Abstract
The colonic epithelial cells represent a border between the colon luminal content, containing notably bacteria and a complex mixture of compounds, and the “milieu interieur” as defined by the French physiologist Claude Bernard. The physical-chemical composition of the luminal content, including luminal pH and bacterial metabolite, that obviously is not constant, is modified for instance according to the diet. Data obtained recently indicate that physical exercise may also modify the colonic luminal content. Evidence has indicated that modification of the luminal content characteristics has, indeed, consequences for the colonic epithelial cells, notably in terms of energy metabolism and DNA integrity. Although such alterations impact presumably the homeostatic process of the colonic epithelium renewal and the epithelial barrier function, their contribution to pathological processes like mucosal inflammation, pre-neoplasia, and neoplasia remains partly elusive. Open questions remain regarding the individual and collective roles of luminal changes, particularly in a long-term perspective. These questions are related particularly to the capacity of the bacterial metabolites to cross the mucus layer before entering the colonocytes, to the concentrations of metabolites in proximity of the colonic crypt stem cells, and to the capacity of colonocytes to detoxicate deleterious compounds, to take up and utilize beneficial compounds.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The colonic epithelium can be viewed as a dynamic structure with a very rapid speed of renewal. Indeed, the colonic epithelium in mammals is renewed within few days. Stem cells residing within the base of the crypts are responsible for continuously producing transit cells that undertake differentiation following a limited number of cellular divisions. This renewal is made through highly coordinated and complex sequences of events beginning with mitosis of pluripotent stem cells situated at the bottom of the colonic crypts. The differentiated cells reach the surface of the colon, where they are removed by detachment-induced apoptosis named Anoïkis. The high division rate of stem cells and the corresponding high apoptotic rate of mature cells lead to the high cellular turnover of the colon epithelium. A dysfunction of oxygen consumption or mitochondrial dysfunction may compromise the epithelium homeostasis and consequently alters its barrier function [1].
Besides, the colonic epithelium is notably responsible for the physiological function of water, electrolyte, and various bacterial metabolites absorption from the lumen to the bloodstream. This absorption is made through absorptive colonocytes which are facing the luminal content, a complex and not fully characterized mixture of bacteria and their metabolites, water, undigested or partially digested dietary/endogenous compounds, particularly from endogenous and alimentary proteins that may be beneficial or deleterious for the epithelium, etc. Occasionally, the homeostatic processes of colonic epithelial self-renewing, possibly associated with disruption of normal functions, are affected, and such alterations may be associated with different physiopathological states including diarrhea [2], mucosal inflammation, and preneoplasic/neoplasic lesions [3].
It is expected from the high energy consumption of the colonic epithelial cells that mitochondrial dysfunction may have a larger impact on their metabolism and physiology. Thus, the objectives of this mini-review are (i) to give some examples of the impact of nutrient intake, especially dietary protein, on the characteristics of the large intestine luminal content composition; (ii) to give a brief overview on the effects of changes of the colonic epithelial cell luminal environment on their physiology and metabolism, with a focus on the effects of some bacterial metabolites; (iii) to examine to what extent such changes, above the adaptive capacities of the colonocytes, may have consequences for the gut health; and finally (iv) to report on some recent results regarding the impact of physical exercise on the luminal environment of colonocytes.
Effects of the diet on the composition of the large intestine luminal content
Undigested or partially digested substrates from both endogenous (digestive secretions, exfoliated cells, mucins, etc.) and dietary sources can be metabolized by the bacteria belonging to the intestinal microbiota [4]. Dietary intervention studies with volunteers revealed that the macronutrient composition of the diet can impact the composition of the large intestine luminal content. Notably, it has been shown that dietary undigestible polysaccharides increase the fecal concentration of short-chain fatty acids (SCFA) [5], while diets with a high fat content increase bile acid secretion in the small intestine, leading to high fecal concentrations of microbiota-derived secondary bile acids, such as deoxycholic acid [6].
Although the digestion of alimentary protein is very efficient, approximately 90% efficiency, some nitrogenous material originating from non-digested proteins are transferred from the small intestine to the large intestine [7] and are degraded by the microbiota and by residual pancreatic enzymes to produce numeral metabolites and gases. These gases, especially, can be beneficial or deleterious for the intestinal epithelium in a concentration-dependent way [8, 9]. High-protein diets increase the fecal concentrations of amino acid-derived bacterial metabolites, such as branched-chain fatty acids, phenolic and indolic compounds, hydrogen sulfide (H2S), and ammonia, among others [10]. Other parameters, such as colonic luminal pH, may also be modified by dietary changes. Ingestion of nondigestible carbohydrates decreases the fecal pH in adults [11], while consumption of high-protein/low carbohydrate diets increases this parameter [12]. Collectively, these studies indicate that the human rectal environment (inferred from feces analysis) is depending on the dietary composition.
Regarding the composition of the colonic microbiota, although considered as globally stable at the individual level [13], this composition can be, however, rapidly affected by environmental modifications, notably from dietary origin [14]. Although modifications of luminal bacterial metabolite composition in inflammatory bowel diseases have been reported [15], it is often a difficult task to determine if such modifications are causes or consequences of these diseases. In the same line of thinking, although intestinal microbiota dysbiosis has been observed in colorectal cancers [16], the respective causal links between the bacterial composition/bacterial metabolic capacity/bacterial metabolite composition and the related pathophysiological situations remain largely elusive.
In this overall context, our mini-review will present several changes in the luminal environment (bacterial metabolite composition, pH, osmolarity) which have been shown to impact, at least in vitro, the colonic epithelial cells with potential implications in digestive disease apparition and development [17].
