Abstract
Background
Pharmacist’s involvement in optimizing medication adherence among diabetic patients has been implemented for over a decade. Diabetes Medication Therapy Adherence Clinic (DMTAC) was set up to educate diabetic patients, monitor treatment outcomes, and manage drug-related problems. While evidence shows that pharmacist-led DMTAC was effective in reducing HbA1c, there was limited data regarding the impact of different intervention types and default to follow-up on glycemic control.
Aim
To assess the impact DMTAC on glycemic control and the difference in glycemic control between hospital and health clinic settings as well as defaulter and non-defaulter. In addition, the impact of pharmacist’s interventions, DMTAC follow-up frequencies, and duration of diabetes on glycemic control were also determined.
Methods
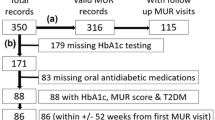
A retrospective study was conducted among diabetes patients under DMTAC care between January 2019 and June 2020 in five hospitals and 23 primary health clinics. Patients’ demographics data, treatment regimens, frequencies of DMTAC visits, defaulter (absent from DMTAC visits) and types of pharmacists’ intervention were retrieved from patients’ medical records and electronic database. HbA1c was collected at baseline, 4–6 months (post-1), and 8–12 months (post-2).
Results
We included 956 patients, of which 60% were females with a median age of 58.0 (IQR: 5.0) years. Overall, the HbA1c reduced significantly from baseline (median: 10.2, IQR: 3.0) to post-1 (median: 8.8, IQR: 2.7) and post-2 (median: 8.3, IQR: 2.6%) (p < 0.001). There were 4317 pharmacists’ interventions performed, with the majority being dosage adjustment (n = 2407, 55.8%), followed by lab investigations (849, 19.7%), drugs addition (653, 15.1%), drugs discontinuation (408, 9.5%). Patients treated in hospitals received significantly more interventions than those treated in primary health clinics (p < 0.001). We observed significantly less reduction in HbA1c in DMTAC follow-up defaulters than non-defaulters after 1 year (− 1.02% vs. − 2.14%, p = 0.001). Frequencies of DMTAC visits (b: 0.19, CI: 0.079–0.302, p = 0.001), number of dosage adjustments (b: 0.83, CI: 0.015–0.151, p = 0.018) and number of additional drugs recommended (b: 0.37, CI: 0.049–0.691, p = 0.024) had positive impact on glycemic control whereas duration of diabetes (b: − 0.0302, CI: − 0.0507, − 0.007, p = 0.011) had negative impact.
Conclusion
Glycemic control improved significantly and sustained up to one year among patients in pharmacists-led DMTAC. However, DMTAC defaulters experienced poorer glycemic control. Considering more frequent visits and targeted interventions by pharmacists at DMTAC resulted in improved HbA1c control, these strategies should be taken into account for future program planning.
Similar content being viewed by others
Background
Diabetes is a global public health concern and one of the top ten causes of mortality worldwide [1]. According to International Diabetes Federation (IDF), there is a continual increase in diabetes prevalence globally, with an estimated 537 million adults living with diabetes in 2021; more than 75% were from low and middle-income countries [2]. Diabetes was associated with an increased risk of mortality due to complications from infections, cardiovascular disease, stroke, and chronic kidney disease and accounted for more than 6.7 million deaths in 2021 [2]. In Malaysia, the prevalence of diabetes in the adult population was 18.3% in 2019, which amounted to 3.9 million adults living with diabetes [3].
Most diabetes patients receive treatment in primary and tertiary care institutions in Malaysia. A multidisciplinary team approach has long been proven effective in improving diabetes health outcomes [4]. Over the years, pharmacists’ roles have expanded beyond the traditional screening, filling, and dispensing roles. Specifically, pharmacists play an integral role in diabetes management, as they are one of the most accessible healthcare professionals in the primary care setting.
