Abstract
In 2021, the International Diabetes Federation (IDF) reported that the prevalence of diabetes in Pakistan was 9.6%, higher than the global average. However, adherence to treatment guidelines, e.g., American Diabetes Association and Pakistan Endocrine Society and prescription patterns for Oral anti-diabetes (OAD), is poorly understood in Pakistan. Therefore, this study aimed to examine the prescribing practices of anti-diabetic medications, an association of lifestyle modification with drugs prescribed, and their effectiveness in preserving ideal glycemic levels in diabetic patients undergoing treatment in tertiary care teaching hospitals in rural and urban Pakistan. In this cross-sectional study, data were collected from prescriptions of outpatient diabetic patients from different rural and urban tertiary care hospitals between October 2021 and February 2022. 388 participants were enrolled in the study for a detailed interview on prescription evaluation and glycemic control. The coinvestigators conducted an interview with the patient and used a pre-validated questionnaire to collect the data. The relationship between following treatment guidelines and clinical and demographic factors was found using chi-square tests for bivariate analyses. The study reported that out of 388, the mean ages of the patients were 48 ± 12.4, and the majority were female. It was observed that 60.1% and 66.5% have uncontrolled fasting and random blood glucose, respectively. The education level of the study participants was also below par to have a complete understanding of the medical condition and self-management therapy. Even though they were taking the right medications—an average prescription regimen included 5.08 medications—52.1% of the studied people had glycated haemoglobin (HbA1c) levels higher than the therapeutic threshold set by the International Diabetes Federation. In this modern era, it was observed that the prescribing trend was still focused on traditional therapeutic options Biguanides, sulfonylureas, and dipeptidyl peptidase-4 inhibitors were prescribed in 64.6% of the patients. A significant association was found between glycemic control and body mass index, adherence to lifestyle modifications, and the number of medications prescribed (p-value < 0.05). The study reveals that Pakistan's prescribing practices do not align with international and national guidelines, leading to a high prevalence of uncontrolled diabetes and widespread use of polypharmacy among patients. To address this issue, policymakers should prioritize establishing a comprehensive national diabetes action plan. Additionally, there is a pressing need to develop diabetes education and awareness programs emphasizing the importance of lifestyle modifications for effective diabetes management.
Similar content being viewed by others
Introduction
Diabetes mellitus, more called diabetes, is a metabolic disorder of multiple etiology characterized by chronic hyperglycemia with disturbances of carbohydrate, fat, and protein metabolism resulting from defects in insulin secretion, insulin action, or both1. Type 2 diabetes is the most common type of diabetes, accounting for over 90% of all diabetes worldwide. In type 2 diabetes, hyperglycemia is the result, initially, of the inability of the body’s cells to respond fully to insulin, a condition termed insulin resistance. According to data from the International Diabetes Federation (IDF) Atlas 10th edition, it was reported that 537 million people were living with diabetes worldwide. However, 74 Million new diabetics were included in the pool from the last estimate made in 2019. There was an overall 16% increase in the population of diabetes globally, and estimatedly, there will be a 46% (783 Million) increase globally by 20452,3,4. According to the 10th Edition of the IDF Diabetes Atlas, released on December 6th, 2022, Pakistan is ranked 3rd globally with almost 33 Million diabetics. It has the highest national prevalence (26.7%) of diabetes globally, with one in four persons reporting having the disease5.
In a recent review study published by Ramzan et al., they comprehensively covered the pattern of anti-diabetes prescription6. It was reported that the global prescription pattern of anti-diabetic medications varies in different regions of the world7,8,9. Metformin is the first-line oral anti-diabetic agent recommended in most guidelines published by the American Association of Clinical Endocrinology and the International Diabetes Federation10,11. In the developed nations, those following the American Diabetes Association and European Association for the Study of Diabetes guidelines tend to have higher prescription levels of glucagon-like peptide-1 GLP-1 and sodium-glucose-linked transporter-2 SGLT-26,12,13. In accumulation to metformin, there were many different combinations of sulfonylureas, dipeptidyl peptidase 4 DPP-4 inhibitors, sodium-glucose linked transporter-2 (SGLT2) inhibitors, and receptor agonists similar to glucagon-like peptide-1 (GLP-1) are commonly prescribed based on the clinical characteristics, co-morbidities, and treatment goals of the individual patient14,15. Various studies reported evolving trends in diabetes medication across European countries. Sulfonylurea use declined, notably in France, which dropped from 35 to 29% between 2001 and 2003 and across Europe between 2008 and 2012. In Spain and Germany, sulfonylurea prescriptions were around 17% and 12%, respectively, with the UK seeing a reduction from 10 to 6% between 2006 and 2010 and even lower for first-line use. Conversely, metformin saw increased usage in France, Germany, and the UK, reaching 91% as a first-line treatment in the UK in 2013. Insulin use varied, increasing from 1.71 to 2.27% in France, while the UK maintained consistent usage. Thiazolidinediones initially surged but declined in most countries, and Dipeptidyl peptidase-4 inhibitors gained popularity, particularly in France and the UK. Glucagon-like peptide-1 receptor agonists showed mixed trends6,12,16,17,18.
