Abstract
Background
Pain, inflammation and fever are serious conditions that are associated with various disease conditions. In modern medicine, non-steroidal anti-inflammatory drugs (NSAIDs), opioids together with corticosteroids have been considered to manage algesia and inflammation-related conditions. However, these conventional drugs are not affordable, not readily available, particularly to people living in rural areas in developing nations. Besides, they are associated with undesirable pharmacological actions. Generally, medicinal plants have been employed to manage various ailments. In Northern-Nigeria, the leaves of Culcasia angolensis (Araceae) are used traditionally to manage pain, fever and inflammation. However, scientific data validating its folkloric claim in treating pain and inflammatory-related abnormalities are not available. Hence, the current study aims to validate the antinociceptive, anti-inflammatory and antipyretic potentials of the methanol leaf extract of Culcasia angolensis (MECA). Phytochemical and acute toxicity effects of the MECA were conducted as per standard experimental procedures. The analgesic potential of the MECA was determined using abdominal writhing elicited by acetic acid and hot plate tests in mice. The actions of the MECA on acute inflammation were conducted using formalin-induced hind paw oedema and carrageenan-induced paw oedema. The Brewer's yeast-induced pyrexia was employed to check its antipyretic effect.
Results
The MECA inhibited abdominal writhes produced by acetic acid administration (p < 0.05) and elevated the pain threshold in the hot plate test. The MECA also reduced the formalin-induced paw oedema. Besides, it produced an effective (p < 0.05) and dose-dependent action against oedema produced by carrageenan and reduced the rectal temperature against the pyrexia caused by Brewer's yeast administration.
Conclusions
The outcome of the study suggests that the MECA could possess pharmacologically active constituents with antinociceptive, anti-inflammatory and antipyretic properties. Therefore, the results justified its ethnomedicinal use to manage pain and inflammatory-associated conditions.
Similar content being viewed by others
Background
Pain can be defined as a disturbing and emotional sensation related to actual or potential damage to body tissues (Fan et al., 2014). The perception of pain could be stimulated by thermal, electrical, biological and chemical stimuli via peripheral pain receptors at the optimum threshold to induce tissue damage (Prasanth et al., 2015). Inflammation is a complicated response to protect the body from injurious agents, including microbes, physical trauma and chemical irritants clinically manifested as heat, redness, swelling and pain (Bleakley & Davison, 2011; Cássia et al., 2013). It composes series of biological and chemical reactions in the body that affects the blood vessels, immunology and different cells around the injured tissue (Ferrero-Miliani et al., 2006). The inflammatory process contributes to protecting the body against an injurious agent (Cássia et al., 2013). Chronic inflammation is associated with many pathological ailments such as cardiovascular system diseases, diabetes mellitus, cancer, arthritis, Alzheimer's disease, pulmonary disease and many more (Ugwu et al., 2018). Pain and inflammation serve as non-specific indications for various pathological disorders (Shojaii et al., 2015). Approximately 30% of the adults globally are disturbed seriously by pain and inflammation related ailments, out of which 20% suffer from chronic diseases (Javed et al., 2020).
Pyrexia (fever) refers to an elevation in the body temperature beyond the homeostatic level as a result of stressful conditions such as ovulation, elevated thyroid hormone secretion, tedious exercise, lesion of the central nervous system (CNS) and infectious agents (Sultana et al., 2015). The human immune system is activated in response to infectious agents to provide an undesirable environment for the microbial agents. Pyrexia usually causes an elevation in the production and secretion of pro-inflammatory biomarkers, namely, interleukin (IL)-1β, IL-α and tissue necrosis factor (TNF)-α, that stimulate prostaglandin (PG) formation and eventually enhance the body temperature (Sultana et al., 2015).
The most commonly utilised analgesic, anti-inflammatory and antipyretic agents prevent PG biosynthesis by inhibiting the cyclooxygenase (COX) enzymes and are accompanied by many pharmacological setbacks (Luo et al., 2018; Sultana et al., 2015). For instance, non-steroidal anti-inflammatory drugs (NSAIDs) produce gastrointestinal disturbances (gastric haemorrhage, ulcer, and perforation), hypertension, liver and kidney damage. Also, opioid analgesic agents result in drowsiness, nausea, vomiting, constipation, respiratory depression, drug addiction, dependence and tolerance (Kumar Manna Ashis, 2009; Luo et al., 2018). Besides, steroids used against chronic inflammatory disorders are associated with adverse drug reactions such as hyperglycaemia, impaired wound healing, increased microbial infection, hypertension, osteoporosis, cognitive deficit and many more (Poetker & Reh, 2010).
Naturally occurring substances have immensely contributed to the progression of orthodox medicine in the prevention and management of many ailments (Alhakmi et al., 2013; Chandra et al., 2012). It has been shown that greater than 80% of the people living in economically limited nations utilize traditional herbal preparations to manage their basic illnesses due to easy accessibility, affordability and perception of their safety (Alhakmi et al., 2013). Therefore, it is vital to increase more efforts to discover more efficacious and affordable drugs of plant origin (Kakoti et al., 2013). Besides, several plant-obtained products have been scientifically validated to possess antinociceptive and anti-inflammatory potentials (Mueller et al., 2010). Therefore, there is a strong need for more researches in complementary and alternative medicine to discover and develop novel, safe and efficacious antinociceptive and anti-inflammatory compounds (Kumar et al., 2015; Zulfiker et al., 2010).
Culcasia angolensis (Araceae) is a robust forest climber with stems that grow above 30 m long. The stems are thick and tough of about 6 cm in diameter that adheres to the host trees through clasping roots (Burkil, 1985). The plant is commonly found in tropical African countries such as Sierra Leone, Cameroon and Angola. The plant is known in English as greater climbing, in Ivory Coast as Kyama, in Ghana as Akan-asante (Burkil, 1985). It is also referred to as Hyrmim in Ham language by the people of Jaba Local Government Area of Kaduna State, Nigeria.
The whole plant is harvested from the wild environment for local use in traditional medicine. The leaves of Culcasia angolensis have been used effectively in treating menstrual problems in Africa (Bown, 2000). Besides, the leaves of Culcasia angolensis have been used to manage pain and inflammation in the Northern part of Nigeria. However, scientific information is not available in the literature to validate the antinociceptive, anti-inflammatory and antipyretic actions of the plant. Therefore, the current research investigates the actions of methanol leaves extract of Culcasia angolensis (MECA) in laboratory animal models of pain, inflammation and pyrexia.
