Abstract
Purpose
The Area Measurement And Depth Underlying Structures (AMADEUS) classification system has been proposed as a valuable tool for magnetic resonance (MR)-based grading of preoperatively encountered chondral defects of the knee joint. However, the potential relationship of this novel score with clinical data was yet to determine. It was the primary intention of this study to assess the correlative relationship of the AMADEUS with patient reported outcome scores in patients undergoing medial open-wedge high tibial valgus osteotomy (HTO). Furthermore, the arthroscopic ICRS (International Cartilage Repair Society) grade evaluation was tested for correlation with the AMADEUS classification system.
Methods
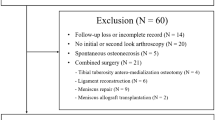
This retrospective, monocentric study found a total of 70 individuals that were indicated for HTO due to degenerative chondral defects of the medial compartment between 2008 and 2019. A preoperative MR image as well as a pre-osteotomy diagnostic arthroscopy for ICRS grade evaluation was mandatory for all patients. The Knee Osteoarthritis Outcome Score (KOOS) including its five subscale scores (KOOS-ADL, KOOS-QOL, KOOS-Sports, KOOS-Pain, KOOS-Symptoms) was obtained preoperatively and at a mean follow-up of 41.2 ± 26.3 months. Preoperative chondral defects were evaluated using the AMADEUS classification system and the final AMADEUS scores were correlated with the pre- and postoperative KOOS subscale sores. Furthermore, arthroscopic ICRS defect severity was correlated with the AMADEUS classification system.
Results
There was a statistically significant correlation between the AMADEUS BME (bone marrow edema) subscore and the KOOS Symptoms subscore at the preoperative visit (r = 0.25, p = 0.04). No statistically significant monotonic association between the AMADEUS total score and the AMADEUS grade with pre- and postoperative KOOS subscale scores were found. Intraoperatively obtained ICRS grade did reveal a moderate correlative relation with the AMADEUS total score and the AMADEUS grade (r = 0.28, p = 0.02).
Conclusions
The novel AMADEUS classification system largely lacks correlative capacity with patient reported outcome measures in patients undergoing HTO. The MR tomographic appearance of bone marrow edema is the only parameter predictive of the clinical outcome at the preoperative visit.
Similar content being viewed by others
Background
Focal cartilage defects of the knee joint are among others a well-known risk factor predisposing to osteoarthritis (OA) of the whole joint. With the raising socioeconomic burden due to osteoarthritis of the knee joint, surgical treatment modalities addressing the recovery of cartilage defects and thereby hindering the accelerated progression to OA are getting increasingly important [13, 15, 19]. Medial open-wedge high tibial valgus osteotomy (HTO) aims to slow down cartilage deterioration in a varus deformity knee by unloading the medial compartment and thereby restoring knee function [1]. The choice of cartilage repair techniques deeply depends on a thorough evaluation of the cartilage defect severity.
It is the purpose of the recently reported AMADEUS (Area Measurement And Depth Underlying Structures) score to aid in the meticulous defect severity grading. This magnetic resonance (MR) – based classification system allows for a thorough assessment of the cartilage defect area and defect depth including the integrity of the subchondral bone which can be transferred to a total score ranging from zero to 100 (0 = worst score, 100 = best score) [11]. Furthermore, the total AMADEUS score can be transformed to an AMADEUS grade ranging from I to IV (I = best grade, IV = worst grade) for an ICRS (International Cartilage Repair Society) like appearance [11]. Relative association of the AMADEUS classification system with the arthroscopically assessed ICRS classification system has already been demonstrated [7], the association of the AMADEUS with patient-reported outcome measures (PROMs) is still widely unknown. Therefore, this is the first study to investigate the correlative capacity of the AMADEUS classification system with the Knee Osteoarthritis Outcome Score (KOOS) in patients undergoing HTO due to degenerative chondral lesions of the medial compartment. Furthermore, the arthroscopically assessed ICRS grade was to evaluate for its relationship with the MR-based AMADEUS system. A weak correlative association between the AMADEUS grading system and the KOOS was hypothesized.