Prescription patterns define the type and character of medication use and adherence to local, state, or federal regulations, such as standardized prescribing practices, the use of medications from the essential drug list, and the use of generic medications19,20. Adherence and the prevention of disease are both advantages of appropriate prescribing. An irrational prescribing pattern develops when the wrong anti-hyperglycemic drug dosage, frequency, or duration is administered21,22. Due to inadequate therapy and unpleasant drug reactions, improper drug administration may also increase patient costs. Loss of confidence between the patient and the practitioner may result from a lack of progress and adverse drug reactions23.
The management of diabetes in Pakistan is challenging due to limited resources, poor access to health care, and a lack of awareness among the general population. Patients with diabetes in Pakistan are managed with a combination of lifestyle modifications and pharmacological interventions24. However, adherence to treatment guidelines and the use of oral antihyperglycemic agents in Pakistan needs to be clarified. Previous studies reported that metformin, sulfonylureas (SU), and dipeptidyl peptidase four inhibitors (DPP-4) are Pakistan's most commonly prescribed oral antihyperglycemic agents. There is a significant variation in the prescription patterns in different regions of the country24,25. There is a need for further research to evaluate prescribing trends and practices in diabetes management in Pakistan to ensure that patients receive optimal care26,27.
According to the United Kingdom Prospective Diabetes Study, intense blood glucose control with sulfonylureas or insulin significantly reduced the risk of microvascular complications28,29. A significant disparity was observed in Pakistan, with multiple research documenting suboptimal prescribing practises. Various studies conducted in different provinces have documented a notable deficiency in medication adherence within the Punjab district. Specifically, it has been seen that a significant proportion of patients, approximately 68%, adhere solely to the first-line recommended therapy, namely Metformin, for the purpose of managing their diabetes. According to a recent survey, persons aged 65 and above with diabetes were prescribed an average of 8.3 medicines30. According to the available data, a notable proportion of patients, specifically 18.7%, were found to have been prescribed with inaccurate dose or inappropriate dosage forms31,32.
The prescribing patterns of antidiabetic medications in Pakistan represent a pressing concern due to the high prevalence of diabetes within the Pakistani population. Prioritizing the use of optimal therapies is essential for effective blood sugar management and the prevention of potential complications. Nevertheless, there is a clear need for in-depth research into the specific trends in the prescription of antidiabetic drugs in Pakistan, underscoring the necessity for further investigation33. Varied regional patterns exist in oral antihyperglycemic agent prescriptions in the country. Fast and long-acting insulin analogs saw increased use, while natural insulin prescriptions decreased significantly (p < 0.001). Metformin, incretin modulators, and fixed oral combinations were prescribed more frequently (p < 0.001). Human insulin was preferred for female and elderly patients34,35. Older patients were less likely to be prescribed metformin and more likely to be prescribed sulphonylureas. There were studies that reported that adding sulphonylureas to the therapy may increase the risk of mortality and risk of hypogycemia36. In the non-means-tested scheme, socioeconomic distinctions were observed in the increased prescribing of newer, more expensive anti-diabetic drugs. Both insulin and oral anti-diabetic medications were prescribed in a manner that varied by region37. In addition, there needs to be more adherence to treatment guidelines, and patients may receive suboptimal therapy. Therefore, it is necessary to evaluate the prescribing patterns of anti-diabetic medications in Pakistan to identify areas for improvement and ensure that patients receive the best possible care38.
Therefore, this study aimed to examine the prescribing practices of anti-diabetic medications, an association of lifestyle modification with medications prescribed, and their effectiveness in preserving ideal glycemic levels in diabetic patients undergoing treatment in tertiary care teaching hospitals in rural and urban Pakistan.
Methodology
Study design
This cross-sectional observational study was conducted in six different tertiary care hospitals from 3 major cities of Pakistan. The study population includes patients with type 2 diabetes mellitus who received care at selected healthcare facilities during the study period (October 2021 and February 2022).
Inclusion criteria
-
1.
Participants had a confirmed diagnosis of type 2 diabetes mellitus based on established diagnostic criteria such as fasting plasma glucose levels, oral glucose tolerance test, or glycated hemoglobin (HbA1c) levels.
-
2.
Participants were 18 years or older and were citizens or residents of Pakistan.
-
3.
Written Informed Consent: participants could provide written informed consent or have a legally authorized representative provide support.
-
4.
Participants were able to provide written informed consent.
-
5.
Participants were on a stable oral antihyperglycemic drug regimen for at least three months before enrollment.
Exclusion criteria
-
1.
Participants diagnosed with type 1 diabetes mellitus were excluded from the study as the focus was on type 2 diabetes mellitus.