Methods
Collection and authentication of the Culcasia angolensis
The Culcasia angolensis was sourced in April, 2020, from Ngaring Nok, Jaba Local Government of Kaduna State, Nigeria. The authentication and identification of the plant were conducted by Mallam Namadi Sanusi at the Herbarium facility of the Botany Department, Faculty of Life Sciences, Ahmadu Bello University (ABU), Zaria, Nigeria. The plant was compared with an existing specimen previously kept at the herbarium (voucher number: 01676).
Laboratory animals
Swiss albino mice of both genders (18–22 g) and adult Wistar rats (160–200 g) utilized for the research were sourced from the animal house section, Department of Pharmacology and Therapeutics, ABU Zaria. They were kept in clean, dried, adequately ventilated polypropylene cages with sufficient and standard laboratory feed (Vital feed, Jos, Nigeria) and water at optimum laboratory environment (room temperature 22 ± 3 °C, relative humidity 30–70% with 12-h light and 12-h dark). The animals were kept for two weeks in order to acclimatise to the laboratory condition before the research activities commenced. The approval for the conduct of the experiment was granted by ABU Ethical Committee on Animal Use and Care Research Policy (ABUCAUC) with a permission number (ABUCAUC/2019/006) and done as per the ARRIVE (Animal Research: Reporting of In Vivo Experiments) guidelines. At the end of the experiment, the animals were anaesthetised with chloroform and euthanized by cervical dislocation. Thereafter, they were buried appropriately based on the University guide of disposing the remains of laboratory animals.
Drugs and chemicals
Acetic acid (Searle Essex, England), formalin, Ketoprofen (Lek Pharmaceuticals company Ltd, Slovenia), normal saline, Brewer's yeast (Angel Yeast Company, China), methanol, carrageenan and morphine (Sigma-Aldrich chemical company, USA).
Plant extraction
The leaves of Culcasia angolensis were dried in a shaded environment and frequently weighed until a standard weight was obtained. The dried leaves were then size-reduced with mortar and pestle. The size-reduced leaves (1500 g) were extracted with 70%v/v methanol with the aid of soxhlet apparatus for 72-h and concentrated at reduced pressure (temperature of 45 °C) on a water bath and subsequently packed in a closed container. An aqueous solution of the extract was prepared with normal saline for each experimental procedure.
Phytochemical investigation
The phytochemical determination to check the possible presence of secondary metabolites in MECA was conducted as per the methods described by Sofowora (1993).
Acute toxicity investigation
The acute toxic actions of the MECA were investigated in rats and mice as per the protocol stated by the Organization of Economic Co-operation and Development (OECD) 423 (OECD, 2001). The oral median lethal dose (LD50) was investigated after the oral administration of the MECA to nulliparous and non-pregnant female rats and mice. Two groups containing three animals (rats and mice separately in different groups) were fasted before the extract administration (food was withheld overnight for rats and 3 h for mice with the provision of water sufficiently). In the first phase, 2000 mg/kg of the MECA was administered to each of the rats and mice and checked for 48-h for any sign of toxicity, including mortality. In the second phase, 5000 mg/kg of the MECA was used, and the rodents were also checked for signs of toxicity one time every 30 min within the first 4-h and subsequently for 14-consecutive days.
Analgesic activity of MECA
Acetic acid-induced abdominal constrictions test
The experimental procedure reported by Okpo et al. (2001) was employed. Thirty (30) mice were categorised at random into five groups (n = 6). The 1st group received normal saline (10 ml/kg), whereas the mice in the 2nd, 3rd, and 4th groups received the MECA at a graded dose (125, 250 and 500 mg/kg), respectively, via oral route. The group 5 animals received standard analgesic compound piroxicam (20 mg/kg) orally (Tanko et al., 2008). Sixty minutes after the treatment mentioned above, all the mice in all the groups received 0.6% v/v of acetic acid (10 ml/kg) via the intraperitoneal route and placed individually in cages. Then, 5 min following the acetic acid injection, the number of abdominal constrictions (stretching of at least one of the hind limbs) was counted for each mouse for 10 min. A decline in the number of the abdominal constrictions related to the normal saline-treated group was recorded as an index of analgesic action and represented as percent inhibition of abdominal constrictions using the following relation:
Hot plate (thermal sensitivity) test
The procedure previously employed by Okolo et al. (1995) was utilised. Thirty (30) mice were categorised at random into five groups (n = 6). The group 1 mice received normal saline (10 ml/kg), and group 5 received the standard analgesic agent morphine (10 mg/kg) orally. Group 2, 3 and 4 received the MECA at a graded dose (125, 250, and 500 mg/kg) via the oral route, respectively. Sixty minutes after the treatment, the mice were placed individually on a hot plate which was set at a temperature of (45 ± 1 °C) for 20 s. The pain response latency (The time immediately after placement of the mice up to the hot plate to the time it licked its paw or jumped off the plate) was observed and recorded at 0, 60, 90, 120 and 150 min. The increase in the pain latency time was considered as an analgesic action.
Anti-inflammatory activity of MECA
Formalin-induced hind-paw oedema
The procedure previously reported by Dubuisson and Dennis (1977) and modified by Tjolsen et al. (1992) was utilised for the study. Thirty adult Wistar rats were categorised at random into five groups (n = 6). They were fasted for 24-h before the commencement of the research process with provision of water ad libitum. The mice in group 1 (negative control) received normal saline (10 m/kg). The 2nd, 3rd, and 4th groups rats received the MECA (125, 250 and 500 mg/kg) orally, respectively, while the 5th group rats received ketoprofen (10 mg/kg) via the intraperitoneal route. 30 min post-treatment, 0.05 ml solution of formalin (2.5% formaldehyde) was administered subcutaneously into the plantar surface of the left hind paw of each rat. Then, the paw diameter was measured with vernier calliper at 0, 1, 2, 3, 4 and 5 h after the formalin administration.
