, Zhang L, Wei W. Src family protein kinase controls the fate of B Cells in autoimmune diseases. Inflammation. 2021;44:423–33. https://doi.org/10.1007/s10753-020-01355-1.
Zeng C, Fang C, Weng H, Xu X, Wu T, Li W. B-cell lymphocyte kinase polymorphisms rs13277113, rs2736340, and rs4840568 and risk of autoimmune diseases: a meta-analysis. Medicine. 2017;96:e7855. https://doi.org/10.1097/MD.0000000000007855.
Song GG, Lee YH. Association between BLK polymorphisms and susceptibility to SLE: a meta-analysis. Z Rheumatol. 2017;76:176–82. https://doi.org/10.1007/s00393-016-0072-8.
Lee YH, Harley JB, Nath SK. CTLA-4 polymorphisms and systemic lupus erythematosus (SLE): a meta-analysis. Hum Genet. 2005;116:361–7. https://doi.org/10.1007/s00439-004-1244-1.
Chang W-W, Zhang L, Yao Y-S, Su H. Association between CTLA-4 exon-1 +49A/G polymorphism and systemic lupus erythematosus: an updated analysis. Mol Biol Rep. 2012;39:9159–65. https://doi.org/10.1007/s11033-012-1788-4.
Zhai J-X, Zou L-W, Zhang Z-X, Fan W-J, Wang H-Y, Liu T, Ren Z, Dai R-X, Ye D. CTLA-4 polymorphisms and systemic lupus erythematosus (SLE): a meta-analysis. Mol Biol Rep. 2013;40:5213–23. https://doi.org/10.1007/s11033-012-2125-7.
Yu L, Shao M, Zhou T, Xie H, Wang F, Kong J, Xu S, Shuai Z, Pan F. Association of CTLA-4 (+49 A/G) polymorphism with susceptibility to autoimmune diseases: a meta-analysis with trial sequential analysis. Int Immunopharmacol. 2021;96:107617. https://doi.org/10.1016/j.intimp.2021.107617.
Lee YH, Harley JB, Nath SK. Meta-analysis of TNF-alpha promoter -308 A/G polymorphism and SLE susceptibility. Eur J Hum Genet. 2006;14:364–71. https://doi.org/10.1038/sj.ejhg.5201566.
Zou Y-F, Feng X-L, Tao J-H, Su H, Pan F-M, Liao F-F, Fan Y, Ye D-Q. Meta-Analysis of TNF-α promoter -308A/G polymorphism and SLE susceptibility in Asian populations. Rheumatol Int. 2011;31:1055–64. https://doi.org/10.1007/s00296-010-1392-7.
Pan H-F, Leng R-X, Wang C, Qin W-Z, Chen L-L, Zha Z-Q, Tao J-H, Ye D-Q. Association of TNF-α promoter-308 A/G polymorphism with susceptibility to systemic lupus erythematosus: a meta-analysis. Rheumatol Int. 2012;32:2083–92. https://doi.org/10.1007/s00296-011-1924-9.
Yang Z-C, Xu F, Tang M, Xiong X. Association between TNF-α promoter -308 A/G polymorphism and systemic lupus erythematosus susceptibility: a case-control study and meta-analysis. Scand J Immunol. 2017;85:197–210. https://doi.org/10.1111/sji.12516.
Chen L, Huang Z, Liao Y, Yang B, Zhang J. Association between tumor necrosis factor polymorphisms and rheumatoid arthritis as well as systemic lupus erythematosus: a meta-analysis. Br J Med Biol Res. 2019;52:e7927. https://doi.org/10.1590/1414-431X20187927.
Fan Y, Tao J-H, Zhang L-P, Li L-H, Ye D-Q. The Association between BANK1 and TNFAIP3 gene polymorphisms and systemic lupus erythematosus: a meta-analysis. Int J Immunogenet. 2011;38:151–9. https://doi.org/10.1111/j.1744-313X.2010.00990.x.
Lee YH, Song GG. Associations between TNFAIP3 gene polymorphisms and systemic lupus erythematosus: a meta-analysis. Genet Test Mol Biomarkers. 2012;16:1105–10. https://doi.org/10.1089/gtmb.2012.0096.
Zhang M-Y, Yang X-K, Pan H-F, Ye D-Q. Associations between TNFAIP3 gene polymorphisms and systemic lupus erythematosus risk: an updated meta-analysis. HLA. 2016;88:245–52. https://doi.org/10.1111/tan.12908.