-
2.
Pregnant or lactating females were excluded from the study due to potential risks associated with medication use during these conditions.
-
3.
Participants with severe renal or hepatic impairment, as determined by clinical assessment or laboratory tests, were excluded due to the potential impact on the metabolism and excretion of oral antihyperglycemic drugs.
-
4.
Participants with a history of diabetic ketoacidosis were excluded due to the potential need for specialized treatment and management.
Ethical approval and consent to participate
The study received ethical approval from the Human Research Ethical Committee of Universiti Sains Malaysia (USM/JEPeM/22090589), the Bio-Ethics Committee (BEC) of Bahauddin Zakariya University, Multan (ACAD/EXT/01/2022), and the Ethical Review Board of Shaheed Zulfkar Ali Bhutto Medical University (1-3/2019/ERB/SZABMU). It was conducted in multiple healthcare facilities throughout Pakistan, both public and private, including Pakistan Institute of Medical Sciences, Capital Development Authority (CDA) hospital, Islamabad, District Health Quarter Hospital, Rawalpindi, City International Hospital Quetta, Royal Healthcare Multan, and Medicare Hospital Rawalpindi. Ethical approval was obtained from the relevant institutional review boards of all participating hospitals, and written informed consent was obtained from study participants with confidentiality maintained throughout the study. The study was conducted per the Declaration of Helsinki and reported according to “The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)” guidelines39,40.
Sampling size
The Rao Soft calculator calculated 384 mandatory sample sizes based on 33% prevalence, 5% margin error, and 95% confidence interval41. The sample size was determined based on the total number of patients with type 2 diabetes mellitus who received care in the selected healthcare facilities during the study period. For this purpose, 450 patients were interviewed, and 388 participants met the study criteria.
where: n is the required sample size, Z is the Z-value corresponding to the desired level of confidence (e.g., 1.96 for a 95% confidence level), p is the estimated prevalence or proportion in the population, E is the desired margin of error or precision.
Data collection
Data were collected by reviewing the medical records of the patients. A predesigned data collection form was used to record the following variables: patient demographics, clinical characteristics, prescription of antihyperglycemic drugs, dosing, and adherence to treatment guidelines. The prescription pattern was analyzed, and compliance with treatment guidelines was determined by comparing it to the ADA’s 2021 recommendations. Several parameters, including Hb1Ac and adherence to therapy, were considered when evaluating prescription adherence to ADA guidelines.
To access the medication adherence level of the study participants, urdu validated version of the Drug Attitude Inventory 10 Items (DAI-10).
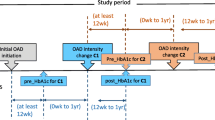
The flow of study is as follows shown in Fig. 1.
Study variables
The study variables include Age, sex, duration of diabetes, body mass index (BMI), co-morbidities, prescription of antihyperglycemic medications, and dose, including the laboratory values of the patients, i.e., HbA1c, fasting blood glucose, random blood glucose, and adherence to treatment guidelines.
Data analysis
Data were analyzed using descriptive statistics, including mean, median, standard deviation, and frequency distributions. A chi-square test was applied to assess the association between prescribed medication and adherence to the recommended guidelines. Statistical analysis was performed using Microsoft Excel 2016 and SPSS version 22.
Results
The study results demonstrate that there were 388 patients, including men (180) and women (208). Patients were divided into five age groups. There were 152 (39%) between 41 and 50 years and 129 (33.2%) between 51 and 60 years. 233 (60.1%) of 388 patients had Fasting Blood Glucose (FBG) > 126 mg/dl, and 258 (66.5%) had Random Blood Glucose (RBG) > 200 mg/dl.
The study has yielded crucial insights into the characteristics and distribution of type 2 diabetes patients. Of particular interest is the fact that 39.0% of diabetes cases were found in the age group of 41–50 years. In comparison, only 1.5% were seen in individuals aged 28–30 years, indicating a significant age-related trend in diabetes prevalence. Additionally, the study found that more females (53.6%) were affected by diabetes than males (46.4%), which is an important observation. Education-wise, over half of the diabetic patients (57.7%) had only a primary level of education, highlighting a significant educational distribution among the diabetic population. Occupation-wise, housewives constituted a substantial proportion of patients (50.8%), indicating the important role of this occupation in diabetes prevalence. Government employees (23.2%) and businessmen (14.9%) also showed significant representation within the diabetic cohort. The study also revealed that the most prevalent co-morbidity was a combination of diabetes and hypertension, affecting 32.5% of patients, providing crucial insights into the health profile of diabetic individuals. Lastly, family history was found to be an essential factor, with the majority (71.6%) of patients having a positive family history of diabetes (Table 1).
