Abstract
Background
Venous–arterial carbon dioxide (CO2) to arterial–venous oxygen (O2) content difference ratio (Cv-aCO2/Ca-vO2) > 1 is supposed to be both sensitive and specific for anaerobic metabolism. What regional hemodynamic and metabolic parameters determine the ratio has not been clarified.
Objectives
To address determinants of systemic and renal, spleen, gut and liver Cv-aCO2/Ca-vO2.
Methods
Post hoc analysis of original data from published experimental studies aimed to address effects of different fluid resuscitation strategies on oxygen transport, lactate metabolism and organ dysfunction in fecal peritonitis and endotoxin infusion, and from animals in cardiac tamponade or hypoxic hypoxia. Systemic and regional hemodynamics, blood flow, lactate uptake, carbon dioxide and oxygen-derived variables were determined. Generalized estimating equations (GEE) were fit to assess contributors to systemic and regional Cv-aCO2/Ca-vO2.
Results
Median (range) of pooled systemic Cv-aCO2/Ca-vO2 in 64 pigs was 1.02 (0.02 to 3.84). While parameters reflecting regional lactate exchange were variably associated with the respective regional Cv-aCO2/Ca-vO2 ratios, only regional ratios were independently correlated with systemic ratio: renal Cv-aCO2 /Ca-vO2 (β = 0.148, 95% CI 0.062 to 0.234; p = 0.001), spleen Cv-aCO2/Ca-vO2 (β = 0.065, 95% CI 0.002 to 0.127; p = 0.042), gut Cv-aCO2/Ca-vO2 (β = 0.117, 95% CI 0.025 to 0.209; p = 0.013), liver Cv-aCO2/Ca-vO2 (β = − 0.159, 95% CI − 0.297 to − 0.022; p = 0.023), hepatosplanchnic Cv-aCO2/Ca-vO2 (β = 0.495, 95% CI 0.205 to 0.786; p = 0.001).
Conclusion
In a mixed set of animals in different shock forms or during hypoxic injury, hepatosplanchnic Cv-aCO2/Ca-vO2 ratio had the strongest independent association with systemic Cv-aCO2/Ca-vO2, while no independent association was demonstrated for lactate or hemodynamic variables.
Similar content being viewed by others
Background
Circulatory shock can be defined as a condition where tissue oxygen delivery does not meet the metabolic needs [1]. Inadequate oxygen delivery may also occur with normal perfusion when arterial oxygen content is critically reduced, e.g., in severe respiratory failure or at high altitude. In septic shock, both global perfusion and arterial oxygen content can be normal, but the metabolic needs may still be insufficiently met as a result of oxygen extraction and/or utilization abnormalities [2]. In all of these conditions, regional blood flow may be redistributed as a consequence of central (e.g., sympathetic nervous system) and/or peripheral (e.g., nitric oxide, shear stress) adaptive mechanisms [3].
In clinical practice, lactate is commonly used as an indicator of adequacy of tissue perfusion [4]. The recently released sepsis-3 definition includes increased blood lactate concentration as a criterion for the diagnosis of septic shock [1]. However, lactate concentration can also increase as a result of impaired ability of the liver to extract lactate [5] or as a consequence of increased aerobic lactate production, e.g., when epinephrine is used to stabilize hemodynamics [6].
When tissue oxygen delivery falls under a critical threshold, oxygen consumption and CO2 production from aerobic metabolism decrease [7]. Since some CO2 is produced from anaerobic metabolism, CO2 production falls less than O2 consumption and therefore, their ratio increases [7]. The combination of venous–arterial CO2 to arterial–venous O2 content difference ratio (Cv-aCO2/Ca-vO2) with arterial lactate levels has been reported to correlate with Sequential Organ Failure Assessment (SOFA) score and mortality [8].
Venous–arterial CO2 partial pressure to arterial–venous O2 content difference ratio (Pv-aCO2/Ca-vO2) is a relatively easily obtainable surrogate of the Cv-aCO2/Ca-vO2: pO2 and PCO2, oxygen saturation (SO2) and hemoglobin (Hb) are widely available in all modern blood gas analyzers, while CO2 content is not easy to measure or calculate. Pv-aCO2/Ca-vO2 has been used to predict systemic hyperlactatemia in critically ill patients [9]. However, it has been shown that decreased blood flow, rather than tissue hypoxia/dysoxia is the main determinant of increased venous–arterial CO2 gradient (Pv-aCO2) [10]. Furthermore, Pv-aCO2 may vary with different values of oxygen saturation due to Haldane effect, and due to changes in dissociation curves if pH, hemoglobin or temperature is changing. Accordingly, Pv-aCO2 may vary at constant total CO2 content [11].
What circulatory or metabolic parameters are best associated with systemic (Cv-aCO2/Ca-vO2) remains unclear. The aim of the present study was to address potential determinants of systemic and regional (renal, spleen, gut and liver) Cv-aCO2/Ca-vO2 in a mixed set of animals in different shock forms or during hypoxic injury. We hypothesized that parameters of hepatosplanchnic perfusion and metabolism are best predicting changes in systemic Cv-aCO2/Ca-vO2.
