Abstract
Kidney injury, including acute kidney injury (AKI) and chronic kidney disease (CKD), has become very common in critically ill patients treated in ICUs. Many epidemiological studies have revealed significant associations of AKI and CKD with poor outcomes of high mortality and medical costs. Although many basic studies have clarified the possible mechanisms of sepsis and septic AKI, translation of the obtained findings to clinical settings has not been successful to date. No specific drug against human sepsis or AKI is currently available. Remarkable progress of dialysis techniques such as continuous renal replacement therapy (CRRT) has enabled control of “uremia” in hemodynamically unstable patients; however, dialysis-requiring septic AKI patients are still showing unacceptably high mortality of 60–80 %. Therefore, further investigations must be conducted to improve the outcome of sepsis and septic AKI. A possible target will be remote organ injury caused by AKI. Recent basic studies have identified interleukin-6 and high mobility group box 1 (HMGB1) as important mediators for acute lung injury induced by AKI. Another target is the disease pathway that is amplified by pre-existing CKD. Vascular endothelial growth factor and HMGB1 elevations in sepsis were demonstrated to be amplified by CKD in CKD-sepsis animal models. Understanding the role of kidney injury as an amplifier in sepsis and multiple organ failure might support the identification of new drug targets for sepsis and septic AKI.
Similar content being viewed by others
Introduction
Sepsis is defined by the Surviving Sepsis Campaign Guideline 2012 (SSCG 2012) as the presence (probable or documented) of infection together with systemic manifestations of infection [1]. Serum creatinine, a widely measured renal function marker, includes the definition by SSCG 2012 as an organ dysfunction variable with a serum creatinine increase of >0.5 mg/dL. A recent acute kidney injury (AKI) definition by the Kidney Disease: Improving Global Outcomes (KDIGO) includes increase in serum creatinine by 0.3 mg/dL within 48 h. Therefore, sepsis and AKI will be observed frequently in critically ill patients in ICUs. In addition, sepsis and AKI synergistically increase the mortality of ICU patients. No specific drug against sepsis and AKI is clinically available. Chronic kidney disease (CKD), defined as glomerular filtration rate (GFR) <60 mL/min/1.73 m2 for 3 months, is increasing all over the world because of not only the greater prevalence of obesity, diabetes, and hypertension but also improved longevity. The prevalence of CKD in ICUs is also increasing. In fact, CKD has recently been recognized as an important risk factor for AKI development and poor outcomes in sepsis. Complication of kidney injury worsens critical illness. Better management for kidney injury will improve the outcomes of sepsis.
Review
Epidemiology of kidney injury in ICU
AKI is a serious complication in critically ill patients because AKI strongly affects outcomes such as mortality and medical costs [2–4]. Recently, the KDIGO has defined diagnostic criteria and severity staging for AKI (Table 1) [5]. A recent meta-analysis involving 154 studies of more than 3,000,000 individuals revealed that one in five adults and one in three children worldwide developed AKI during a hospital episode of care [6]. The overall incidence of AKI in ICU patients ranges from 20 to 50 %. The severity of AKI was significantly associated with mortality [7]. It is noteworthy that dialysis-requiring AKI in ICU shows the highest mortality. Recent data from the Nationwide Inpatient Sample show a rapid increase of the incidence of dialysis-requiring AKI during the past decade in the USA [8].