In the analysis of laboratory parameters, it's worth noting that most patients (60.1%) had a fasting blood glucose level above 126 mg/dl, while 66.5% had a random blood glucose level exceeding 200 mg/dl. Regarding HbA1c levels, more than half of the patients (52.1%) had levels above 7.0. These results are significant as they highlight the prevalence of elevated blood glucose and HbA1c levels among the studied population, underscoring the need for effective diabetes management strategies.
A study of medication usage was observed in patients with Type 2 diabetes in a total of 388 prescriptions. The mean number of antihyperglycemic drugs per prescription was found to be 5.08, with a range of 1 to 3 drugs per prescription. The percentage of antihyperglycemic drugs prescribed was calculated as follows: 13.7% for Biguanides, 1% for DPP4i, 18.3% for Biguanides plus DPP4i, 5.7% for Sulfonylurea, 14.4% for Human Insulin, 3.9% for Sodium-Glucose Linked Transporter 2 (SGLT-2) plus Modern Insulin (insulin analog), 26% for Biguanides plus Sulfonylurea and DPP4i, 13.1% for Biguanides plus DPP4Ii and Insulin, 3.4% for Biguanides plus Sodium-Glucose Linked Transporter 2 (SGLT-2), and only 0.5% for SGLT-2 and DPP4i (Table 2).
Further analysis of medication usage (Fig. 2) revealed that the majority of patients with Type 2 diabetes received triple therapy (26%), while 34.7% received monotherapy.
These findings suggest that healthcare providers use a combination of medications to effectively manage the condition, the most common combination being Biguanides, Sulfonylurea and DPP4i. These results have important implications for the management of Type 2 diabetes and highlight the need for individualized treatment plans to achieve optimal results.
The study on diabetes treatment combinations revealed that patients were administered monotherapy, dual therapy, and triple therapy. The utilization of Metformin, Sulphonylureas, and DPP-4 inhibitors has witnessed a notable rise in their application for the management of diabetes. The study revealed that a total of 50.6% of patients were treated solely with metformin, resulting in an average HbA1c reduction of 6.28%. A total of 21% of patients utilized sulphonylureas as a monotherapy, which led to a mean reduction in HbA1c levels of 6.86 units. Metformin and Sulphonylureas were administered to 48.3% of the patient cohort, resulting in a mean HbA1c value of 6.73. Nevertheless, a notable proportion of 53.1% of participants made a transition from Sulphonylureas to Metformin, which subsequently led to an average HbA1c level of 7.60. It is noteworthy that a significant proportion of patients, specifically 95.9%, were administered a combination of Metformin and DPP-4 inhibitors.
This treatment approach resulted in a mean HbA1c level of 7.87. The combination of Metformin with SGLT-2 inhibitors or GLP-1 agonists exhibited the highest level of glycated hemoglobin (HbA1c) at 10.33. The findings of the study indicate that the combination of Metformin-Sulphonylureas-DPP-4 is frequently employed as an effective treatment for diabetes. In contrast, the efficacy of other combinations in controlling HbA1c levels exhibited considerable variability as indiacated in the Table 3.
The data on treatment adherence reveals that 59.6% of patients demonstrated good adherence to their prescribed treatments, indicating a strong commitment to managing their health. Around 35.7% displayed moderate adherence, suggesting room for improvement, while 4.7% exhibited poor adherence as evident by Fig. 3.
To evaluate the association among sociodemographic characteristics, the chi-square test was applied, as represented in Table 4. The result of the association suggests that there was no significant association between glycemic levels and characteristics like gender, Age, and duration of treatment. However, a significant association was observed between patients with higher body mass index (BMI) (p-value < 0.001). It can be seen that there was a higher count of patients with uncontrolled glycemic levels falling into the overweight and obese category. Another important factor to compare among the wild study population is that the majority of them were on combination therapy, and despite using various oral antidiabetics, they are still unable to control their blood glucose levels (p-value < 0.05). In contrast, it was widely observed in the study population that those individuals who tend to follow the guidelines for lifestyle modifications given by the treating physician or diabetes educators have better glycemic control (p-value < 0.001). Overall, patients with better adherence to medical therapy and lifestyle modifications tend to have significantly better glycemic control.
Discussion
The present study aimed to analyze the prescription patterns for oral antihyperglycemic drugs (OADs) and the adherence to treatment guidelines in patients with type 2 diabetes mellitus in Pakistan. The study findings revealed that the mean number of OADs prescribed per prescription was 5.08, with the most common combination being Biguanides, Sulfonylurea, and DPP4i. Type 2 diabetes mellitus is a chronic metabolic disorder resulting from insulin action and secretion defects. Type 2 diabetes mellitus has reached epidemic proportions worldwide; it has been studied that more than 220 million people had the disease in 201042. A study shows that 336 million people have diabetes mellitus, and the number of diabetic patients will be 552 million by 20305.