Carrageenan-induced paw oedema
The protocol previously conducted by Winter et al. (1962) and Magaji et al. (2007) was adopted. Thirty adult Wistar rats were randomly categorised into five groups (n = 6). The 1st group received normal saline (10 ml/kg), and the 5th group received ketoprofen (10 mg/kg). The 2nd, 3rd, and 4th groups received the MECA at a graded dose (125, 250 and 500 mg/kg), respectively, via the oral route. Sixty minutes after the above-mentioned treatment, the rat in each group was injected with 1% carrageenan (0.1 ml) into the sub-plantar surface of the rat right hind paw. The oedema diameter was measured at 0, 1, 2, 3, 4 and 5 h with the aid of vernier calliper. The increase in paw diameter was calculated as the difference in paw diameter before and after administration of the carrageenan at each time interval. Besides, the percentage inhibition of oedema was calculated for each animal group with respect to the negative control group as follows:
Antipyretic activity of MECA
Brewer's yeast-induced pyrexia
The procedure previously reported by Loux et al. (1972) was employed. Thirty adult rats of both genders were selected and randomised into five groups (n = 6). The rectal temperature of each rat was checked using the rectal thermometer. The fever was stimulated in each rat by administering 20% Brewer's yeast suspension (20 ml/kg) subcutaneously on the back of each rat just under the nape of the neck. Following the yeast injection, food was withheld. Eighteen (18) hours later, the rectal temperature was then measured and recorded for each of the animals, which was repeated after 30 min, and only rats with at least 0.5 °C rise in body temperature were selected for the study. The rats in the 1st group were administered normal saline (10 ml/kg) orally, whereas group 5 received standard antipyretic agent acetaminophen (150 mg/kg) via the intraperitoneal route, respectively (Balamurugan et al., 2009). The rats in the 2nd, 3rd, and 4th groups received the MECA (125, 250, and 500 mg/kg), respectively, via the oral route. The rectal temperature of each rat was taken at 0, 1, 2 and 3 h after the treatment.
Statistical analysis
All the results were presented as mean values ± standard error of the mean (SEM) in figures and tables. One-way analysis of variance (ANOVA) was used to analyse the abdominal constriction induced by acetic acid test results. However, repeated measure ANOVA was performed to analyse the results of hot plate test, formalin-induced paw oedema, paw oedema produced by carrageenan models and fever caused by Brewer's yeast followed by Bonferroni post hoc test. The result was taken significant at p ≤ 0.05.
Results
Extractive value of MECA
A sticky black solid extract (107.6 g) was obtained from 1500 g of the powdered leaf of the Culcasia angolensis sample, representing a percentage yield of 7.20% w/w.
Phytochemical constituents
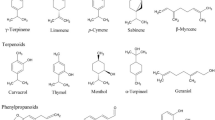
Preliminary phytochemical investigation of MECA showed carbohydrates, cardiac glycosides, triterpenes, saponins, tannins, flavonoids, steroids and alkaloids.
Acute toxicity study
After administering the MECA via oral route to both mice and rats, there were no mortality and obvious signs of toxic effects at the 2000 and 5000 mg/kg. Therefore, the oral LD50 of the MECA was more than 5000 mg/kg.
Action of MECA on acetic acid-induced writhes test
The MECA remarkably (p < 0.05) declined the frequency of abdominal constrictions dose-dependently. Also, the piroxicam used as the standard agent elicited significant reduction (p ≤ 0.001) in the number of abdominal writhes. There was no significant difference in the number of abdominal constrictions in the extract-treated groups and the standard drug. Besides, the MECA elicited the highest action at the dose of 500 mg/kg in a similar way to the piroxicam. Figure 1 shows the effect of the MECA on the abdominal constriction.
Action of the MECA on hot plate test
The MECA remarkably (p < 0.05) increased the mean reaction time at 90, 120 and 150 min relative to the control group. It produced a dose-dependent increase in the mean reaction time to the thermal pain at 120 and 150 min compared to the normal saline-treated group. Also, the morphine (10 mg/kg) used as the standard agent elicited significant elevation (p ≤ 0.01) in the mean reaction time at 60, 90, 120 and 150 min. There was no significant difference in the mean reaction time to the thermal pain perception between the MECA-treated groups and the morphine. In fact, the MECA exerted a remarkable (p < 0.01) elevation in the mean reaction time similar to the morphine (10 mg/kg) at 120 and 150 min post-treatment. The action of MECA on thermally induced pain is presented in Table 1
Actions of MECA on formalin-induced hind-paw oedema
The MECA at all the doses (125, 250 and 500 mg/kg) and ketoprofen exerted a remarkable (p < 0.001) decline in the paw oedema exerted by formalin at the fourth and fifth hours post-treatments comparable to the control. There was no significant difference in the paw oedema between the extract-treated groups and the standard drug used (ketoprofen). In fact, the effect of the extract was comparable to the standard agent. The action of the MECA on formalin-induced nociception is presented in Table 2.
The actions of the MECA on carrageenan-induced paw oedema
The MECA (125, 250 and 500 mg/kg) exerted a dose-dependent declined in the carrageenan-induced paw oedema at the third (9.6%, 30.4%, 48.9%), fourth (28.4%, 51.5%, 60.4%) and fifth (27.3%, 54.5%, 63.6%) hours, which was significant (p < 0.001) at 250 and 500 mg/kg compared to the control group. In comparison with the normal saline-treated group, ketoprofen (10 mg/kg) exerted remarkable (p ≤ 0.01 and p < 0.001) reduction in the carrageenan-induced paw oedema. There was no significant difference observed in the mean paw diameter between the MECA-treated groups and the standard agents. The result of the action of the MECA on paw oedema elicited by carrageenan is presented in Table 3.
Effect of MECA on Brewer's yeast-induced pyrexia
There was an elevation in the rats' rectum temperature in all the treated groups 18-h post administration of the Brewer's yeast. Zero hour was taken as the baseline for all the treatment groups and was compared with 1, 2 and 3 h. The extract showed a dose-depended reduction in the temperature at the second hour which was significant (p ≤ 0.05) at the highest dose (500 mg/kg). The MECA at all the doses remarkably (p ≤ 0.05) declined the rectal temperature at the third hour in a dose-dependent manner. Besides, the paracetamol (150 mg/kg) used as the standard antipyretic agent significantly (p ≤ 0.01) lowered the temperature when compared to the control group. The highest effect was seen in the group that received the MECA at 500 mg/kg, similar to the effect exerted by the standard antipyretic agent at the third hour. There was no statistical significant difference in rectal temperature of the MECA-treated groups (125, 250, and 500 mg/kg) and paracetamol (150 mg/kg). The action of the MECA on the fever induced by Brewer's yeast is shown in Table 4.
Discussion
Therapeutic compounds from herbal sources have drawn the scientific community's attention and people for use against various diseases. Several medicinal plants have been reported to possess chemical compounds to prevent and manage pain as well as inflammation-related disorders (Bahmani et al., 2014). Due to the possible adverse drug reactions and low efficacy of the currently available therapeutic compounds for treating pain and inflammation, the use of herbal products in complementary medicine has been on the increase to control pain and inflammation (Nasri & Shirzad, 2013). The plant Culcasia angolensis has been utilised in Northern-Nigeria for pain and inflammation. Therefore, the current experiment checked the antinociceptive, anti-inflammatory, and antipyretic actions of its leaves extract to justify its traditional claim and propose for further research to develop safe and effective therapeutic agents for use against pain and inflammation disorders.