Bacterial metabolites and colonic epithelium energy metabolism
The gastrointestinal tract consumes 20% of the whole body oxygen consumption while representing approximately 5% of body weight. Absorptive colonic epithelial cells utilize energy substrates from both the luminal and basolateral sides. Fuels from arterial origin are mainly amino acids including L-glutamine, L-glutamate, and L-aspartate, but also D-glucose [18].
SCFA (namely acetate, propionate, and butyrate) are major luminal fuels for colonocytes. These compounds are produced by the intestinal microbiota from undigestible polysaccharides [19] and several amino acids originating from undigested protein [20]. For instance, butyrate plays an important role on oxygen consumption in order to favor energy metabolism [21]. Data showing that butyrate uptake is impaired in the inflamed colonic mucosa. It has also been suggested that the reduction of butyrate availability may decrease the physiological functions of this SCFA, especially butyrate, in colonocytes [22]. In addition, to act as a luminal fuel in colonocytes, butyrate acts as a regulator of gene expression in these cells [23] (Fig. 1).
Schematic representation of the microbiota-derived butyrate metabolism and effects on colonocytes. Butyrate, which is produced from undigested carbohydrates and some protein-derived amino acids, diffuses through the mucus layers before entering colonocytes. Butyrate enters the cell via MCT1 (monocarboxylate transporter 1) and is oxidized in the mitochondria allowing ATP production. A part of cytosolic acetyl CoA produced from butyrate is used for histone acetylation, while unmetabolized butyrate inhibits histone deacetylase (HDAC) activity. Increased histone acetylation then modulates gene expression in colonocytes
Hydrogen sulfide, which is produced by some intestinal bacteria from endogenous and exogenous sulfur-containing substrates, influences colonocyte health via mitochondrial metabolism and inflammation resolution. Evidences have suggested that, under specific conditions such as hypoxia, H2S contributes to generate adenosine triphosphate (ATP) [24, 25]. Then, when oxygen is insufficient, colonocytes are capable of obtaining energy demand via sulfide oxidation (S2O32−). Indeed, this oxidation process is an adaptation of colonocytes, and it involves a sulfide quinone reductase (SQR) activity, which also contributes to colonocytes tolerance [26]. Besides, H2S inflammatory signaling is dependent on its concentration and colonocytes’ ability to detoxify this gas transmitter. At low concentrations, H2S has been shown to upregulate cyclooxygenase-2 (COX-2) expression [27] and to reduce prostaglandin E2 synthesis, chemokines, cytokines, and other protein expressions that are related to factor nuclear kappa B (NF-κB) pathway [28] (Fig. 2). COX-2 is important for maintenance of mucosal defense in the gastrointestinal tract, as well as in inflammation resolution [27]. Hydrogen sulfide is also capable of inhibiting phosphodiesterases via elevation of second messengers, such as cyclic AMP and/or cyclic GMP levels, which contribute to its anti-inflammatory role in colonocytes and lowering blood pressure [29]. ATP-sensitive potassium channel can be activated by H2S, especially from endogenous origin, which may attenuate pain in colonic inflammation [30] and leukocytes activation [31]. Moreover, H2S may interfere on leukocytes adherence, notably neutrophils, in vascular endothelium and diminishes both leukocyte recruitment and infiltration under tissue injury condition [31]. Those cells infiltrated by neutrophils can undergo apoptosis and be cleaned by macrophage type 2, which have anti-inflammatory phenotype [27, 31]. Therefore, it seems that H2S, at low concentrations, plays an important role in inflammation resolution in colonocytes through several pathways, and this resolution, in turn, may also favor tissue repair (Fig. 2).
Schematic representation of the microbiota-derived H2S metabolism and effects on colonocytes. Hydrogen sulfide (H2S) is produced from several dietary and endogenous sulfur-containing compounds and diffuses through the mucus layers and colonocyte apical membrane. Left panel: When H2S concentration is low, mitochondria can detoxicate it through oxidation into thiosulfate (S2O32−) via sulfide quinone reductase (SQR) in the sulfide oxidizing unit. H2S can also be used for ATP production when oxygen (O2) is low. Moreover, H2S is able to support inflammation resolution through inhibition of phosphodiesterases (PDE), downregulation of NF-κB pathway, and enhancement of cyclooxygenase-2 (COX-2) expression. In addition, H2S is able to activate ATP-potassium sensitive channel (KATP channel), which may be involved with reduced pain and inflammation. Right panel: When H2S is high, thus exceeding colonocyte detoxification capacity, it inhibits mitochondrial cytochrome c oxidase activity, leading to a decrease O2 consumption. Raised concentration of the intra-cytoplasmic H2S increases the expression of genes related to inflammation
On the other hand, H2S as well as p-cresol and ammonia, at excessive luminal concentrations, interferes with colonocyte respiration, at least in in vitro experiments. Hydrogen sulfide inhibits, above a threshold value, markedly, although in a reversible way, the colonocyte oxygen consumption and ATP production [32] (Fig. 2). This inhibition of cell respiration corresponds to the inhibition of the mitochondrial cytochrome C oxidase activity, one of the main components of mitochondrial respiration [33]. At concentration where H2S inhibits oxygen consumption in colonocytes, this gaseous compound increases the expression of several inflammation-related genes [8]. The cytoplasmic concentration of this agent can increase the capacity of colonocytes of detoxifyed H2S in the mitochondria and then impact gene expression in the nuclei (Fig. 2). Indeed, studies have shown H2S detoxification impairment in patients with Crohn’s disease [34] and also butyrate β-oxidation impairment in patients with ulcerative colitis [35]. Moreover, this metabolite was capable of supporting colonic tumor growth through stimulation of cell bioenergetics and cell proliferation [36]. Another bacterial metabolite, p-cresol, which is produced from L-tyrosine by the intestinal microbiota and which is present in the feces at low millimolar concentration, partially inhibits oxygen consumption in colonocytes [9]. Ammonia (considered as the sum of NH4+ and NH3), which is produced by the bacterial microbiota from amino acid deamination and hydrolysis of urea by the bacterial ureases, is present at millimolar concentrations in the colonic luminal content [20]. Millimolar concentrations of ammonia dose-dependently inhibit SCFA oxidation [37] and basal oxygen consumption in colonocytes [38]. However, colonocytes appear to be able to face moderate increase of ammonia luminal concentration by metabolizing ammonia in L-glutamine and L-citrulline, respectively, in the cytosol and mitochondria of colonocytes [39, 40].