Liu X, Qin H, Wu J, Xu J. Association of TNFAIP3 and TNIP1 polymorphisms with systemic lupus erythematosus risk: a meta-analysis. Gene. 2018;668:155–65. https://doi.org/10.1016/j.gene.2018.05.062.
Lu M-M, Xu W-D, Yang J, Ye Q-L, Feng C-C, Li J, Pan H-F, Tao J-H, Wang J, Ye D-Q. Association of TNFSF4 polymorphisms with systemic lupus erythematosus: a meta-analysis. Mod Rheumatol. 2013;23:686–93. https://doi.org/10.1007/s10165-012-0708-8.
Wang J-M, Yuan Z-C, Huang A-F, Xu W-D. Association of TNFSF4 rs1234315, rs2205960 polymorphisms and systemic lupus erythematosus susceptibility: a meta-analysis. Lupus. 2019;28:1197–204. https://doi.org/10.1177/0961203319862610.
Fu Y, Lin Q, Zhang Z-R. Association of TNFSF4 polymorphisms with systemic lupus erythematosus: a meta-analysis. Adv Rheumatol. 2021;61:59. https://doi.org/10.1186/s42358-021-00215-2.
Moreno-Eutimio MA, Martínez-Alemán CE, Aranda-Uribe IS, Aquino-Jarquin G, Cabello-Gutierrez C, Fragoso JM, Barbosa-Cobos RE, Saavedra MA, Ramírez-Bello J. TNFSF4 is a risk factor to systemic lupus erythematosus in a Latin American population. Clin Rheumatol. 2021;40:929–39. https://doi.org/10.1007/s10067-020-05332-9.
Xu K, Peng H, Zhou M, Wang W, Li R, Zhu K-K, Zhang M, Wen P-F, Pan H-F, Ye D-Q. Association study of TRAF1/C5 polymorphism (rs10818488) with susceptibility to rheumatoid arthritis and systemic lupus erythematosus: a meta-analysis. Gene. 2013;517:46–54. https://doi.org/10.1016/j.gene.2012.12.092.
Zhu L, Chen P, Sun X, Zhang S. Associations between polymorphisms in the IL-1 gene and the risk of rheumatoid arthritis and systemic lupus erythematosus: evidence from a meta-analysis. Int Arch Allergy Immunol. 2021;182:234–42. https://doi.org/10.1159/000510641.
Lee YH, Lee HS, Choi SJ, Ji JD, Song GG. The association between interleukin-6 polymorphisms and systemic lupus erythematosus: a meta-analysis. Lupus. 2012;21:60–7. https://doi.org/10.1177/0961203311422711.
Yang Z, Liang Y, Qin B, Zhong R. A meta-analysis of the association of IL-6 -174 G/C and -572 G/C polymorphisms with systemic lupus erythematosus risk. Rheumatol Int. 2014;34:199–205. https://doi.org/10.1007/s00296-013-2855-4.
Cui YX, Fu CW, Jiang F, Ye LX, Meng W. Association of the interleukin-6 polymorphisms with systemic lupus erythematosus: a meta-analysis. Lupus. 2015;24:1308–17. https://doi.org/10.1177/0961203315588971.
Liu J, Liao M-Q, Cao D-F, Yang Y, Yang Y, Liu Y-H, Zeng F-F, Chen X-H. The association between interleukin-6 gene polymorphisms and risk of systemic lupus erythematosus: a meta-analysis with trial sequential analysis. Immunol Invest. 2021;50:259–72. https://doi.org/10.1080/08820139.2020.1769646.
Wang B, Zhu J-M, Fan Y-G, Xu W-D, Cen H, Pan H-F, Ye D-Q. Association of the -1082G/A polymorphism in the interleukin-10 gene with systemic lupus erythematosus: a meta-analysis. Gene. 2013;519:209–16. https://doi.org/10.1016/j.gene.2013.01.026.
Yuan Y, Wang X, Ren L, Kong Y, Bai J, Yan Y. Associations between interleukin-10 gene polymorphisms and systemic lupus erythematosus risk: a meta-analysis with trial sequential analysis. Clin Exp Rheumatol. 2019;37:242–53.
Chen S, Jiang F, Ren J, Liu J, Meng W. Association of IL-18 polymorphisms with rheumatoid arthritis and systemic lupus erythematosus in Asian populations: a meta-analysis. BMC Med Genet. 2012;13:107. https://doi.org/10.1186/1471-2350-13-107.