Materials and methods
Study population and design
This retrospective study was approved by the local ethics committee and the requirement for informed consent was waived. A total of 70 patients were indicated for HTO at a single university orthopedic center from 2008 to 2019 and data were retrospectively analyzed by means of digitally archived medical records. Inclusion criteria for this study were defined as follows: (1) enduring knee pain predominantly of the medial compartment of the knee, (2) varus deformity of the tibial plateau of the affecting limb, (3) preserved and intact lateral and retropatellar knee compartment, (4) preoperatively performed MR exam of the knee of sufficient quality for evaluation of the chondral integrity, (5) either radiographically (MRI) or arthroscopically diagnosed focal cartilage defect of the medial compartment. Patients with early osteoarthritic changes of the medial compartment rather than a focal cartilage defect were not found eligible for this study. At the beginning of the study, a sample size calculation was performed based on the hypothesis of a weak correlation between the AMADEUS and the KOOS.
Surgical technique
All patients were obligated to obtain a full-length weight bearing radiograph of the lower limb before surgery. Correction deformity was planned according to the radiographs and the correction angle of the opening wedge hinge was calculated. Target parameters for the correction osteotomy were defined as follows: 1) Intersection of the weightbearing line at 62.5% of the mediolateral tibial plateau width which roughly corresponds to the lateral tibial spine in the coronal plane; 2) a mechanical femorotibial angle of 3 to 5 degrees of valgus were desired; 3) Relocating the weight bearing axis through the Fujisawa point (i.e. 30% to 40% lateral to the midpoint) [6]. Surgical-wise, a medial approach was used and a biplanar L-shaped medial osteotomy was subsequently performed. The posteromedial site was gradually opened until the desired correction angle was achieved. The correction angle was checked intraoperatively using fluoroscopy. Afterwards, the osteotomy site was secured using plate fixation (TomoFix, Synthes, Solothan, Switzerland). The postoperative protocol encompassed a six-week period of non-weightbearing ambulation accompanied by passive motion exercises. A braced hinge allowing the knee-flexion up to 90 degrees was further applied for 6 weeks. After radiographic controls were obtained 6 weeks postoperatively progressive weightbearing was commenced and knee flexion was no longer limited.
Patient reported outcome measures (PROMs)
Patient reported outcome measures were evaluated using the KOOS including its five sub-divisions (KOOS-Pain, KOOS-Symptoms, KOOS-ADL, KOOS-QOL and KOOS-Sports) and established guidelines for final scoring were used [3]. For this study, all patients were asked to fill in the KOOS questionnaire the day before surgery and at specific re-visits postoperatively.
AMADEUS grading
The routinely obtained preoperative MR-scans of the affected knee were analyzed by one experienced and in musculoskeletal imaging trained radiologist who was otherwise not involved in the clinical setting of this study, as well as by one physician in residency training for orthopedic surgery. Chondral defects of the medial compartment were evaluated according to the AMADEUS protocol recently published by Jungmann et al. [11]. Sagittal and coronal images of a cartilage sensitive sequence (i.e. MR images of an intermediate-weighted (IM) or T2-weighted fast spin echo (FSE) sequence or a proton-density (PD) weighted sequence in combination with an T2-weighted FSE in at least two planes) were used for evaluation of the total defect size area. Furthermore, defect depth of the chondral defect was graded into four increments (no defect, signal alteration, partial thickness, and full thickness) and the integrity of the subchondral bone was evaluated separately with three increments (no bony defect, bony defect ≤ 5 mm in depth and bony defect > 5 mm in depth). Additionally, the presence of a surrounding bone marrow edema (BME) was also noted. Based on the subscores, a total AMADEUS score ranging from zero (severe cartilage defect) to 100 (no osteochondral defect) was formed. The AMADEUS total score was then transferred to an AMADEUS grade ranging from I (minimal defect severity) to IV (highest defect severity) according to the AMADEUS protocol recently published [11]. Example images for defect severity grading are given in Fig. 1.