In a study conducted in a community setting in the United States, pharmacist education and interventions resulted in a 1.3% decrease in glycosylated hemoglobin (HbA1c) [5]. Meanwhile, in a similar setting in Australia, a more significant proportion of diabetic patients achieve HbA1c < 7% following a 9-month intervention period by pharmacists compared to the control group. In addition to HbA1c reduction, patients' well-being and adherence improved [6]. A meta-analysis further consolidates the evidence that pharmacists’ interventions could improve HbA1c, blood pressure, and body mass index (BMI) in diabetic patients [7].
Since 2006, a diabetic outpatient program called Diabetes Medication Therapy Adherence Clinic (DMTAC) has been run by pharmacists in hospitals and health clinics in Malaysia. DMTAC pharmacists must undergo a structured training program within the Ministry of Health Malaysia before providing services. Patients enrolled in the service are required to visit the pharmacists at an average interval of one month for medication and disease education, treatment outcome monitoring, identification, and management of drug-related problems [8].
Previous local studies had reported positive outcomes in pharmacists-led DMTAC service. In the Penang state of Malaysia, a study by Lim et al. reported a mean HbA1c reduction of 1.73% and fasting plasma glucose (FPG) improvement of 2.65 mmol/L following the completion of 8 DMTAC visits in a tertiary hospital [9]. Another study in a university hospital reported HbA1c reduction from 9.66% to 8.47% in patients who received pharmacist interventions [10]. Significant HbA1c reductions were also observed among patients in district hospitals after one-year follow-up in a pharmacist-led diabetes program [11]. Moreover, the multi-center retrospective study that involved 14 health clinics in Malaysia showed 1% reduction in HbA1c among 56 type 2 diabetes mellitus patients [12].
Although several studies observed HbA1c reduction in patients with diabetes undergoing DMTAC program, most were conducted either in hospital or primary health clinic settings. Hence, there was a lack of evidence on the glycemic outcome among DMTAC patients in hospital as compared to primary health clinic settings. Moreover, data was limited regarding the types of intervention performed by pharmacists, frequency of DMTAC visits, and default rate. In this study, we aimed to evaluate the impact of DMTAC on glycemic control and the difference in glycemic control between hospitals and primary health clinics as well as between defaulter and non-defaulters. We also aimed to determine the impact of pharmacist’ interventions, the frequency of DMTAC visits and duration of diabetes on glycemic control among diabetic patients.
Methods
This multicenter, retrospective study was conducted in all public healthcare facilities within the state of Penang, Malaysia, including five hospitals and 23 primary health clinics. This study was registered in National Medical Research Registry (NMRR-20-414-53115) and obtained ethical approval from the Medical Research Ethnics Committee, Ministry of Health Malaysia. All patients under the care of the Diabetes Medication Therapy Adherence Clinic (DMTAC) between January 2019 to June 2020 in the selected study sites were screened for eligibility. We included patients with diabetes mellitus aged 18 years and above recruited into DMTAC and excluded pregnant women, patients with end stage renal failure (eGFR < 15 mL/min/m2) and those with missing data.
DMTAC was operated based on Diabetes Medication Therapy Adherence Protocol by Pharmaceutical Services Division, Ministry of Health Malaysia [8]. The insulin titration or dose adjustment was performed based on Practical Guide to Insulin Therapy in Type 2 Diabetes Mellitus and Clinical Practice Guideline Management of Type 2 Diabetes Mellitus [13, 14]. Several interventions were undertaken within the DMTAC, encompassing medication initiation or discontinuations, dosage adjustments, and recommendations for laboratory investigations. Notably, the pharmacists were granted authorization by the physicians to carry out insulin dosage adjustments during the DMTAC sessions that occurred between the physicians' follow-up visits, while other interventions took place during the regular physician appointments.
DMTAC pharmacists routinely documented patients’ medical, social, and family histories, drug-related issues, interventions, laboratory data, treatment regimens, and adherence using the Malaysian Medication Adherence Tool (MyMAAT) score within the Pharmacy Information System (PhIS), an electronic database. The retrospective study data were retrieved from the patient medical records and the (PhIS). Patients' demographic information, treatment regimens, types of healthcare facilities, frequencies of DMTAC visits, default to follow-up rates, and details of pharmacists’ interventions, including recommendations to add or discontinue medications, dosage adjustments, and suggestions for laboratory investigations, were collected and recorded in a standardized electronic data collection form.