Methods
We used original data from previously published studies [5, 12, 13]. They were performed in accordance with the National Institutes of Health guidelines for the care and use of experimental animals and with the approval of the Animal Care Committee of the Canton of Bern, Switzerland.
The first study (COHORT-1) was designed to address the impact of two different fluid resuscitation strategies (moderate-volume and high-volume replacement) on mortality, sepsis-associated organ dysfunction and mitochondrial function in animals submitted to either fecal peritonitis or endotoxin infusion [12].
The second study (COHORT-2) was performed to evaluate oxygen transport, lactate handling and mitochondrial function in animals challenged with fecal peritonitis, cardiac tamponade or hypoxic hypoxia [5, 13].
In both studies, animals were followed until 24 h after randomization or until death, if earlier. After 24 h, animals were euthanized with an overdose of potassium chloride [5, 12, 13]. The full study protocols of original studies can be found elsewhere [5, 12, 13].
Surgical preparation
With animals in supine position, a midline laparotomy was performed and abdominal cavity exposed [5, 12, 13]. Catheters for pressure monitoring and blood sampling were inserted into the carotid, hepatic and pulmonary arteries and into jugular, hepatic, portal, renal, mesenteric and splenic veins [5, 12, 13]. A large bore catheter for fluid administration was inserted into the femoral vein. Ultrasound Doppler flow probes (Transonic® Systems Inc., Ithaca, NY, USA) were placed around the carotid, superior mesenteric, hepatic, splenic and renal arteries, celiac trunk and around the portal vein [5, 12, 13]. A drainage catheter was inserted into the urinary bladder. Finally, two large bore drains were inserted via both flanks of the animals. The surgical procedure was followed by a 12-h period of hemodynamic stabilization [5, 12, 13].
Experimental protocol COHORT-1
After a 12-h period of hemodynamic stabilization, animals were randomized into six groups (n = 8 each, total 48 pigs) as follows: fecal peritonitis, endotoxin, or controls, each with either moderate-volume fluid resuscitation (10 ml/kg/h of Ringer's lactate) or high [15 ml/kg/h Ringer's lactate + 5 ml/kg/h hydroxyethyl starch (HES) 130/04, 6% (Voluven®, Fresenius, Stans, Switzerland)] for 24 h or until death, if earlier [12].
Fecal peritonitis was induced by peritoneal instillation through a peritoneal drainage tube of 1 g per kg body weight of autologous feces dissolved in 200 ml glucose 5% solution [12]. In the other groups, the same amount of sterile glucose solution was instilled. The intra-peritoneal drains were maintained clamped during the following 6 h [12]. In the endotoxin groups, endotoxin (lipopolysaccharide from Escherichia coli 0111:B4, 20 mg/l in 5% dextrose; Sigma®, Steinheim, Germany) was infused into the right atrium [12].
Experimental protocol COHORT-2
After 12-h period of hemodynamic stabilization, animals were randomized for a 24-h experiments into four groups (n = 8 each; total 32 pigs) as follow: fecal peritonitis, cardiac tamponade, hypoxic hypoxia, and controls [5, 13]. Following the 3R principles, COHORT-1 and 2 studies shared the control (n = 8) and fecal peritonitis groups (n = 8).
Fecal peritonitis was induced by instilling 1 g per kg body weight of autologous feces, dissolved in warmed glucose solution, in the abdominal cavity. In the other groups, the same amount of sterile glucose solution was instilled. The intra-peritoneal drains were clamped during the first 6 h [5, 13]. Cardiac tamponade was induced by filling the pericardial sac with HES 130/04, 6% (Voluven®, Fresenius Kabi, Bad Homburg, Germany) through the catheter positioned during the operation, aiming at a cardiac output of 60 ml/kg/min at 6 h, 50 ml/kg/min at 12 h, 40 ml/kg/min at 18 h, and 30 ml/kg/min at 24 h, respectively [13]. Hypoxic hypoxia was induced by reducing the fraction of inspired oxygen (FiO2) to 21% at 6 h, 18% at 12 h, 17% at 18 h, and 16% at 24 h [13]. When FiO2 was reduced below 21%, nitrogen was added to the gas mix. All pigs received Ringer’s lactate solution (10 ml/kg/h) during the experiment [13].
Blood measurements
Blood samples for the measurement of hemoglobin (OSM3, Pig module, Radiometer, Copenhagen, Denmark), blood gases (ABL 520, Radiometer, Copenhagen, Denmark), and lactate (YSI 2300 Stat Plus, Yellow Springs Instruments, CA, USA) were taken at baseline and after 3, 6, 12, 18 and 24 h from pulmonary and carotid arteries, and from hepatic, portal, renal, mesenteric and splenic veins [5, 12, 13]. Blood sampling was also performed before 24 h if the animals exhibited a persistent decrease in mean arterial pressure (MAP) below 50 mmHg; these samples were considered as end values [5, 12, 13].