Wen D, Liu J, Du X, Dong J-Z, Ma C-S. Association of interleukin-18 (-137G/C) polymorphism with rheumatoid arthritis and systemic lupus erythematosus: a meta-analysis. Int Rev Immunol. 2014;33:34–44. https://doi.org/10.3109/08830185.2013.816699.
Niu Z, Zhang P, Tong Y. Value of HLA-DR genotype in systemic lupus erythematosus and lupus nephritis: a meta-analysis. Int J Rheum Dis. 2015;18:17–28. https://doi.org/10.1111/1756-185X.12528.
Xue K, Niu W-Q, Cui Y. Association of HLA-DR3 and HLA-DR15 polymorphisms with risk of systemic lupus erythematosus. Chin Med J (Engl). 2018;131:2844–51. https://doi.org/10.4103/0366-6999.246058.
Xu W-D, Pan H-F, Xu Y, Ye D-Q. interferon regulatory factor 5 and autoimmune lupus. Expert Rev Mol Med. 2013;15:e6. https://doi.org/10.1017/erm.2013.7.
Hu W, Ren H. A meta-analysis of the association of IRF5 polymorphism with systemic lupus erythematosus. Int J Immunogenet. 2011;38:411–7. https://doi.org/10.1111/j.1744-313X.2011.01025.x.
Wang J-M, Huang A-F, Yuan Z-C, Su L-C, Xu W-D. Association of IRF5 rs2004640 polymorphism and systemic lupus erythematosus: a meta-analysis. Int J Rheum Dis. 2019;22:1598–606. https://doi.org/10.1111/1756-185X.13654.
Li Y, Chen S, Li P, Wu Z, Li J, Liu B, Zhang F, Li Y. Association of the IRF5 rs2070197 polymorphism with systemic lupus erythematosus: a meta-analysis. Clin Rheumatol. 2015;34:1495–501. https://doi.org/10.1007/s10067-015-3036-5.
Ji JD, Lee WJ, Kong KA, Woo JH, Choi SJ, Lee YH, Song GG. Association of STAT4 polymorphism with rheumatoid arthritis and systemic lupus erythematosus: a meta-analysis. Mol Biol Rep. 2010;37:141–7. https://doi.org/10.1007/s11033-009-9553-z.
Yuan H, Feng J-B, Pan H-F, Qiu L-X, Li L-H, Zhang N, Ye D-Q. A meta-analysis of the association of STAT4 polymorphism with systemic lupus erythematosus. Mod Rheumatol. 2010;20:257–62. https://doi.org/10.1007/s10165-010-0275-9.
Wang J-M, Xu W-D, Huang A-F. Association of STAT4 gene rs7574865, rs10168266 polymorphisms and systemic lupus erythematosus susceptibility: a meta-analysis. Immunol Invest. 2021;50:282–94. https://doi.org/10.1080/08820139.2020.1752712.
Lee YH, Bae S-C. The miR-146a polymorphism and susceptibility to systemic lupus erythematosus and rheumatoid arthritis: a meta-analysis. Z Rheumatol. 2015;74:153–6. https://doi.org/10.1007/s00393-014-1509-6.
Sun H-Y, Lv A-K, Yao H. Relationship of miRNA-146a to Primary Sjögren’s Syndrome and to Systemic Lupus Erythematosus: A Meta-Analysis. Rheumatol Int. 2017;37:1311–6. https://doi.org/10.1007/s00296-017-3756-8.
Ji JD, Cha ES, Lee WJ. Association of MiR-146a polymorphisms with systemic lupus erythematosus: a meta-analysis. Lupus. 2014;23:1023–30. https://doi.org/10.1177/0961203314534512.
Fu L, Jin L, Yan L, Shi J, Wang H, Zhou B, Wu X. Comprehensive review of genetic association studies and meta-analysis on miRNA polymorphisms and rheumatoid arthritis and systemic lupus erythematosus susceptibility. Hum Immunol. 2016;77:1–6. https://doi.org/10.1016/j.humimm.2014.09.002.
Liu F, Liang Y, Zhao Y, Chen L, Wang X, Zhang C. Meta-analysis of association of microRNAs genetic variants with susceptibility to rheumatoid arthritis and systemic lupus erythematosus. Medicine. 2021;100:e25689. https://doi.org/10.1097/MD.0000000000025689.
