Abstract
Background
Obesity in children has become one of the key concerns of the World Health Organization, and the incidence of related non-communicable diseases is also rising. This study evaluates the effect of family sports participation on the treatment and prevention of obesity in children aged 0–14 years by systematic analysis.
Method
A literature review from 2000 to 2020 was conducted. According to PRISMA-IPD (Preferred Reporting Items for MetaAnalyses of individual participant data) guidelines. The two researchers independently assessed the risk and bias of the articles, obtained a comprehensive, high-quality result, and extracted the data based on the Cochrane intervention system review manual. Randomized controlled trials (RCTs) were selected from the searches that used family sports interventions or family sports combined with dietary adjustments and behavioral habits change. Only studies targeting overweight or obese children aged 0–14 years were included.
Results
The search resulted in a total of 16 studies. Across all 16 studies, there were a total of 1680 participants in the experimental groups and 1701 participants in the control groups. The results are as follows: body mass index (BMI) (SMD-RE = − 4.10, 95% CI (− 0.84 to 0.02), Z = 1.88, p = 0.06); Body weight (SMD-RE = − 0.77, 95% CI (− 1.53 to − 0.01), Z = 2.00, p = 0.05); Waist circumference (SMD-RE = − 0.45, 95% CI (− 1.36 to 0.47), Z = 0.96, p = 0.34); and Body fat rate (SMD-FE = − 0.06, 95% CI (− 0.22 to 0.11), Z = 0.69, p = 0.49). Hence, through family sports intervention among obese children, juvenile and obese body composition—BMI, body weight, waist circumference, and body fat rate—are all reduced. But only body weight was statistically significant.
Conclusions
Compared with the samples without family sports, the weight of obese children participating in family sports decreased, but there were no significant differences in other relevant physical indicators. Follow-up research should examine large-scale clinical trials with family sports as a single factor intervention, which are needed to provide stronger evidence of the intervention effect. However, family activities can help obese children grow and develop by improving their exercise capacity, enhancing their lifestyles, and facilitating communication and relationships with their parents. In the future, long-term sports training plans for children with obesity should be implemented.
Similar content being viewed by others

Background
Over the last 40 years, childhood obesity has increased tenfold. The World Health Organization (WHO) predicts that the number of obese children will increase from 41 million in 2018 to a staggering 70 million by 2025, and the proportion of overweight or obese people is worrying [1]. Obese children (aged 0–14) are the research objects of pediatric obesity in the field of medicine [2]. Obesity has been linked to internal environment disorder, gene variation, organ mutation, iatrogenic conditions, viruses, environmental and behavioral characteristics, and performance genetics [3]. However, the main mechanisms underlying childhood obesity are the consumption of high-caloric food, remaining sedentary for extended periods of time, and nonparticipation in physical activity and exercise [4]. When caloric intake is higher than consumption, excess calories are stored in the body in the form of fat, which leads to the imbalance of energy metabolism that results in obesity [5].
Presently, pediatric obesity treatment mainly attempts to limit energy intake by changing a child’s lifestyle One of these lifestyle changes is engagement in family sports. Family sports are organized and selected by family members to satisfy their family's enjoyment of life and health needs through physical exercise activities, effectively correcting children's bad habits and cultivating participation in lifelong sports [6,7,8,9,10]. Family sports intervention is commonly used in clinical medical experiments for physical therapy aimed at certain diseases. Long-term family physical exercise can reduce the incidence of cardiovascular diseases and chronic diseases in children.
Families bear the basic social responsibility of raising and educating children. Family sports is a supplement to school sports and plays an irreplaceable role. The intervention object of family sports is not only for children, but also for parents [11]. Parents play a key role in enabling their children's fitness, as they are responsible for directly supervising and managing children's behavior. Parenting behavior (e.g., role model behavior for imitation by children; setting rules and boundaries; etc.) influences children's behavior and eating habits. Childhood behavior plays a significant role in determining lifelong preferences and healthy behaviors, so it is necessary to shape and form a good lifestyle as soon as possible [9, 12].
Parents or supervisors directly organize and enact physical activity plans to realize off-campus sports activities. School sports supervision and organization of children's physical activities are limited in time and space [7]. The implementation of school sports and community sports requires family sports to assist: The community provides sports facilities and logistical support [13], and relevant education departments should continue to provide children and their families with opportunities for sports and health education, improve their self-efficacy in participating in sports activities, and support the ability of families to organize sports activities independently [14]. The organic integration of family, school, and community sports cultivates engagement with sports resources inside and outside the school, creating a convenient environment for children to participate in physical activities.