Example MR images for illustration of chondral defect severity grading according to the AMADEUS protocol. A Proton density fat saturated (coronal view) and T2-weighted (sagittal view) MRI images. Example of a patient with a full chondral defect but with an intact subchondral layer. The defect area was measured as 1.06 cm2. A bone marrow edema is clearly visible in the proton density fat weighted images (cornal view). This corresponds to a total AMADEUS score of 60 points: First digit “Area”: 30 points (> 1 cm2 to ≤ 2 cm2), second digit “Depth”: 0 points (full thickness), third digit “Underlying Structures”: 30 points (no bony defect), fourth digit “Bone Marrow Edema”: 0 points (present bone marrow edema). B Proton density fat saturated (coronal view) and T2-weighted fast spine echo (sagittal view) images. Example of a patient with a full chondral defect and concomitant lesion of the subchondral layer. The defect area was measured as 2.27 cm2. A bone marrow edema was not visible. This corresponds to a total AMADEUS of 30 points: First digit “Area”: 20 points (> 2 cm2 to ≤ 4 cm2), second digit “Depth”: 0 points (full thickness), third digit “Underlying Structures”: 0 points (Bony defect > 5 mm), fourth digit “Bone Marrow Edema”: 10 points (no present bone marrow edema)
Statistics
Statistical analysis was performed using SPSS statistical software (SPSS, Chicago, IL, USA, Version 27). A p-value of 0.05 was set as level of significance. Normal distribution was tested using the Kolmogorov-Smirnov test and Shapiro-Wilk test. Distribution und quantities were assessed for categorical variables. For numeric data, mean values and standard deviations were calculated. Differences between pre- and postoperative values in the PROMs scores were assessed using a paired T-Test or one-way ANOVA analysis with a post-hoc Bonferroni Test. In case of non-parametric data, the Mann-Whitney U or Kruskal-Wallis-Test were used instead. Correlative relationship between the different variables was calculated using to the non-parametric Spearman rank correlation coefficient (Spearman R). The strength of the association was evaluated according to the suggestions of Chan et al. [4]. Interrater reliability was calculated using the cohens kappa coefficient. A sample size calculation was performed before the study, assuming a weak correlation (r = 0.3) between the AMADEUS and KOOS scores aiming at statistical power of 0.80. Based on these parameters, a minimal number of 67 patients were needed.
Results
A total of 70 patients were included in this study with a strong prevalence of male patients (64 male patients vs. six female patients). Descriptive data of the patient cohort are depicted in Table 1.
Regarding the AMADEUS subscores, there was a statistically significant correlation between the AMADEUS BME (bone marrow edema) subscore and the KOOS-Symptoms subscore at the preoperative visit (Table 2, Fig. 2). No statistically significant monotonic association between the AMADEUS total score and the AMADEUS grade with pre- and postoperative KOOS subscale scores were found. Intraoperatively obtained ICRS grade did reveal a moderate correlative relation with the AMADEUS total score and the AMADEUS grade (Table 3). However, the ICRS grade did not reveal a correlative capacity with the pre- and postoperative KOOS subscales scores (Fig. 3).
The mean AMADEUS total score including the AMADEUS subscores as well as the pre- and postoperative KOOS subscores are depicted in Table 4. Figure 4 shows the distribution of the four AMADEUS subscores within the patient collective. Furthermore, mean KOOS subscore values did not differ significantly between distinct AMADEUS grades at the pre- and postoperative visit (Table 5). Patients with concomitant BME surrounding the cartilage defect area had a significantly lower KOOS-Symptoms subscore at the preoperative visit (p = 0.04). This finding was not present for the postoperative visit.