CKD has also been recognized as a public health problem because its incidence and prevalence continue to increase, entailing poor outcomes and high costs [9, 10]. CKD is defined by a decreased estimated glomerular filtration rate (eGFR) calculated with age, gender, and by serum creatinine concentration (Table 2). In Japan, one in eight adults is estimated to be complicated with CKD, which is well known to contribute strongly to cardiovascular disease and high mortality [11]. Moreover, CKD, along with sepsis, is an important risk factor for AKI development [12]. Actually, CKD is found in approximately 30 % of AKI patients in the ICU [13, 14]. Hsu and colleagues reported that the odds ratios of AKI development were elevated progressively from 1.95 to 40.07 for stage 3 (45 < eGFR < 60) through stage 5 CKD (eGFR < 15) patients compared to patients with stage 1 and 2 CKD (eGFR > 60) [15]. Several observational studies found that 0.9–6.8 % of all patients admitted to the ICU have a prior diagnosis of end-stage renal disease (ESRD) [16]. Although the incidence of non-dialysis CKD in ICU has been poorly investigated, the prevalence of CKD in the ICU is assumed to be much higher than that of ESRD.
Pathophysiology of septic acute kidney injury
AKI is a syndrome with a broad spectrum of etiologies, and several mechanisms including ischemic/hypoxic, nephrotoxic, and inflammatory insults contribute to AKI development (Fig. 1). Depending on different clinical settings such as post-cardiac surgery, contrast media exposure, severe heart failure with low output, and sepsis, pathophysiology and clinical features of AKI will be different. Among these etiologies, sepsis is the leading cause of AKI in ICUs [14]. Reportedly, 45–70 % of all AKI is associated with sepsis [17–19]. Patients with both sepsis and AKI are widely recognized as having an unacceptably high mortality rate [17, 20]. Bagshaw and colleagues reported that in-hospital and ICU mortalities of septic AKI were increased, respectively, to 30 and 20 % and that higher mortality was observed across all the AKI severity categories [20].
Pathophysiology of AKI. Three major areas of ischemia, inflammation, and direct toxic injury to the kidney contribute to the pathogenesis of AKI with significant overlap. Each mechanistic pathway identified by basic studies will be categorized into one of these major areas; however, some will lie simultaneously in two or three areas. Details are described in other review articles [71–73]. ROS reactive oxygen species, TLR toll-like receptor, HMGB1 high mobility group box 1, ABx antibiotics
Several pathophysiological mechanisms that are relatively specific for sepsis-induced AKI have been proposed (Table 3). Recent review articles discuss these mechanisms precisely [21–26], and a detailed description on this issue is beyond the aim of this review. Because of the complexity of sepsis and AKI, it should be noted that no single pathway can explain all the features of septic AKI. Each septic AKI patient moves along an individual disease trajectory. Therefore, the therapeutic targets vary with the underlying pre-existing conditions, time course, and disease trajectory of sepsis and AKI. Although many potential drug targets have been identified in animal models of sepsis and AKI, translation from animals to humans has been exceedingly difficult. The failure to translate results from animals to humans has been attributed to disease characteristics of sepsis and AKI (complexity and heterogeneity), inappropriate clinical trials, and animal models that do not fully mimic human sepsis [27].
Remote organ injury induced by acute kidney injury
Dialysis-requiring AKI shows unacceptably high mortality of 40–50 % [28], with mortality increasing to 60–80 % when associated with distant organ dysfunction such as cardiac and respiratory failure [29, 30]. Remarkable progress has taken place in renal replacement therapy (RRT) in critical care. Therefore, uremic conditions of hemodynamically unstable patients in ICU can be treated successfully using continuous RRT (CRRT) [31]. Nevertheless, dialysis has not decreased mortality appreciably [8, 28, 32]. Although AKI in the ICU is associated with a high mortality, factors other than loss of kidney function appear to contribute to poor outcomes: non-dialysis-requiring AKI patients show considerably higher mortality than ESRD patients show [33].
Based on these observations, many basic researchers have started to elucidate the mechanisms of distant organ dysfunction caused by AKI [34]. The most investigated distant organ is the lung. Respiratory failure, which is frequently observed in septic patients, is caused by vascular leakage and subsequent pulmonary edema. Volume overload caused by AKI amplifies lung injury, but it can be prevented by removing excess extracellular fluid [35]. However, several clinical studies have implicated inflammation in the pathogenesis of lung injury complicated with AKI. For instance, elevated blood levels of inflammatory mediators such as plasminogen activator inhibitor-1, interleukin-6 (IL-6), and soluble tumor necrosis factor receptors are observed in ARDS patients complicated with AKI compared with non-AKI [36].