In summary, the occurrence of obesity is closely related to lifestyle and behavior habits. Scientific family sports intervention is one of the most important methods for treating and intervening in children's obesity. However, there is no meta-analysis on children's obesity by family sports intervention, and it is impossible to get a clear result analysis.
Methods
This paper uses a meta-analysis method to systematically evaluate the intervention effect of family sports participation (single-factor and multifactor assistance) on children's obesity through a meta-analysis. Specifically, we examine how family sports intervention affects four key outcome indicators of obesity: body mass index (BMI), weight, waist circumference, and body fat rate.
Search strategy and study selection
Example keywords searches include “Family Sports,” “Children,” “Obesity,” and “Family Sports,” among others. The following databases were searched: China National Knowledge Infrastructure (CNKI), VIP, Scopus, WanFang, PubMed, Embase, SpringerLink, ScienceDirect, Google Scholar, Cochrane Library, and Web of Science. The time period during which we searched the literature was 2006–2020.
We use the Web of Science search as an example in Table 1 to illustrate our study’s search strategy. In the basic search, each subject word was searched separately from the free word, and then a combination search in the historical search was performed. The index system included Science Citation Index Expanded (SCI-E), Social Sciences Citation Index (SSCI), Arts and Humanities Citation Index (A&HCI), Conference Proceedings Citation Index—Science (CPCI-S), Conference Proceedings Citation Index—Social Sciences and Humanities (CPCI-SSH), Emerging Sources Citation Index (ESCI), Current Chemical Reactions—Expanded (CCR-E), and Index Chemicus (IC). The time span reflected all active years of research.
The results were exported and supplemented with literature tracing, manual search, and other methods to collect the text. A total of 4311 documents were retrieved. We used the EndNote X8 document management software to organize and review the documents. After reading the document titles, keywords, and abstracts, we excluded documents that were not related to the research intervention method, population, or research purpose of this topic, resulting in a sample of 125 papers. Finally, we excluded the data that did not sufficiently meet our statistical requirements for analysis. This resulted in a final sample of 16 papers.
Across all studies, the baseline of the experimental group and the control group was parallel and comparable, and all were clearly described.
Inclusion/exclusion criteria
Next, we looked to incorporate the literature in the PICOS paradigm, which is reflected as follows:
-
(P) Population. The research population is children (0–14 years old) with obesity. There are no restrictions on the gender and race of the study population.
-
Intervention. The purpose of physical exercise through the family sports intervention is to meet a given family's needs for both enjoyment and, more importantly, physical health. Examples of family sports intervention include aerobic exercise, confrontation training, high-intensity interval training and continuous training, low-intensity large-volume exercise, etc.
-
(C) Control. The experimental structure relies on the intervention of family sports participation or family sports combined with other interventions (diet adjustment, behavioral habits intervention). The control groups saw no interventions.
-
(O) Outcomes. The outcome index of treatment effects includes one or more of the following four obesity indicators: BMI, weight, waist circumference, and body fat rate.
-
(S) The experiments were designed as randomized controlled trials.
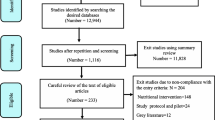
The process of document selection and inclusion is shown in Fig. 1. EndNote X8 document management software was used to organize and review the documents, read the document titles, keywords, and abstracts, and exclude documents that were irrelevant to the research intervention method, population, or research purpose of this topic. The Chinese literature search was restricted to core journals, such as SCI, CSCI, and CSCD. Non-Chinese studies were assembled from SCI-E, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI, and CCR-E.
Studies that emerged from the search results were excluded if they were not RCTs, had a sample size of less than 15, or whose research flow with regard to the intervention experiment was vague. Additionally, studies were excluded whose outcome indicators did not have one of the four indicators of BMI, weight, waist circumference, and body fat rate. There are no four indicators in the outcome indicators of the study. There are baseline data, lack of outcome data, and incomplete data in the research results.
Data extraction and quality assessment
Data were extracted independently by two authors using a standardized data extraction form. The extracted data were entered into a specialized database and checked independently by the third author. The basic information extracted included author, year, sample size, intervention/controls details, and outcome variables (weight, waist circumference, BMI, and body fat rate).
The quality assessment of the literature needed to be assessed by two independent authors using the Cochrane Risk of Bias Assessment Form. Quality assessment was performed for each study included in this meta-analysis, and a third reviewer was required to perform the quality assessment if disagreement remained after the assessment by two authors.
The literature risk quality evaluation of the 16 studies includes:
-
(a)
the selection of random methods;
-
(b)
whether there was implemented allocation concealment;
-
(c)
whether the participants and staff were blind;
-
(d)
whether the results were assessed using a blind method;
-
(e)
whether there were incomplete reporting outcomes;
-
(f)
whether there were selective reporting and other deviations.