Calculations
Systemic oxygen delivery (DO2) and consumption (VO2) and CO2 variables were calculated according the standard formulas as follows [5, 12, 13]:
-
DO2 = CaO2 × CO
-
VO2 = (CaO2 − CvO2) × CO
-
O2ER = (CaO2 − CvO2)/CaO2
-
CaO2 = (Hb × SaO2 × 1.34) × (PaO2 × 0.0031)
-
CvO2 = (Hb x SvO2 × 1.34) × (PvO2 × 0.0031)
-
Da-vO2 = CaO2 − CvO2
-
Pv-aCO2 = PvCO2 − PaCO2,
where CO represents cardiac output expressed in ml/kg/min, Hb represents hemoglobin expressed in g/dl, O2ER represents the oxygen extraction ratio, CaO2 and CvO2 represent the arterial and venous O2 content expressed in ml/dl and PaCO2 and PvCO2 represent, respectively, arterial and venous CO2 partial pressures expressed in mmHg. CO2 contents were calculated according to the Douglas formula [11]:
-
Plasma CO2 solubility (S) = 0.0307 + [0.00057 × (37 – T)] + [0.00002 × (37 − T)2], were temperature (T) is expressed as °C.
-
pK’ = 6.086 + [0.042 × (7.4 − pH)] + [(38 − T) × {0.00472 + [0.00139 × (7.4 − pH)]}], were (pK’) is the apparent dissociation constant of carbonic acid, and (pH) is the potential of hydrogen (acidity).
-
Plasma CO2 content (plasma CCO2, ml/dl) = 2.226 × S × plasma PCO2 × [1 + (10pH–pK’)], where (S) is the solubility coefficient for CO2.
-
Blood CO2 content (Blood CCO2, ml/dl) = Plasma CCO2 × 1 − {(0.0289 × Hb) ÷ [3.352 − (0.456 × SO2)] × (8.142 − pH)]}, where SO2 is the oxygen saturation in the blood.
Time course of blood lactate levels (lactate disappearance) was defined as change in blood lactate levels (%) during a 6-h period [14]. Blood lactate exchange were calculated as follows [5, 14]:
-
Hepatic lactate uptake (µmol/kg/min) = hepatic lactate influx − hepatic lactate efflux.
-
Hepatic lactate influx (µmol/kg/min) = (portal venous lactate × portal vein blood flow) + (arterial lactate × hepatic arterial blood flow).
-
Hepatic lactate efflux (µmol/kg/min) = hepatic venous lactate × (portal venous blood flow + hepatic arterial blood flow).
-
Other regional lactate exchanges (renal, gut and spleen): regional lactate influx–regional lactate efflux.
-
Whole body venous efflux (µmol/kg/min): cardiac output × mixed venous lactate concentration.
Statistical analysis
All data are presented as n/n total (%) or median values with range. Normality was tested by the Kolmogorov–Smirnov test. Relationship between arterial lactate and base excess was assessed in the whole cohort with simple linear regression and Pearson correlation coefficient. Cv-aCO2/Ca-vO2 were compared between the different regions with Kruskal–Wallis test followed by pairwise comparisons with Mann–Whitney U test.
To account for longitudinal and correlated response variables, regression analysis based on generalized estimating equations (GEE) were fit to assess contributors to regional (renal, spleen, gut and liver) and systemic Cv-aCO2/Ca-vO2. Contributors to regional (renal, spleen, gut and liver) Cv-aCO2/Ca-vO2 included into the models were perfusion pressure [mean arterial blood pressure (MAP) minus central venous pressure (CVP)], venous hemoglobin, pH, pCO2, pO2, base excess and lactate, regional blood flow, regional DO2, VO2, and O2ER, regional lactate uptake and lactate gradient (regional venous lactate–arterial lactate). All regional (renal, spleen, gut and liver) predictors showing a p < 0.05 were entered into a final model aiming to address contributors to systemic Cv-aCO2/Ca-vO2. Unstandardized coefficients (β) along with their 95% confidence interval (95% CI) were reported.
To perform a sensitivity analyses, the model was re-assessed including only observations in which systemic Cv-aCO2/Ca-vO2 was higher than 1.0, which indicates anaerobic metabolism [7]. To address potential group effects, the experimental group (control group, fecal peritonitis, endotoxin infusion, cardiac tamponade and hypoxic hypoxia) was introduced as a predictor into the final models.
The SPSS™ (IBM™ Statistical Package for the Social Science version 26.0) were used for statistical analyses and GraphPad Prism version 7.0 (GraphPad Software, California, USA) was used for graph plotting.
Results
Sixty-four domestic pigs (48 from cohort-1, and 16 from cohort-2) of both sexes [weight: 41.5 (35.0–48.9) kg, median (range)] were included in this study. Overall mortality was 40.6% (26/64 animals), with a median survival time of 24 (7–24) h. Mortality accordingly to experimental study groups is presented in Additional file 1: Table S1.
