Abstract
Background
Post-resuscitation hemodynamic level is associated with outcomes. This study was conducted to investigate if post-resuscitation diastolic blood pressure (DBP) is a favorable prognostic factor.
Methods
Using TaIwan Network of Targeted Temperature ManagEment for CARDiac Arrest (TIMECARD) registry, we recruited adult patients who received targeted temperature management in nine medical centers between January 2014 and September 2019. After excluding patients with extracorporeal circulation support, 448 patients were analyzed. The first measured, single-point blood pressure after resuscitation was used for analysis. Study endpoints were survival to discharge and discharge with favorable neurologic outcomes (CPC 1–2). Multivariate analysis, area under the receiver operating characteristic curve (AUC), and generalized additive model (GAM) were used for analysis.
Results
Among the 448 patients, 182 (40.7%) patients survived, and 89 (19.9%) patients had CPC 1–2. In the multivariate analysis, DBP > 70 mmHg was an independent factor for survival (adjusted odds ratio [aOR] 2.16, 95% confidence interval [CI, 1.41–3.31]) and > 80 mmHg was an independent factor for CPC 1–2 (aOR 2.04, 95% CI [1.14–3.66]). GAM confirmed that DBP > 80 mmHg was associated with a higher likelihood of CPC 1–2. In the exploratory analysis, patients with DBP > 80 mmHg had a significantly higher prevalence of cardiogenic cardiac arrest (p = 0.015) and initial shockable rhythm (p = 0.045).
Conclusion
We found that DBP after resuscitation can predict outcomes, as a higher DBP level correlated with cardiogenic cardiac arrest.
Similar content being viewed by others
Background
Post-cardiac arrest care is crucial for arrested patients, especially for those not returning to baseline consciousness. One of the approaches is to optimize these patients’ hemodynamic status. Several observational studies have shown that hypotension in post-resuscitated patients is related to poor outcomes [1,2,3,4,5,6]. Current guidelines recommend maintaining mean blood pressure (MBP) higher than 65 mmHg or systolic blood pressure (SBP) higher than 90 mmHg [7, 8]. European Resuscitation Council guidelines also recommend an individualized hemodynamic target in the post-cardiac arrest care period [8].
The lower limit of cerebral autoregulation might become higher in post-resuscitated patients [9]. Targeting higher blood pressure (BP) might theoretically improve cerebral blood perfusion and neurologic outcomes [10]. However, current evidence is not conclusive, and several observational studies have reported controversial results [6, 11,12,13,14,15,16,17]. Recent randomized studies reported no difference in long-term cognitive function, serum neuron-specific enolase level, or brain image findings when targeting higher MBP levels during early post-cardiac arrest care [18,19,20]. However, these studies were conducted with small sample sizes.
Targeted treatment for diastolic blood pressure (DBP) level during the post-resuscitated period is less studied. The physiological significance of DBP differs from that of SBP. A higher DBP level indicates higher peripheral vascular resistance, better coronary vessel perfusion, and better survival in cardiogenic shock patients [21]. Only one study reported a correlation between DBP level during the first 6 h of care in an intensive care unit (ICU) and neurologic outcomes of cardiac arrest patients [22]. Recent studies have shown the prognostic value of DBP during cardiopulmonary resuscitation (CPR) in predicting successful resuscitation [23,24,25].
In this study, we aimed to demonstrate the correlation between patients’ outcomes and hemodynamic parameters when return of spontaneous circulation (ROSC) occurs. We hypothesized that DBP during ROSC is a prognostic factor for outcomes of cardiac arrest patients. We also sought to explain the possible pathophysiological relation between DBP and the outcomes.
Methods
Study population and setting
In January 2014, the Taiwan Society of Emergency and Critical Care Medicine launched the TaIwan Network of Targeted Temperature ManagEment for CARDiac Arrest (TIMECARD) registry to establish a study cohort of patients treated with targeted temperature management (TTM). The TIMECARD registry is a nationwide, multicenter, post-cardiac arrest care registry collecting information on patients with TTM in Taiwan. Enrolled patients included non-traumatic out-of-hospital cardiac arrest (OHCA) or in-hospital cardiac arrest (IHCA) adult survivors who were treated with TTM in nine medical centers in Taiwan [26].