Data synthesis and statistical analysis
Data statistics and meta-analysis were performed using RevMan 5 software, and effect scales were calculated by calculating weighted mean differences (WMD) or standardized mean differences (SMD) and 95% confidence intervals (CI) to assess the effectiveness of the home exercise intervention in each outcome indicator. Fixed-effects model tests were used in case of consistent outcome indicators or when the studies were homogeneous (I2 ≤ 50%, p > 0.1), and random-effects model tests were used in case of large heterogeneity in outcome indicators (I2 > 50%, p < 0.1).
The results of the analysis were interpreted using forest plots, and obese children were divided into two groups by child age classification criteria: preschool age 0–6 years and school age 7–14 years, and subgroup analysis was performed for each outcome indicator.
Results
Description of the included studies
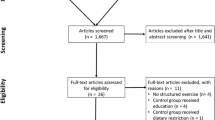
The flowchart of studies’ selection is presented in Fig. 1. Our electronic search identifies 4787 studies (6 from CNKI, 386 from PubMed, 3915 from Web of Science, 63 from Springer, 243 from Scopus, 24 from Embase, and 150 from ScienceDirect). Of those studies, 1897 citations were retrieved after the exclusion of duplicates. Among them, 0 study was excluded in EndNote literature management software. Then, screening is done by two authors reading the title and abstract. Both were required to reach a consensus, and if disagreement still existed after discussion, the opinion of a third reviewer was solicited. Ultimately, 16 studies met all of the inclusion criteria and were eligible to be included in the final meta-analysis [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30]. Tables 2 and 3 provide an overview.
Figure 2(1) and (2) shows that the overall quality risk from the literature is low. The risk bias summary chart shows that two of the articles (Döring et al. 2016 and Sacher et al. 2010) have high-risk bias. The intervention measures are composed of different exercise forms and different exercise doses, so it is impossible to judge whether the above key factors have potential influencing effects. The above evidence is insufficient and threatens the high quality of results. Participants and staff guide the experiments, and the resulting evaluation is not blind. The results of the report are not comprehensive, and some reports are optional statements (Table 4).
We document that because of the close interaction between family members and research members, participants were aware of the measurement method, which directly precludes blind measurement. Seven of the documents did not explain whether they were blind to the staff, and thus there might be a high risk of bias. Only four documents had a low risk of bias. At present, a long-term randomized controlled study on family sports as the main single factor intervention for juvenile obesity is currently being run. The differences in the degree of intervention of family sports combined with diet and behavior intervention and the length of intervention (3–39 months) lead to differences in the effect of outcome indicators [31, 32].
The impact of family sports intervention on children's BMI
From the perspective of clinical analysis, the intervention population of each literature has a relatively large span. Ages are divided into two subgroups of 0–6 years and 7–14 years for data processing and analysis. As can be seen from the forest chart in Fig. 3, the participation of family sports has a significant impact on the BMI of obese children.
For the 11 articles included in this analysis, the outcome index BMI system shows χ2 = 0.46, df = 10, p < 0.00001, I2 > 50%. The heterogeneity of the included literature is relatively high, and it can be analyzed with a random-effects model. SMD-RE = − 0.41, 95% CI (− 0.84 to 0.02), Z = 1.88, p = 0.06, which is not statistically significant. Among them, there are five subgroups of 0–6 years old and six subgroups of 7–14 years old, respectively. There were 1308 experimental groups and 1337 control groups.
Meta-results of 11 literature subgroups show χ2 = 4.10, df = 1, p = 0.04, I2 = 75.6%, and moderate subgroups differences decreased less. We exclude each article piecemeal to check the sensitivity and observe the results of the effect size change. The research results show that the merged results are highly robust. The total statistics reflect the overall situation of the 11 studies, and the effect differences between the experimental group and the control group are higher.
The results show that the intervention of family sports can reduce the BMI of obese children. Figure 4 shows two subgroup funnel charts: The white dots and red dots are concentrated in the middle and top of the vertical axis of the graph, indicating that the sample size is large, indicating greater accuracy. Hence, it is closer to the true value, and the distribution of points is relatively concentrated. Specifically, we observe that the publication bias of the above literature is low.
The effect of family sports intervention on children's weight
The forest chart in Fig. 5 shows that family sports participation has a significant impact on the weight of obese children. A total of seven articles were included in this analysis. The outcome index weight system analysis shows: χ2 = 1.00, df = 6, p < 0.00001, I2 > 50%. The heterogeneity of the included literature is relatively high and can only be analyzed with a random-effects model.