Experimental studies using animal AKI models such as renal ischemia-reperfusion injury (IRI) and bilateral nephrectomy (BNx) have identified several different mechanisms by which AKI causes lung injury, including increased neutrophil infiltration, vascular permeability, dysregulation of salt and water transporters, and inflammatory cytokine and chemokine expressions [34, 37, 38]. Faubel and colleagues demonstrated that circulating IL-6 is a pathogenic mediator of lung injury in AKI [39, 40]. Toll-like receptor 4 (TLR4) plays fundamental roles in pathogen recognition and activation of innate immunity. TLR4 recognizes lipopolysaccharide (LPS), heparan sulfate, heat shock proteins, and high mobility group box 1 (HMGB1) [41]. Actually, HMGB1 has been shown to activate NF-κB by interacting with TLR4 on target cells [42]. BNx-induced lung injury characterized by neutrophil infiltration was partly reduced in TLR4-mutant C3H/HeJ mice, which is deficient in TLR4 signaling. Elevated blood HMGB1 levels were observed after BNx. Blockade of HMGB1 attenuated lung injury only in TLR4-wild type C3H/HeN mice. These observations suggest that TLR4–HMGB1 pathway contributes to lung injury induced by AKI (Fig. 2) [43].
Amplification of multiple organ failure by pre-existing kidney injury
Epidemiological studies of human sepsis have demonstrated the importance of pre-existing comorbid conditions including CKD [44, 45]. Reportedly, patients with CKD have increased risk of morbidity and mortality from sepsis [46–48], although limited data are available for non-dialysis CKD patients [49]. These findings suggest that sepsis and septic AKI in clinical settings are remarkably influenced by underlying CKD. Star and colleagues established two-stage mouse models of pre-existing renal disease with subsequent sepsis (CKD-sepsis) to mimic the complexity of human sepsis [50, 51]. CKD was induced by 5/6 nephrectomy (5/6Nx) or folic acid injection. Evidence of CKD as reduced GFR and pathological renal injury such as glomerular sclerosis and interstitial fibrosis was observed 2 or 4 weeks after. Then, these CKD animals were subjected to cecum ligation and puncture (CLP) surgery, the most widely used animal model of sepsis [52, 53], which induces polymicrobial bacteremia and sepsis because of needle puncture of the ligated cecum, causing leakage of fecal contents into the peritoneum.
These CKD-sepsis models showed remarkably high mortality with increased blood levels of vascular endothelial growth factor (VEGF) and HMGB1. Although sepsis induced by CLP alone increased these mediators, CKD-sepsis animals showed significantly higher levels than non-CKD-sepsis did. It must be addressed that the CKD condition caused mild but significant VEGF and HMGB1 elevations before sepsis induction and acute complete loss of renal function by BNx also caused VEGF and HMGB1 elevations in blood. Importantly, VEGF neutralization with soluble fms-like tyrosine kinase 1 (sFLT-1) (a soluble VEGF receptor) and HMGB1-neutralizing antiserum attenuated other organ injury including the liver and lungs and improved the survival of CKD-sepsis animals. Taken together, pre-existing renal injury amplifies sepsis disease progression and sepsis-induced AKI by increasing VEGF and HMGB1.
The pro-inflammatory cytokine HMGB1 secreted from dying cells induces the release of other cytokines from macrophages and other cell types [54–56]. HMGB1 can induce the additional release of HMGB1 in RAW 264.7 cells [57]. Therefore, HMGB1 seems to amplify inflammation by positive feedback. Several basic studies have demonstrated that HMGB1 neutralizing therapy improves mortality of sepsis in non-CKD mice [57–59]. This treatment would work well in CKD-sepsis, which shows a more severe form of sepsis. Can we translate these findings on HMGB1 into clinical terms? In vitro analysis revealed that surface-treated polyacrylonitrile (AN69ST), which is now clinically available in Japan, shows a high capacity to adsorb HMGB1 [60]. Further investigation is necessary to elucidate the role of HMGB1 in human sepsis complicated with CKD.