Patients were resuscitated and treated according to current guidelines [7, 8]. Patients with sustained ROSC and remaining in a comatose state received TTM for less than 12 h in the ICU. Comatose state was defined by a Glasgow Coma Scale score of less than 8 or inability to obey commands. Cooling was performed using cooling blankets or venous cooling catheters according to the protocols in each hospital. Core body temperature was recorded using esophageal probes or venous catheters. The targeted temperature of 33 °C was achieved as soon as possible, maintained for 24 h, and followed by a slow rewarming stage until the body temperature reached 36.5 °C at a rate of 0.25 °C per hour. The hemodynamic status was recorded by non-invasive blood pressure (NIBP) monitoring in the emergency department (ED) or general ward and using an arterial catheter in the ICU.
Patients’ demographic factors, medical histories, and cardiac arrest variables were recorded in the registry according to the Utstein style after reviewing pre-hospital and hospital medical records [27]. In addition to Utstein style parameters, details of resuscitation, hemodynamic status during ROSC, new-onset complications during post-cardiac arrest care, performing of percutaneous coronary intervention (PCI), and extracorporeal membrane oxygenation (ECMO) during resuscitation were also recorded.
Patient selection, data acquisition, and outcome measurements
In this study, the study population was retrospectively retrieved from the TIMECARD registry for the period of January 2014 to September 2019. Adult non-traumatic OHCA or IHCA survivors treated with TTM were included. Patients with a pre-arrest cerebral performance category (CPC) 3–4 were excluded from the study due to the neurologic endpoints of this study. Patients who received ECMO support during resuscitation were also excluded because hemodynamic monitoring was often influenced by extracorporeal pumping.
Patients’ demographic data, underlying comorbidities, cardiac arrest etiologies, initial rhythms, total CPR durations, total epinephrine dosages during CPR and performing of PCI were analyzed. The first measured, single-point BP after achieving ROSC was used for analysis. The BP was mostly monitored by NIBP because almost all cardiac arrests occurred in the ED or ward. SBP and DBP were recoded accordingly. MBP was estimated by the following formula: MBP = DBP + 1/3 (SBP – DBP). New-onset complications during post-cardiac arrest care, such as bleeding, severe infection, arrhythmia, seizure, and hypoglycemia were analyzed to explain the possible pathophysiology mechanism. If the abovementioned complications occurred within the first 7 days of ICU admission, then these complications were defined as new-onset complications. New-onset bleeding was defined as any visible bleeding with a need for further blood transfusion. New-onset severe infection was defined as the development of any new pneumonia patches, septic shock, or bacteremia. The endpoints of this study were survival to discharge and discharge with favorable neurologic outcomes (CPC 1–2).
Statistical analysis
Continuous variables were converted to categorial subgroups using appropriate methods due to the non-normal distribution. Categorical variables were presented as case numbers and percentages. The Chi-square test or Fisher exact test was used for univariate analysis. Those variables with p-values < 0.1 were included in a stepwise logistic regression for predicting independent variables of outcomes. Independent variables were presented with adjusted odds ratios (aORs) and 95% confidence intervals (CIs). Receiver operating characteristic (ROC) curves for survival and favorable neurologic outcomes were plotted according to SBP, MBP, and DBP values. The generalized additive model (GAM) was used to visualize the association between DBP and favorable outcomes. The threshold DBP value for better outcomes was determined by testing incremental cut-off values of DBP until there was no difference between the two groups in the multivariate analysis. Finally, the threshold was used for stratifying the study population into two groups with high and low DBP values. Outcomes, characteristics, and post-cardiac arrest complications of these two groups were compared by exploratory analysis. All statistical analyses were performed using STATA software version 16 (StataCorp, TX, USA).
Results
Overview
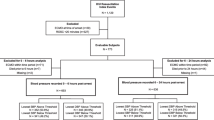
During the study period, a total of 540 patients were enrolled in the TIMECARD registry. Thirty-seven (7%) patients were excluded for pre-arrest CPC 3–4, and 55 patients (11.0%) were excluded for receiving ECMO. Thus, a total of 448 patients were included in the final analysis (Fig. 1). A total of 182 patients (40.6%) had survival to discharge, and 89 patients (19.9%) were discharged with favorable neurologic outcomes.