The seven studies on the influence of body weight show SMD-RE = − 0.77, 95% CI (− 1.53 to − 0.01), Z = 2.00, p = 0.05, which has a statistical significance. The intervention group and the control group have significant differences before and after the intervention. After excluding each article one by one to check the sensitivity, we observe no change in the result of the effect size, indicating that there is no literature to be excluded.
Additional evaluation shows that the results of the literature data merger are more robust. Among them, there are three subgroups for 0–6-year-old children and four subgroups of 7–14-year-old children. There were 499 experimental groups and 463 control groups.
Results of the meta-analysis show that for 0–6-year-old children the heterogeneity is almost zero (p = 0.56, I2 = 0%), whereas the 7–14-year-old children group possesses greater heterogeneity (p = 0.83, I2 = 0%). The difference between the two subgroups and the total subgroup indicates the heterogeneity of the systematic analysis of the subgroup literature (p < 0.00001, I2 = 99.4%). The diamond shape falls in the experimental group, which shows the effect analysis of the two sub-combinations. The difference between the experimental group and control group clearly shows that participation in family sports has a significant effect on weight loss in obese children.
The effect of family sports intervention on the waist circumference of children
As can be seen from the forest map in Fig. 6, participation in family sports has a significant impact on the waist circumference of obese children. A total of seven articles were included in this analysis. The outcome index weight system analysis shows that the heterogeneity of the included literature is relatively high and can only be analyzed with a random-effects model (χ2 = 1.47, df = 6, p < 0.00001, I2 > 50%). Seven articles on the impact of waist circumference show that a significant effect is not obvious (SMD-RE = − 0.45, 95% CI (− 1.36 to 0.47), Z = 0.96, p = 0.34). The diamond on the forest map leans to the left in the associated forest chart (Fig. 6), which shows that there is a significant difference between the experimental group and the control group after the experiment. This difference is significant before and after the experiment. The experimental group had a significant reduction in waist circumference in children aged 0–6, but not in children aged 7–14 or overall.
By excluding each article one by one to check the sensitivity, we observe that the result of the effect size has no change. The consolidation result of the data from each article is robust. Among them, there are two subgroups of 0–6 years old and five subgroups of 7–14 years old. There were 803 experimental groups and 826 control groups. Results of the meta-analysis subgrouping indicate that the heterogeneity risk of systematic analysis of the subgroup literature is still high (p = 0.002, I2 = 89.1%).
The effect of the two sub-combinations is then analyzed. According to the total results, the difference between the experimental group and the control group is high, and the diamond on the forest map falls on the left side. The results show that participation in family sports has a significant effect on the waist circumference of obese children.
The effect of family sports intervention on the body fat rate of children
As can be seen from the forest map in Fig. 7, family sports participation has a significant impact on the weight of obese teenagers. A total of five articles were included. The age of the population belongs only to the 7–14-year-old children group; hence, no subgroup analysis of age was required. The experimental group included 300 children, and 275 participants were in the control group. Outcome indicators systemic analysis of body fat rate shows: χ2 = 0.54, df = 4, p = 0.97, I2 < 50%.
The homogeneity of the included literature is high, using a fixed-effects model analysis. Five articles on the impact on body weight show: SMD-FE = − 0.06, 95% CI (− 0.22 to 0.11), the total effect value Z = 0.69, p = 0.49. The statistical analysis shows no significance.
After excluding each article to check sensitivity, we find no change in the results of the effect size, indicating that there is no literature to be excluded, and the evaluation shows that the results of the literature data merger are relatively robust. The total effect of diamond was decreasing, but there was no statistical significance, indicating that there was no significant difference between the experimental group and the control group before and after the experiment. There was no significant effect on body fat percentage in obese children participating in family sports activities.
Discussion
This project reflects the first comprehensive meta-analysis of the impact of family sports intervention on childhood obesity using a quantitative synthetic statistical method. We reviewed 16 RCT studies where the focal intervention method (family sports participation) and other intervention measures (diet adjustment and behavioral habit intervention) were used to treat and prevent obesity in children. The experimental intervention periods lasted at least 3 months.