Then, it appears that some bacterial metabolites, such as H2S, at a given concentration, and SCFA are regulators of colonocyte metabolism. However, when present in the colonic luminal content at excessive concentrations, H2S, p-cresol, and ammonia can act on colonocytes as “metabolic troublemakers” by acting, mainly, on the mitochondrial activity [41].
Possible links between physical exercise and intestinal microbiota
We are far away from the precise mechanisms that connect exercise and intestinal microbiota. It is supported that the exercise, especially the aerobic exercise, plays a role on intestinal microbiota by altering parameters that influence the intestinal microenvironment. Recently, a paper from our laboratory concerning exercise, nutrition, and intestinal microbiota [42] was published, and we will present below some topics.
Short-chain fatty acids
Exercise may increase acetate-, propionate-, and butyrate-producing bacteria species [43, 44]. Matsumoto et al. [45] were the first to show that voluntary exercise in animals is able to change SCFA production (mainly n-butyrate) in the cecum. In addition, this study reported alteration in the cecal microbiota profile after exercise with greater predominance of butyrate-producing bacteria species [45]. This shift in butyrate production and bacteria composition in the exercised group was also shown by Evans et al. [43].
The possible effect of aerobic exercise on the microbial composition is the environment change which has been connected to a pH decrease in the gut from SCFA production. SCFA contribute to decrease pH in the large intestine and decrease the transformation of primary to secondary bile acids promoting colonic acidification. Changes in the intestinal luminal pH may modify the environment in such way that it becomes more favorable for the proliferation of commensal bacterial species [42, 46].
After being absorbed by colonocytes, SCFA can participate in intestinal metabolism. Acetate and propionate are preferred for other organs, while butyrate is the major fuel for colonocytes. Specifically, butyrate can promote cell differentiation and cell cycle arrest and inhibit the enzyme histone deacetylase, [47]. Also, butyrate can improve mitochondrial metabolism via β-oxidation and AMP-activated protein kinase (AMPK) activation in colonocytes [48].
Moreover, studies have shown that butyrate may induce mucin synthesis [49] and improve gut barrier integrity by increasing tight junction assembly [50,51,52]. Mucins are the protective layer consisting of glycoproteins that form the intestinal barrier which limit exposure of mucosa to toxins and bacteria. This mucin layer has been recognized to play an important role in the interaction with intestinal microbiota and may serve as a substrate for intestinal bacteria, such as the commensal species Akkermansia muciniphila. Because of this, the mucin layer contributes to modulate the microbial community composition [52].
Butyrate production in the large intestine is associated with production of heat shock protein 70 (Hsp70). Hsp70 maintains the functional and structural properties of intestinal epithelial cells in response to intense prolonged exercise [53]. Since exercise and butyrate stimulate epithelial cell Hsp70 production, this may provide structural and functional stability to intestinal epithelial cells undergoing unfavorable conditions.
Bile acids
Exercise has been reported to increase excretion of primary bile acids in the gastrointestinal tract. Since SCFA, specifically butyrate (that has been reported to be increased by exercise), diminishes the conversion of bile acids into secondary bile acids, physical activity may, consequently, favor the rising of primary bile acids concentrations in the intestinal luminal content [54, 55]. The primary bile acids have established anti-microbial activity [55]. In agreement with this hypothesis, Islam et al. [56] demonstrated that cholic acid induced substantial changes in the cecal microbiome composition by stimulating the growth of Firmicutes at the expense of Bacteroidetes and provoked outgrowth of several bacteria in the Clostridia and Erysipelotrichi classes. Antimicrobial activity of the bile acids may elicit selective pressure on the bacterial communities in exercised mice, leading to a shift of the intestinal microbiota composition [55, 56]. Besides, some bile acid-tolerant microbes are sulfur-reducing bacteria, such as Bilophila wadsworthia. In animal-based diet, for example, this species can thrive and favors inflammation via H2S production [57].
Furthermore, secondary bile acids produced by intestinal microbiota influence mitochondrial metabolism. Intestinal microbiota can convert primary bile acids into secondary bile acids. The latter, in turn, interacts with mitochondria through farnesoid X receptor (FXR) and G-coupled membrane protein 5 (TGR5) [58]. These transcription factors regulate other proteins that are involved in fatty acid uptake and oxidation, such as peroxisome proliferator-activated receptor alpha (PPAR-α) and steroid response element binding protein 1-c (SREBP-1c) [59].
Hence, exercise is able to modulate both butyrate and bile acids exercise which are involved in intestinal metabolism and health homeostasis. In addition, it seems that they can be influenced by H2S, especially when H2S is produced via microbiota.
Bacterial metabolites and colonic epithelial cell DNA integrity
By using the sensitive H2AX genotoxicity test, p-cresol has been found to alter dose-dependently the DNA integrity in colonocytes without cytotoxic effects [9]. Phenol, which is produced by the intestinal microbiota from L-tyrosine, can react with nitrite, leading to the formation of the mutagenic compound p-diazoquinone [60].