Default to follow-up was defined as absence in all DMTAC follow-ups between physician’s follow-ups, where patients only met DMTAC pharmacists during the doctor’s follow-up. The primary outcome was HbA1c level and were collected at baseline, 4–6 months (post-1), and 8–12 months (post-2). The secondary outcomes were the difference in HbA1c between diabetic patients in hospital and primary health clinic settings, difference in HbA1c between defaulter and non-defaulter and the impact of pharmacist’ interventions, the frequency of DMTAC visits, and duration of diabetes on HbA1c.
Convenience sampling with proportionate representation was utilized in this retrospective study. Patients were selected based on their availability in medical records, and a higher number of subjects were included from sites with larger patient populations. The sample size was determined using PS software version 3.1.6, employing a one-sided paired Z-test. A significance level (alpha) of 0.05 and a power of 0.9 were assumed. The data were expected to follow a normal distribution with a standard deviation of 1.7 [12]. Based on an estimated difference in mean HbA1c of 0.5%, a sample size of 123 patients was calculated to be required to reject the null hypothesis. Considering an anticipated dropout rate of 20%, a total sample size of 148 patients was derived. The chosen Type I error probability for this test of the null hypothesis was 0.05.
The data were analyzed using IBM Statistical Package for Social Sciences (SPSS) software Version 16.0. Data in categorical values were presented in frequency and analyzed using Chi-square. The HbA1c data was not normally distributed for all patients and comparison between hospitals and primary health clinics. Hence, Wilcoxon signed rank test and Mann–Whitney U test were used for within and between groups comparison respectively. Meanwhile, paired t-tests and independent t-tests were used for within and between groups comparison for the HbA1c data for defaulter and non-defaulters as the data was normally distributed. The relationship between difference in HbA1c and number of DMTAC visits, pharmacist’ interventions and duration of diabetes were analyzed using linear regression analysis. Results were significant if p-values were less than 0.05.
Results
956 subjects were analyzed, including 395 from hospitals and 561 from health clinics. The median age of the patients was 58 years old (IQR: 15), with 574 females (60.0%) and 407 Malays (42.6%). Compared to health clinics, hospital patients missed more DMTAC appointments (21.8% vs. 12.3%, p < 0.001). However, significantly more pharmacists’ interventions were performed in hospitals compared to health clinics (median 5.0 vs. 3.0, p < 0.001).
819 patients had dyslipidemia (85.7%), followed by 748 with hypertension (78.2%), 184 with cardiovascular disease (19.2%), 253 with neuropathy (26.5%), 227 with nephropathy (23.7%) and 202 with retinopathy (21.1%).
781 patients (81.7%) recruited in DMTAC had insulin treatment. The proportion of patients who received at least one type of insulin at health clinics (87.5%) was higher than those in hospitals (72.7%). Meanwhile, patients who visited hospitals received more interventions than those in health clinics [hospital median: 5 (IQR: 4), health clinics median: 3 (IQR: 5), p < 0.001] (Table 1).
HbA1c reduced significantly among patients recruited in DMTAC in hospitals and health clinics from baseline to post 1 and post 2 (Fig. 1). However, there was no significant difference in HbA1c improvement between hospitals and health clinics from baseline to post 1 (− 1.1% vs. − 1.4%, p = 0.062) and baseline to post 2 (− 1.5% vs. 2.0%, p = 0.058), respectively.
At baseline, there was no difference in HbA1c between defaulters and non-defaulters (11.1 vs. 10.7, p = 0.226) (Fig. 2). In post 1, HbA1c improved significantly from baseline (− 1.63%, p < 0.001) among non-defaulters, and there was no significant difference among defaulters (− 0.57%, p = 0.05). In post 2, even though HbA1c reduced significantly among defaulters from baseline (− 1.02%, p = 0.006), non-defaulters had a significantly higher magnitude of improvement (− 2.14, p = 0.001) (Fig. 2). Other factors like gender, race, type of regimen, and type of facilities were not significantly associated with HbA1c reduction.