These results have important implications for managing type 2 diabetes in Pakistan. The high prevalence of poor glycemic control indicates that healthcare providers must reevaluate their treatment strategies and ensure that patients receive individualized treatment plans based on their medical history, lifestyle, and other co-morbidities. Additionally, healthcare providers should regularly monitor their patient's glycemic control to adjust treatment plans to achieve optimal outcomes43.
According to the Pakistan Endocrine Society (PES) guidelines 2021 (Appendix A), biguanides are first-line agents in type 2 diabetes. When glucose control targets are not achieved, add SGLT-2. If metformin is not used first-line, add a dipeptidyl peptidase-4 inhibitor (DPP-4), or a thiazolidinedione must be initiated in the patient. Moreover it was also recommended that is patient is having choronic obesity GLP-1 agonist must be initated. A rapid-acting insulin secretagogue is an alternative to sulfonylureas44.
Previous research has investigated the patterns of prescription for antidiabetic drugs within the Diabetes Registry Tyrol for the period spanning from 2012 to 2018. Significantly, Sodium/Glucose Cotransporter 2 inhibitors (SGLT-2i) exhibited a noteworthy rise in prescription rates (p < 0.001), along with metformin (p = 0.002), gliptins (p = 0.013), and glucagon-like peptide-1 agonists (GLP-1a) (p = 0.017). In contrast, there was a notable decrease in the number of prescriptions for sulfonylurea medications (p < 0.001). Metformin has been identified as the antidiabetic drug with the highest prescription rate, accounting for 51.3% of all prescriptions. Following metformin, insulin/analogs were the second most commonly prescribed drug at a rate of 34.6%. Gliptins were prescribed at a rate of 28.2%, while SGLT-2i, sulfonylurea, glitazones, GLP-1a, and glucosidase inhibitors were prescribed at rates of 11.7%, 9.1%, 3.7%, 2.8%, and 0.4% respectively. Significantly, the observed changes in prescription patterns remained consistent over the study, occurring prior to disseminating international and national guidelines. This suggests that physicians can adjust their practices based on developing clinical data, even before formal revisions to established standards45,46,47.
A comparison of the present study with previous studies conducted in Pakistan revealed some similarities and differences. For example, a study in Karachi reported that the most commonly prescribed OADs were Biguanides and Sulfonylureas, which is consistent with the present study. However, the study also reported that DPP4i was the most frequently prescribed class of OAD, which is in contrast to the present study27.
Furthermore, a study conducted in Lahore reported that 63% of the patients had poor glycemic control, similar to the present study's findings. However, the study also identified that Age, sex, and duration of treatment significantly affected glycemic control, in contrast to the current study's findings48.
Willey et al. study has shown that monotherapy can provide adequate glucose control. However, our investigation discovered a statistically significant relationship between glycemic control, monotherapy, and combination treatment. We found a statistically significant correlation between glycemic control, BMI, anti-diabetic medicine therapy, and lifestyle change49,50,51.
Therefore, even with optimal therapy with anti-diabetic medications, lifestyle change combined with anti-diabetic drug treatment can improve glycemic control in individuals with Type 2 diabetes.
The results of this study are consistent with previous research conducted in South Asia, which has also reported that metformin is the most commonly prescribed drug for diabetes mellitus type 2. For example, a study conducted in India by Tripathi et al. found that metformin was the most frequently prescribed drug, followed by sulfonylureas and DPP-4 inhibitors52. Another study conducted in Bangladesh by Akter et al. reported similar findings, with metformin being the most commonly prescribed drug, followed by sulfonylureas and meglitinides53.
However, the present study revealed a lower adherence rate to treatment guidelines than previous research conducted in Pakistan. A survey by Tabassum et al. reported that only 41.6% of total prescribed medications are in recommendation with the guidelines suggested by the American Diabetes Association30. Similarly, a study conducted in Lahore reported high adherence to treatment guidelines, with 80.5% of patients receiving the recommended medications54.
Our study's lower adherence rate to treatment guidelines could be attributed to several factors, including a need for more awareness among healthcare professionals about the latest treatment guidelines, poor patient education, and limited medication access. These findings highlight the need for healthcare professionals in Pakistan to be trained in the latest treatment guidelines and make more significant efforts to improve patient education and medication access.
The study has not considered other factors that could affect prescription patterns and adherence to treatment guidelines, such as the socioeconomic status of patients, access to healthcare, and cultural beliefs about diabetes management. These factors could affect the generalizability and applicability of the study findings.
Conclusion
In conclusion, our study sheds light on imperative considerations for diabetes management in Pakistan. The findings underscore the critical necessity of tailoring treatment approaches to individual patients, considering their unique medical histories and lifestyles to achieve optimal glycemic control. The healthcare landscape must evolve to meet these demands, necessitating the implementation of updated training for healthcare providers, augmented patient education efforts, and enhanced medication accessibility.