Numerous other bacterial metabolites have been identified to alter DNA integrity in colonocytes. They include the fecal pentaenes, which are produced by the microbiota presumably from polyunsaturated ether phospholipids, and represent potent mutagens towards colonocyte DNA [61]. Deoxycholic acid produced in the colon by the intestinal microbiota is also acting as a DNA-damaging agent [62]. Acetaldehyde, which is produced from ethanol by the intestinal microbiota, is considered as a possible co-carcinogenic compound in the rectum [63]. From these examples of genotoxic bacterial metabolites, it is largely conceivable that long-term exposure of colonic crypt cells to excessive DNA-damaging bacterial metabolites would increase the risk of unrepaired DNA lesions in these cells [64].
Bacterial metabolites and colonic epithelial barrier function
Some bacterial metabolites have been suspected to affect, either positively or negatively, the colonic epithelial barrier function. For instance, it has been proposed that exogenous H2S, by reducing disulfide bonds in mucus, would increase the permeability of the mucous layer to luminal compounds, including the heme compound originating notably from red meat consumption [65]. Interestingly, evidence has been presented indicating that altered mitochondrial function induced by uncoupling agents in colonocytes cause intestinal barrier dysfunction [66], raising the view that perturbed mitochondrial function is associated with impaired epithelial integrity. Conversely, endogenous H2S may have beneficial effects on colonic mucus production [67]. Also, the bacterial metabolite indole, which is produced from L-tryptophan, has been shown to act as a beneficial luminal compound by increasing epithelial cell tight-junction resistance [68]. Lastly, butyrate is also recognized as a bacterial metabolite which enhances the intestinal barrier function [69].
Bacterial metabolites and pH
The pH in the human large intestine is slightly acidic in the caecum while being close to neutrality in the left colon and rectum [70]. The luminal pH depends on the respective concentrations of a very complex mixture of acidic and alkaline compounds in the large intestine. Modifications of the luminal pH may affect colonic epithelial cell physiology. Interestingly, lower colonic luminal pH in patients with ulcerative colitis has been observed [71]. In an experimental rodent model with chemically induced colon carcinogenesis, lower luminal pH is associated with higher tumor yield and increased epithelial cell proliferation [72]. Conversely, a low pH inhibits the synthesis by the intestinal microbiota of the DNA-damaging secondary bile acids [73]. In addition, acidic extracellular pH has been shown to shift colorectal epithelial cell death from apoptosis to necrosis upon exposure to short-chain fatty acids [74]. Lastly, low external pH is able to increase markedly the expression of the multidrug resistance (MDR) protein in human colon carcinoma cell lines [75], thus rendering these cells more resistant to chemotherapeutic agents.
Then, it appears that a more acidic luminal pH is associated with both beneficial and deleterious effects on colonocytes. These effects are apparently different according to the status of colonocytes, i.e., healthy or neoplasic.
Physical exercise and colonic luminal content characteristics
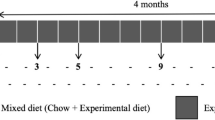
Recent studies strongly suggest that physical exercise can impact the characteristics of the intestinal luminal contents and notably the microbiota composition. Matsumoto et al. [45] were among the first to report that physical exercise modifies intestinal microbiota composition. More recently, it has been shown that the effects of exercise on intestinal microbiota are partly independent from dietary changes [76]. Studies have suggested that moderate aerobic exercise may contribute to the growth of butyrate-producing bacteria [77]. The training status and intensity of exercise appear to impact the proliferation of specific bacteria, such as Faecalibacterium prausnitzii, beneficial bacteria for the digestive tract [78]. A study with human volunteers reported increased microbiota diversity and richness in elite rugby players when compared with control groups with low physical activity and low or high body mass index. Interestingly, these athlete volunteers reported high protein consumption compared to the sedentary controls and, despite of there is no H2S-related data on this study, it seems that exercise and diet can change intestinal microbiota composition orthogonally [79]. This hypothesis is also supported by Kang et al. [80]. Also, the authors found that trained men presented a high level of SCFA on fecal samples when compared with sedentary men [79]. Likewise, Estaki et al. [81] analyzed the fecal microbiota of individuals with different fitness and demonstrated that cardiorespiratory fitness was positively correlated with increased intestinal microbial diversity and butyrate concentrations. The authors found a microbiome enriched in butyrate-producing bacteria, such as Lachnospiraceae, Roseburia, and Clostridiales, and high level of butyrate concentrations on individuals with high fitness.
So far, evidences have suggested an influence on the intestinal environment (mainly intestinal bacteria and their metabolites concentrations) by exercise, especially moderate aerobic exercise (60–65% VO2max) [42,43,44, 50, 78, 80]. However, studies differ among themselves in relation to the methods applied and are no data related to the exercise effect on the luminal H2S production/concentration.
Conclusion and future prospects
According to experimental studies with animal models and colonocytes, there is no doubt that changes in the luminal environment of colonic epithelial cells, and notably high concentrations of several bacterial metabolites, impact major aspects of their physiology and metabolism. Notably, such high concentrations of individual bacterial metabolites impact colonocyte energy metabolism, intestinal barrier, and inflammatory resolution and DNA integrity.
Several crucial unresolved questions remained, notably those related to the genotoxic effects of several bacterial metabolites in close vicinity with the colonic crypt stem cells, a parameter difficult to measure for obvious technical reasons. Indeed, since the crypt stem cells appear to be the cells at the origin of colorectal cancer [82, 83], the identification of the luminal compounds at the origin of mutations in these cells, as well as the threshold of concentrations above which genotoxic effects are observed, represents important parameters to be determined.
Another important point to take into consideration is related to the capacity of the bacterial metabolites to cross the mucus layers before entering colonocytes through the brush-border membranes. As a matter of fact, much experimental studies have been performed with colonocytes directly exposed to bacterial metabolites dissolved in the incubation medium. From that point of view, intraluminal colonic instillation of bacterial metabolites in anesthetized animals represents an experimental design which is closer to the physiological situation [8].