The acute toxic effect evaluation is utilised to determine the potentially noxious effects of chemical substances following acute administration (Musila et al., 2017). In the screening of pharmacological activity of a chemically undefined compound, the acute toxic effect is the initial procedure, especially the investigation of LD50 of the compound (Kpemissi et al., 2020). Besides, the test is essential in searching for the biological effects of therapeutic compounds (Ugwah-oguejiofor et al., 2019). After acute administration of a compound via oral route at 5000 mg/kg, if there is an absence of signs of harmful effects and loss of lives of the animals following 14 days observational period, the chemical substance could be safe, and the LD50 could be estimated to be more than 5 g/kg (Qin et al., 2009). Therefore, the findings in the current study have shown that the LD50 of the MECA orally could be more than 5000 mg/kg. Previous research reported by Ahmad et al. (2020a, 2020b) revealed that the oral LD50 of Combretum hypopilinum was higher than 5000 mg/kg. In another study by Yerima et al. (2014), the oral LD50 of the Tamarindus indica bark was also greater than 5000 mg/kg. Besides, Toma et al. (2015) reported the oral LD50 of roots extract of Echinops kebericho to be above 5000 mg/kg.
The constriction of mice abdomen elicited by the injection of acetic acid is a sensitive experimental protocol frequently utilized to investigate the potential peripherally and centrally acting antinociceptive agents. This pharmacological model of nociception is highly sensitive and capable of detecting the analgesic activity of compounds at doses that may be ineffective with other pain models (Kakoti et al., 2013). Acetic acid is known to stimulate COX enzymes that mediate the conversion of arachidonic acid to prostaglandins, the potent mediator of pain and inflammation. NSAIDs abolish abdominal constrictions caused by acetic acid by inhibiting COX activity peripherally and eventually block the production and release of chemical mediators involved in inflammation (Donkor et al., 2013). Besides, the administration of acetic acid stimulates nociceptors and promotes hyperalgesia by mediating the synthesis and release of noxious endogenous chemical substances, including PG, bradykinins, substance P, histamine, serotonin and cytokines that sensitise pain receptors at the nerve terminal end (Pacheco et al., 2019). From the finding in this research, the MECA could have therefore elicited its analgesic action by attenuating the synthesis and activity of COX peripherally and subsequently blocked the production and release of pain and inflammatory chemical agents such as PGE2, bradykinins, histamine, serotonin, substance P as well as cytokines. Recent research by Jo et al. (2021) demonstrated the abdominal writhing inhibitory action of Aucklandia lappa root extract produced by acetic acid. In another study by Josabad et al. (2021), Cuphea aequipetala exerted a dose-dependent effect against acetic acid-produced abdominal constriction. In a previous experiment by Zakaria et al. (2018), the Nigella Sativa and Eucheuma cottonii extracts remarkably abolished the frequency of abdominal writhes exerted by the acetic acid.
Hot plate model as a thermally induced pain stimulus is frequently employed to determine the potential centrally acting analgesic compounds that produce analgesic actions by pharmacological interactions with opioidergic receptors in the CNS (Ermilo et al., 2020). The model comprises the neurogenic and central mechanisms of pain at the supraspinal and spinal levels (Taher et al., 2015). The opioid analgesic agents, such as morphine, alleviate pain by elevating the pain threshold level at the spinal cord and change the brain's perception of pain via interaction with mu (µ) opioid receptors. Besides, kappa (ƙ) receptors in the spinal cord also contribute to the antinociceptive action (Angst & Clark, 2006). Based on the outcome in this research, the MECA considerably prolonged the reaction time to the thermal stimulus, suggestive of a central antinociceptive mechanism. Several medicinal plants have been reported to possess analgesic action in hot plate test. For example, Javed et al. (2020) reported an analgesic action of Indigofera argentea on the hot plate model. The methanol stem extract of Diplotropis purpurea elicited an analgesic action in the hot plate model (Cruz et al., 2019). In accordance with the experiment by Rahman et al. (2020), the seed of Holarrhena antidysenterica exerted a dose-dependent elevation in the pain latency in thermally induced pain. In contrast, the ethanol extract of Senna septemtrionalis did not affect the pain latency (Ermilo et al., 2020). The capability of the MECA to attenuate the pain in the acetic acid-induced abdominal constriction and hot plate models indicates further that its antinociceptive activity could be via many processes that combine peripheral and central pain pathways.
The formalin-induced paw oedema is among the most commonly used models to check agents' anti-inflammatory ability (Soyocak et al., 2019). The model is used to validate both centrally and peripherally acting pain-relieving agents such as narcotics and acetylsalicylic acid, respectively. Formalin produces pain by mediating the release of substance P centrally and stimulating the terminal end of pain receptors. It also activates the release of histamine, serotonin, PG and bradykinin, as well as sensitisation of the spinal cord (Fabiana et al., 2018). Therefore, the MECA could possess its pain attenuating action by antagonizing the release of histamine, substance P, serotonin, PG, and bradykinin responsible for hyperalgesia. Similar research by Helal et al. (2020) has shown the capability of the Leea macrophylla to minimise the formalin-induced paw oedema.
Carrageenan-induced inflammation happens to be the most commonly used animal model to check the anti-inflammatory actions of phytocompounds (Taher et al., 2015). The model is vital in determining the oedema-inhibitory effects of pharmacological agents that act via inhibiting several inflammatory as well as pro-inflammatory chemical substances such as PG, histamine, leukotrienes, bradykinin and TNF-α (Rosas et al., 2019; Taher, 2012). It is an accepted test used to validate the anti-inflammatory actions of biological agents (Vongtau et al., 2004). Carrageenan is a phlogistic and non-antigenic agent with no apparent systemic effect. The administration of the carrageenan activates the kinin system, stimulate the neutrophils accumulation, the production and release of several inflammatory chemical substances, including cytokines and prostanoids, as well as mast cell degranulation. It has been shown that the acute inflammation caused as a result of carrageenan administration involves two stages (biphasic). The initial stage of the oedema process combines the actions of histamine and serotonin, whereas the later stage is a result of PG release that promotes the accumulation of inflammatory fluids at the site of inflammation (Taher, 2012). NSAIDs remarkably inhibit PG synthesis and eventually block the oedema formation following the carrageenan administration (Taher, 2012). Our finding in this study revealed that the MECA could efficiently attenuate acute inflammation by inhibiting histamine, serotonin and/ PG synthesis and release. Besides, the remarkable anti-inflammatory action of the MECA was observed at the second phase of the inflammatory process (3-h after the carrageenan administration). Therefore, the effect of the MECA could be mediated via inhibiting PG. Many herbal preparations have elicited inhibitory action against carrageenan-induced paw oedema. For instance, Nguyen et al. (2020) reported the capability of Periplaneta americana to inhibit paw oedema produced by carrageenan. Previous research has shown that the aqueous and methanol extract of Gmelina arborea remarkably declined the paw oedema (Kaur et al., 2018). Besides, Scapinello et al. (2019) research revealed the ability of Philodendron bipinnatifidum stem extract to abolish carrageenan-induced paw oedema.