As the prevalence of diabetes continues to rise in Pakistan, urgent systemic interventions are required. A comprehensive national action plan is essential, focusing on multifaceted strategies such as heightened public awareness, promotion of healthy lifestyle practices, and improved infrastructure for diabetes care and treatment access. Our study contributes substantively to the discourse on diabetes management in Pakistan, providing a foundation for evidence-based practices and policy initiatives.
Continued research is pivotal for a nuanced understanding of the complex factors influencing prescription patterns and guideline adherence in the Pakistani context. This ongoing inquiry will not only deepen our comprehension of diabetes management challenges but also inform future policies and practices, facilitating effective responses to the evolving health landscape. In essence, our research underscores the pressing need for tailored, informed, and dynamic approaches to diabetes care in Pakistan to address the increasing burden of this prevalent health concern comprehensively.
Limitation
This study has limitations, focusing narrowly on physicians' antidiabetic prescribing practices while neglecting patient adherence, comorbidity management, and lifestyle adjustments crucial to diabetes care. Limited to established diabetic patients with year-long follow-ups, it misses early-stage insights. The exclusive reliance on quantitative data excludes nuanced perspectives from qualitative methods. Comparative analyses across regions and healthcare systems in Pakistan are lacking. Intervention studies to assess initiatives like educational programs are absent. To advance diabetes care research in Pakistan, future studies should embrace a longitudinal approach, integrate qualitative methods, conduct cross-regional comparisons, and include interventions for a more comprehensive understanding.
Future recommendation
To advance type 2 diabetes management in Pakistan, crucial research avenues are outlined. Longitudinal studies over extended periods offer insights into prescribing patterns and adherence trends. Integrating qualitative methods, like interviews, enriches understanding. Regional comparisons within Pakistan illuminate prescribing variations, guiding targeted interventions. Intervention studies, focusing on education and communication strategies, optimize prescribing practices. Evaluating health system dynamics, technology's role, collaboration, and long-term cost-effectiveness refines diabetes care. Addressing these imperatives elevates knowledge and enhances type 2 diabetes management in Pakistan.
Data availability
The data sets used and analyzed during the current study are available from the corresponding author at a reasonable request.
Code availability
The collected data were analyzed using statistical tools in SPSS version 22.0 data analyzing software.
Abbreviations
- BMI:
-
Body Mass Index
- CI:
-
Confidence Interval
- DM:
-
Diabetes
- DPP4i:
-
Dipeptidyl peptidase 4 inhibitors
- Govt.:
-
Government
- HbA1c:
-
Glycosylated hemoglobin
- HI:
-
Human insulin
- I:
-
Insulin
- MI:
-
Modern insulin/insulin analogue
- SD:
-
Standard deviation
- SGLT-2:
-
Sodium-Glucose-Linked Transporter-2
- SU’s:
-
Sulphonylureas
References
Organization, W. H. Classification of Diabetes Mellitus. (2019).
Zimmet, P., Alberti, K. & Shaw, J. Global and societal implications of the diabetes epidemic. Nature 414, 782–787 (2001).
Hsu, C.-C. et al. Effect of bariatric surgery vs medical treatment on type 2 diabetes in patients with body mass index lower than 35: Five-year outcomes. JAMA Surg. 150, 1117–1124 (2015).
Mohammadi, S., Karim, N. A., Talib, R. A. & Amani, R. Knowledge, attitude and practices on diabetes among type 2 diabetic patients in Iran: A cross-sectional study. Science 3, 520–524 (2015).
Duran, A. et al. Introduction of IADPSG criteria for the screening and diagnosis of gestational diabetes mellitus results in improved pregnancy outcomes at a lower cost in a large cohort of pregnant women: The St. Carlos Gestational Diabetes Study. Diabetes Care 37, 2442–2450 (2014).
Ramzan, S., Timmins, P. & Hasan, S. S. Trends in global prescribing of antidiabetic medicines in primary care: A systematic review of literature between 2000–2018. Primary Care Diabetes 13, 409–421 (2019).
Mata-Cases, M., Franch-Nadal, J., Real, J. & Mauricio, D. Glycaemic control and antidiabetic treatment trends in primary care centres in patients with type 2 diabetes mellitus during 2007–2013 in Catalonia: A population-based study. BMJ Open 6, e012463 (2016).
Geier, A. S. et al. Patterns and determinants of new first-line antihyperglycaemic drug use in patients with type 2 diabetes mellitus. Diabetes Res. Clin. Practice 106, 73–80 (2014).
Datta-Nemdharry, P., Thomson, A., Beynon, J. & Donegan, K. Patterns of anti-diabetic medication use in patients with type 2 diabetes mellitus in England and Wales. Pharmacoepidemiol. Drug Saf. 26, 127–135 (2017).
Association, A. D. Standards of care in diabetes—2023 abridged for primary care providers. Clin. Diabetes 41, 4–31 (2023).
Blonde, L. et al. American Association of Clinical Endocrinology clinical practice guideline: Developing a diabetes mellitus comprehensive care plan—2022 update. Endocr. Practice 28, 923–1049 (2022).