Characteristics and predictive factors of survival to discharge
The results of the univariate and multivariate analyzes for predictive factors of survival are listed in Table 1. In the univariate analysis, the ROSC DBP distributions of the survival and non-survival groups differed significantly (p < 0.001), while ROSC SBP showed no difference (p = 0.061). ROSC DBP had an area under the ROC (AUROC) of 0.61 (0.56–0.68) for survival to discharge, while ROSC SBP had an AUROC of 0.58 (0.53–0.64, Fig. 2). In the multivariate analysis, heart failure, end-stage renal disease, initial rhythm, epinephrine dosage, ROSC DBP, and PCI were independent factors for predicting survival to discharge. Patients with ROSC DBP in the range of 70–80 mmHg [aOR: 3.31 (1.65–6.64)], 80–90 mmHg [aOR: 2.13 (1.03–4.40)], and > 90 mmHg [aOR: 1.95 (1.11–3.42)] showed a greater chance of survival than patients with ROSC DBP < 60 mmHg.
Receiver operating characteristic (ROC) curves of systolic blood pressure (SBP), mean blood pressure (MBP), and diastolic blood pressure (DBP) for outcomes. AUROC area under the receiver operating characteristic curve, SBP systolic blood pressure, MBP mean blood pressure, DBP diastolic blood pressure, CPC cerebral performance scale
Characteristics and predictive factors of favorable neurologic outcomes
The results of the univariate and multivariate analyses for predictive factors of favorable neurologic outcomes when discharged are listed in Table 2. In the univariate analysis, the ROSC DBP distributions of the groups with favorable and non-favorable neurologic outcomes differed significantly (p = 0.003), while ROSC SBP showed no difference (p = 0.116). ROSC DBP had an AUROC of 0.64 (0.58–0.70) for CPC 1–2, while ROSC SBP had an AUROC of 0.58 (0.51–0.64, Fig. 2). In the multivariate analysis, diabetes mellitus, malignancy, patients’ bystander status, initial rhythm, CPR duration, and epinephrine dosage were independent factors for predicting favorable neurologic outcomes. Patients with ROSC DBP > 90 mmHg [aOR: 2.73 (1.22–6.10)] showed a greater chance of favorable neurologic outcomes than patients with ROSC DBP < 60 mmHg.
Testing of DBP thresholds for favorable outcomes
The relationship between DBP values and favorable outcomes determined by GAM is shown in Fig. 3. GAM revealed a sigmoid curve in both survival and favorable neurologic outcomes. The cut-off values (log odds > 0; i.e., odds > 1) of DBP were around 70–80 mmHg for both survival and favorable neurologic outcomes.
The DBP threshold for better outcomes was further investigated by subgroup analysis according to incremental DBP cut-off points. The unadjusted and adjusted odds ratios of each DBP threshold, when using patients with DBP values lower than each threshold as a reference, are listed in Table 3. The association between DBP and outcomes decreased with increasing DBP cut-off points. In the multivariate analysis, DBP thresholds of 60, 70, and 80 mmHg were associated with favorable neurologic outcomes. When the DBP threshold reached 90 mmHg, the association with favorable neurologic outcomes was no longer present.
Characteristics of patients with different DBP levels
An exploratory analysis of the characteristics of patients with different DBP levels was performed to evaluate the possible pathophysiological link between DBP and outcomes (Table 4). The DBP cut-off value was set at 80 mmHg according to the results of the threshold analysis. The percentages of survival to discharge (35.8% vs 47.8%, p = 0.012), favorable neurologic outcomes (14.6% vs 27.8%, p = 0.001), male gender (60.1% vs 69.4%, p = 0.043), initial shockable rhythm (28.7% vs 37.8%, p = 0.045), and cardiac etiologies (43.7% vs 55.6%, p = 0.015) were significantly higher in patients with higher DBP. The prevalence of new-onset post-cardiac arrest complications showed no difference between the two groups.
Discussion
In this study, we found that the DBP distributions of patients with and without favorable outcomes when discharged differed significantly, while SBP distributions did not. We further proved that DBP was the only independent hemodynamic predictor by stepwise multivariate logistic regression. The correlation between DBP and favorable outcomes was visualized by GAM, which presented a sigmoid curve in both outcomes. GAM and incremental threshold analysis demonstrated that the DBP cut-off value for favorable neurologic outcomes was around 80 mmHg. We further found that the patient subgroup with higher DBP levels had a higher chance of cardiogenic cardiac arrest and initial shockable rhythm.