Finally, by better identifying the changes in the luminal environment, which are associated with both dietary modifications and/or physical exercise and which increase or decrease the risk of alteration of the normal process of colonic/rectal epithelia renewal and functions, it will become possible to intervene rationally for limiting the risk of pathology from inflammatory and neoplasic type in these anatomical parts of the intestine.
Abbreviations
- AMPK:
-
AMP-activated protein kinase
- ATP:
-
Adenosine triphosphate
- COX-2:
-
Cyclooxygenase-2
- FXR:
-
Farnesoid X receptor (FXR)
- H2S:
-
Hydrogen sulfide
- Hsp70:
-
Heat shock protein 70
- MDR:
-
Multidrug resistance
- NF-κB:
-
Factor nuclear kappa B
- PPAR-α:
-
Peroxisome proliferator-activated receptor alpha
- SCFA:
-
Short-chain fatty acids
- SQR:
-
Sulfide quinone reductase
- SREBP-1c:
-
Steroid response element binding protein 1-c
- TGR5:
-
G-coupled membrane protein 5
- VO2max:
-
Maximum oxygen consumption
References
Barker N. Adult intestinal stem cells: critical drivers of epithelial homeostasis and regeneration. Nat Rev Mol Cell Biol. 2014;15:19–33.
Payne CM, Fass R, Bernstein H, Giron J, Bernstein C, Dvorak K, Garewal H. Pathogenesis of diarrhea in the adult: diagnostic challenges and life-threatening conditions. Eur J Gastroeneterol Hepatol. 2006;18:1047–51.
Terzic J, Grivennikov S, Karin E, Karin M. Inflammation and colon cancer. Gastroenterology. 2010;138:2101–44.
Macfarlane GT, Macfarlane S. Human colonic microbiota: ecology, physiology, and metabolic potential of intestinal bacteria. Scand J Gastroenterol. 1997;222:3–9.
Duncan SH, Belenguer A, Holtrop G, Johnstone AM, Flint HJ, Lobley GE. Reduced dietary intake of carbohydrates by obese subjects results in decreased concentrations of butyrate and butyrate-producing bacteria in feces. Appl Environ Microbiol. 2007;73:1073–8.
Reddy B, Engle A, Katsifis S, Simi B, Bartram HP, Perrino P, Mahan C. Biochemical epidemiology of colon cancer: effect of types of dietary fiber on fecal mutagens, acid, and neutral sterols in healthy subjects. Cancer Res. 1989;49:4629–35.
Gaudichon C, Mahe S, Benamouzig R, Luengo C, Fouillet H, Dare S, Van Oycke M, Ferriere F, Rautureau J, Tome D. Net postprandial utilization of [15N]-labeled milk protein nitrogen is influenced by diet composition in humans. J Nutr. 1999;129:890–5.
Beaumont M, Andriamihaja M, Lan A, Khodorova N, Audebert M, Blouin JM, Grauso M, Lancha L, Benetti PH, Benamouzig R, Tomé D, Bouillaud F, Davila AM, Blachier F. Detrimental effects for colonocytes of an increased exposure to luminal sulfide: the adaptive response. Free Radic Biol Med. 2016;93:155–64.
Andriamihaja M, Lan A, Beaumont M, Audebert M, Wong X, Yamada K, Yin Y, Tomé D, Carrasco-Pozo C, Gottelend M, Kong X, Blachier F. The deleterious metabolic and genotoxic effects of the bacterial metabolite p-cresol on colonic epithelial cells. Free Radic Biol Med. 2015;85:219–27.
Windey K, De Preter V, Verbeke K. Relevance of protein fermentation to gut health. Mol Nutr Food Res. 2012;56:184–96.
Petry N, Egli I, Chassard C, Lacroix C, Hurrell R. Inulin modifies the bifidobacteria population, fecal lactate concentration, and fecal pH but does not influence iron absorption in women with low iron status. Am J Clin Nutr. 2012;96:325–31.
Russell WR, Gratz SW, Duncan SH, Holtrop G, Ince J, Scobbie L, Duncan G, Johnstone AM, Lobley GE, Wallace RJ, Duthie GG, Flint HJ. High-protein, reduced carbohydrate weight-loss diets promote metabolic profiles likely to be detrimental to colonic health. Am J Clin Nutr. 2011;93:1062–72.
Zoetendal EG, Akkermans AD, De Vos WM. Temperature gradient gel electrophoresis analysis of 16S rRNA from human fecal samples reveals stable and host-specific communities of active bacteria. Appl Environ Microbiol. 1998;64:3854–9.
David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, Ling AV, Devlin AS, Varma Y, Fischbach MA, Biddinger SB, Dutton RJ, Turnbaugh PJ. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–63.
Bjerrum JT, Wang Y, Hao F, Coskun M, Ludwig C, Gunther U, Nielsen OH. Metabonomics of human fecal extracts characterize ulcerative colitis, Crohn’s disease and healthy individuals. Metabolomics. 2015;11:122–33.
Vipperla K, O’Keefe SJ. Diet, microbiota, and dysbiosis: a recipe for colorectal cancer. Food Funct. 2016;7:1731–40.
Blachier F, Beaumont M, Andriamihaja M, Davila AM, Lan A, Grauso M, Armand L, Benamouzig R, Tomé D. Changes in the luminal environment of the colonic epithelial cells and physiopathological consequences. Am J Pathol. 2017;187(3):476–86.
Blachier F, Boutry C, Bos C, Tomé D. Metabolism and functions of L-glutamate in the epithelial cells of the small and large intestines. Am J Clin Nutr. 2009;90:814S–21S.