Many researchers have used yeast-induced pyrexia to screen compounds with potential antipyretic activity (Abbasi et al., 2017). The fever usually begins following the stimulation of the immunological system and alteration of the temperature regulatory centre in the hypothalamus. It is induced after tissue damage or pyrogens' action that leads to the synthesis and release of the cytokine (Javed et al., 2020). In the hypothalamus, the cytokines provoke the production of PGE2 that mediates fever. The microvascular cells are the principal cells in the CNS responsible to synthesise PGE2 that eventually induce pyrexia abundantly. Besides, activated white blood cells, endothelial cells and macrophages at the inflammation location participate in the fever mechanisms (Taïwe et al., 2011). Looking at the outcomes of the research, the MECA could possess inhibitory action on PG biosynthesis via central mechanisms that are responsible for the observed antipyretic activity. An experiment by Kong et al. (2014) highlighted the antipyretic action of Rheum palmatum. The ethanolic extract of Indigofera argentea significantly declined the yeast-induced pyrexia (Javed et al., 2020).
Steroids, saponins, glycosides, flavonoids, tannins, alkaloids, together with terpenes, have anti-inflammatory and pain-attenuating actions (Ishola et al., 2014; Matos et al., 2010; Udo et al., 2020). Specifically, flavonoids including quercetin, biflavonoids, luteolin, rutin as well as triterpenoids inhibit COX, lipoxygenase, phospholipase A2 and C enzymes production, whereas the analgesic activity is mediated by interacting with opioid receptors (Ofuegbe et al., 2014). Besides, triterpenes also possess antinociceptive action (Okokon et al., 2017). The cardiac glycosides, triterpenes, tannins, steroids, flavonoids, saponins and alkaloids in the MECA could be the reasons for the potential antinociceptive, anti-inflammatory and antipyretic activities.
Conclusions
The current research has demonstrated that the MECA may possess some bioactive phytocomponents with pain-attenuating, anti-inflammatory and antipyretic actions, which validate the ethnopharmacological claim of Culcasia angolensis to manage pain and inflammatory diseases. Therefore, further investigations should be conducted on the plant to elucidate the mechanisms and molecular basis of its observed pharmacological actions to develop novel compounds for treating pain and inflammatory-related disorders.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABU:
-
Ahmadu Bello University
- ABUCAUC:
-
Ahmadu Bello University Ethical Committee on Animal Use and Care Research Policy
- ANOVA:
-
Analysis of variance
- ARRIVE:
-
Animal research: reporting of in vivo experiments
- CNS:
-
Central nervous system
- COX:
-
Cyclooxygenase
- IL:
-
Interleukin
- Ket:
-
Ketoprofen
- LD50 :
-
Median lethal dose
- MECA:
-
Methanol leaf extract of Culcasia angolensis
- MOR:
-
Morphine
- N/S:
-
Normal saline
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- OECD:
-
Organization of Economic Co-operation and Development
- PCM:
-
Paracetamol
- PG:
-
Prostaglandin
- SEM:
-
Standard error of the mean
- TNF:
-
Tissue necrosis factor
References
Abbasi, W. M., Ahmad, S., Perveen, S., & Rehman, T. (2017). Journal of traditional and complementary medicine preliminary phytochemical analysis and in vivo evaluation of antipyretic effects of hydro-methanolic extract of Cleome scaposa leaves. Journal of Traditional Chinese Medical Sciences. https://doi.org/10.1016/j.jtcme.2017.05.004
Ahmad, M. H., Zezi, A. U., Anafi, S. B., Danraka, R. N., & Alhassan, Z. (2020a). Evaluation of antidiarrhoeal activity of methanol extract of Combretum hypopilinum Diels (Combretaceae) leaves in mice. Advance Pharmaceutical Journal, 5(2), 54–61. https://doi.org/10.31024/apj.2020.5.2.3
Ahmad, M. H., Zezi, A. U., Bola, A. S., Alhassan, Z., Mohammed, M., & Danraka, R. N. (2020b). Mechanisms of antidiarrhoeal activity of methanol leaf extract of Combretum hypopilinum diels (Combretaceae): Involvement of opioidergic and (α1 and β)-adrenergic pathways. Journal of Ethnopharmacology, 269, 113750. https://doi.org/10.1016/j.jep.2020.113750
Alhakmi, F., Kumar, S., & Khan, S. A. (2013). Estimation of total phenolic content, in-vitro antioxidant and anti- inflammatory activity of flowers of M oringa oleifera. Asian Pacific Journal of Tropical Biomedicine, 3(8), 623–627. https://doi.org/10.1016/S2221-1691(13)60126-4
Angst, M. S., & Clark, D. J. (2006). A qualitative systematic review. Anesthesiology, 104, 570–587.
Ashis, K. M., & Jena, J. (2009). Anti-inflammatory and analgesic activity of bark extract of pterospermum acerifolium. International Journal of Current Pharmaceutical Research, 1(1), 32–37.
Bahmani, M., Shirzad, H., Majlesi, M., Shahinfard, N., & Kopaei, M. R. (2014). A review study on analgesic applications of Iranian medicinal plants. Asian Pacific Journal of Tropical Biomedicine, 7(Suppl 1), S43–S53. https://doi.org/10.1016/S1995-7645(14)60202-9
Balamurugan, M., Parthasarathi, K., Cooper, E. L., & Ranganathan, L. S. (2009). Anti-inflammatory and anti-pyretic activities of earthworm extract—Lampito mauritii (Kinberg). Journal of Ethnopharmacology, 121(2), 330–332. https://doi.org/10.1016/j.jep.2008.10.021
Bleakley, C. M., & Davison, G. W. (2011). Cryotherapy and inflammation : Evidence beyond the cardinal signs. Physical Therapy Reviews, 15(6), 430–435. https://doi.org/10.1179/1743288X10Y.0000000014
Bown, D. (2000). Aroids: Plants of the Arum family. Timber Press.
Burkill, H. M. (1985). The useful plants ofWest Tropical Africa (2nd ed., Vol. 1). Royal Botanical Gardens Kew.