Ebrahimiyan H, Mostafaei S, Aslani S, Faezi ST, Farhadi E, Jamshidi A, Mahmoudi M. Association between complement gene polymorphisms and systemic lupus erythematosus: a systematic review and meta-analysis. Clin Exp Med. 2021. https://doi.org/10.1007/s10238-021-00758-0.
Fan Y, Li L-H, Pan H-F, Tao J-H, Sun Z-Q, Ye D-Q. Association of ITGAM polymorphism with systemic lupus erythematosus: a meta-analysis. J Eur Acad Dermatol Venereol. 2011;25:271–5. https://doi.org/10.1111/j.1468-3083.2010.03776.x.
Ye D, Sun X, Guo Y, Shao K, Qian Y, Huang H, Liu B, Wen C, Mao Y. Genetically determined selenium concentrations and risk for autoimmune diseases. Nutrition. 2021;91–92:111391. https://doi.org/10.1016/j.nut.2021.111391.
Ye D, Zhu Z, Huang H, Sun X, Liu B, Xu X, He Z, Li S, Wen C, Mao Y. Genetically predicted serum iron status is associated with altered risk of systemic lupus erythematosus among european populations. J Nutr. 2021;151:1473–8. https://doi.org/10.1093/jn/nxab015.
Ye D, Liu B, He Z, Huang L, Qian Y, Shao K, Wen C, Mao Y. Assessing the associations of growth differentiation factor 15 with rheumatic diseases using genetic data. Clin Epidemiol. 2021;13:245–52. https://doi.org/10.2147/CLEP.S305024.
Dan Y-L, Wang P, Cheng Z, Wu Q, Wang X-R, Wang D-G, Pan H-F. Circulating adiponectin levels and systemic lupus erythematosus: a two-sample mendelian randomization study. Rheumatology. 2021;60:940–6. https://doi.org/10.1093/rheumatology/keaa506.
Xiang K, Wang P, Xu Z, Hu Y-Q, He Y-S, Chen Y, Feng Y-T, Yin K-J, Huang J-X, Wang J, et al. Causal effects of gut microbiome on systemic lupus erythematosus: a two-sample Mendelian randomization study. Front Immunol. 2021;12:667097. https://doi.org/10.3389/fimmu.2021.667097.
Yang G, Schooling CM. Investigating genetically mimicked effects of statins via HMGCR inhibition on immune-related diseases in men and women using Mendelian randomization. Sci Rep. 2021;11:23416. https://doi.org/10.1038/s41598-021-02981-x.
Bae S-C, Lee YH. Causal association between periodontitis and risk of rheumatoid arthritis and systemic lupus erythematosus: a Mendelian randomization. Z Rheumatol. 2020;79:929–36. https://doi.org/10.1007/s00393-019-00742-w.
Bae S-C, Lee YH. Vitamin D level and risk of systemic lupus erythematosus and rheumatoid arthritis: a Mendelian randomization. Clin Rheumatol. 2018;37:2415–21. https://doi.org/10.1007/s10067-018-4152-9.
Bae S-C, Lee YH. Coffee consumption and the risk of rheumatoid arthritis and systemic lupus erythematosus: a Mendelian randomization study. Clin Rheumatol. 2018;37:2875–9. https://doi.org/10.1007/s10067-018-4278-9.
Bae SC, Lee YH. Alcohol intake and risk of systemic lupus erythematosus: a Mendelian randomization study. Lupus. 2019;28:174–80. https://doi.org/10.1177/0961203318817832.
Inamo J. Association between celiac disease and systemic lupus erythematosus: a mendelian randomization study. Rheumatology. 2020;59:2642–4. https://doi.org/10.1093/rheumatology/keaa071.
Wang P, Dan Y-L, Wu Q, Tao S-S, Yang X-K, Wang D-G, Ye D-Q, Shuai Z-W, Pan H-F. Non-causal effects of smoking and alcohol use on the risk of systemic lupus erythematosus. Autoimmun Rev. 2021;20:102890. https://doi.org/10.1016/j.autrev.2021.102890.
Basta F, Fasola F, Triantafyllias K, Schwarting A. Systemic lupus erythematosus (SLE) therapy: the old and the new. Rheumatol Ther. 2020;7:433–46. https://doi.org/10.1007/s40744-020-00212-9.
Acknowledgements
Not applicable.
Funding
Hui Zheng received a grant from the Sichuan Youth Science and Technology Innovation Research Team (No. 2021JDTD0007).