Systemic hemodynamics, oxygen transport and lactate kinetics
Systemic hemodynamics, oxygen transport, acid–base balance and lactate kinetics from each study group have been previously reported [5, 12, 13]. The median of achieved values at different time points for the whole studied cohort are displayed in Table 1.
Briefly, animals submitted to fecal peritonitis became hypotensive while cardiac output, systemic DO2 and arterial lactate levels increased. Endotoxin infusion resulted increased cardiac output and mean pulmonary artery pressure (MPAP) while systemic VO2 and O2ER remained stable. Cardiac tamponade animals exhibited systemic arterial hypotension and decreased DO2 while systemic O2ER and arterial lactate levels increased. Hypoxic hypoxia resulted in increased cardiac output while systemic DO2 and O2ER remained unchanged [5, 12, 13].
Systemic carbon dioxide and oxygen variables
Acid–base balance from each study group have been previously reported [5, 12, 13]. Base excess inversely correlated with arterial lactate levels (r = − 0.65, p < 0.001; Additional file 1: Figure S1). The median of achieved values at different time points for the whole studied cohort are displayed in Table 2.
Median of pooled systemic Cv-aCO2/Ca-vO2 was 1.02 (0.02 to 3.84). During the experimental period, median Cv-aCO2 and Ca-vO2 decreased while their ratio remained unchanged (Table 2).
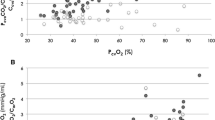
Systemic Cv-aCO2/Ca-vO2 was neither correlated with arterial lactate (β = 0.22, 95% CI − 0.16 to 0.61; p = 0.249), lactate disappearance (β = − 5.65, 95% CI − 38.0 to 26.7; p = 0.732) nor with whole-body venous lactate efflux (β = 5.31, 95% CI − 15.6 to 26.2; p = 0.619) (Fig. 1).
Scatter plot between systemic venous–arterial CO2 to arterial–venous O2 content difference ratio (Cv-aCO2/Ca-vO2) and arterial lactate, lactate disappearance and whole-body venous lactate efflux. β = unstandardized coefficient, CI = confidence interval, Cv-aCO2/Ca-vO2 = venous–arterial CO2 to arterial–venous O2 content difference ratio, whole-body venous efflux = cardiac output × mixed venous lactate concentration, lactate disappearance (%) = initial lactate − final lactate/initial lactate × 100
Regional blood flow, lactate uptake and Cv-aCO2/Ca-vO2
Median total hepatic blood flow, total hepatosplanchnic blood flow, superior mesenteric artery blood flow and spleen artery blood flow increased during the experimental period, with maximal values observed at the end of study. Renal artery blood flow remained stable during experimental period (Table 3). Hepatic lactate uptake and hepatosplanchnic lactate uptake increased during the study period and were markedly positive (lactate extraction). Renal, mesenteric and splenic lactate uptake, which were all slightly negative (lactate release), remained stable (Table 3).
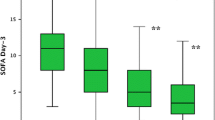
Median (range) of pooled hepatic, hepatosplanchnic, renal, mesenteric and spleen Cv-aCO2/Ca-vO2 were, respectively, 0.82 (0.0–6.9), 1.0 (0.2–3.4), 1.1 (0.1–4.7), 1.2 (0.1–5.0) and 1.2 (0.0–6.0) (Additional file 1: Fig. S2). Values for the whole cohort at different time points are displayed in Table 3, and separate values for the individual experimental groups in Additional file 1: Fig. S3.
Contributors to regional (renal, spleen, gut and liver) Cv-aCO2/Ca-vO2 for the whole cohort are presented in Additional file 1: Tables S2–S5). Contributors to regional (renal, spleen, gut and liver) Cv-aCO2 /Ca-vO2 for time points which systemic Cv-aCO2/Ca-vO2 > 1.0 only are presented in Additional file 1: Tables S6–S9.
Contributors to systemic Cv-aCO2/Ca-vO2
Renal Cv-aCO2/Ca-vO2 (β = 0.148, 95% CI 0.062 to 0.234; p = 0.001), spleen Cv-aCO2/Ca-vO2 (β = 0.065, 95% CI 0.002 to 0.127; p = 0.042), gut Cv-aCO2/Ca-vO2 (β = 0.117, 95% CI 0.025 to 0.209; p = 0.013), liver Cv-aCO2/Ca-vO2 (β = − 0.159, 95% CI − 0.297 to − 0.022; p = 0.023) and hepatosplanchnic Cv-aCO2/Ca-vO2 (β = 0.495, 95% CI 0.205 to 0.786; p = 0.001)— but none of the other parameters—were independently correlated with systemic Cv-aCO2/Ca-vO2 (Table 4).