We specifically select four common measurement indicators for meta-analysis across both age-groups [33]. Our analysis shows that the combined results of interventions on body weight are statistically significant, but the combined results of interventions on BMI, waist circumference, and body fat rate are not statistically significant. In particular, four common measures were selected for meta-analysis across two age-groups. Our analysis showed that the comprehensive effect of intervention on body weight was statistically significant, while the comprehensive effect on BMI, waist circumference, and body fat percentage was not. Only the comprehensive effect of body weight was statistically significant on the left side of the experimental group, indicating that the intervention of the experimental group could effectively reduce body weight. Our meta-analysis of increasing children's physical activities shows a different intervention effect as that of Brown, which studied the family-based intervention measures and found that children's physical activity level is increased through family participation [34, 35]. Additionally, Pamungkas studied family-based treatment and prevention interventions on children's obesity: Systematic review and meta-analysis disclose that family management can increase the frequency of physical activity and reduce sedentary time [36]. The possible reasons for this result are great differences in the level of evidence found in the research results, and the high risk of heterogeneity may be caused by the specific intervention populations and measures. These intervention populations have ethnic differences, the family economic level is inconsistent, and the age span of children is large. Moreover, the physiological development speed of men and women is different, which may affect obesity levels across gender[37, 38]. Most studies do not limit the spread of growth, social factors, and family class to the outcome indicators. Additionally, the 16 papers included in this study use a variety of intervention methods. Six studies use family sports, behavioral habits, and dietary adjustment for joint intervention, and 10 studies use only family sports intervention and dietary adjustment for intervention. System overview shows that the intervention effects of family sports intervention, dietary intervention, and behavioral habits alone are not as efficient as those of the combinations [39].
The research on the treatment and prevention of childhood obesity by British health improvement institutions mainly focuses on five topics: (a) family sports activities and interventions encourage and promote health; (b) family planning, taking parents as the main change element; (c) family behavior correction procedures; (d) behavior correction subjects are children; and (e) exercise treatment scheme [40].
Places family at the center of the intervention, as they are required to provide continuous exercise therapy, thereby cultivating an exemplary teaching environment for children in shaping their behavior habits. Family members are encouraged to supervise and manage the implementation of children's sports plans [41,42,43].
This study also offers a review of the design and recommendations for home exercise prescriptions for treating childhood obesity, as follows. The main purpose of family exercise therapy is to reduce the total fat content and visceral fat content of children and parents, increase the lean body weight, accelerate the consumption of excess energy in the body, maintain the balance of energy in the body, improve the level of resting metabolism, improve the level of lipid metabolism, and reduce metabolic and cardiovascular complications. When designing family exercise interventions, exercise training should reflect children’s growth and development rules, as well as age and gender differences, in order to appropriately enhance their physical health. For example, aerobic training, anti-group training, or combined exercise training are mainly used in home sports studies, and both types of exercise can effectively reduce total fat [44]. However, resistance exercise is more effective in increasing lean body weight and reducing the proportion of body fat [45].
Neral suggests principles to govern the use of family exercise therapy: (a) The principle of safe exercise should try to avoid sports injuries; (b) the principle of training plan arrangement varies from person to person; (c) the principle of gradual and orderly training load arrangement; (d) develop the principle of good behavior habits, reduce sedentary behavior, and increase physical activity; and (d) promoting overall health is the first principle [46].
Likewise, the Korean pediatric obesity group offers four strategies for exercise therapy: (a) Physical activity time should not exceed one hour. Young children participate in unstructured sports activities and older children participate in recreational sports activities; (b) exercise for one hour every day in an organized and planned way under parental supervision; (c) clarify the goal of physical activity in multidisciplinary obesity treatment, and make exercise plans for negative energy balance; and (d) appropriate exercise therapy strategies can be selected according to children of different ages and obesity degree.
Table 5 shows that the five factors considered in the design of family exercise prescription for obese children are exercise mode, exercise frequency, progressive load, exercise intensity, and duration. Family sports is characterized by varied and convenient daily physical activities wherein family members are encouraged to participate with children to increase physical activities, and children are the targets for intervention. Generally, obese children's primary exercise is arranged to walk for 10 min every 3–5 days, gradually increasing to exercise frequency every day. Exercise duration should be 60–80 min, with medium and high intensity (55%–90% maximum heart rate) as the main factor [47]. The monitoring and evaluation of exercise tasks provide records of goal tables and create an exercise log (space, duration, and prescribed training means of behavioral goals).
We also offer a number of suggestions for how to prescribe specific exercise regimens for children based on our research. These include: (a) developing appropriate exercise load according to children's obesity and children's physical fitness (especially patients with back, knee, and heel pain) to avoid joint injury; (b) paying attention to the foundation of children's early sports in order to cultivate healthy habits, interest in sports, and the concept of lifelong sports; and (c) paying attention to the growth and development of different ages and changes in human body composition [48,49,50,51].
For the treatment of childhood obesity, the main means are to increase physical activity and limit calories [52]. Specifically, obese children should focus on increasing lean body weight and reducing the proportion of body fat [53]. These children should strictly follow the sequence of sports training (preparation activities–intensive training–relaxation and stretching) and use social resources (environment, venue, facilities, media learning, etc.) [54, 55]. Diet therapy can help limit the total calorie intake of patients. Behavioral therapy can help patients improve sedentary behavior and lack of dyskinesia, and cultivate healthy eating and behavior habits [56]. The foundational elements of these behavior change skills include self-monitoring, goal setting, self-efficacy, problem-solving, recurrence prevention, and stimulation control.