The mean chondral defect sizes of the medial compartment are depicted in Table 6. 74% of the chondral lesions were located at the medial femoral condyle in the central weight-bearing area whereas 26% of chondral defects were found at the medial tibial plateau. Interestingly, the majority of defects was small in total diameter (90.2% below 2 cm2) but with a relatively deep extension into the chondral layers (56.3% full or partial thickness defects).
Regarding the interrater reliability of the AMADEUS total score, a fair agreement was found between both raters (k = 0.23, p = 0.00).
Discussion
As a main result of this study, a moderate correlative relation could be demonstrated between the AMADEUS BME subscore and the KOOS-Symptoms subscale at the preoperative visit. However, there was no correlative capacity of the AMADEUS total score or the AMADEUS grade with the KOOS subscale scores. Moreover, the AMADEUS BME subscore did not reveal correlative association with the KOOS-Symptoms and the remaining KOOS subscales at the postoperative visit.
These findings suggest that the MR based evaluation of chondral defect severity as assessed with the AMADEUS is not able to fully reflect the clinical condition in terms of function and pain. This finding is supported by a recent study of Runer et al. who also could not demonstrate a correlative capacity of the AMADEUS classification system with the knee specific IKDC questionnaire at the preoperative visit [23]. However, the only radiographic feature of the AMADEUS that is linked to the clinical condition of knee is the presence of a BME surrounding the cartilage defect. In this study, the presence of a BME was associated with a lower KOOS Symptoms subscale score at the preoperative visit and subanalysis revealed a statistically significant difference in the KOOS-Symptoms subscale score between patients with and without BME. Furthermore, the presence of BME in addition to cartilage defects has been reported as a frequent side effect with an incidence of 55% to 83% [12, 22]. Nevertheless, its role and influence on the functional outcome before and after cartilage repair surgery remains controversial. Niemeyer et al. indicated worse functional outcome in terms of the IKDC score before and after autologous chondrocyte implantation (ACI) in cases with BME [17]. Contrary, Niethammer et al. was not able to demonstrate inferior results in patients with concomitant BME following ACI [18]. Notably, Yang et al. found a nearly significant correlation between the presence of BME and the preoperative functional outcome scores in patients undergoing HTO [25]. Regarding the postoperative visit, the same authors did not find a significant difference in the functional outcome scores concluding that a preoperative BME may not influence the postoperative outcome following HTO [25]. This finding goes along with the results of the present study as there was no difference in the functional outcome scores at the postoperative visit following HTO.
As the second important finding of this study, there was a moderate correlative relation between the MR based AMADEUS total score and AMADEUS grade with the arthroscopically assessed ICRS grade of the cartilage defect. This result is well in line with recently published literature [7]. Especially with current treatment guidelines being based on the ICRS classification system, the AMADEUS classification system yields the potential for a non-invasive diagnostic tool of therapeutic relevance.
The relationship between MR based radiographic findings and its translation into clinical outcome in patients with knee related problems has been topic of ongoing interest from the year one [2, 9, 14]. So far, several studies have been conducted to evaluate a potential correlation of radiographic MRI data with the clinical outcome at the postoperative stage after surgical cartilage repair techniques have been applied [5, 8, 10, 16, 20]. While most of these studies show a relatively high inconsistency between radiographic and clinical data, less is known for a potential correlative relationship at the preoperative visit. Runer et al. investigated the correlation of the novel AMADEUS classification system with various clinical outcome scores including the International Knee Documentation Committee (IKDC), Short-Form-12 (SF-12) and the Core Outcome Measures Index (COMI) in a patient cohort undergoing autologous chondrocyte implantation (ACI) [23]. As a result, they could demonstrate only a weak correlative capacity of the AMADEUS grading with the preoperatively evaluated COMI score [23]. This finding requires further scientific acknowledgement, as it is unusual for a non-knee-specific patient assessed questionnaire to be more sensitive and concurrent with radiographic data than established knee specific questionnaires like the IKDC and KOOS. To our knowledge, the KOOS has not yet put to test for a correlative relationship with the AMADEUS classification system, which seems inevitable, as the KOOS is another highly validated and often used knee specific questionnaire. Tanner et al. analyzed eleven different knee specific self-assessed questionnaires and concluded that the IKDC and KOOS constitute the evaluation tools that are most important and useful to patients with knee related problems [24].