Additional analysis
When only systemic Cv-aCO2/Ca-vO2 > 1.0 were included in the analysis, only renal Cv-aCO2/Ca-vO2 (β = 0.099, 95% CI 0.039 to 0.159; p = 0.001), Gut Cv-aCO2/Ca-vO2 (β = 0.120, 95% CI 0.015 to 0.225; p = 0.025), liver Cv-aCO2/Ca-vO2 (β = − 0.323, 95% CI − 0.508 to − 0.138; p = 0.001) and hepatosplanchnic Cv-aCO2/Ca-vO2 (β = 0.641, 95% CI 0.274 to 1.008; p = 0.001) remained independently correlated with systemic Cv-aCO2/Ca-vO2 (Additional file 1: Table S10).
The inclusion of experimental group (fecal peritonitis, endotoxin infusion, cardiac tamponade and hypoxic hypoxia) as a predictor into the final models assessing contributors to Cv-aCO2/Ca-vO2 did not affect the results (Additional file 1: Tables S11 and S12).
Discussion
We found that variables indicating regional lactate transport and oxygen extraction ratios correlated with regional but not systemic Cv-aCO2/Ca-vO2 ratios. The best predictor of systemic Cv-aCO2/Ca-vO2 ratio was the hepatosplanchnic Cv-aCO2/Ca-vO2 ratio (β = 0.495), while the other regional ratios correlated also, albeit to a weaker extent. If only systemic Cv-aCO2/Ca-vO2 > 1 were included in the analysis, also renal and spleen lactate gradients correlated with systemic Cv-aCO2/Ca-vO2 ratios.
In patients with acute lung injury, septic or cardiogenic shock, a Pv-aCO2/Ca-vO2 > 1.4 predicted hyperlactatemia [9]. In contrast to this study, we aimed to predict Cv-aCO2/Ca-vO2 ratios from regional blood flows, and lactate and other metabolism related variables. Our findings may be explained by a high regional heterogeneity in terms of tolerance to anemic and hypoxic insults [15], and differences in the availability of adaptive mechanisms among various organs/systems [16]. Therefore, markers indicating tissue dysoxia in one organ may be diluted by those of other organs with more resources to adapt.
In our fluid-resuscitated experimental models, arterial lactate levels increased only moderately, and not in all animals. Despite this, we found overall associations between lactate-related parameters and Cv-aCO2/Ca-vO2 in all regions. Since the regional Cv-aCO2/Ca-vO2 determined systemic Cv-aCO2/Ca-vO2 to some extent, we suggest that increasing systemic Cv-aCO2/Ca-vO2 is useful to detect subtle regional metabolic alterations, even if values are smaller than 1.
Lactate and lactic acidosis are not exclusively related to anaerobic metabolism [17]. Interpretation of lactate in shock and hypoxia has evolved from being a marker of anaerobic metabolism, to represent part of an adaptive mechanism to provide an alternative substrate to vital organs such as kidney, brain and heart (lactate shuttle theory) [18]. Experimental data support the concept that respiratory quotient, expressed as the ratio between CO2 production (VCO2), and oxygen consumption (VO2) is a reliable marker of anaerobic threshold [19]. Our study found that neither arterial lactate, nor lactate disappearance, nor whole-body venous lactate efflux are associated with RQ (measured as Cv-aCO2/Ca-vO2), potentially suggesting that lactate may be, at least in part, associated to aerobic metabolism in the hypoxia and shock models assessed in this study. The slower lactate kinetics of lactate compared to blood gas variables may provide another explanation in some cases, as discussed by others [8]. However, our data demonstrate that lactate concentrations > 2 mmol/l were almost always associated with negative base excess values. Finally, Cv-aCO2 may not increase in states of tissue hypoxia when venous blood flow is high enough to wash out CO2 produced by the hypoxic cells [20].
The hepatosplanchnic region was the most important contributor to systemic Cv-aCO2/Ca-vO2. It could be argued that this is a consequence of the greater amount of tissue perfused in this compared to the other regions. On the other hand, we have demonstrated in humans that changes in hepatosplanchnic metabolism and blood flow dissociate from those of systemic blood flow and metabolism [21, 22]. Furthermore, one has to acknowledge that blood flow is not a component of Cv-aCO2/Ca-vO2 values—the main drivers are pCO2, Hb and SO2. Therefore, higher rates of CO2 production related to O2 consumption in the hepatosplanchnic compared to other regions could have accounted for the high contribution of hepatosplanchnic to systemic Cv-aCO2/Ca-vO2. However, we found that Cv-aCO2/Ca-vO2 ratios were lowest in the hepatosplanchnic region. Nevertheless, in low flow and/or high metabolic circumstances, portal venous oxygen content and therefore hepatic oxygen delivery will decrease over-proportionally, also because portal flow represents around 2/3 of total liver perfusion—this renders the region, especially the liver, at risk for inadequate oxygen supply [23].