Author information
Authors and Affiliations
Contributions
All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: HZ. Acquisition, analysis, or interpretation of data: X-YX, QC, Y-ZS, L-WL, and CH. Drafting of the manuscript: X-YX. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: X-YX and HZ. Administrative, technical, or material support: HZ. Supervision: HZ.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A: search strategy
PubMed
Systematic review
#1 “Lupus Erythematosus, Systemic”[Mesh]OR Systemic lupus erythematosus OR Systemic Lupus Erythematosus OR Lupus Erythematosus Disseminatus OR Libman-Sacks Disease OR Disease, Libman-Sacks OR Libman Sacks Disease.
#2 risk factor[MeSH Terms] OR Factor, Risk OR Risk Factor OR Social Risk Factors OR Factor, Social Risk OR Factors, Social Risk OR Risk Factor, Social OR Risk Factors, Social OR Social Risk Factor OR Health Correlates OR Correlates, Health OR Population at Risk OR Populations at Risk OR Risk Scores OR Risk Score OR Score, Risk OR Risk Factor Scores OR Risk Factor Score OR Score, Risk Factor.
#3 #1 AND #2 AND (meta-analysis[Filter] OR systematic review[Filter]).
Mendelian randomization study
#1 “Lupus Erythematosus, Systemic”[Mesh]OR Systemic lupus erythematosus OR Systemic Lupus Erythematosus OR Lupus Erythematosus Disseminatus OR Libman-Sacks Disease OR Disease, Libman-Sacks OR Libman Sacks Disease.
#2 Mendelian Randomization Analysis [MeSH Terms].
#3 #1 AND #2.
Embase
Systematic review
#1’systemic lupus erythematosus':ti,ab,kw OR sle:ti,ab,kw.
#2’risk factors':ti,ab,kw OR 'risk factor':ti,ab,kw.
#3’systematic review':ti,ab,kw OR 'meta analysis':ti,ab,kw.
#4 #1 AND #2
#5 #4 AND #3.
Mendelian randomization study
#1'systemic lupus erythematosus':ti,ab,kw OR sle:ti,ab,kw.
#2'mendelian randomization analysis':ti,ab,kw OR 'mendelian randomization study':ti,ab,kw OR 'mendelian randomization':ti,ab,kw.
#3 #1 AND #2.
Appendix B: AMSTAR-2 scale for the assessment of systematic reviews
Study ID | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | Methodological quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Agrawal [25] | N | Y | Y | Y | Y | Y | N | Y | PY | N | NM | N | NM | Y | NM | Y | Low |
Chua [21] | N | N | Y | PY | Y | Y | N | PY | PY | N | Y | Y | Y | Y | Y | N | Critically low |
Costenbader [18] | N | N | Y | PY | Y | Y | N | PY | PY | N | Y | Y | Y | Y | Y | N | Critically low |
Janowsky [23] | N | N | N | PY | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Critically low |
Jiang [19] | Y | N | Y | PY | N | Y | N | PY | PY | N | Y | Y | Y | Y | Y | N | Critically low |
Parisis [20] | N | N | Y | N | Y | Y | Y | PY | Y | N | Y | Y | N | Y | Y | Y | Critically low |
Ponvilawan [11] | N | N | Y | PY | Y | N | N | PY | N | N | NM | N | N | Y | Y | Y | Critically low |
Rees [2] | N | N | N | Y | N | N | N | Y | N | N | NM | NM | Y | Y | NM | Y | Critically low |
Sakthiswary [26] | N | N | Y | PY | Y | N | Y | PY | PY | N | NM | NM | Y | Y | NM | Y | Critically low |
Shigesi [5] | N | Y | Y | PY | Y | Y | Y | PY | PY | N | Y | Y | Y | Y | Y | Y | Moderate |
Wang (22) | Y | Y | Y | PY | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High |
Wang [17] | Y | N | Y | PY | Y | Y | N | Y | Y | N | Y | Y | Y | Y | Y | Y | Critically low |
Wongtrakul [12] | N | N | Y | PY | Y | Y | N | PY | N | N | Y | Y | Y | N | Y | N | Critically low |
Youssefi [24] | N | N | Y | PY | Y | N | N | PY | N | N | N | N | N | Y | N | Y | Critically low |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xiao, XY., Chen, Q., Shi, YZ. et al. Risk factors of systemic lupus erythematosus: an overview of systematic reviews and Mendelian randomization studies. Adv Rheumatol 63, 42 (2023). https://doi.org/10.1186/s42358-023-00323-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-023-00323-1