HBAIC differences at baseline, post-1, and post-2 between defaulters and non-defaulters. Data that was normally distributed was presented in Mean ± SD. aAnalysis using paired t-test and not significantly different, p > 0.05. bAnalysis using paired t-test and significantly different, p < 0.05. cAnalysis using independent t-test and not significantly different, p = 0.226. dAnalysis using independent t-test and significantly different, p = 0.001
Out of the four types of interventions performed by DMTAC pharmacists, dosage adjustment was the most commonly suggested (55.8%), followed by lab investigations recommendations (19.7%), adding medications (15.1%) and medications discontinuation (9.5%) (Table 2).
In the multiple linear regression model, frequencies of DMTAC visits from baseline to post 1 (b = 0.19, CI: 0.079–0.302, p = 0.001) and duration of DM (b = − 0.0302, CI: − 0.0507 to − 0.007, p = 0.011) were predicting factors of HbA1C reduction from baseline to post 1. The final model equation was: HbA1C reduction from baseline to post 1 = 1.15 + (0.19 × number of MTAC visit) − (0.032 × duration of diabetes), R2 = 0.042.
The frequencies of DMTAC visits did not predict HBAIC reduction from baseline to post 2 (p = 0.056). However, the number of dosage adjustments and the addition of anti-diabetic agent were associated with HbA1c differences from baseline to post 2 (Table 3). The final model equation was: HBAIC reduction from baseline to post 2 = 1.618 + (0.83 × number of dosage adjustment) + (0.37 × number of addition of antidiabetic agent), R2 = 0.040.
Discussion
This study revealed a significant HbA1c reduction among diabetic patients after DMTAC visits. This was in line with two small-scale Malaysian studies conducted in a health clinic and a tertiary hospital, which demonstrated a smaller degree but significant HbA1c reduction [15, 16]. Within expectations, we observed that patients who did not default from follow-up achieved a significantly lower level of HbA1c in both time points than defaulters. Several other factors, such as the frequencies of DMTAC visits, duration of diabetes, number of dosage adjustments, and antidiabetic agents were identified as independent predictors of HbA1c levels.
Overall, improvement in HbA1c was observed among all the subjects, including the defaulters, from baseline until post-2, which was up to a year. Several studies reported similar findings. A study in three internal medicine clinics in Northeast Ohio showed a significant reduction in HbA1c in the pharmacist-led diabetes management group compared to the usual physician care group 6 months post-index [17]. This corresponded with a randomized clinical trial in the United States showing a significant reduction of 2.5% in HbA1c over 12 months of pharmacists’ care [18]. While the effectiveness of pharmacist-led diabetes mellitus management was unequivocally demonstrated, we further investigated different system and patient-related factors which predicted its effectiveness denominated by HbA1c level, which was not widely reported in the literature.
Notably, there was a significant difference in HbA1c reduction between DMTAC defaulters and non-defaulters. Patients who adhered to DMTAC follow-up were more likely to experience a greater magnitude of HbA1c reduction. Surprisingly, there was limited literature regarding the impact of adherence to diabetes clinic follow-up schedules on HbA1c levels. Two studies in the 1980s and 1990s reported that patients who defaulted to diabetes clinic follow-up had significantly poorer control of HbA1c and developed more vascular-related complications [19, 20]. A recent study consolidated those findings, further explaining the reasons for defaulting follow-up in diabetes clinics [21]. The most common reason for defaulting was multiple clinics and forgetting appointments due to other comorbidities [21]. In this study, eight out of ten patients had hypertension and dyslipidemia, while two out of five had at least one macro or microvascular diseases. This could indicate the need to treat diabetic patients with a more holistic and multidisciplinary approach by combining different clinics and reducing the number of follow-ups. The applicability of other approaches such as phone-call education, flexi-hours clinics, web-based virtual counselling, and digital self-monitoring applications should be examined to minimize default among diabetic patients.