In terms of determinants of systemic Cv-aCO2/Ca-vO2, regional veno-arterial lactate gradients were only significantly associated when Cv-aCO2/Ca-vO2 was > 1 and specifically in kidney and spleen. Kidney is an important organ for lactate disposal, accounting for about 30% of its systemic turnover. In the kidney, lactate is used for gluconeogenesis and as a substrate for ATP production, similarly to brain and heart [18, 24]. On the other hand, spleen lactate metabolism is very poorly described. A recent paper about inter-organ metabolite exchange metabolomics mapped that spleen is one of the organs which the highest production of lactate in the body at rest [25]. In our study, spleen together with mesenteric region was also the organ with the highest Cv-aCO2/Ca-vO2 gradients, suggesting that this organ operated at a level closer to anaerobic condition than other organs.
Limitations of the present study include the retrospective nature (post hoc analysis of previous studies), and a pooling of several models. It seems obvious that evaluation of the parameters in each group separately would have resulted in more overt changes over time. The drawback of this approach is the relatively small n per group. The advantage of a pooled group is the large range of variables and a better simulation of a mixed ICU patient population. Conceptually, one would expect that higher lactate concentrations go together with higher Cv-aCO2/Ca-vO2 values, independently of group or time point, if both reflect tissue hypoxia. Furthermore, we did not find an effect of the model on the association between the various parameters with regional or systemic Cv-aCO2/Ca-vO2 ratios. Given the design of the original studies and the fixed time points of blood sampling, we could neither determine how fluid resuscitation in the sepsis models affected regional and systemic Cv-aCO2/Ca-vO2 ratios, nor the association of Cv-aCO2/Ca-vO2 ratios with signs of systemic inflammation and tissue injury. Therefore, we cannot provide mechanistic explanations for our findings—this should be done in further, prospective studies. Lastly, it can be argued, that hepatosplanchnic and splenic/mesenteric values are mathematically and physiologically coupled, as they share the arterial variables, and because the latter contribute to the former. By using a strict pre-analysis protocol to obtain blood and measure the parameters included in Cv-aCO2/Ca-vO2 values, and by measuring hemoglobin and oxygen saturation with a module specific for pig blood, we believe that measurement errors largely have been avoided. We acknowledge that, e.g., mesenteric Cv-aCO2/Ca-vO2 values contribute to hepatosplanchnic values—as all regional values contribute to systemic values. In the present study, we were interested in Cv-aCO2/Ca-vO2 values of both single organs (spleen, gut, kidney) and the whole hepatosplanchnic region—especially also because blood sampling from the liver vein is clinically feasible, whereas samples from portal and splenic veins can be obtained only intra-operatively. Conversely, strengths are the provision of data where data have been lacking so far, and the ethical commitment with the 3R principle (Replacement, Reduction and Refinement) on animal research.
The overall aim of this analysis was to improve our understanding about contributors to systemic Cv-aCO2/Ca-vO2 values, since the latter may offer a more specific indicator of anaerobic metabolism than lactate. While we found that only regional Cv-aCO2/Ca-vO2 contributed to the respective systemic values, contributors to regional Cv-aCO2/Ca-vO2 values differed in the regions (e.g., regional lactate gradient in the kidney, venous independent of arterial lactate in the gut; MAP-CVP in the hepatosplanchnic region but not in the kidney)—especially when regional Cv-aCO2/Ca-vO2 values were > 1. These data are preliminary and have not been prospectively studied. However, we believe they are important for hypothesis generation about how different regions can metabolically adapt to insults—and about potentially modifiable factors.
Conclusion
In a mixed set of animals in different shock states or with hypoxic injury, regional variables representing local lactate transport and oxygen extraction ratios correlated with the respective regional Cv-aCO2/Ca-vO2 ratios. However, only regional Cv-aCO2/Ca-vO2 ratios were independently associated with systemic Cv-aCO2/Ca-vO2.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- β :
-
Unstandardized coefficient
- BL:
-
Baseline
- CI:
-
Confidence interval
- CO:
-
Cardiac output
- CaCO2 :
-
Arterial CO2 content
- CvCO2 :
-
Venous CO2 content
- Cv-aCO2 :
-
Venous–arterial CO2 content difference
- CaO2 :
-
Arterial O2 content
- CvO2 :
-
Venous O2 content
- Ca-vO2 :
-
Arterial–venous O2 content difference
- Cv-aCO2/Ca-vO2 :
-
Venous–arterial CO2 to arterial–venous O2 content difference ratio
- CVP:
-
Central venous pressure
- DO2 :
-
Systemic oxygen delivery
- End:
-
End of the experiment (at 24 h of resuscitation or before death if earlier)