Conclusion
A meta-analysis of 16 studies showed that compared with the samples without family sports, the weight of obese children participating in family sports decreased, but there were no significant differences in other relevant physical indicators. However, the evidence is limited with high heterogeneity and bias in the literature, and no adverse events have been documented. Moreover, long-term regular interaction generates a healthy and close relationship between parents and children. In other words, family activities have a positive impact on children's growth, and intervention measures based on family sports can prevent children's obesity and act as an integral part of weight loss. Additionally, it is necessary to further study the efficiency of different forms of family sports intervention measures and avoid possible adverse events. In order to find more efficient treatment and prevention of childhood obesity, it is necessary to constantly practice and innovate the methods and means of family sports. Follow-up research should examine large-scale clinical trials with family sports as a single factor intervention, which is needed to provide stronger evidence of the intervention effect.
In the future, long-term sports training plans for children with obesity should be implemented. Relevant government departments and education departments should provide sports professional knowledge, behavioral intervention guidance, and continuous education support to instill knowledge of nutrition and empirically backed exercise regimens for children in different obesity treatment periods.
Availability of data and materials
The data that support the fundings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- BMI:
-
Body mass index
- RCTs:
-
Randomized controlled trials
- CNKI:
-
China National Knowledge Infrastructure
- SCI-E:
-
Science Citation Index—Expanded
- SSCI:
-
Social Sciences Citation Index
- A&HCI:
-
Arts and Humanities Citation Index
- CPCI-S:
-
Conference Proceedings Citation Index—Science
- CPCI-SSH:
-
Conference Proceedings Citation Index—Social Sciences and Humanities
- ESCI:
-
Emerging Sources Citation Index
- CCR-E:
-
Current Chemical Reactions—Expanded
- IC:
-
Index Chemicus
- WHO:
-
World Health Organization
- SMD:
-
STD mean difference
- CI:
-
Confidence interval
- Z :
-
Z-Score
- SMD-RE:
-
STD mean difference—random-effects models
- SMD-FE:
-
STD mean difference—fixed-effects models
- WMD:
-
Weighted mean differences
- etc.:
-
Et cetera
References
World Health Organization. Taking action on childhood obesity. https://apps.who.int/iris/bitstream/handle/10665/274792/WHO-NMH-PND-ECHO-18.1-eng.pdf?ua=1. World Health Organization; 2018.
The United Nations Convention on the Rights of Children. https://www.un.org/zh/documents/treaty/files/A-RES-44-25.shtml. Accessed 18 Nov 2002.
McGovern L, Johnson JN, Paulo R, et al. Treatment of pediatric obesity: a systematic review and meta-analysis of randomized trials. J Clin Endocrinol Metab. 2008;93(12):4600–5.
Vos M, Barlow SE. Update in childhood and adolescent obesity. Pediatric Clin. 2011;58(6):15–7. https://doi.org/10.1016/j.pcl.2011.09.016.
Krebs NF, Jacobson MS. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112(2):424–30.
Jensen MD, Ryan DH. New obesity guidelines: promise and potential. JAMA. 2014;311(1):23–4.
De Salis M. Child education: perspectives, opportunities and challenges. New York: Nova Science Publishers; 2020.
Pamungkas RA, Chamroonsawasdi K. Home-based interventions to treat and prevent childhood obesity: a systematic review and meta-analysis. Behav Sci. 2019;9(4):38. https://doi.org/10.3390/bs9040038.
World Health Organization. EU adopts action plan on childhood obesity 2014–2020. 2014. http://www.euro.who.int/en/health-topics/disease-prevention/physical-activity/news/news/2014/03/eu-adopts-action-plan-on-childhood-obesity-2014-2020. Accessed Feb 2017.
Noonan K, Reichman NE, Corman H, et al. School and community involvement of adolescents with chronic health conditions. J Adolesc Health. 2020;67:576–82.
Alkon A, Crowley AA, Neelon SEB, et al. Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children’s body mass index. BMC Public Health. 2014;14(1):215.
Rubin DA, Duran AT, Haqq AM, et al. Changes in cardiometabolic markers in children with Prader–Willi syndrome and nonsyndromic obesity following participation in a home-based physical activity intervention. Pediatr Obes. 2018;13(11):734–43.
Zhou ZX. A comparative study on the ways to cultivate and promote children’s physical activities in China and the United States. Beijing: Capital Institute of Physical Education; 2020.
Brown HE, Atkin AJ, Panter J, et al. Family-based interventions to increase physical activity in children: a systematic review, meta-analysis and realist synthesis. Obes Rev. 2016;17(4):345–60.