By selecting patients with mainly degenerative chondral defects due to medial overload of the knee joint, the KOOS seemed most appropriate for the patient cohort of this study, as the KOOS has been validated both for osteochondral defects and osteoarthritis (OA) of the knee joint [3, 21]. It seems uncontroversial that the relationship between clinical and radiographic data is remarkedly influenced by the PROMs chosen for a specific subset of patients. A PROM that may demonstrate a weak sensitivity and specificity or may not even yield validation for the subset of patients considered in a study, will negatively influence a potential correlative association.
This study has several limitations and strengths. There was only one study cohort considered for this study. Diversifying the patient population in terms of the applied surgical procedure would have added additional strength to this study. The same holds true for the evaluated PROM. Analysis of various self-assessed generic and knee-specific questionnaires would have amplified the strength of this study. Unfortunately, the native AMADEUS protocol does not regard the size of the adjacent BME which would have enhanced the study quality.
Yet this is the first study investigating the relationship of the novel AMADEUS classification system with the knee specific KOOS questionnaire. Furthermore, this is the first study considering the AMADEUS for patients undergoing HTO. By inclusion of a total of 70 patients, the number of included individuals seemed to be sufficient when compared to similar studies regarding this topic [11, 23].
Conclusion
The novel AMADEUS classification system largely lacks correlative capacity with patient reported outcome measures in patients undergoing HTO. The MR tomographic appearance of bone marrow edema is the only parameter predictive of the clinical outcome at the preoperative visit.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACI:
-
Autologous Chondrocyte Implantation
- AMADEUS:
-
Area Measurement And Depth and Underlying Structure
- COMI:
-
Core Outcome Measures Index
- HTO:
-
High tibial valgus osteotomy
- ICRS:
-
International Cartilage Repair Society
- IKDC:
-
International Knee Documentation Committee
- KOOS:
-
Knee Osteoarthritis Outcome Score
- MRI:
-
Magnetic resonance imaging
- OA:
-
Osteoarthritis
- PROM:
-
Patient reported outcome measure
References
Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P (2007) The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy 23:852–861
Bedson J, Croft PR (2008) The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord 9:116
Bekkers JE, de Windt TS, Raijmakers NJ, Dhert WJ, Saris DB (2009) Validation of the knee injury and osteoarthritis outcome score (KOOS) for the treatment of focal cartilage lesions. Osteoarthr Cartil 17:1434–1439
Chan Y (2003) Biostatistics 104: correlational analysis. Singap Med J 44:614–619
Choi YS, Potter HG, Chun TJ (2008) MR imaging of cartilage repair in the knee and ankle. Radiographics 28:1043–1059
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am 10:585–608
Heinz T, Meller F, Luetkens KS, Horas K, Schäfer T, Rudert M et al (2022) Can the MRI based AMADEUS score accurately assess pre-surgery chondral defect severity according to the ICRS arthroscopic classification system? J Exper Orthop 9:83
Henderson I, Tuy B, Connell D, Oakes B, Hettwer W (2003) Prospective clinical study of autologous chondrocyte implantation and correlation with MRI at three and 12 months. J Bone Joint Surg 85:1060–1066 British
Hernández-Vaquero D, Fernández-Carreira JM (2012) Relationship between radiological grading and clinical status in knee osteoarthritis. A multicentric study. BMC Musculoskeletal Disorders 13:1–8
Ho YY, Stanley AJ, Hui JH-P, Wang S-C (2007) Postoperative evaluation of the knee after autologous chondrocyte implantation: what radiologists need to know. Radiographics 27:207–220
Jungmann PM, Welsch GH, Brittberg M, Trattnig S, Braun S, Imhoff AB et al (2016) Magnetic resonance imaging score and classification system (AMADEUS) for assessment of preoperative cartilage defect severity. CARTILAGE 8:272–282