Cássia, R. D., Andrade, L. N., & De Sousa, D. P. (2013). A review on anti-inflammatory activity of monoterpenes. Molecules, 18, 1227–1254. https://doi.org/10.3390/molecules18011227
Chandra, S., Chatterjee, P., Dey, P., & Bhattacharya, S. (2012). Evaluation of in vitro anti-inflammatory activity of coffee against the denaturation of protein. Asian Pacific Journal of Tropical Biomedicine, 2(1), S178–S180. https://doi.org/10.1016/S2221-1691(12)60154-3
Cruz, L. A., Díaz, M. A., Gupta, M. P., López-pérez, J. L., Morán-pinzón, J., Guerrero, E., Cruz, L. A., Díaz, M. A., Gupta, M. P., & López-pérez, J. L. (2019). Assessment of the antinociceptive and anti- inflammatory activities of the stem methanol extract of Diplotropis purpurea assessment of the antinociceptive and anti-inflammatory activities of the stem. Pharmaceutical Biology, 57(1), 1–5. https://doi.org/10.1080/13880209.2019.1628074
Donkor, K., Antwi, S., Nutifafa, J. A., Nii, T., Martey, O., & Okine, L. K. (2013). Analgesic and anti-inflammatory activities of Asena, a herbal preparation for treatment of arthritis, using rodent models. Medicinal and Aromatic Plant Research Journal, 1(2), 20–29.
Dubuisson, D., & Dennis, S. G. (1977). The formalin test: A quantitative study of the analgesic effects of morphine, meperidine, and brain stem stimulation in rats and cats. Pain, 4, 161–174.
Ermilo, V., Argáez, A., Domínguez, F., Moreno, D. A., Alberto, M., Espinoza, I., Cesar, J., Riegos, L., Ceballos, E., Juan, G., Zapata, R., Lorenzo, M., De, F., Sánchez, S., Angel, E., & Alonso, J. (2020). Anti-inflammatory and antinociceptive effects of an ethanol extract from Senna septemtrionalis. Inflammopharmacology, 28(2), 541–549. https://doi.org/10.1007/s10787-019-00657-7
Fabiana, A., Spindola, H. M., Lucia, A., Ruiz, T. G., Ernesto, J., Carvalho, D., Carlos, F., & Garcia, V. L. (2018). Biomedicine & Pharmacotherapy Antinociceptive and anti-edema properties of the ethyl acetate fraction obtained from extracts of Coriandrum sativum Linn. leaves. Biomedicine & Pharmacotherapy, 103, 1617–1622. https://doi.org/10.1016/j.biopha.2018.04.196
Fan, S., Ali, N. A., & Basri, D. F. (2014). Evaluation of analgesic activity of the methanol extract from the galls of Quercus infectoria (Olivier) in rats. Evidence-Based Complementary and Alternative Medicine. https://doi.org/10.1155/2014/976764
Ferrero-Miliani, L., Nielsen, O. H., Andersen, P., & Girardin, S. (2006). Chronic inflammation: Importance of NOD 2 and NALP 3 in interleukin-1 b generation. Clinical and Experimental Immunology, 147, 227–235. https://doi.org/10.1111/j.1365-2249.2006.03261.x
Helal, K., Rahman, A., Taher, M., Tangpong, J., Hajjar, D., Alelwani, W., Makki, A. A., & Reza, A. S. M. A. (2020). Journal of King Saud University-Science Hot methanol extract of Leea macrophylla (Roxb) manages chemical-induced inflammation in rodent model. Journal of King Saud University Science, 32(6), 2892–2899. https://doi.org/10.1016/j.jksus.2020.07.014
Ishola, I. O., Agbaje, E. O., Adeyemi, O. O., & Shukla, R. (2014). Analgesic and anti-inflammatory effects of the methanol root extracts of some selected Nigerian medicinal plants. Pharmaceutical Biology, 52(9), 1208–1216. https://doi.org/10.3109/13880209.2014.880487
Javed, F., Jabeen, Q., Aslam, N., & Mehmood, A. (2020). Pharmacological evaluation of analgesic, anti-inflammatory and antipyretic activities of ethanolic extract of Indigofera argentea Burm. f. Journal of Ethnopharmacology, 259, 112966. https://doi.org/10.1016/j.jep.2020.112966
Jo, H., Lee, G., Baek, C. Y., Song, H. S., & Lee, D. (2021). Analgesic and anti-inflammatory effects of aucklandia lappa root extracts on acetic acid-induced writhing in mice and monosodium iodoacetate-induced osteoarthritis in rats. Plants, 10(42), 1–12. https://doi.org/10.3390/plants10010042
Josabad, A., Castro, A., Arana, V., Eunice, A., Barrientos, Y., Alberto, M., Camacho, R., Wrobel, K., Cesar, J., Romero, T., & León, C. (2021). Antinociceptive and anti inflammatory effects of Cuphea aequipetala Cav (Lythraceae). Inflammopharmacology, 29(1), 295–306. https://doi.org/10.1007/s10787-020-00709-3
Kakoti, B. B., Pradhan, P., Borah, S., Mahato, K., & Kumar, M. (2013). Analgesic and anti-inflammatory activities of the methanolic stem bark extract of Nyctanthes arbor-tristis Linn. BioMed Research International, 826295, 1–6. https://doi.org/10.1155/2013/826295
Kaur, S., Mohinder, P., Bedi, S., & Kaur, N. (2018). Anti-inflammatory effect of methanolic extract of Gmelina arborea bark and its fractions against carrageenan induced paw oedema in rats. Natural Product Research, 32(23), 2861–2864. https://doi.org/10.1080/14786419.2017.1385005
Kong, X., Wan, H., Su, X., Zhang, C., Yang, Y., Li, X., Yao, L., & Lin, N. (2014). Rheum palmatum L. and Coptis chinensis Franch, exert antipyretic effect on yeast-induced pyrexia rats involving regulation of TRPV1 and TRPM8 expression. Journal of Ethnopharmacology, 153(1), 160–168. https://doi.org/10.1016/j.jep.2014.02.007
Kpemissi, M., Metowogo, K., Melila, M., Veerapur, V. P., Negru, M., Taulescu, M., Potârniche, A., Shivalingaiah, D., Adinarayanashetty, T., Vijayakumar, S., Eklu-gadegbeku, K., & Aklikokou, K. (2020). Acute and subchronic oral toxicity assessments of Combretum micranthum (Combretaceae) in Wistar rats. Toxicology Reports, 7, 162–168. https://doi.org/10.1016/j.toxrep.2020.01.007
Kumar, C. U., Pokuri, V. K., & Pingali, U. (2015). Evaluation of the analgesic activity of standardized aqueous extract of Terminalia chebula in healthy human participants using hot air pain model. Journal of Clinical and Diagnostic Research, 9(5), 1–4. https://doi.org/10.7860/JCDR/2015/11369.5916
Loux, J. J., Depalma, P. D., & Yankel, S. L. (1972). Antipyretic testing of aspirin in rats1. Toxicology and Applied Pharmacology, 22, 672–675. https://doi.org/10.1016/0041-008X(72)90295-5
Luo, H., Zhu, D., Chen, Y., Jiang, R., & Yu, P. (2018). Study on the structure of ginseng glycopeptides with anti-inflammatory and analgesic activity. Molecules. https://doi.org/10.3390/molecules23061325
Magaji, M. G., Anuka, J. A., Abdu-Aguye, I., Yaro, A. H., & Hussaini, I. M. (2007). Preliminary studies on anti-inflammatory and analgesic activities of Securinega virosa (Euphorbiaceae) in experimental animal models. Journal of Medicinal Plants Research, 2(2), 039–044.