Current studies regarding the optimal hemodynamic level during post-cardiac arrest care are inconclusive [28]. Several randomized trials also demonstrated no long-term benefit in targeting a higher hemodynamic level [18,19,20]. However, all these studies focused on SBP and MBP in the post-cardiac arrest period. Only one study found that the lowest DBP during the first 6 h after ICU admission related to the outcomes [22]. Our study was different in that it targeted the hemodynamic level immediately after ROSC, while other studies mainly focused on the ICU period. The benefit of our study design was that it eliminated the confounding effect of inotropic agents and TTM, which strongly affect hemodynamic levels due to the inconsistent use of inotropic agents and different TTM protocols. Other studies similar to our study reported a relationship between outcomes and early hemodynamic level after resuscitation [1, 3, 13]. However, these studies were conducted on patients with pre-hospital ROSC, and only SBP was addressed.
DBP and SBP have different physiologic features. SBP is more sensitive to large artery compliance, cardiac contractility, and intravascular volume change than DBP [29,30,31]. An initial target SBP of 90 mmHg is commonly used in circulatory shock. However, DBP is more related to peripheral vascular resistance if aortic valve function is intact [29, 31,32,33]. Due to decreasing peripheral vascular tone in sepsis, some studies suggested DBP as a more reliable predictor of better outcomes of septic shock patients than SBP [32, 33]. DBP is also strongly related to coronary perfusion during the diastolic phase [34]. Better coronary perfusion is a key determinant of successful resuscitation [35]. Greater DBP values during CPR were associated with a greater chance of ROSC in children and a porcine model [23,24,25].
Our study found that higher DBP values in the early post-resuscitation stage correlated with good outcomes. Two theories might explain the underlying mechanism of the correlation between DBP and the favorable prognosis of cardiac arrest patients. One theory assumes that DBP is correlated with coronal perfusion pressure. Therefore, a better DBP directly leads to better myocardial perfusion and a greater chance of survival. The other theory assumes that the DBP level represents the severity of post-cardiac arrest syndrome [31, 36]. Post-cardiac arrest syndrome, including systemic ischemia and reperfusion injury, is similar to septic shock and can cause peripheral vascular tone loss [36]. As mentioned above, DBP can represent peripheral vascular resistance as well as post-cardiac arrest syndrome. Cardiac arrest patients with initial shockable rhythm and cardiac etiologies were assumed to have shorter no-flow time, less ischemic stress, and less post-cardiac arrest syndrome than those with non-shockable and non-cardiac etiologies [37,38,39]. This hypothesis correlated with our study finding that patients with a higher DBP level had a greater chance of having initial shockable rhythm and cardiogenic cardiac arrest (Table 4). Males had a higher risk of cardiogenic arrest, as seen by the higher correlation between male gender and DBP value in this study. Incidences of other new-onset complications, including bleeding, arrhythmia, sepsis, and seizure, were not different. These severe complications might have multiple causes and cannot be simply explained by the DBP level alone.
The study findings have some clinical implications. First, SBP and MBP are the primary hemodynamic targets for circulatory shock and organ perfusion. However, these two parameters physiologically represent only part of the systemic hemodynamics. Our study showed that ROSC DBP is a more reliable hemodynamic parameter than SBP and can reflect the level of post-cardiac arrest syndrome. DBP can also serve as a surrogate marker of systemic vascular resistance if advanced hemodynamic parameters, such as pulmonary artery catheters or pulse contour cardiac output catheters, are not available. Second, our study suggested that a DBP around 80 mmHg might be a possible clinical target for better outcomes. Theoretically, a higher target BP might improve cerebral blood flow according to the right shift of cerebral autoregulation after cardiac arrest, but recent randomized trials showed no difference in long-term outcomes [18,19,20]. However, the hemodynamic target of these studies was MBP. Our study pointed out a possible DBP target in post-resuscitation care. Future studies emphasizing the optimal DBP level during the post-resuscitation period should be conducted.
