Abstract
Background
Sepsis is a systemic inflammatory response syndrome caused by infectious disease. Severe sepsis and septic shock are extremely serious conditions with poor prognoses. It is reported that cytokines are deeply involved in the disease mechanism. Continuous hemodiafiltration (CHDF) using a poly(methyl methacrylate) (PMMA) membrane is reported to adsorb various cytokines and improve the status of patients with sepsis. Recently, another cytokine-adsorbing hemofilter, acrylonitrile-co-methallyl sulfonate surface-treated (AN69ST) membrane, has become available for CHDF in patients with sepsis. However, the clinical efficacy of this membrane remains unclear. Therefore, in this study, we compared the efficacy of AN69ST and PMMA membranes.
Methods
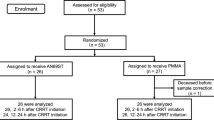
This retrospective study included patients with severe sepsis or septic shock who underwent CHDF for at least 24 h in the intensive care unit from January 2013 to August 2016.
Results
This study included 49 patients who underwent CHDF, 32 using an AN69ST membrane and 17 using a PMMA membrane. In the AN69ST and PMMA groups, average age was 71.1 ± 11.4 years and 74.7 ± 9.4 years, respectively, and percentage of men was 71.9 and 88.2%, respectively. Severity of sepsis and vital signs were not significantly different between groups at the start of CHDF. In addition, 28-day mortality was not significantly different between groups (43.8 vs. 35.3%, P = 0.1625). However, heart rate in the AN69ST group decreased significantly early in the course of CHDF (6, 12, and 24 h, P < 0.05) compared with the PMMA group.
Conclusions
AN69ST and PMMA membranes showed equivalent efficacy. Furthermore, CHDF using an AN69ST membrane may be effective for early stabilization of vital signs.
Similar content being viewed by others
Background
Sepsis is a systemic inflammatory response syndrome caused by infectious disease [1]. Severe sepsis and septic shock are extremely serious conditions with poor prognoses [2, 3]. It is reported that cytokines are deeply involved in the disease mechanism. Although various treatments for sepsis have been used, none has been sufficient. Of the available options, blood purification therapy for cytokine removal is reported to be successful [4]. With regard to high-flow and high-volume renal replacement therapy, results have been positive [5, 6] or negative [7, 8], with no clear conclusion. However, continuous renal replacement therapy (CRRT), which removes cytokines by taking advantage of the characteristics of membranes, such as poly(methyl methacrylate) (PMMA), is often used [9, 10]. Although another hemofilter, acrylonitrile-co-methallyl sulfonate surface-treated (AN69ST) membrane, has recently become available in Japan [11], results regarding its clinical efficacy are scarce. In addition, there is no study comparing the AN69ST membrane with another hemofilter with cytokine-adsorption ability, such as PMMA. Therefore, in this study, we investigated the clinical efficacy of the AN69ST membrane in the acute phase.
Methods
Patients and data collection
This retrospective study included patients with severe sepsis or septic shock who underwent CRRT for at least 24 h in the intensive care unit from January 2013 to August 2016. Sepsis was diagnosed by meeting at least two systemic inflammatory response syndrome criteria due to a presumed infection [1]. Severe sepsis is that causing organ dysfunction. As CRRT, continuous hemodiafiltration (CHDF) was performed, starting with a dialysate flow rate of 400 mL/h and a replacement solution flow rate of 400 mL/h, which was adjusted appropriately. A double-lumen catheter was placed in the internal jugular vein as vascular access. Heparin and/or nafamostat mesylate was used with judgment in each case. Judgment of when to start and finish CHDF was determined by consultation with multiple intensive care staff members and nephrologists. The membranes used for CHDF were PMMA and AN69ST.
At the start of CHDF, patients’ age, sex, physical findings, cause of sepsis, and laboratory data were collected from their medical records. Acute Physiology and Chronic Health Evaluation II (APACHE II) [12] and sequential organ failure assessment (SOFA) [13] scores also were calculated. Vital signs and catecholamine index (CAI) were evaluated at the start of CHDF and at 6, 12, 24, 48, and 72 h. Twenty-eight-day survival rate was also calculated. Patients’ vital signs and CAI at 72 h were included even if CHDF was already finished at that time. CAI was calculated as follows: dopamine level (μg/kg/min) + dobutamine level (μg/kg/min) + noradrenaline level (μg/kg/min) × 100.
Statistical analysis
Baseline characteristics were presented descriptively with average and SD values and were tested using the Mann-Whitney U test for parametrical data and χ 2 test for nonparametrical data. Logistic regression analysis and stratified analysis were performed to evaluate 28-day survival. P values of <0.05 were considered statistically significant.
Results
Baseline characteristics
Table 1 shows the clinical characteristics of the 49 patients included in this study. Of them, 32 underwent CHDF using an AN69ST membrane, while 17 used a PMMA membrane; average age was 71.1 ± 11.4 years and 74.7 ± 9.4 years, respectively, and percentage of men was 71.9 and 88.2%, respectively. As a result, almost all CHDF was performed with AN69ST membrane after becoming available although discussed by multiple intensive care staff members and nephrologists. Severity of sepsis and vital signs at the start of CHDF were not significantly different between groups. The percentage of ventilator user did not show significant difference between both groups. Compared with patients using an AN69ST membrane, those using a PMMA membrane received combination therapy with polymyxin B-immobilized fiber column hemoperfusion (PMX) more frequently (58.8 vs. 25.0%, P = 0.0194).