Hamer HM, Jonkers D, Venema K, Vanhoutvin S, Toost FJ, Brummer RJ. Review article: the role of butyrate on colonic function. Aliment Pharmacol Ther. 2008;27:104–19.
Blachier F, Mariotti F, Huneau JF, Tomé D. Effects of amino acid-derived luminal metabolites on the colonic epithelium and physiopathological consequences. Amino Acids. 2007;33:547–62.
Chun C, Zheng L, Colgan SP. Tissue metabolism and host-microbial interactions in the intestinal mucosa. Free Radic Biol Med. 2017;105:86–92.
Thibault R, Blachier F, Darcy-Vrillon B, de Coppet P, Bourreille A, Segain JP. Butyrate utilization by the colonic mucosa in inflammatory bowel diseases: a transport deficiency. Inflamm Bowel Dis. 2010;16:684–95.
Andriamihaja M, Chaumontet C, Tomé D, Blachier F. Butyrate metabolism in human colon carcinoma cells: implications concerning its growth-inhibitory effect. J Cell Physiol. 2009;218:58–65.
Fu M, Zhang W, Wu L, Yang G, Li H, Wang R. Hydrogen sulfide (H2S) metabolism in mitochondria and its regulatory role in energy production. Proc Natl Acad Sci U S A. 2012;109(8):2943–8.
Szabo C, Ransy C, Módis K, Andriamihaja M, Murghes B, Coletta C, Olah G, Yanagi K, Bouillaud F. Regulation of mitochondrial bioenergetic function by hydrogen sulfide. Part I. Biochemical and physiological mechanisms. Br J Pharmacol. 2014;171(8):2099–122.
Lagoutte E, Mimoun S, Andriamihaja M, Chaumontet C, Blachier F, Bouillaud F. Oxidation of hydrogen sulfide remains a priority in mammalian cells and causes reverse electron transfer in colonocytes. Biochim Biophys Acta. 2010;1797(8):1500–11.
Wallace JL, Ferraz JG, Muscara MN. Hydrogen sulfide: an endogenous mediator of resolution of inflammation and injury. Antioxid Redox Signal. 2012;17(1):58–67.
Oh GS, Pae HO, Lee BS, Kim BN, Kim JM, Kim HR, Jeon SB, Jeon WK, Chae HJ, Chung HT. Hydrogen sulfide inhibits nitric oxide production and nuclear factor-kappaB via heme oxygenase-1 expression in RAW264.7 macrophages stimulated with lipopolysaccharide. Free Radic Biol Med. 2006;41(1):106–19.
Bucci M, Papapetropoulos A, Vellecco V, Zhou Z, Pyriochou A, Roussos C, Roviezzo F, Brancaleone V, Cirino G. Hydrogen sulfide is an endogenous inhibitor of phosphodiesterase activity. Arterioscler Thromb Vasc Biol. 2010;30(10):1998–2004.
Distrutti E, Sediari L, Mencarelli A, Renga B, Orlandi S, Antonelli E, Roviezzo F, Morelli A, Cirino G, Wallace JL, Fiorucci S. Evidence that hydrogen sulfide exerts antinociceptive effects in the gastrointestinal tract by activating KATP channels. J Pharmacol Exp Ther. 2006;316(1):325–35.
Zanardo RC, Brancaleone V, Distrutti E, Fiorucci S, Cirino G, Wallace JL. Hydrogen sulfide is an endogenous modulator of leukocyte-mediated inflammation. FASEB J. 2006;20(12):2118–20.
Leschelle X, Goubern M, Andriamihaja M, Blottiere HM, Couplan E, Gonzales-Barroso MD, Petit C, Pagniez A, Chaumontet C, Mignotte B, Bouillaud F, Blachier F. Adaptative metabolic response of human colonic epithelial cells to the adverse effects of the luminal compound sulfide. Biochim Biophys Acta. 2005;1725:201–12.
Mimoun S, Andriamihaja M, Chaumontet C, Atanasiu C, Benamouzig R, Blouin JM, Tomé D, Bouillaud F, Blachier F. Detoxification of H2S by differentiated colonic epithelial cells: implication of the sulfide-oxidizing unit and of the cell respiratory capacity. Antiox Redox Signal. 2012;17:1–10.
Arijs I, Vanhove W, Rutgeerts P, Schuit F, Verbeke K, De Preter V. Decreased mucosal sulfide detoxification capacity in patients with Crohn’s disease. Inflamm Bowel Dis. 2013;19(5):E70–2.
De Preter V, Arijs I, Windey K, Vanhove W, Vermeire S, Schuit F, Rutgeerts P, Verbeke K. Decreased mucosal sulfide detoxification is related to an impaired butyrate oxidation in ulcerative colitis. Inflamm Bowel Dis. 2012;18(12):2371–80.
Szabo C, Coletta C, Chao C, Módis K, Szczesny B, Papapetropoulos A, Hellmich MR. Tumor-derived hydrogen sulfide, produced by cystathionine-β-synthase, stimulates bioenergetics, cell proliferation, and angiogenesis in colon cancer. Proc Natl Acad Sci U S A. 2013;110(30):12474–9.
Cremin JD, Fitch MD, Fleming SE. Glucose alleviates ammonia-induced inhibition of short-chain fatty acid metabolism in rat colonic epithelial cells. Am J Phys. 2003;285:G105–14.
Andriamihaja M, Davila AM, Eklou-Lawson M, Petit N, Delpal S, Allek F, Blais A, Delteil C, Tomé D, Blachier F. Colon luminal content and epithelial cell morphology are markedly modified in rats fed with a high-protein diet. Am J Phys. 2010;299:G1030–7.