While there was no difference in glycemic control between patients who visited DMTAC in hospitals and primary health clinics, we observed a higher default rate in hospital patients. This was similar to a previous local study, despite we observed a lower degree of differences [22]. In Malaysia, public hospitals are located in cities, while public health clinics are scattered to provide broad coverage of healthcare services, including rural areas [23]. Hence, primary health clinics are generally more accessible compared to hospitals. Furthermore, hospitals have a higher patient load and may require a longer waiting time than primary health clinics [24]. Considering the higher default rate in hospitals, there is a potential need to discharge patients with controlled HbA1c from hospitals to primary health care based on a set of pre-determined criteria [25]. It is therefore critical to strengthen primary health care through upgrading basic infrastructures and human resources, improve training and capacity of primary care staff, integrating hospital and primary care and enhancing community-based care to optimize its utilization among diabetes patients [26].
We further analyzed the predictors that led to HbA1c reduction. During the first phase of DMTAC follow-up (four to six months post-recruitment), more frequent DMTAC visits had a positive impact on glycemic control, whereas a longer duration of diabetes produced negative impact. Patients with a longer duration of diabetes exhibited poorer HbA1c control, which may be attributed to factors such as disease progression, cumulative metabolic effects, and the potential development of complications over time [27]. An increase in the frequencies of DMTAC visits enabled pharmacists to monitor patients’ responses more closely and hence optimize their antidiabetic regimen timely. Nevertheless, our findings contradict previous reports. Two local studies and a Japanese study revealed that patients who underwent intensive and less-intensive follow-ups demonstrated a similar level of glycemic control [12, 28, 29]. Interestingly, we did not observe such an impact in the second phase (eight to twelve months post-recruitment) of DMTAC follow-up. Taken together, more intensive follow-ups at the initial six months may benefit the patients and could be tapered down once the patients are stabilized to optimize human resources and treatment costs.
On the other hand, optimization of diabetic treatment significantly improved glycemic control in the longer time horizon of DMTAC follow-up. We found that pharmacists-led interventions, particularly dosage adjustment and the addition of antidiabetic agents, contributed significantly to HbA1c reduction. Our findings were substantiated by a randomized controlled trial in the primary health settings, which involved pharmacist-led dosage adjustment, drug-related problem detections, and alteration of medication regimen [30]. Javaid et al. reported that patients who received those interventions demonstrated better glycemic, blood pressure, and lipid control [26]. Diabetes treatment involves complex algorithms and regimens, necessitating individualized treatment plans, especially when involved insulin [31]. This was tested in another randomized control trial, where subjects on insulin treatment achieved superior glycemic control when they received intervention comprised of digital system integration in a blood glucose measuring device, which assists health providers in timely insulin dose adjustment [32]. The efficacy and feasibility of such a technologies-driven model warrant further investigation among diabetic patients in local settings.
To our best knowledge, this was the first real-world study that evaluated system and patient-related factors, including frequencies of follow-up, default rate, types of facilities, and interventions that was associated with improvement in glycemic control. This study has a few limitations. Due to the retrospective design, causality establishment was not warranted. Although patients were followed up for up to one year in our study, the longer-term efficacy of the DMTAC service remains uncertain. Therefore, future studies should investigate the impact of such programs on patients’ self-care behaviors and assess glycemic improvement over extended periods to evaluate the sustainability of the observed benefits. Further research investigating the factors and consequences of defaulting on diabetic clinics is warranted, specifically exploring tangible health outcomes beyond surrogate markers such as glycemic control.
Conclusion
DMTAC services led to significant improvements in glycemic control across all subgroups. Default rate was higher in hospitals, and defaulters demonstrated poorer HbA1c control. More frequent DMTAC visits and specific pharmacist interventions resulted in improved glycemic control. However, the different roles of these predictors across the two DMTAC follow-up phases suggest the benefits of intensive early follow-up and tailoring medication regimens according to individual needs in long-term diabetes management. The findings underscore the vital role of pharmacists in diabetes care and offer guidance to policymakers for determining key performance indicators in DMTAC.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to confidentiality of patients, but are available from the corresponding author on reasonable request.