Maguire, A., Mitchell, B. D. & Ruzafa, J. C. Antihyperglycaemic treatment patterns, observed glycaemic control and determinants of treatment change among patients with type 2 diabetes in the United Kingdom primary care: A retrospective cohort study. BMC Endocr. Disord. 14, 1–11 (2014).
Rizzo, M. et al. The effects of liraglutide on glucose, inflammatorymarkersandlipoprotein metabolism: Current knowledge and future perspective. Clin. Lipidol. 8, 173–181 (2013).
Patti, A. M., Giglio, R. V., Papanas, N., Rizzo, M. & Rizvi, A. A. Future perspectives of the pharmacological management of diabetic dyslipidemia. Expert Rev. Clin. Pharmacol. 12, 129–143 (2019).
ElSayed, N. A. et al. 2. Classification and diagnosis of diabetes: Standards of care in diabetes—2023. Diabetes Care 46, S19–S40 (2023).
Wilkinson, S. et al. Changing use of antidiabetic drugs in the UK: Trends in prescribing 2000–2017. BMJ Open 8, e022768 (2018).
Christensen, D. H., Rungby, J. & Thomsen, R. W. Nationwide trends in glucose-lowering drug use, Denmark, 1999–2014. Clin. Epidemiol. 8, 381–387 (2016).
Overbeek, J. A. et al. Type 2 diabetes mellitus treatment patterns across Europe: A population-based multi-database study. Clin. Therap. 39, 759–770 (2017).
Strom, B. L. What is pharmacoepidemiology? Pharmacoepidemiology. 6, 1–26 (2019).
Lim, L. L. et al. Real-world usage of sulphonylureas in Asian patients with type 2 diabetes using the Joint Asia Diabetes Evaluation (JADE) register. Diabetes Obesity Metab. 25, 208–221 (2023).
Organization, W. H. The rational use of drugs: Review of major issues. (1985).
Rahman, M. M., Munia, A. T., Sikdar, K. Y. K. & Sarkar, M. R. A cross-sectional study on current prescription trends and errors in outpatient department of a Bangladeshi secondary care district hospital. Perspect. Clin. Res. 13, 161 (2022).
Holt, R. I. et al. The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 44, 2589–2625 (2021).
Arokiasamy, P., Salvi, S. & Selvamani, Y. Global burden of diabetes mellitus: Prevalence, pattern, and trends. in Handbook of Global Health, 495–538 (2021).
Ali, Z., Imam, S. F., Adnan, M., Shabbir, I. & Rahat, T. Prescription pattern of antidiabetic drugs among type 2 diabetes patients of Sir Ganga Ram Hospital, Lahore. Pak. J. Med. Res. 54, 96 (2015).
Adnan Ali, A., Rahman, S. U., Ahmad, S., Hussain, H. & Khan, A. Prescribing pattern of drugs for diabetic patients in a Tertiary Care Private Sector Hospital, Peshawar, Pakistan.
Uddin, F., Ali, B. & Junaid, N. Prevalence of diabetic complications in newly diagnosed type 2 diabetes patients in Pakistan: Findings from national registry. J. Ayub Med. Coll. Abbottabad. 30, 15;30(4-Sup). (2019).
King, P., Peacock, I. & Donnelly, R. The UK prospective diabetes study (UKPDS): Clinical and therapeutic implications for type 2 diabetes. Br. J. Clin. Pharmacol. 48, 643 (1999).
Adler, A. I. et al. Development and progression of nephropathy in type 2 diabetes: The United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int. 63, 225–232 (2003).
Saher, T. et al. Doctors’ adherence to guidelines recommendations and glycaemic control in diabetic patients in Quetta, Pakistan: Findings from an observational study. Front. Med. 9, 978345 (2022).
Ur Rahman, J. et al. Assessment of prescribing patterns and medication errors related to prescriptions in hospitalized diabetes mellitus type-2 patients in Khyber Pakhtunkhwa, Pakistan. J. Pharm. Health Services Res. 14, 49–54 (2023).
Khan, M., Ullah, R., Khan, A., Khan, S. & Riaz, M. Assessment of prescriptions in the endocrinology department of a tertiary care hospital in Pakistan using World Health Organization guidelines. Adv. Preventive Med. 2020, 3705704, 6 pages (2020).
Shah, S. W. et al. Prescribing pattern of antihypertensive drugs in hypertensive patients with non-insulin dependent diabetes mellitus at tertiary care hospitals in Karachi Pakistan. J. Pharm. Res. Int. 33(56B), 107–112 (2021).
Michaelidou, M., Pappachan, J. M. & Jeeyavudeen, M. S. Management of diabesity: Current concepts. World J. Diabetes 14, 396 (2023).
Patti, A. M. et al. Impact of glucose-lowering medications on cardiovascular and metabolic risk in type 2 diabetes. J. Clin. Med. 9, 912 (2020).