Perspectives for development of new treatment
Both sepsis and AKI have been recognized as a “graveyard for pharmaceutical companies” [61, 62] because no specific drug is currently available for these diseases in a clinical setting. Several new findings focusing on remote organ injury in AKI and amplification of septic reaction by CKD described above may suggest that humoral mediator removal would be effective in sepsis complicated with kidney injury. So far, efficient elimination of IL-6 and HMGB1 by blood purification technique has been reported. On the other hand, clinical trials that evaluated high-volume hemofiltration (HVHF) failed to show any protection even though HVHF could show significant removal of humoral mediators from the blood [63–65]. Another potential therapeutic strategy is mesenchymal stem cell (MSC) implantation. MSCs exhibit multiple beneficial properties by attenuating the inflammatory response, modulating immune cells, and promoting tissue healing [66–68]. MSCs are expected to home to sites of injury and use paracrine mechanisms to change the local environment to improve organ function and survival. Some study demonstrated the amelioration of sepsis-induced AKI by MSC administration [69, 70]. MSCs may be able to show their protective effects by regulating inflammatory cells and mediators with adaption to environmental changes induced by kidney injury complication.
Conclusions
Complications of acute and chronic kidney injury are associated significantly with poor outcomes of sepsis. Although many epidemiological studies have already demonstrated these associations, the precise mechanisms by which kidney injury has a significant impact on other organs in sepsis remain unclear. Understanding the role of kidney injury as an amplifier in sepsis and multiple organ failure might enable the identification of new drug targets for sepsis and septic AKI.
References
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637.
Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, et al. Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med. 2002;30:2051–8.
Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16:3365–70.
Mandelbaum T, Scott DJ, Lee J, Mark RG, Malhotra A, Waikar SS, et al. Outcome of critically ill patients with acute kidney injury using the Acute Kidney Injury Network criteria. Crit Care Med. 2011;39:2659–64.
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int. 2012; Suppl 2:1–138.
Susantitaphong P, Cruz DN, Cerda J, Abulfaraj M, Alqahtani F, Koulouridis I, et al. World incidence of AKI: a meta-analysis. Clin J Am Soc Nephrol. 2013;8:1482–93.
Srisawat N, Hoste EE, Kellum JA. Modern classification of acute kidney injury. Blood Purif. 2010;29:300–7.
Hsu RK, McCulloch CE, Dudley RA, Lo LJ, Hsu CY. Temporal changes in incidence of dialysis-requiring AKI. J Am Soc Nephrol. 2013;24:37–42.
Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–47.
Trivedi H. Cost implications of caring for chronic kidney disease: are interventions cost-effective? Adv Chronic Kidney Dis.17:265–70.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–305.
Kane-Gill SL, Sileanu FE, Murugan R, Trietley GS, Handler SM, Kellum JA. Risk factors for acute kidney injury in older adults with critical illness: a retrospective cohort study. Am J Kidney Dis. 2015;65:860–9.
Mehta RL, Pascual MT, Soroko S, Savage BR, Himmelfarb J, Ikizler TA, et al. Spectrum of acute renal failure in the intensive care unit: the PICARD experience. Kidney Int. 2004;66:1613–21.
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294:813–8.
Hsu CY, Ordonez JD, Chertow GM, Fan D, McCulloch CE, Go AS. The risk of acute renal failure in patients with chronic kidney disease. Kidney Int. 2008;74:101–7.
Bagshaw SM, Uchino S. End-stage kidney disease patients in the intensive care unit. Nephrol Dial Transplant. 2009;24:1714–7.