Eklou-Lawson M, Bernard F, Neveux N, Chaumontet C, Bos C, Davila-Gay AM, Tomé D, Cynober L, Blachier F. Colonic luminal ammonia and portal blood L-glutamine and L-arginine concentrations: a possible link between colon mucosa and liver ureagenesis. Amino Acids. 2009;37:751–60.
Mouillé B, Robert V, Blachier F. Adaptative increase of ornithine production and decrease of ammonia metabolism in rat colonocytes after hyperproteic diet ingestion. Am J Phys. 2004;287:G344–51.
Blachier F, Davila AM, Mimoun S, Benetti PH, Atanasiu C, Andriamihaja M, Benamouzig R, Bouillaud F, Tomé D. Luminal sulfide and large intestine mucosa: friend or foe? Amino Acids. 2010;39:335–47.
Costa AV, Leite G, Resende A, Blachier F, Lancha AH Jr. Exercise, nutrition and gut microbiota: possible links and consequences. Int J Sport Exercise Med. 2017; (in press)
Evans CC, LePard KJ, Kwak JW, et al. Exercise prevents weight gain and alters the gut microbiota in a mouse model of high fat diet-induced obesity. PLoS One. 2014;9(3):e92193.
Wong JMW, de Souza R, Kendall CWC, Emam A, Jenkins DJA. Colonic health: fermentation and short chain fatty acids. J Clin Gastroenterol. 2006;40(3):235–43.
Matsumoto M, Inoue R, Tsukahara T, et al. Voluntary running exercise alters microbiota composition and increases n-butyrate concentration in the rat cecum. Biosci Biotechnol Biochem. 2008;72(2):572–6.
Lewis K, Lutgendorff F, Phan V, Söderholm JD, Sherman PM, McKay DM. Enhanced translocation of bacteria across metabolically stressed epithelia is reduced by enhanced translocation of bacteria across metabolically stressed epithelia is reduced by butyrate. Inflamm Bowel Dis. 2010;16(7):1138–48.
Tremaroli V, Bäckhed F. Functional interactions between the gut microbiota and host metabolism. Nature. 2012;489(7415):242–9.
den Besten G, Gerding A, van Dijk TH, Ciapaite J, Bleeker A, van Eunen K, Havinga R, Groen AK, Reijngoud DJ, Bakker BM. Protection against the metabolic syndrome by guar gum-derived short-chain fatty acids depends on peroxisome proliferator-activated receptor γ and glucagon-like Peptide-1. PLoS One. 2015;10(8):e0136364.
Monolayers C-C, Peng L, Li Z, Green RS, Holzman IR, Lin J. Butyrate enhances the intestinal barrier by facilitating tight junction assembly via activation of AMP-activated protein kinase. J Nutr. 2009;139(9):1619–25.
Mika A, Van Treuren W, González A, Herrera JJ. Exercise is more effective at altering gut microbial composition and producing stable changes in lean mass in juvenile versus adult male F344 rats. PLoS One. 2015;10(5):e0125889.
Aronsson L, Huang Y, Parini P, Korach-André M, Hakansson J, Gustafsson JA, et al. Decreased fat storage by Lactobacillus paracasei is associated with increased levels of Angiopoietin-like 4. PLoS One. 2010;5(9):e13087.
Johansson MEV, Larsson JMH, Hansson GC. The two mucus layers of colon are organized by the MUC2 mucin, whereas the outer layer is a legislator of host—microbial interactions. Proc Natl Acad Sci U S A. 2011;108(Suppl 1):4659–65.
Malago JJ, Koninkx JFJG, Van Dijk JE. The heat shock response and cytoprotection of the intestinal epithelium. Cell Stress Chaperones. 2002;7(2):191–9.
Hagio M, Matsumoto M, Yajima T, Hara H, Ishizuka S. Voluntary wheel running exercise and dietary lactose concomitantly reduce proportion of secondary bile acids in rat feces. J Appl Physiol (1985). 2010;109(3):663–8.
Kurdi P, Kawanishi K, Mizutani K, Yokota A. Mechanism of growth inhibition by free bile acids in lactobacilli and bifidobacteria. J Bacteriol. 2006;188(5):1979–86.
Islam KBMS, Fukiya S, Hagio M, Fujii N, Ishizuka S. Bile acid is a host factor that regulates the composition of the cecal microbiota in rats. Gastroenterology. 2011;141(5):1773–81.
David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, Ling AV, Devlin AS, Varma Y, Fischbach MA, Biddinger SB, Dutton RJ, Turnbaugh PJ. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505(7484):559–63.
Nie YF, Hu J, Yan XH. Cross-talk between bile acids and intestinal microbiota in host metabolism and health. J Zhejiang Univ Sci B. 2015;16(6):436–46.
Joyce SA, Gahan CG. Bile acid modifications at the microbe-host interface: potential for nutraceutical and pharmaceutical interventions in host health. Annu Rev Food Sci Technol. 2016;7:313–33.
Kikugawa K, Kato T. Formation of a mutagenic diazoquinone by interaction of phenol with nitrite. Food Chem Toxicol. 1988;26:209–14.
Hinzman MJ, Novotny C, Ullah A, Shamsuddin AM. Fecal mutagen fecapentaene-12 damages mammalian colon epithelial DNA. Carcinogenesis. 1987;8:1475–9.
Hamer HM, De Preter V, Windey K, Verbeke K. Functional analysis of colonic bacterial metabolism: relevant to health? Am J Phys. 2012;302:G1–9.
Seitz HK, Simanowski UA, Garzon FT, Rideout JM, Peters TJ, Koch A, Berger M, Einecke H, Maiwald M. Possible role of acetaldehyde in ethanol-related rectal cocarcinogenesis in the rat. Gastroenterology. 1990;98:406–13.
Gill CI, Rowland IR. Diet and cancer: assessing the risk. Br J Nutr. 2002;88:S73–87.