Comparison of 28-day mortality
Figure 1 shows the Kaplan-Meier plot of 28-day survival in patients who underwent CHDF using an AN69ST or PMMA membrane. Twenty-eight-day mortality was not significantly different between groups (43.8 vs. 35.3%, P = 0.1625). Figures 2 and 3 show stratified analysis according to APACHE II and SOFA scores without kidney score. Figure 4 shows the forest plot of odds ratios for 28-day survival. Stratified and multivariate analyses showed no significant difference in mortality between groups. Furthermore, the level of creatinine at 28 days was not different significantly (Table 1).
Forest plot of odds ratios (ORs) for 28-day survival with continuous hemodiafiltration using an acrylonitrile-co-methallyl sulfonate surface-treated (AN69ST) membrane. APACHE II Acute Physiology and Chronic Health Evaluation II, CI confidence interval, MBP mean blood pressure, PMX polymyxin B-immobilized fiber column hemoperfusion
Time course of vital signs and CAI
Figure 5a shows blood pressure in patients who underwent CHDF using an AN69ST or PMMA membrane. There were no significant differences between groups. Figure 5b shows heart rate (HR) and body temperature in such patients. Early in the course of CHDF (6, 12, and 24 h), patients using an AN69ST membrane showed more stable HR than those using a PMMA membrane. Figure 6 shows various parameters which affect vital signs. There was no difference in CAI, fluid removal rate, or the level of albumin.
Discussion
In this study, we compared patients with sepsis who underwent CHDF using an AN69ST or PMMA membrane. AN69ST and PMMA membranes showed equivalent survival. Furthermore, patients using an AN69ST membrane demonstrated rapid stabilization of HR.
There has been no report comparing the clinical efficacy of AN69ST and PMMA membranes. Our study is distinctive in that we focused on patients with sepsis. Some previous studies have reported that CHDF using an AN69ST membrane showed significantly better survival than expected in patients with sepsis [14, 15]. The present report showed nearly equal survival between AN69ST and PMMA membranes, indicating the effectiveness of AN69ST. However, the expected survival rate from APACHE II scores is of a considerably old age, and caution is necessary because survival is considered to be further improved by the current progress in treatment.
When performing CHDF, there are renal and nonrenal indications. In the latter case, cytokine removal is the main purpose. In patients with sepsis, cytokine storm plays a central role in the pathologic condition, and cytokine removal is considered to be effective, as in this study. In the present study, there were no significant differences in urea nitrogen or creatinine levels at the start of CHDF between groups. Furthermore, because multiple intensive care unit physicians and nephrologists at a single institution decided when to start and finish CHDF by discussion, there was little deviation in the criteria for CHDF, even though different membranes with cytokine-adsorption ability were selected. In this study, although we did not measure the levels of cytokines, we presumed that rapid HR stabilization was due to cytokine removal because other parameters which affect HR, such as body temperature, dose of dopamine, fluid removal rate, and the level of albumin, did not show significant difference between both groups.
In our study, although the differences were not significant, the AN69ST group tended to have more severe values for SOFA score, lactate level, and CAI. However, the equivalent survival between groups seems to indicate the effectiveness of the AN69ST membrane. In addition, HR stabilized faster in the AN69ST group than in the PMMA group. We consider that this may be due to the difference in mechanisms: the AN69ST membrane adsorbs cytokines by utilizing an electrical charge, while the PMMA membrane adsorbs cytokines by ensnaring them in the surface pores [16]. However, because we did not measure cytokine level, we are not able to discuss this point further. Nonetheless, it is possible that cytokine easily removed by the AN69ST membrane contributed to earlier improvement of vital signs.
For comparison between membranes, we targeted patients who underwent CHDF for more than 24 h. Patients who died within 24 h after the start of CHDF were too critical to evaluate the differences between membranes. These most severe cases have pathologic conditions with advanced organ dysfunction and may require intensive treatment at an earlier stage.
The prevalence of PMX usage was significantly higher in PMMA group. In this study, after becoming available, almost all CHDF was performed using AN69ST membrane without PMX. It may be a facility trend. Because the efficacy of PMX is reported [17], identical prognosis in AN69ST membrane group with low prevalence of PMX usage may be showing advantageous aspect, comparing to PMMA group with higher prevalence of PMX usage.
On the other hand, cost of medical equipments is an important problem. As of 2016 in Japan, AN69ST membrane is about 10% more expensive than PMMA membrane. In this study, we did not examine the life span of membranes because we changed membranes every 24 h before clotting. If life span of AN69ST membrane is longer, the cost problem may be solved.