Neveu H, Kleinknecht D, Brivet F, Loirat P, Landais P. Prognostic factors in acute renal failure due to sepsis. Results of a prospective multicentre study. The French Study Group on Acute Renal Failure. Nephrol Dial Transplant. 1996;11:293–9.
Silvester W, Bellomo R, Cole L. Epidemiology, management, and outcome of severe acute renal failure of critical illness in Australia. Crit Care Med. 2001;29:1910–5.
Bagshaw SM, Laupland KB, Doig CJ, Mortis G, Fick GH, Mucenski M, et al. Prognosis for long-term survival and renal recovery in critically ill patients with severe acute renal failure: a population-based study. Crit Care. 2005;9:R700–9.
Bagshaw SM, George C, Bellomo R, Committee ADM. Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care. 2008;12:R47.
Zarjou A, Agarwal A. Sepsis and acute kidney injury. J Am Soc Nephrol. 2011;22:999–1006.
Zarbock A, Gomez H, Kellum JA. Sepsis-induced acute kidney injury revisited: pathophysiology, prevention and future therapies. Curr Opin Crit Care. 2014;20:588–95.
Parikh SM, Yang Y, He L, Tang C, Zhan M, Dong Z. Mitochondrial function and disturbances in the septic kidney. Semin Nephrol. 2015;35:108–19.
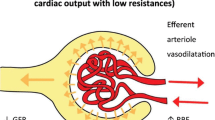
Prowle JR, Bellomo R. Sepsis-associated acute kidney injury: macrohemodynamic and microhemodynamic alterations in the renal circulation. Semin Nephrol. 2015;35:64–74.
Shum HP, Yan WW, Chan TM. Recent knowledge on the pathophysiology of septic acute kidney injury: a narrative review. J Crit Care. in press
Zafrani L, Payen D, Azoulay E, Ince C. The microcirculation of the septic kidney. Semin Nephrol. 2015;35:75–84.
Doi K, Leelahavanichkul A, Yuen PS, Star RA. Animal models of sepsis and sepsis-induced kidney injury. J Clin Invest. 2009;119:2868–78.
Wald R, McArthur E, Adhikari NK, Bagshaw SM, Burns KE, Garg AX, et al. Changing incidence and outcomes following dialysis-requiring acute kidney injury among critically ill adults: a population-based cohort study. Am J Kidney Dis. 2014;65:870–7.
Chao CT, Hou CC, Wu VC, Lu HM, Wang CY, Chen L, et al. The impact of dialysis-requiring acute kidney injury on long-term prognosis of patients requiring prolonged mechanical ventilation: nationwide population-based study. PLoS One. 2012;7, e50675.
Chertow GM, Christiansen CL, Cleary PD, Munro C, Lazarus JM. Prognostic stratification in critically ill patients with acute renal failure requiring dialysis. Arch Intern Med. 1995;155:1505–11.
Prowle JR, Bellomo R. Continuous renal replacement therapy: recent advances and future research. Nat Rev Nephrol. 2010;6:521–9.
Hsu RK, McCulloch CE, Ku E, Dudley RA, Hsu CY. Regional variation in the incidence of dialysis-requiring AKI in the United States. Clin J Am Soc Nephrol. 2013;8:1476–81.
Clermont G, Acker CG, Angus DC, Sirio CA, Pinsky MR, Johnson JP. Renal failure in the ICU: comparison of the impact of acute renal failure and end-stage renal disease on ICU outcomes. Kidney Int. 2002;62:986–96.
Grams ME, Rabb H. The distant organ effects of acute kidney injury. Kidney Int. 2012;81:942–8.
Schrier RW, Wang W. Acute renal failure and sepsis. N Engl J Med. 2004;351:159–69.
Liu KD, Glidden DV, Eisner MD, Parsons PE, Ware LB, Wheeler A, et al. Predictive and pathogenetic value of plasma biomarkers for acute kidney injury in patients with acute lung injury. Crit Care Med. 2007;35:2755–61.