- MAP:
-
Mean arterial blood pressure
- MPAP:
-
Mean pulmonary artery pressure
- O2ER:
-
Systemic oxygen extraction
- PaO2 :
-
Arterial oxygen partial pressure
- PaCO2 :
-
Arterial carbon dioxide partial pressure
- Pv-aCO2 :
-
Venous-to-arterial carbon dioxide difference
- Pv-aCO2/Ca-vO2 :
-
Ratio between venous-to-arterial carbon dioxide difference and arterial–venous oxygen content difference
- RQ:
-
Respiratory quotient
- SpO2 :
-
Peripheral oxygen saturation
- SVRI:
-
Systemic vascular resistance index
- SvO2 :
-
Mixed venous oxygen saturation
- VO2 :
-
Systemic oxygen consumption
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 315:801–810
Correa TD, Vuda M, Blaser AR, Takala J, Djafarzadeh S, Dunser MW, Silva E, Lensch M, Wilkens L, Jakob SM (2012) Effect of treatment delay on disease severity and need for resuscitation in porcine fecal peritonitis. Crit Care Med 40:2841–2849
Brander L, Jakob SM, Knuesel R, Savolainen H, Widmer MK, Schmidli J, Takala J (2006) Effects of low abdominal blood flow and dobutamine on blood flow distribution and on the hepatic arterial buffer response in anaesthetized pigs. Shock 25:402–413
Kraut JA, Madias NE (2015) Lactic acidosis. N Engl J Med 372:1078–1079
Gorrasi J, Eleftheriadis A, Takala J, Brandt S, Djafarzadeh S, Bruegger LE, Bracht H, Jakob SM (2013) Different contribution of splanchnic organs to hyperlactatemia in fecal peritonitis and cardiac tamponade. BiomedResInt 2013:251084
Levy B, Desebbe O, Montemont C, Gibot S (2008) Increased aerobic glycolysis through beta2 stimulation is a common mechanism involved in lactate formation during shock states. Shock 30:417–421
Ospina-Tascon GA, Hernandez G, Cecconi M (2016) Understanding the venous-arterial CO2 to arterial-venous O2 content difference ratio. Intensive Care Med 42:1801–1804
Ospina-Tascon GA, Umana M, Bermudez W, Bautista-Rincon DF, Hernandez G, Bruhn A, Granados M, Salazar B, Arango-Davila C, De Backer D (2015) Combination of arterial lactate levels and venous-arterial CO2 to arterial-venous O2 content difference ratio as markers of resuscitation in patients with septic shock. Intensive Care Med 41:796–805
Mekontso-Dessap A, Castelain V, Anguel N, Bahloul M, Schauvliege F, Richard C, Teboul JL (2002) Combination of venoarterial PCO2 difference with arteriovenous O2 content difference to detect anaerobic metabolism in patients. Intensive Care Med 28:272–277
Vallet B, Teboul JL, Cain S, Curtis S (2000) Venoarterial CO(2) difference during regional ischemic or hypoxic hypoxia. J Appl Physiol (1985) 89:1317–1321
Douglas AR, Jones NL, Reed JW (1988) Calculation of whole blood CO2 content. J Appl Physiol (1985) 65:473–477
Brandt S, Regueira T, Bracht H, Porta F, Djafarzadeh S, Takala J, Gorrasi J, Borotto E, Krejci V, Hiltebrand LB, Bruegger LE, Beldi G, Wilkens L, Lepper PM, Kessler U, Jakob SM (2009) Effect of fluid resuscitation on mortality and organ function in experimental sepsis models. Crit Care 13:R186
Regueira T, Djafarzadeh S, Brandt S, Gorrasi J, Borotto E, Porta F, Takala J, Bracht H, Shaw S, Lepper PM, Jakob SM (2012) Oxygen transport and mitochondrial function in porcine septic shock, cardiogenic shock, and hypoxaemia. Acta Anaesthesiol Scand 56:846–859
Correa TD, Pereira AJ, Brandt S, Vuda M, Djafarzadeh S, Takala J, Jakob SM (2017) Time course of blood lactate levels, inflammation, and mitochondrial function in experimental sepsis. Crit Care 21:105
Lauscher P, Kertscho H, Schmidt O, Zimmermann R, Rosenberger P, Zacharowski K, Meier J (2013) Determination of organ-specific anemia tolerance. Crit Care Med 41:1037–1045
Stanley WC, Chandler MP (2002) Energy metabolism in the normal and failing heart: potential for therapeutic interventions. Heart Fail Rev 7:115–130
Levy B, Gibot S, Franck P, Cravoisy A, Bollaert PE (2005) Relation between muscle Na+K+ ATPase activity and raised lactate concentrations in septic shock: a prospective study. Lancet 365:871–875
Brooks GA (2018) The science and translation of lactate shuttle theory. Cell Metab 27:757–785
Cohen IL, Sheikh FM, Perkins RJ, Feustel PJ, Foster ED (1995) Effect of hemorrhagic shock and reperfusion on the respiratory quotient in swine. Crit Care Med 23:545–552
Dubin A, Estenssoro E, Murias G, Pozo MO, Sottile JP, Baran M, Piacentini E, Canales HS, Etcheverry G (2004) Intramucosal-arterial Pco2 gradient does not reflect intestinal dysoxia in anemic hypoxia. J Trauma 57:1211–1217
Ruokonen E, Takala J, Kari A, Saxén H, Mertsola J, Hansen EJ (1993) Regional blood flow and oxygen transport in septic shock. Crit Care Med 21:1296–1303
Uusaro A, Ruokonen E, Takala J (1996) Splanchnic oxygen transport after cardiac surgery: evidence for inadequate tissue perfusion after stabilization of hemodynamics. Intensive Care Med 22:26–33
Rasmussen A, Skak C, Kristensen M, Ott P, Kirkegaard P, Secher NH (1999) Preserved arterial flow secures hepatic oxygenation during haemorrhage in the pig. J Physiol 516(Pt 2):539–548