Matos, N. D., Moraes, C., Rezende, D., Paredes, S., Eline, M., Pinto, C., & Dias, P. (2010). Characterization of the antinociceptive and anti-inflammatory activities of fractions obtained from Copaifera multijuga Hayne. Journal of Ethnopharmacology, 128, 177–183. https://doi.org/10.1016/j.jep.2010.01.005
Mueller, M., Hobiger, S., & Jungbauer, A. (2010). Anti-inflammatory activity of extracts from fruits, herbs and spices. Food Chemistry, 122(4), 987–996. https://doi.org/10.1016/j.foodchem.2010.03.041
Musila, M. N., Ngai, D. N., Mbiri, J. W., Njagi, S. M., Mbinda, W. M., & Ngugi, M. P. (2017). Acute and sub-chronic oral toxicity study of methanolic extract of Caesalpinia volkensii (Harms). Journal of Drug Metabolism & Toxicology, 08(01), 1–8. https://doi.org/10.4172/2157-7609.1000222
Nasri, H., & Shirzad, H. (2013). Toxicity and safety of medicinal plants. Journal of HerbMed Pharmacology, 2(2), 21–22.
Nguyen, T., Chen, X., Chai, J., Li, R., Han, X., Chen, X., Liu, S., Chen, M., & Xu, X. (2020). Biomedicine & pharmacotherapy antipyretic, anti-inflammatory and analgesic activities of Periplaneta americana extract and underlying mechanisms. Biomedicine & Pharmacotherapy, 123, 109753. https://doi.org/10.1016/j.biopha.2019.109753
Ofuegbe, S. O., Adedapo, A. A., & Adeyemi, A. A. (2014). Anti-inflammatory and analgesic activities of the methanol leaf extract of Phyllanthus amarus in some laboratory animals. Journal of Basic and Clinical Physiology and Pharmacology, 25(2), 175–180. https://doi.org/10.1515/jbcpp-2013-0084
Okokon, J. E., Augustine, N. B., Mohanakrishnan, D., Okokon, J. E., Augustine, N. B., & Mohanakrishnan, D. (2017). Antimalarial, antiplasmodial and analgesic activities of root extract of Alchornea laxiflora. Pharmaceutical Biology, 55(1), 1022–1031. https://doi.org/10.1080/13880209.2017.1285947
Okolo, C. O., Johnson, P. B., Abdurahman, E. M., Abdu-Aguye, I., & Hussaini, I. M. (1995). Analgesic effect of Irvingia gabonensis stem bark extract. Journal of Ethnopharmacology, 45(2), 125–129. https://doi.org/10.1016/0378-8741(94)01199-A
Okpo, S. O., Fatokun, F., & Adeyemi, O. O. (2001). Analgesic and anti-inflammatory activity of Crinum glaucum aqueous extract. Journal of Ethnopharmacology, 78(2–3), 207–211. https://doi.org/10.1016/S0378-8741(01)00318-X
Organisation for Economic Cooperation and Development (OECD). (2001). Guidelines for the testing of chemicals: health effect test no. 423. Acute oral toxicity-acute toxic class method, Paris, France.
Pacheco, S. D. G., Gasparin, A. T., Jesus, C. H. A., Sotomaior, B. B., Ventura, A. C. S. S. B., Redivo, D. D. B., & da Cunha, J. M. (2019). Antinociceptive and anti-inflammatory effects of bixin, a carotenoid extracted from the seeds of Bixa orellana authors. Planta Medica, 85(16), 1216–1224. https://doi.org/10.1055/a-1008-1238
Poetker, D. M., & Reh, D. D. (2010). A comprehensive review of the adverse effects of systemic corticosteroids. Otolaryngologic Clinic, 43, 753–768. https://doi.org/10.1016/j.otc.2010.04.003
Prasanth, K. M., Suba, V., Ramireddy, B., & Srinivasa, B. P. (2015). Acute and subchronic oral toxicity assessment of the ethanolic extract of the root of Oncoba spinosa (Flacourtiaceae) in rodents. Tropical Journal of Pharmaceutical Research, 14(10), 1849–1855. https://doi.org/10.4314/tjpr.v14i10.16
Qin, Y., Wu, X., Huang, W., Gong, G., Li, D., He, Y., & Zhao, Y. (2009). Acute toxicity and sub-chronic toxicity of steroidal saponins from Dioscorea zingiberensis C. H. Wright in rodents. Journal of Ethnopharmacology Journal, 126, 543–550. https://doi.org/10.1016/j.jep.2009.08.047
Rahman, M., Alam, N. M. M., & Hasan, N. (2020). Heliyon In vivo and in silico evaluation of antinociceptive activities of seed extract from the Holarrhena antidysenterica plant. Heliyon, 6, e03962. https://doi.org/10.1016/j.heliyon.2020.e03962
Rosas, E. C., Correa, L. B., & Henriques, M. G. (2019). Antiinflammatory properties of schinus terebinthifolius and its use in arthritic conditions. Bioactive Food as Dietary Interventions for Arthritis and Related Inflammatory Diseases. https://doi.org/10.1016/B978-0-12-813820-5.00028-3
Scapinello, J., Girardi, L., Schindler, M. S. Z., Sabrina, G., Maria, A., Boligon, A. A., Niero, R., Saraiva, T. E. S., Pulz, N., Heemann, A., Oliveira, J. V., Dal, J., & Oliveira, D. D. (2019). Antinociceptive and anti-inflammatory activities of Philodendron bipinnatifidum Schott ex Endl (Araceae). Journal of Ethnopharmacology, 236, 21–30. https://doi.org/10.1016/j.jep.2019.02.037
Shojaii, A., Motaghinejad, M., Norouzi, S., & Motevalian, M. (2015). Evaluation of anti-inflammatory and analgesic activity of the extract and fractions of astragalus hamosus in animal models. Iranian Journal of Pharmaceutical Research, 14(1), 263–269.