References
GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Lond Engl. 2016;388:1659–724.
International Diabetes Federation. International Diabetes Federation Diabetes Atlas.
National Health and Morbidity Survey. Institute for Public Health, Ministry of Health Malaysia; 2019.
Siaw MYL, Lee JY-C. Multidisciplinary collaborative care in the management of patients with uncontrolled diabetes: a systematic review and meta-analysis. Int J Clin Pract. 2019;73:e13288.
Meade LT, Tart RC, Buzby HL. Evaluation of diabetes education and pharmacist interventions in a rural, primary care setting. Diabetes Spectr Publ Am Diabetes Assoc. 2018;31:90–5.
Armour CL, Taylor SJ, Hourihan F, Smith C, Krass I. Implementation and evaluation of Australian pharmacists’ diabetes care services. J Am Pharm Assoc JAPhA. 2004;44:455–66.
van Eikenhorst L, Taxis K, van Dijk L, de Gier H. Pharmacist-led self-management interventions to improve diabetes outcomes. A systematic literature review and meta-analysis. Front Pharmacol. 2017;8:891.
Protocol Medication Therapy Adherence Clinic: Diabetes. Pharmaceutical Services Division, Ministry of Health Malaysia; 2014.
Lim PC, Lim K. Evaluation of a pharmacist-managed Diabetes Medication Therapy Adherence Clinic. Pharm Pract. 2010;8:250–4.
Butt M, Mhd Ali A, Bakry MM, Mustafa N. Impact of a pharmacist led diabetes mellitus intervention on HbA1c, medication adherence and quality of life: a randomised controlled study. Saudi Pharm J SPJ. 2016;24:40–8.
Tiang Lau B, Zulaikha Ismail S, Yen Ng S, Mohmmad N. Impact of pharmacist-led diabetes program on glycated hemoglobin and diabetes-related hospitalizations in a district-level hospital: a pilot retrospective cohort study. Int J Adv Life Sci Res. 2018;1:26–36.
Lee XY, Selvadurai S, Cheah KY, Noh NB, Gan CB, Teng J, Hamdi AH, Haron N. Impact of pharmacist-managed Diabetes Medication Therapy Adherence Clinic (DMTAC) in government health clinics. Malays J Pharm Sci. 2015;13(1):43–51.
Ministry of Health Malaysia. Clinical Practice Guideline: Practical Guide to Insulin Therapy in Type 2 Diabetes Mellitus. Ministry of Health Malaysia. Kuala Lumpur, Malaysia. 2011.
Ministry of Health Malaysia. Clinical Practice Guideline Management of Type 2 Diabetes Mellitus. Ministry of Health Malaysia. 6th Edition. Kuala Lumpur, Malaysia. 2021.
Abdullah MJ, Tew MM, Tan PH, Koh JH, Osman NM, Chan HK. Pharmacist-managed diabetes clinic in Malaysia—does the number of follow-up visits really matter? J Pharm Pract Community Med. 2018;4:55–9.
Alison C, Anselm S. The effectiveness of Diabetes Medication Therapy Adherence Clinic to improve glycaemic control among patients with type 2 diabetes mellitus: a randomised controlled trial. Med J Malaysia. 2020;75:246–53.
Pontefract BA, King BS, Gothard DM, King CA. Impact of pharmacist-led diabetes management in primary care clinics. Innov Pharm. 2018;9:1–8.
Rothman RL, Malone R, Bryant B, Shintani AK, Crigler B, Dewalt DA, et al. A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. Am J Med. 2005;118:276–84.
Hammersley MS, Holland MR, Walford S, Thorn PA. What happens to defaulters from a diabetic clinic? Br Med J Clin Res Ed. 1985;291:1330–2.