This study has several limitations. First, this was a retrospective study, and the study population was retrieved from nine medical centers. Differences among facilities in TTM protocols or post-cardiac arrest management, including nutritional support, and glucose management, could not be addressed in this study. Second, several important prognosis factors, including lactate level, blood gas analysis, urine output, and echocardiography results, were not collected due to the limited registry design. In this study, we aimed to predict patients’ outcomes based on variables at the time of ROSC. Therefore, several post-cardiac arrest care factors, TTM factors and TTM complications were not included in the prediction model. Third, we only evaluated the hemodynamic level at one time point in this study. The complexity of the relationship between hemodynamics, outcomes, inotropic agents, and TTM in the later post-resuscitation period was not addressed. Fourth, we sought to define an optimal hemodynamic level for better outcomes. However, we could only prove the relationship between DBP values and favorable outcomes through statistical analysis. It is unknown whether higher DBP levels lead to better outcomes or patients with better outcomes have higher DBP levels. A further prospective study is needed to estimate the optimal DBP level for post-cardiac arrest patients. Finally, data on the patients’ long-term outcomes after discharge were not available from the registry.
Conclusion
ROSC DBP is an independent hemodynamic predictor of better outcomes. A higher DBP value correlated with a higher prevalence of initial shockable rhythm and cardiogenic cardiac arrest. This finding verifies the hypothesis that DBP level can represent the severity of ischemic stress or post-cardiac arrest syndrome. A further prospective study is needed to determine the optimal DBP value of post-cardiac arrest patients.
Availability of data and materials
The data that support the findings of this study are available from the Taiwan Society of Emergency and Critical Care Medicine, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the Taiwan Society of Emergency and Critical Care Medicine.
Abbreviations
- MBP:
-
Mean blood pressure
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- ICU:
-
Intensive care unit
- ROSC:
-
Return of spontaneous circulation
- TTM:
-
Targeted temperature management
- OHCA:
-
Out-of-hospital cardiac arrest
- IHCA:
-
In-hospital cardiac arrest
- NIBP:
-
Non-invasive blood pressure
- ED:
-
Emergency department
- PCI:
-
Percutaneous coronary intervention
- ECMO:
-
Extracorporeal membrane oxygenation
- CPC:
-
Cerebral performance category
- ROC:
-
Receiver operating characteristic
- GAM:
-
Generalized additive model
- DM:
-
Diabetes mellitus
- HTN:
-
Hypertension
- CAD:
-
Coronary artery disease
- HF:
-
Heart failure
- COPD:
-
Chronic obstructive pulmonary disease
- ESRD:
-
End-stage renal disease
- CPR:
-
Cardiopulmonary resuscitation
- PEA:
-
Pulseless electrical activity
- VT:
-
Ventricular arrhythmia
- VF:
-
Ventricular fibrillation
References
Bray JE, Bernard S, Cantwell K, Stephenson M, Smith K. The association between systolic blood pressure on arrival at hospital and outcome in adults surviving from out-of-hospital cardiac arrests of presumed cardiac aetiology. Resuscitation. 2014;85(4):509–15.
Chiu YK, Lui CT, Tsui KL. Impact of hypotension after return of spontaneous circulation on survival in patients of out-of-hospital cardiac arrest. Am J Emerg Med. 2018;36(1):79–83.
Lacocque J, Siegel L, Sporer KA. Prehospital, post-ROSC blood pressure and associated neurologic outcome. Am J Emerg Med. 2021;49:195–9.
Laurikkala J, Wilkman E, Pettilä V, Kurola J, Reinikainen M, Hoppu S, et al. Mean arterial pressure and vasopressor load after out-of-hospital cardiac arrest: associations with one-year neurologic outcome. Resuscitation. 2016;105:116–22.
Trzeciak S, Jones AE, Kilgannon JH, Milcarek B, Hunter K, Shapiro NI, et al. Significance of arterial hypotension after resuscitation from cardiac arrest. Crit Care Med. 2009;37(11):2895–903; quiz 904.
Young MN, Hollenbeck RD, Pollock JS, Giuseffi JL, Wang L, Harrell FE, et al. Higher achieved mean arterial pressure during therapeutic hypothermia is not associated with neurologically intact survival following cardiac arrest. Resuscitation. 2015;88:158–64.
Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Part 3: adult basic and advanced life support: 2020 American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142(16_Suppl2):S366-s468.
Soar J, Böttiger BW, Carli P, Couper K, Deakin CD, Djärv T, et al. European Resuscitation Council Guidelines 2021: adult advanced life support. Resuscitation. 2021;161:115–51.