Rong XJ. Efficacy of comprehensive treatment of simple obesity in preschool children. Chin Coal Indus Med J. 2007;(02):126-7.
Zeng T, Liu P, Deng LQ, Huang T. Analysis of 35 cases of simple obese children after intervention of waist circumference and body mass index. J Qiqihar Med Coll. 2013;34(10):1434-5.
Luo JJ, Xu J, Shi JH. Effectiveness of community comprehensive intervention model for intervention of preschool obese young children. Shangh Prevent Med. 2017;29(10):780-3.
Wang Z. Effect of Comprehensive Therapy on Simple Obesity in Preschool Children. Stud Clin Med Eng. 2016;23(07):935-6.
Saelens B E, Grow H M, Stark L J, et al. Efficacy of increasing physical activity to reduce children's visceral fat: A pilot randomized controlled trial. Int J Pediatr Obes. 2011;6(2):102-12.
Rodearmel S J, Wyatt H R, Stroebele N, et al. Small changes in dietary sugar and physical activity as an approach to preventing excessive weight gain: the America on the Move family study. Pediatrics. 2007;120(4):e869-79.
Okely A D, Collins C E, Morgan P J, et al. Multi-site randomized controlled trial of a child-centered physical activity program, a parent-centered dietary-modification program, or both in overweight children: the HIKCUPS study. J Pediatr. 2010;157(3):388-94.
Ahmad N, Shariff Z M, Mukhtar F, et al. Family-based intervention using face-to-face sessions and social media to improve Malay primary school children’s adiposity: a randomized controlled field trial of the Malaysian REDUCE programme. Nutr J. 2018;17(1):74.
Alkon A, Crowley A A, Neelon S E B, et al. Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children’s body mass index. BMC Publ Health 2014;14(1):1-13.
Döring N, Ghaderi A, Bohman B, et al. Motivational interviewing to prevent childhood obesity: a cluster RCT. Pediatrics. 2016;137(5):220-226
Nyström C D, Sandin S, Henriksson P, et al. A 12-month follow-up of a mobile-based (healthy) obesity prevention intervention in pre-school children: the MINISTOP randomized controlled trial. BMC Publ Health. 2018;18(1):658.
Sacher P M, Kolotourou M, Chadwick P M, et al. Randomized controlled trial of the MEND program: a family‐based community intervention for childhood obesity. Obesity. 2010;18(S1):S62-S68.
Oliva A, Parra Á, Reina M C. Personal and contextual factors related to internalizing problems during adolescence[C]//Child Youth Care Forum. Springer US. 2014;43(4):505–20.
Chen J L. Household income, maternal acculturation, maternal education level and health behaviors of Chinese-American children and mothers. J Immigrant Minor Health. 2009;11(3):198-204.
Christison A L, Evans T A, Bleess B B, et al. Exergaming for health: a randomized study of community-based exergaming curriculum in pediatric weight management. Games Health J. 2015;5(6):413-21.
Epstein L H, Paluch R A, Gordy C, et al. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediat Adolesc Med. 2000;154(3):220-6
Zeng T, Liu P, Deng LQ, Huang T. Analysis of 35 cases of simple obese children after intervention of waist circumference and body mass index. J Qiqihar Med Coll. 2013;34(10):1434–5.
Xu JZ, Xu YZ. Study on comprehensive intervention of obesity in preschool children. China Rural Med. 2012;19(10):28–9.
Monasta L, Batty G D, Macaluso A, et al. Interventions for the prevention of overweight and obesity in preschool children: a systematic review of randomized controlled trials. Obes Rev, 2011;12(5):107-18.
Yu SM. Biological analysis of obesity and weight loss by aerobic exercise (review). J Beijing Sport Univ. 2001;34(1):62–3.
Markert J, Herget S, Petroff D, et al. Telephone-based adiposity prevention for families with overweight children (TAFF-Study): one year outcome of a randomized, controlled trial. Int J Environ Res Public Health. 2014;11(10):10327–44.
Cordellat A, Padilla B, Grattarola P, et al. Multicomponent exercise training combined with nutritional counselling improves physical function, biochemical and anthropometric profiles in obese children: a pilot study. Nutrients. 2020;12(9):2723.
García-Hermoso A, Ramírez-Vélez R, Ramírez-Campillo R, et al. Concurrent aerobic plus resistance exercise versus aerobic exercise alone to improve health outcomes in paediatric obesity: a systematic review and meta-analysis. Br J Sports Med. 2018;52(3):161–6.
Cohen TR, Hazell TJ, Vanstone CA, et al. A family-centered lifestyle intervention for obese six-to eight-year-old children: results from a one-year randomized controlled trial conducted in Montreal, Canada. Can J Public Health. 2016;107(4–5):e453–60.