Kijowski R, Stanton P, Fine J, De Smet A (2006) Subchondral bone marrow edema in patients with degeneration of the articular cartilage of the knee joint. Radiology 238:943–949
Klug A, Gramlich Y, Rudert M, Drees P, Hoffmann R, Weißenberger M et al (2021) The projected volume of primary and revision total knee arthroplasty will place an immense burden on future health care systems over the next 30 years. Knee Surg Sports Traumatol Arthrosc 29:3287–3298
Larsson AC, Petersson I, Ekdahl C (1998) Functional capacity and early radiographic osteoarthritis in middle-aged people with chronic knee pain. Physiother Res Int 3:153–163
Litwic A, Edwards MH, Dennison EM, Cooper C (2013) Epidemiology and burden of osteoarthritis. Br Med Bull 105:185–199
Marlovits S, Singer P, Zeller P, Mandl I, Haller J, Trattnig S (2006) Magnetic resonance observation of cartilage repair tissue (MOCART) for the evaluation of autologous chondrocyte transplantation: determination of interobserver variability and correlation to clinical outcome after 2 years. Eur J Radiol 57:16–23
Niemeyer P, Salzmann G, Steinwachs M, Südkamp NP, Schmal H, Lenz P et al (2010) Presence of subchondral bone marrow edema at the time of treatment represents a negative prognostic factor for early outcome after autologous chondrocyte implantation. Arch Orthop Trauma Surg 130:977–983
Niethammer TR, Valentin S, Gülecyüz MF, Roßbach BP, Ficklscherer A, Pietschmann MF et al (2015) Bone marrow edema in the knee and its influence on clinical outcome after matrix-based autologous chondrocyte implantation: results after 3-year follow-up. Am J Sports Med 43:1172–1179
Oliveria SA, Felson DT, Reed JI, Cirillo PA, Walker AM (1995) Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum 38:1134–1141
Recht MP, Goodwin DW, Winalski CS, White LM (2005) MRI of articular cartilage: revisiting current status and future directions. AJR Am J Roentgenol 185:899
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther 28:88–96
Rubin DA, Harner CD, Costello JM (2000) Treatable chondral injuries in the knee: frequency of associated focal subchondral edema. Am J Roentgenol 174:1099–1106
Runer A, Jungmann P, Welsch G, Kümmel D, Impellizzieri F, Preiss S et al (2019) Correlation between the AMADEUS score and preoperative clinical patient-reported outcome measurements (PROMs) in patients undergoing matrix-induced autologous chondrocyte implantation (MACI). J Orthop Surg Res 14:87
Tanner SM, Dainty KN, Marx RG, Kirkley A (2007) Knee-specific quality-of-life instruments: which ones measure symptoms and disabilities most important to patients. Am J Sports Med 35:1450–1458
Yang H-Y, Kang S-J, Kwak W-K, Song E-K, Seon J-K (2020) The influence of preoperative Tibial bone marrow edema on outcomes after medial opening-wedge high Tibial osteotomy. JBJS 102(23):2068–2076
Acknowledgments
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. This publication was supported by the Open Access Publication Fund of the University of Wuerzburg.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the manuscript. TH was involved in the study design and manuscript drafting. FM, IS and KSL were responsible for data acquisition and interpretation. Data analysis was performed by KH, PMA and TH. MW was responsible for study supervision and was a major contributor in writing and drafting the manuscript. MR, SR and KLS were involved in data interpretation and designing the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The following study was presented to the local ethics committee. The need for approval has been waived.
Consent for publication
Not applicable.
Competing interests
They authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heinz, T., Meller, F., Luetkens, K.S. et al. The AMADEUS score is not a sufficient predictor for functional outcome after high tibial osteotomy. J EXP ORTOP 10, 9 (2023). https://doi.org/10.1186/s40634-023-00575-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-023-00575-2