Meyer C, Stumvoll M, Dostou J, Welle S, Haymond M, Gerich J (2002) Renal substrate exchange and gluconeogenesis in normal postabsorptive humans. Am J Physiol Endocrinol Metab 282:E428-434
Jang C, Hui S, Zeng X, Cowan AJ, Wang L, Chen L, Morscher RJ, Reyes J, Frezza C, Hwang HY, Imai A, Saito Y, Okamoto K, Vaspoli C, Kasprenski L, Zsido GA 2nd, Gorman JH 3rd, Gorman RC, Rabinowitz JD (2019) Metabolite exchange between mammalian organs quantified in pigs. Cell Metab 30:594-606.e593
Acknowledgements
The work was performed in the Experimental Surgery Facility, DBMR, University of Bern. We thank the Research Nurses, Olgica Beslac and Daniel Mettler for their assistance during the experiments. TDC would like to thank Eliézer Silva, Henrique Sutton de Sousa Neves, Luiz Vicente Rizzo and Oscar Fernando Pavão dos Santos for their support and encouragement during his postdoctoral fellowship at Department of Intensive Care Medicine, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
Funding
This work was supported by the Swiss National Science Foundation (Grant nº 32003B-127619) and the Stiftung für die Forschung in Anästhesiologie und Intensivmedizin, Bern, awarded to SMJ.
Author information
Authors and Affiliations
Contributions
TDC, AJP, JT and SMJ devised the study protocol. TDC and SMJ analyzed the data. TDC and AJP wrote the first manuscript draft. SMJ and JT critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the National Institutes of Health guidelines for the care and use of experimental animals and with the approval of the Animal Care Committee of the Canton of Bern, Switzerland.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
40635_2020_353_MOESM1_ESM.docx
Additional file 1 (DOCX 750 kb) Table S1. Survival accordingly to study groups. Values represent n/n total (%).Table S2. Correlation between renal venous-arterial CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2) and systemic and regional hemodynamics, kidney vein hemoglobin and blood gas analysis, and lactate uptake (n = 313). Table S3. Correlation between spleen venous-arterial CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2) and systemic and regional hemodynamics, spleen vein hemoglobin and blood gas analysis, and lactate uptake (n = 294). Table S4. Correlation between gut venous-arterial CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2) and systemic and regional hemodynamics, mesenteric vein hemoglobin and blood gas analysis, and lactate uptake (n = 312). Table S5. Correlations between liver venous-arterial CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2) and systemic and regional hemodynamics, liver vein hemoglobin and blood gas analysis, and lactate uptake (n = 313). Table S6. Correlation between renal venous-arterial CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2) and systemic and regional hemodynamics, kidney vein hemoglobin and blood gas analysis, and lactate uptake (n = 170; including only systemic Cv-aCO2/Ca-vO2 > 1.0). Table S7. Correlation between spleen venous-arterial CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2) and systemic and regional hemodynamics, spleen vein hemoglobin and blood gas analysis, and lactate uptake (n = 162; including only systemic Cv-aCO2/Ca-vO2 > 1.0). Table S8. Correlation between gut venous-arterial CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2) and systemic and regional hemodynamics, mesenteric vein hemoglobin and blood gas analysis, and lactate uptake (n = 166; including only systemic Cv-aCO2/Ca-vO2 > 1.0). Table S9. Correlations between liver venous-arterial CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2) and systemic and regional hemodynamics, liver vein hemoglobin and blood gas analysis, and lactate uptake (n=171; including only systemic Cv-aCO2/Ca-vO2 > 1.0). Table S10. Contributors to systemic venous-arterial CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2) (n = 147; including only systemic Cv-aCO2/Ca-vO2 > 1.0). Table S11. Contributors to systemic venous-arterial CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2) after adjusting for experimental group (n = 255). Table S12. Contributors to systemic venous-arterial CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2) after adjusting for experimental group (n = 147; including only systemic Cv-aCO2/Ca-vO2 > 1.0). Figure S1. Linear regression and correlation between arterial lactate and base excess. Figure S2. Boxplot of pooled hepatic, hepatosplanchnic, renal, mesenteric and spleen venous-arterial CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2). Figure S3. Systemic and regional CO2 to arterial-venous O2 content difference ratio (Cv-aCO2/Ca-vO2) accordingly to experimental models.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Corrêa, T.D., Pereira, A.J., Takala, J. et al. Regional venous–arterial CO2 to arterial–venous O2 content difference ratio in experimental circulatory shock and hypoxia. ICMx 8, 64 (2020). https://doi.org/10.1186/s40635-020-00353-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40635-020-00353-9