Saelens BE, Grow HM, Stark LJ, et al. Efficacy of increasing physical activity to reduce children’s visceral fat: a pilot randomized controlled trial. Int J Pediatr Obes. 2011;6(2):102–12.
Viana RB, Naves JPA, Coswig VS, et al. Is interval training the magic bullet for fat loss? A systematic review and meta-analysis comparing moderate-intensity continuous training with high-intensity interval training (HIIT). Br J Sports Med. 2019;53(10):655–64.
Muollo V, Rossi AP, Milanese C, et al. The effects of exercise and diet program in overweight people–Nordic walking versus walking. Clin Interv Aging. 2019;14:1555.
Brand C, Martins CMDL, Lemes VB, et al. Effects and prevalence of responders after a multicomponent intervention on cardiometabolic risk factors in children and adolescents with overweight/obesity: action for health study. J Sports Sci. 2020;38(6):682–91.
Beckerman-Hsu JP, Aftosmes-Tobio A, Gavarkovs A, et al. Communities for healthy living (CHL) a community-based intervention to prevent obesity in low-income preschool children: process evaluation protocol. Trials. 2020;21(1):1–13.
Bonney E, Ferguson G, Burgess T, et al. Benefits of activity-based interventions among female adolescents who are overweight and obese. Pediatr Phys Ther. 2019;31(4):338–45.
Brasil I, Monteiro W, Lima T, et al. Effects of judo training upon body composition, autonomic function, and cardiorespiratory fitness in overweight or obese children aged 8-to 13 years. J Sports Sci. 2020;38:1–9.
Altay N, Toruner EK, Akgun-Citak E. Determine the BMI levels, self-concept and healthy life behaviours of children during a school based obesity training programme. AIMS Public Health. 2020;7(3):535.
Chen P, Wang D, Shen H, et al. Physical activity and health in Chinese children and adolescents: expert consensus statement 2020. Br J Sports Med. 2020;54:1321–31.
Adom T, De Villiers A, Puoane T, et al. School-based interventions targeting nutrition and physical activity, and body weight status of African children: a systematic review. Nutrients. 2020;12(1):95.
Yetgin MK, Agopyan A, Küçükler FK, et al. The effects of resistance and aerobic exercises on adiponectin, insulin resistance, lipid profile and body composition in adolescent boys with obesity. Istanb Med J. 2020.
Domaradzki J, Cichy I, Rokita A, et al. Effects of Tabata training during physical education classes on body composition, aerobic capacity, and anaerobic performance of under-, normal-and overweight adolescents. Int J Environ Res Public Health. 2020;17(3):876.
Diao H, Wang H, Yang L, et al. The impacts of multiple obesity-related interventions on quality of life in children and adolescents: a randomized controlled trial. Health Qual Life Outcomes. 2020;18(1):1–9.
Da Silva MR, Waclawovsky G, Perin L, et al. Effects of high-intensity interval training on endothelial function, lipid profile, body composition and physical fitness in normal-weight and overweight-obese adolescents: a clinical trial. Physiol Behav. 2020;213:112728.
Crowe M, Sampasa-Kanyinga H, Saunders TJ, et al. Combinations of physical activity and screen time recommendations and their association with overweight/obesity in adolescents. Can J Public Health. 2020;111(4):515–22.
Yu H, Li F, Hu Y, et al. Improving the metabolic and mental health of children with obesity: a school-based nutrition education and physical activity intervention in Wuhan, China. Nutrients. 2020;12(1):194.
Lobstein T, Swinburn B. Health promotion to prevent obesity//Global perspectives on health promotion effectiveness. New York, NY: Springer; 2007. p. 125–50.
Martínez-Andrade GO, Cespedes EM, Rifas-Shiman SL, et al. Feasibility and impact of Creciendo Sanos, a clinic-based pilot intervention to prevent obesity among preschool children in Mexico City. BMC Pediatr. 2014;14(1):77.
Acknowledgements
Support from the Middle-aged Students in Hubei Province Excellent Innovation Research Team (T201925) is also gratefully acknowledged.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
LY and CL equally contributed as first authors. TL, LC, YL, and XM conceived and designed the project. YL conceptualized the research idea, performed the statistical analysis, and wrote the first draft. LC, YN, and XQ collected the data. YL, LC, and YN performed the analyses. YL, LC, and WY drafted the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, L., Liang, C., Yu, Y. et al. Family sports interventions for the treatment of obesity in childhood: a meta-analysis. J Health Popul Nutr 41, 40 (2022). https://doi.org/10.1186/s41043-022-00317-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-022-00317-7