Kramer AA, Postler G, Salhab KF, Mendez C, Carey LC, Rabb H. Renal ischemia/reperfusion leads to macrophage-mediated increase in pulmonary vascular permeability. Kidney Int. 1999;55:2362–7.
Rabb H, Wang Z, Nemoto T, Hotchkiss J, Yokota N, Soleimani M. Acute renal failure leads to dysregulation of lung salt and water channels. Kidney Int. 2003;63:600–6.
Ahuja N, Andres-Hernando A, Altmann C, Bhargava R, Bacalja J, Webb RG, et al. Circulating IL-6 mediates lung injury via CXCL1 production after acute kidney injury in mice. Am J Physiol Renal Physiol. 2012;303:F864–72.
Klein CL, Hoke TS, Fang WF, Altmann CJ, Douglas IS, Faubel S. Interleukin-6 mediates lung injury following ischemic acute kidney injury or bilateral nephrectomy. Kidney Int. 2008;74:901–9.
Medzhitov R. Toll-like receptors and innate immunity. Nat Rev Immunol. 2001;1:135–45.
Park JS, Svetkauskaite D, He Q, Kim JY, Strassheim D, Ishizaka A, et al. Involvement of toll-like receptors 2 and 4 in cellular activation by high mobility group box 1 protein. J Biol Chem. 2004;279:7370–7.
Doi K, Ishizu T, Tsukamoto-Sumida M, Hiruma T, Yamashita T, Ogasawara E, et al. The high mobility group box 1-Toll-like receptor 4 pathway contributes to the acute lung injury induced by bilateral nephrectomy. Kidney Int. 2014;86:316–26.
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10.
Guidet B, Aegerter P, Gauzit R, Meshaka P, Dreyfuss D, Group CU-RS. Incidence and impact of organ dysfunctions associated with sepsis. Chest. 2005;127:942–51.
James MT, Laupland KB, Tonelli M, Manns BJ, Culleton BF, Hemmelgarn BR, et al. Risk of bloodstream infection in patients with chronic kidney disease not treated with dialysis. Arch Intern Med. 2008;168:2333–9.
Naqvi SB, Collins AJ. Infectious complications in chronic kidney disease. Adv Chronic Kidney Dis. 2006;13:199–204.
Thamer M, Ray NF, Fehrenbach SN, Richard C, Kimmel PL. Relative risk and economic consequences of inpatient care among patients with renal failure. J Am Soc Nephrol. 1996;7:751–62.
Dalrymple LS, Go AS. Epidemiology of acute infections among patients with chronic kidney disease. Clin J Am Soc Nephrol. 2008;3:1487–93.
Leelahavanichkul A, Huang Y, Hu X, Zhou H, Tsuji T, Chen R, et al. Chronic kidney disease worsens sepsis and sepsis-induced acute kidney injury by releasing high mobility group box protein-1. Kidney Int. 2011;80:1198–211.
Doi K, Leelahavanichkul A, Hu X, Sidransky KL, Zhou H, Qin Y, et al. Pre-existing renal disease promotes sepsis-induced acute kidney injury and worsens outcome. Kidney Int. 2008;74:1017–25.
Buras JA, Holzmann B, Sitkovsky M. Animal models of sepsis: setting the stage. Nat Rev Drug Discov. 2005;4:854–65.
Deitch EA. Rodent models of intra-abdominal infection. Shock. 2005;24 Suppl 1:19–23.
Andersson U, Wang H, Palmblad K, Aveberger AC, Bloom O, Erlandsson-Harris H, et al. High mobility group 1 protein (HMG-1) stimulates proinflammatory cytokine synthesis in human monocytes. J Exp Med. 2000;192:565–70.
Scaffidi P, Misteli T, Bianchi ME. Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Nature. 2002;418:191–5.