Sundgreen C, Larsen FS, Herzog TM, Knudsen GM, Boesgaard S, Aldershvile J. Autoregulation of cerebral blood flow in patients resuscitated from cardiac arrest. Stroke. 2001;32(1):128–32.
Skåre C, Karlsen H, Strand-Amundsen RJ, Eriksen M, Skulberg VM, Sunde K, et al. Cerebral perfusion and metabolism with mean arterial pressure 90 vs. 60 mmHg in a porcine post cardiac arrest model with and without targeted temperature management. Resuscitation. 2021.
Ameloot K, Meex I, Genbrugge C, Jans F, Boer W, Verhaert D, et al. Hemodynamic targets during therapeutic hypothermia after cardiac arrest: a prospective observational study. Resuscitation. 2015;91:56–62.
Huang CH, Tsai MS, Ong HN, Chen W, Wang CH, Chang WT, et al. Association of hemodynamic variables with in-hospital mortality and favorable neurological outcomes in post-cardiac arrest care with targeted temperature management. Resuscitation. 2017;120:146–52.
Javaudin F, Desce N, Le Bastard Q, De Carvalho H, Le Conte P, Escutnaire J, et al. Impact of pre-hospital vital parameters on the neurological outcome of out-of-hospital cardiac arrest: Results from the French National Cardiac Arrest Registry. Resuscitation. 2018;133:5–11.
Roberts BW, Kilgannon JH, Hunter BR, Puskarich MA, Shea L, Donnino M, et al. association between elevated mean arterial blood pressure and neurologic outcome after resuscitation from cardiac arrest: results from a multicenter prospective cohort study. Crit Care Med. 2019;47(1):93–100.
Russo JJ, Di Santo P, Simard T, James TE, Hibbert B, Couture E, et al. Optimal mean arterial pressure in comatose survivors of out-of-hospital cardiac arrest: an analysis of area below blood pressure thresholds. Resuscitation. 2018;128:175–80.
Russo JJ, James TE, Hibbert B, Yousef A, Osborne C, Wells GA, et al. Impact of mean arterial pressure on clinical outcomes in comatose survivors of out-of-hospital cardiac arrest: Insights from the University of Ottawa Heart Institute Regional Cardiac Arrest Registry (CAPITAL-CARe). Resuscitation. 2017;113:27–32.
Grand J, Lilja G, Kjaergaard J, Bro-Jeppesen J, Friberg H, Wanscher M, et al. Arterial blood pressure during targeted temperature management after out-of-hospital cardiac arrest and association with brain injury and long-term cognitive function. Eur Heart J Acute Cardiovasc Care. 2020;9(4_suppl):S122–30.
Ameloot K, De Deyne C, Eertmans W, Ferdinande B, Dupont M, Palmers PJ, et al. Early goal-directed haemodynamic optimization of cerebral oxygenation in comatose survivors after cardiac arrest: the neuroprotect post-cardiac arrest trial. Eur Heart J. 2019;40(22):1804–14.
Ameloot K, Jakkula P, Hästbacka J, Reinikainen M, Pettilä V, Loisa P, et al. Optimum blood pressure in patients with shock after acute myocardial infarction and cardiac arrest. J Am Coll Cardiol. 2020;76(7):812–24.
Jakkula P, Pettilä V, Skrifvars MB, Hästbacka J, Loisa P, Tiainen M, et al. Targeting low-normal or high-normal mean arterial pressure after cardiac arrest and resuscitation: a randomised pilot trial. Intensive Care Med. 2018;44(12):2091–101.
Rigamonti F, Graf G, Merlani P, Bendjelid K. The short-term prognosis of cardiogenic shock can be determined using hemodynamic variables: a retrospective cohort study*. Crit Care Med. 2013;41(11):2484–91.
Annoni F, Dell’Anna AM, Franchi F, Creteur J, Scolletta S, Vincent JL, et al. The impact of diastolic blood pressure values on the neurological outcome of cardiac arrest patients. Resuscitation. 2018;130:167–73.
Berg RA, Sutton RM, Reeder RW, Berger JT, Newth CJ, Carcillo JA, et al. Association between diastolic blood pressure during pediatric in-hospital cardiopulmonary resuscitation and survival. Circulation. 2018;137(17):1784–95.