Archibald LK, Gill GV. Diabetic clinic defaulters—who are they and why do they default? Pract Diabetes Int. 1992;9:13–4.
Defaulters PS. Are they worse off? Analysing reasons for this phenomenon amongst patients with diabetes with and without HIV infection. J Endocrinol Metab Diabetes South Afr. 2020;25:70–9.
Abdullah F, Han TM, Md Aris MA, Osman IF. Charateristics and reasons for diabetic-defaulters between primary care clinics and diabetic specialist clinic: a prospective cohort study in Kuantan, Malaysia. IIUM Med J Malays. 2016;15.
Ariff KM, Teng CL. Rural health care in Malaysia. Aust J Rural Health. 2002;10:99–103.
Pillay DIMS, Ghazali RJDM, Manaf NHA, Abdullah AHA, Bakar AA, Salikin F, et al. Hospital waiting time: the forgotten premise of healthcare service delivery? Int J Health Care Qual Assur. 2011;24:506–22.
Umpierrez GE, Reyes D, Smiley D, Hermayer K, Khan A, Olson DE, et al. Hospital discharge algorithm based on admission HbA1c for the management of patients with type 2 diabetes. Diabetes Care. 2014;37:2934–9.
Freijser L, Annear P, Tenneti N, Gilbert K, Chukwujekwu O, Hazarika I, et al. The role of hospitals in strengthening primary health care in the Western Pacific. Lancet Reg Health West Pac. 2023;33: 100698.
Haghighatpanah M, Nejad ASM, Haghighatpanah M, Thunga G, Mallayasamy S. Factors that correlate with poor glycemic control in type 2 diabetes mellitus patients with complications. Osong Public Health Res Perspect. 2018;9(4):167–74. https://doi.org/10.24171/j.phrp.2018.9.4.05.
Beh YS, Gopalsamy K, Lee SLF, Vengadasalam VPP. Impact of Diabetes Medication Therapy Adherence Clinic (DMTAC) appointment intervals on glycemic control in public health clinics across Perak, Malaysia. Malays Fam Physician. 2022;17:105–13.
Ukai T, Ichikawa S, Sekimoto M, Shikata S, Takemura Y. Effectiveness of monthly and bimonthly follow-up of patients with well-controlled type 2 diabetes: a propensity score matched cohort study. BMC Endocr Disord. 2019;19:43.
Javaid Z, Imtiaz U, Khalid I, Saeed H, Khan RQ, Islam M, et al. A randomized control trial of primary care-based management of type 2 diabetes by a pharmacist in Pakistan. BMC Health Serv Res. 2019;19:409.
Chun J, Strong J, Urquhart S. Insulin initiation and titration in patients with type 2 diabetes. Diabetes Spectr. 2019;32:104–11.
Bergenstal RM, Johnson M, Passi R, Bhargava A, Young N, Kruger DF, et al. Automated insulin dosing guidance to optimise insulin management in patients with type 2 diabetes: a multicentre, randomised controlled trial. The Lancet. 2019;393:1138–48.
Acknowledgements
We would like to thank the Director General of Health Malaysia for his approval to publish this article. Appreciation extended to all DMTAC pharmacists in Penang. Penang Pharmaceutical Services Division and the endocrinologists, family medicine specialists and doctors for their support to DMTAC programme.
Funding
This was a self-funded study.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this work including conceptualization, data curation, writing and review of manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was registered in the National Medical Research Registry (NMRR ID-20-414-53115) and approved by Medical Research Ethical Committee [KKM/NIHSEC/P20-604(6)]. All research procedures were conducted according to the Malaysian Guidelines Good Clinical Practice (4th edition) and other relevant guidelines for research.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lim, P.C., Tan, H.H., Mohd Noor, N.A. et al. The impact of pharmacist interventions, follow-up frequency and default on glycemic control in Diabetes Medication Therapy Adherence Clinic program: a multicenter study in Malaysia. J of Pharm Policy and Pract 16, 83 (2023). https://doi.org/10.1186/s40545-023-00583-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40545-023-00583-8