Yang H, Wang H, Czura CJ, Tracey KJ. The cytokine activity of HMGB1. J Leukoc Biol. 2005;78:1–8.
Qin S, Wang H, Yuan R, Li H, Ochani M, Ochani K, et al. Role of HMGB1 in apoptosis-mediated sepsis lethality. J Exp Med. 2006;203:1637–42.
Yang H, Ochani M, Li J, Qiang X, Tanovic M, Harris HE, et al. Reversing established sepsis with antagonists of endogenous high mobility group box 1. Proc Natl Acad Sci U S A. 2004;101:296–301.
Wang H, Bloom O, Zhang M, Vishnubhakat JM, Ombrellino M, Che J, et al. HMG-1 as a late mediator of endotoxin lethality in mice. Science. 1999;285:248–51.
Yumoto M, Nishida O, Moriyama K, Shimomura Y, Nakamura T, Kuriyama N, et al. In vitro evaluation of high mobility group box 1 protein removal with various membranes for continuous hemofiltration. Ther Apher Dial. 2011;15:385–93.
Riedemann NC, Guo RF, Ward PA. Novel strategies for the treatment of sepsis. Nat Med. 2003;9:517–24.
Jo SK, Rosner MH, Okusa MD. Pharmacologic treatment of acute kidney injury: why drugs haven’t worked and what is on the horizon. Clin J Am Soc Nephrol. 2007;2:356–65.
Clark E, Molnar AO, Joannes-Boyau O, Honore PM, Sikora L, Bagshaw SM. High-volume hemofiltration for septic acute kidney injury: a systematic review and meta-analysis. Crit Care. 2014;18:R7.
Joannes-Boyau O, Honore PM, Perez P, Bagshaw SM, Grand H, Canivet JL, et al. High-volume versus standard-volume haemofiltration for septic shock patients with acute kidney injury (IVOIRE study): a multicentre randomized controlled trial. Intensive Care Med. 2013;39:1535–46.
Borthwick EM, Hill CJ, Rabindranath KS, Maxwell AP, McAuley DF, Blackwood B. High-volume haemofiltration for sepsis. Cochrane Database Syst Rev. 2013;1, CD008075.
Wannemuehler TJ, Manukyan MC, Brewster BD, Rouch J, Poynter JA, Wang Y, et al. Advances in mesenchymal stem cell research in sepsis. J Surg Res. 2012;173:113–26.
Kusadasi N, Groeneveld AB. A perspective on mesenchymal stromal cell transplantation in the treatment of sepsis. Shock. 2013;40:352–7.
Ho MS, Mei SH, Stewart DJ. The immunomodulatory and therapeutic effects of mesenchymal stromal cells for acute lung injury and sepsis. J Cell Physiol. 2015;230:2606–17.
Nemeth K, Leelahavanichkul A, Yuen PS, Mayer B, Parmelee A, Doi K, et al. Bone marrow stromal cells attenuate sepsis via prostaglandin E(2)-dependent reprogramming of host macrophages to increase their interleukin-10 production. Nat Med. 2009;15:42–9.
Luo CJ, Zhang FJ, Zhang L, Geng YQ, Li QG, Hong Q, et al. Mesenchymal stem cells ameliorate sepsis-associated acute kidney injury in mice. Shock. 2014;41:123–9.
Schrier RW, Wang W, Poole B, Mitra A. Acute renal failure: definitions, diagnosis, pathogenesis, and therapy. J Clin Invest. 2004;114:5–14.
Bonventre JV, Yang L. Cellular pathophysiology of ischemic acute kidney injury. J Clin Invest. 2011;121:4210–21.
Molitoris BA. Therapeutic translation in acute kidney injury: the epithelial/endothelial axis. J Clin Invest. 2014;124:2355–63.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author declares that he has no competing interests.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Doi, K. Role of kidney injury in sepsis. j intensive care 4, 17 (2016). https://doi.org/10.1186/s40560-016-0146-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-016-0146-3