Sofowora, A. (1993). Medicinal plants and traditional medicine in Africa (2nd ed.). Spectrum Books Ltd.
Soyocak, A., Kurt, H., Cosan, D. T., Saydam, F., Calis, I. U., Kolac, U. K., Koroglu, Z. O., Degirmenci, I., Mutlu, F. S., & Gunes, H. V. (2019). Tannic acid exhibits anti-inflammatory effects on formalin-induced paw edema model of inflammation in rats. Human and Experimental Toxicology. https://doi.org/10.1177/0960327119864154
Sultana, S., Asif, H. M., Akhtar, N., & Ahmad, K. (2015). Asian Pacific journal of tropical disease medicinal plants with potential antipyretic activity : A review. Asian Pacific Journal of Tropical Disease, 5(Suppl 1), S202–S208. https://doi.org/10.1016/S2222-1808(15)60890-8
Taher, Y. A. (2012). Antinociceptive activity of Mentha piperita leaf aqueous extract in mice. Libyan Journal of Medicine, 7(1), 1–6. https://doi.org/10.3402/ljm.v7i0.16205
Taher, Y. A., Samud, A. M., El-taher, F. E., Ben-Hussin, G., Elmezogi, J. S., Al-mehdawi, B. F., & Salem, H. A. (2015). Experimental evaluation of antiinflammatory, antinociceptive and antipyretic activities of Clove oil in mice. Libyan Journal of Medicine. https://doi.org/10.3402/ljm.v10.28685
Taïwe, G. S., Bum, E. N., Talla, E., Dimo, T., Weiss, N., Sidiki, N., Dawe, A., Clarisse, F., Moto, O., Dzeufiet, P. D., & Waard, M. D. (2011). Antipyretic and antinociceptive effects of Nauclea l root decoction and possible mechanisms of action. Pharmaceutical Biology, 49(1), 15–25. https://doi.org/10.3109/13880209.2010.492479
Tanko, Y., Magaji, G. M., Yerima, M., Magaji, R. A., & Mohammed, A. (2008). Anti-nociceptive and anti-inflammatory activities of aqueous leaves extract of Ocimum Gratissimum (Labiate) in Rodents. African Journal of Traditional, Complementary and Alternative Medicines, 5(2), 141–146.
Tjolsen, A., Berge, O.-G., Hunskaar, S., Rosland, H. J., & Hole, K. (1992). The formalin test: An evaluation of the method. Pain, 51(1), 5–17.
Toma, A., Deyno, S., Fikru, A., Eyado, A., & Beale, A. (2015). In vivo antiplasmodial and toxicological effect of crude ethanol extract of Echinops kebericho traditionally used in treatment of malaria in Ethiopia. Malaria Journal. https://doi.org/10.1186/s12936-015-0716-1
Udo, U. E., Echeme, J. O., & Igwe, O. U. (2020). Phytochemical, anti-inflammatory and analgesic properties of stembark extract and fractions of Lonchocarpus sericeus Poir. (Papilionaceae) in albino mice. Avicenna Journal of Phytomedicine, 10(6), 584–593.
Ugwah-oguejiofor, C. J., Okoli, O. C., Ugwah, M. O., Umaru, M. L., Ogbulie, C. S., Mshelia, H. E., Umar, M., & Njan, A. A. (2019). Acute and sub-acute toxicity of aqueous extract of aerial parts of Caralluma dalzielii N. E. Brown in mice and rats. Heliyon, 5(1), 79. https://doi.org/10.1016/j.heliyon.2019.e01179
Ugwu, D. I., Okoro, U. C., Onyeoziri, P., Gupta, A., & Okafor, S. N. (2018). Novel anti-inflammatory and analgesic agents : Synthesis, molecular docking and in vivo studies. Journal of Enzyme Inhibition and Medicinal Chemistry, 33(1), 405–415. https://doi.org/10.1080/14756366.2018.1426573
Vongtau, H. O., Abbah, J., Mosugu, O., Chindo, B. A., Ngazal, I. E., Salawu, A. O., Kwanashie, H. O., & Gamaniel, K. S. (2004). Antinociceptive profile of the methanolic extract of Neorautanenia mitis root in rats and mice. Journal of Ethnopharmacology, 92(2–3), 317–324. https://doi.org/10.1016/j.jep.2004.03.014
Winter, C. A., Risley, E. A., & Nuss, G. W. (1962). Carrageenin-induced edema in hind paw. Experimental Biology and Medicine, 3(111), 544–547.
Yerima, M., Anuka, J. A., Salawu, O. A., & Abdu-Aguye, I. (2014). Antihyperglycaemic activity of the stem-bark extract of Tamarindus indica L. on experimentally induced hyperglycaemic and normoglycaemic Wistar rats. Pakistan Journal of Biological Sciences, 17(3), 414–418. https://doi.org/10.3923/pjbs.2014.414.418
Zakaria, A., Jais, M. R., & Ishak, R. (2018). Analgesic properties of Nigella sativa and Eucheuma Cottonii Extracts. Journal of Natural Science Biology and Medicine, 9, 23–26. https://doi.org/10.4103/jnsbm.JNSBM
Zulfiker, A. H. M., Rahman, M. M., Hossain, M. K., Hamid, K., & Mazumder, M. E. H. (2010). In vivo analgesic activity of ethanolic extracts of two medicinal plants-Scoparia dulcis L. and Ficus racemosa Linn. Biological Medicine, 2(2), 42–48.
Acknowledgements
The authors are grateful to all staff of the Pharmacology and Therapeutics Department, ABU, Nigeria, for the support throughout the period of conducting the research
Plant authentication
The Culcasia angolensis was identified at the Herbarium part of the Botany Department, Faculty of Life Sciences, ABU, Zaria, Nigeria, (voucher number: 01676) when compared with the deposited specimen.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
IGA contributed to conceptualisation, investigation, data curation, writing—original draft, data analysis. DDA contributed to conceptualisation, investigation, writing and review. MV contributed to writing and review. OFK contributed to formal analysis. OAL contributed to writing. MHA contributed to writing, review and editing. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The permission to conduct the experiment was granted by the Ahmadu Bello University Ethical Committee on Animal Use and Care Research Policy (protocol number: ABUCAUC/2019/006) and carried out as per the Animal Research: Reporting of In Vivo Experiments (ARRIVE) guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nock, D.D., Abraham, I.G. & Ahmad, M.H. Potential pharmacological properties of methanol leaves extract of Culcasia Angolensis (Araceae): antinociceptive, antiinflammatory and antipyretic activities in laboratory animals. JoBAZ 83, 7 (2022). https://doi.org/10.1186/s41936-022-00269-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41936-022-00269-8