Ijssennagger N, Belzer C, Hooiveld GJ, Dekker J, van Mil SW, Muller M, Kleerebezem M, van der Meer R. Gut microbiota facilitates dietary heme-induced epithelial hyperproliferation by opening the mucus barrier in colon. Proc Natl Acad Sci U S A. 2015;112:10038–43.
Wang A, Keita AV, Phan V, McKay CM, Schoultz I, Lee J, Murphy MP, Fernando M, Ronaghan N, Balce D, Yates R, Dicay M, Beck PL, MacNaughton WK, Soderholm JD, McKay DM. Targeting mitochondria-derived reactive oxygen species to reduce epithelial barrier dysfunction and colitis. Am J Pathol. 2014;184:2516–27.
Motta JP, Flannigan KL, Agbor TA, Beatty JK, Blackler RW, Workentine ML, Da Silva GJ, Wang R, Buret AG, Wallace JL. Hydrogen sulfide protects from colitis and restores intestinal microbiota biofilm and mucus production. Inflamm Bowel Dis. 2015;21(5):1006–17.
Bansal T, Alaniz RC, Wood TK, Jayaraman A. The bacterial signal indole increases epithelial cell tight junction resistance and attenuates indicators of inflammation. Proc Natl Acad Sci U S A. 2010;107:228–33.
Peng L, Zi ZR, Green RS, Holzman IR, Lin J. Butyrate enhances the intestinal barrier by facilitating tight junction assembly via activation of AMP-activated protein kinase in Caco-2 cell monolayers. J Nutr. 2009;138:1619–25.
McDougall CJ, Wong R, Scudera P, Lesser M, DeCosse JJ. Colonic mucosal pH in humans. Dig Dis Sci. 1993;38:542–5.
Nugent SG, Kumar D, Rampton DS, Evans DF. Intestinal luminal pH in inflammatory bowel disease: possible determinants and implications for therapy with aminosalicylates and other drugs. Gut. 2001;48:571–7.
Jacobs LR, Lupton JR. Relationship between colonic luminal pH, cell proliferation, and colon carcinogenesis. Cancer Res. 1986;46:1727–34.
Christl SU, Bartram HP, Paul A, Kelber E, Scheppach W, Kasper H. Bile acid metabolism by colonic bacteria in continuous culture: effects of starch and pH. Ann Nutr Metab. 1997;41:45–51.
Lan A, Lagadic-Gossmann D, Lemaire C, Brenner C, Jan G. Acidic extracellular pH shifts colorectal cancer cell death from apoptosis to necrosis upon exposure to propionate and acetate, major end products of the human probiotic propionibacteria. Apoptosis. 2007;12:573–91.
Wei LY, Roepe PD. Low external pH and osmotic shock increase the expression of human MDR protein. Biochemistry. 1994;33:7229–38.
Campbell SC, Wisniewski PJ, Noji M, McGuinness LR, Haggblom MM, Lightfoot SA, Joseph LB, Kerkhof LJ. The effects of diet and exercise on intestinal integrity and microbial diversity in mice. PLoS One. 2016;11(3):e0150502.
Monda V, Villano I, Messina A, Valenzano A, Esposito T, Moscatelli F, et al. Exercise modifies the gut microbiota with positive health effects. Oxidative Med Cell Longev. 2017;2017:3831972.
Petriz BA, Castro AP, Almeida JA, Gomes CP, Fernandes GR, Kruger RH, Pereira RW, Franco OL. Exercise induction of gut microbiota modifications in obese, non-obese and hypertensive rats. BMC Genomics. 2014;15(1):511.
Clarke SF, Murphy EF, O’Sullivan O, Lucey AJ, Humphreys M, Hogan A, Hayes P, O’Reilly M, Jeffery IB, Wood-Martin R, Kerins DM, Quigley E, Ross RP, O’Toole PW, Molloy MG, Falvey E, Shanahan F, Cotter PD. Exercise and associated dietary extremes impact on gut microbial diversity. Gut. 2014;63:1913–20.
Kang SS, Jeraldo PR, Kurti A, Miller ME, Cook MD, Whitlock K, Goldenfeld N, Woods JA, White BA, Chia N, Fryer JD. Diet and exercise orthogonally alter the gut microbiome and reveal independent associations with anxiety and cognition. Mol Neurodegener. 2014;9:36.
Estaki M, Pither J, Baumeister P, Leittle JP, Gill SK, Ghsosh S, et al. Cardiorespiratory fitness as a predictor of intestinal microbial diversity and distinct metagenomic functions. Microbiome. 2016;8(4):42.
Barker N, Ridgway RA, van Es JH, van de Wetering M, Begthel H, van den Born M, Danenberg E, Clarke AR, Sansom OJ, Clevers H. Crypt stem cells as the cells of origin of intestinal cancer. Nature. 2009;457:608–11.
Ricci-Vitiani L, Fabrizi E, Palio E, De Maria R. Colon cancer stem cells. J Mol Med (Berl). 2009;87:1097–104.
Acknowledgements
The authors wish to thank the University of Sao Paulo, INRA, AgroParisTech, and Université Paris-Saclay for their supports that started this new research focus on 2013 with the FAPESP grants 2012/07319-0. This review is originating from a conference presented on October 20, 2016, at the International Symposium on Exercise, Nutrition and Gut Microbiota, University of Sao Paulo, Brazil – Sponsor by FAPESP Grants 2014/13235-9.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the construction of this manuscript, mainly with respect to the idea, writing, and revision of the same one. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Blachier, F., de Sá Resende, A., da Silva Fogaça Leite, G. et al. Colon epithelial cells luminal environment and physiopathological consequences: impact of nutrition and exercise. Nutrire 43, 2 (2018). https://doi.org/10.1186/s41110-018-0061-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41110-018-0061-6