Hougen, I. et al. Safety of add-on sulfonylurea therapy in patients with type 2 diabetes using metformin: A population-based real-world study. BMJ Open Diabetes Res. Care 9, e002352 (2021).
Zaharan, N., Williams, D. & Bennett, K. Prescribing of antidiabetic therapies in Ireland: 10-year trends 2003–2012. Irish J. Med. Sci. 183, 311–318 (2014).
Faizullah, M., Umar, M. I., Anwar, M. & Sarfraz, M. K. A cross-sectional study on knowledge, attitude and practices of medical doctors towards antibiotic prescribing patterns and resistance in Khyber Pakhtun Khawah, Pakistan. (2017).
Goodyear, M. D., Krleza-Jeric, K. & Lemmens, T. Vol. 335 624–625 (British Medical Journal Publishing Group, 2007).
Von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 370, 1453–1457 (2007).
Raosoft, I. Sample size calculator by Raosoft. Inc, in (2020).
Alberti, K. G. M., Zimmet, P., Shaw, J., Group, I. E. T. F. C. The metabolic syndrome—A new worldwide definition. Lancet 366, 1059–1062 (2005).
Bergman, M. et al. Petition to replace current OGTT criteria for diagnosing prediabetes with the 1-hour post-load plasma glucose≥ 155 mg/dl (8.6 mmol/L). Diabetes Res. Clin. Practice 146, 18–33 (2018).
Khan, K. A. Pakistan Endocrine Society (PES)—2020 guidelines for management of type 2 diabetes mellitus & cardiometabolic syndrome. J. Pak. Med. Assoc. 70, S1-52 (2020).
Engler, C. et al. Long-term trends in the prescription of antidiabetic drugs: Real-world evidence from the Diabetes Registry Tyrol 2012–2018. BMJ Open Diabetes Res. Care 8, e001279 (2020).
Khan, K. A. Pakistan Endocrine Society (PES)-2020 Guidelines for management of Type IIdiabetes mellitus and cardiometabolic syndrome. JPMA (2020).
Ceriello, A., Monnier, L. & Owens, D. Glycaemic variability in diabetes: Clinical and therapeutic implications. Lancet Diabetes Endocrinol. 7, 221–230 (2019).
Sultana, R. et al. Awareness and lifestyle practices among type-II diabetics pertaining to the disease attended at outpatient clinics of Nawabshah, Shaheed Benazirabad. J. Pharm. Res. Int. 33, 67–75 (2021).
Ramzan, B. et al. Impact of diabetes-related knowledge and medication adherence on quality of life among type 2 diabetes patients in a tertiary health facility in Multan, Pakistan. Trop. J. Pharm. Res. 21, 871–877 (2022).
Ramzan, B. et al. Impact of diabetes educator on diabetes management: findings from diabetes educator assisted management study of diabetes. Arch. Pharm. Practice 13, 43-50 (2022).
Willey, C. J., Andrade, S. E., Cohen, J., Fuller, J. C. & Gurwitz, J. H. Polypharmacy with oral antidiabetic agents: An indicator of poor glycemic control. Am. J. Managed Care 12, 435 (2006).
Tripathi, R., Tyagi, S. & Goel, V. Metformin in gestational diabetes mellitus. Indian J. Med. Res. 145, 588 (2017).
Akter, F. et al. Clinical characteristics and short term outcomes after recovery from COVID-19 in patients with and without diabetes in Bangladesh. Diabetes Metab. Syndrome Clin. Res. Rev. 14, 2031–2038 (2020).
Saeed, H., Saleem, Z., Naeem, R., Shahzadi, I. & Islam, M. Impact of health literacy on diabetes outcomes: A cross-sectional study from Lahore, Pakistan. Public Health 156, 8–14 (2018).
Acknowledgements
The author acknowledges the hospital authorities for their cooperation during the study.
Author information
Authors and Affiliations
Contributions
Conceptualization: S.C.O., M.D.B., Data curation: M.U.W., M.A., A.R., T.M. Formal analysis: A.S., M.D.B. Investigation: M.U.W., A.S., N.B., and T.M. Methodology: A.U.H.C., M.D.B., A.R., S.C.O., and Z.-U.-D.B. Project administration: M.D.B. Resources: M.D.B. Supervision: S.C.O., Z.-U.-D.B. Validation: M.A., A.R., A.S., T.M., and N.B. Visualization: M.D.B. Writing—original draft: M.D.B., T.M., and A.S. Writing—review & editing: M.D.B., S.C.O., M.U.W. and Z.-U.-D.B. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Butt, M.D., Ong, S.C., Rafiq, A. et al. An observational multi-center study on type 2 diabetes treatment prescribing pattern and patient adherence to treatment. Sci Rep 13, 23037 (2023). https://doi.org/10.1038/s41598-023-50517-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-50517-2
- Springer Nature Limited