Morgan RW, French B, Kilbaugh TJ, Naim MY, Wolfe H, Bratinov G, et al. A quantitative comparison of physiologic indicators of cardiopulmonary resuscitation quality: diastolic blood pressure versus end-tidal carbon dioxide. Resuscitation. 2016;104:6–11.
O’Brien CE, Santos PT, Reyes M, Adams S, Hopkins CD, Kulikowicz E, et al. Association of diastolic blood pressure with survival during paediatric cardiopulmonary resuscitation. Resuscitation. 2019;143:50–6.
Chang HC, Tsai MS, Kuo LK, Hsu HH, Huang WC, Lai CH, et al. Factors affecting outcomes in patients with cardiac arrest who receive target temperature management: the multi-center TIMECARD registry. J Formos Med Assoc. 2022;121(1 Pt 2):294–303.
Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care. Perioperat Resuscit Circ. 2015;132(13):1286–300.
Rikhraj KJK, Wood MD, Hoiland RL, Thiara S, Griesdale DEG, Sekhon MS. Determining optimal mean arterial pressure after cardiac arrest: a systematic review. Neurocrit Care. 2021;34(2):621–34.
Pinto E. Blood pressure and ageing. Postgrad Med J. 2007;83(976):109–14.
Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013;369(18):1726–34.
Lamia B, Chemla D, Richard C, Teboul JL. Clinical review: interpretation of arterial pressure wave in shock states. Crit Care. 2005;9(6):601–6.
Ospina-Tascón GA, Teboul JL, Hernandez G, Alvarez I, Sánchez-Ortiz AI, Calderón-Tapia LE, et al. Diastolic shock index and clinical outcomes in patients with septic shock. Ann Intensive Care. 2020;10(1):41.
Benchekroune S, Karpati PC, Berton C, Nathan C, Mateo J, Chaara M, et al. Diastolic arterial blood pressure: a reliable early predictor of survival in human septic shock. J Trauma. 2008;64(5):1188–95.
Feigl EO. Coronary physiology. Physiol Rev. 1983;63(1):1–205.
Naim MY, Sutton RM, Friess SH, Bratinov G, Bhalala U, Kilbaugh TJ, et al. Blood pressure- and coronary perfusion pressure-targeted cardiopulmonary resuscitation improves 24-hour survival from ventricular fibrillation cardiac arrest. Crit Care Med. 2016;44(11):e1111–7.
Nolan JP, Neumar RW, Adrie C, Aibiki M, Berg RA, Böttiger BW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A Scientific Statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke. Resuscitation. 2008;79(3):350–79.
Granfeldt A, Wissenberg M, Hansen SM, Lippert FK, Lang-Jensen T, Hendriksen OM, et al. Clinical predictors of shockable versus non-shockable rhythms in patients with out-of-hospital cardiac arrest. Resuscitation. 2016;108:40–7.
Rajan S, Folke F, Hansen SM, Hansen CM, Kragholm K, Gerds TA, et al. Incidence and survival outcome according to heart rhythm during resuscitation attempt in out-of-hospital cardiac arrest patients with presumed cardiac etiology. Resuscitation. 2017;114:157–63.
Stankovic N, Høybye M, Holmberg MJ, Lauridsen KG, Andersen LW, Granfeldt A. Factors associated with shockable versus non-shockable rhythms in patients with in-hospital cardiac arrest. Resuscitation. 2021;158:166–74.
Acknowledgements
We thank the Taiwan Society of Emergency and Critical Care Medicine for establishing the TIMECARD registry.
Funding
No funding to declare.
Author information
Authors and Affiliations
Contributions
CHH and HCHC were involved in the study design. MST, LKK, HHH, WCH, CHL, and CHH were involved in the data acquisition. CYC, MST, CLT, and CHH were involved in statistical analysis and data interpretation. CYC drafted the first manuscript. CLT and CHH made the final revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Research Ethics Committee of National Taiwan University Medical College.
Consent for publication
Not applicable.
Competing interests
All authors declare that there is no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chi, CY., Tsai, MS., Kuo, LK. et al. Post-resuscitation diastolic blood pressure is a prognostic factor for outcomes of cardiac arrest patients: a multicenter retrospective registry-based analysis. j intensive care 10, 39 (2022). https://doi.org/10.1186/s40560-022-00631-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-022-00631-6