Our study has some limitations. First, because this was a retrospective study, the backgrounds of both groups were not completely matched. In addition, criteria for the start of CHDF were not clearly defined. However, because multiple physicians determined when to start and finish CHDF by discussion, it is considered that there was no large deviation in judgment. Nonetheless, the start and end criteria for CHDF should be clear. Second, we did not measure the cytokine level. Because HR was stabilized early in the AN69ST group, we should determine whether this was due to the type of cytokines that can be removed.
Conclusions
Patients who underwent CHDF using an AN69ST or PMMA membrane showed similar prognoses. Furthermore, CHDF using an AN69ST membrane may be effective for early stabilization of vital signs.
Abbreviations
- AN69ST:
-
Acrylonitrile-co-methallyl sulfonate surface-treated
- APACHE II:
-
Acute Physiology and Chronic Health Evaluation II
- CAI:
-
Catecholamine index
- CHDF:
-
Continuous hemodiafiltration
- CRRT:
-
Continuous renal replacement therapy
- HR:
-
Heart rate
- PMMA:
-
Poly(methyl methacrylate)
- PMX:
-
Polymyxin B-immobilized fiber column hemoperfusion
- SOFA:
-
Sequential organ failure assessment
References
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31:1250–6.
Moreno RP, Metnitz B, Adler L, Hoechtl A, Bauer P, Metnitz PG, et al. Sepsis mortality prediction based on predisposition, infection and response. Intensive Care Med. 2008;34:496–504.
Silva E, Pedro Mde A, Sogayar AC, Mohovic T, Silva CL, Janiszewski M, et al. Brazilian Sepsis Epidemiological Study (BASES study). Crit Care. 2004;8:R251–60.
Bellomo R, Tipping P, Boyce N. Continuous veno-venous hemofiltration with dialysis removes cytokines from the circulation of septic patients. Crit Care Med. 1993;21:522–6.
Ronco C, Bellomo R, Homel P, Brendolan A, Dan M, Piccinni P, et al. Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet. 2000;356:26–30.
Saudan P, Niederberger M, De Seigneux S, Romand J, Pugin J, Perneger T, et al. Adding a dialysis dose to continuous hemofiltration increases survival in patients with acute renal failure. Kidney Int. 2006;70:1312–7.
RENAL Replacement Therapy Study Investigators, Bellomo R, Cass A, Cole L, Finfer S, Gallagher M, et al. Intensity of continuous renal-replacement therapy in critically ill patients. N Engl J Med. 2009;361:1627–38.
VA/NIH Acute Renal Failure Trial Network, Palevsky PM, Zhang JH, O'Connor TZ, Chertow GM, Crowley ST, et al. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008;359:7–20.
Nakamura M, Oda S, Sadahiro T, Hirayama Y, Watanabe E, Tateishi Y, et al. Treatment of severe sepsis and septic shock by CHDF using a PMMA membrane hemofilter as a cytokine modulator. Contrib Nephrol. 2010;166:73–82.
Matsuda K, Moriguchi T, Harii N, Yanagisawa M, Harada D, Sugawara H. Comparison of efficacy between continuous hemodiafiltration with a PMMA high-performance membrane dialyzer and a PAN membrane hemofilter in the treatment of septic shock patients with acute renal failure. Contrib Nephrol. 2011;173:182–90.
Haase M, Bellomo R, Baldwin I, Haase-Fielitz A, Fealy N, Davenport P, et al. Hemodialysis membrane with a high-molecular-weight cutoff and cytokine levels in sepsis complicated by acute renal failure: a phase 1 randomized trial. Am J Kidney Dis. 2007;50:296–304.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10.
Shiga H, Hirasawa H, Nishida O, Oda S, Nakamura M, Mashiko K, et al. Continuous hemodiafiltration with a cytokine-adsorbing hemofilter in patients with septic shock: a preliminary report. Blood Purif. 2014;38:211–8.
Hirasawa H, Oda S, Nakamura M, Watanabe E, Shiga H, Matsuda K. Continuous hemodiafiltration with a cytokine-adsorbing hemofilter for sepsis. Blood Purif. 2012;34:164–70.
Yumoto M, Nishida O, Moriyama K, Shimomura Y, Nakamura T, Kuriyama N, et al. In vitro evaluation of high mobility group box 1 protein removal with various membranes for continuous hemofiltration. Ther Apher Dial. 2011;15:385–93.
Cruz DN, Antonelli M, Fumagalli R, Foltran F, Brienza N, Donati A, et al. Early use of polymyxin B hemoperfusion in abdominal septic shock: the EUPHAS randomized controlled trial. JAMA. 2009;301:2445–52.
Acknowledgements
We would like to thank Editage (www.editage.jp) for the English language editing.
Funding
Not applicable.
Availability of data and materials
Please contact the author for data requests.
Authors’ contributions
AT and DI designed the study. AT performed the statistical analysis and wrote the manuscript. All authors participated in the care of the patients. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Institutional Review Board of Japanese Red Cross Nagoya Daini Hospital (No. 1044) and was conducted under the Declaration of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tanaka, A., Inaguma, D., Nakamura, T. et al. Effect of continuous hemodiafiltration using an AN69ST membrane in patients with sepsis. Ren Replace Ther 3, 12 (2017). https://doi.org/10.1186/s41100-017-0093-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-017-0093-z