Abstract
Tuberous sclerosis complex (TSC) is a neurodevelopmental disorder caused by mutations in the TSC1 and TSC2 genes and autosomal dominantly inherited. These mutations cause hyperactivation of the mammalian Target of Rapamycin (mTOR) pathway, leading to the development of nonmalignant masses involving various organ systems. Patients with TSC also experience neuropsychiatric symptoms collectively termed Tuberous Sclerosis Complex Associated Neuropsychiatric Disorder (TAND). Due to research advancements in TSC, patients now live well beyond the age of 50. Many experience objective impairment of memory and executive function, supported by formal neuropsychological testing, beginning in their late 40s. Biomarker analysis has described elevated levels of phosphorylated tau-181 in the cerebrospinal fluid of patients with TAND. Tau-PET imaging has also shown focal accumulation of the radiotracer flortaucipir (AV1451), suggesting that TSC may be a neurodegenerative disorder arising from accumulation of phosphorylated tau. However, the flortaucipir tracer has been reported to have significant off-target binding, preventing definitive conclusions from being drawn about the molecular etiology of neurodegeneration in TSC. Therefore, we initiated the Colocalization of AV1451 and Phosphorylated Tau in Adult brain tissue (CAPA) study. This study aimed to determine if flortaucipir is bound to phosphorylated tau in brains of patients with TSC and further sought to determine the specific tau isoform seen in TSC. Our results show that flortaucipir labels the 3R/4R isoform of phosphorylated tau, commonly seen in Alzheimer’s disease. However, amyloid staining was negative in brains of adult patients with TSC. Therefore, we conclude that TAND symptoms are due to the accumulation of the phosphorylated tau isoform seen in Alzheimer’s disease. This study suggests that hyperactivation of the mammalian Target of Rapamycin pathway may play a role in the amyloid-independent development of 3R/4R tau aggregation. Our findings could lead to a new era of anti-tau therapies used to treat both disorders.
Similar content being viewed by others
Introduction
Various isoforms of phosphorylated tau have been described as a neuropathological substrate for several neurodegenerative diseases. This group of disorders are commonly referred to as tauopathies. The 3R and 4R isoforms of phosphorylated tau are well established [4] and are associated with various neurodegenerative conditions: the 3R tau is predominantly seen in Pick’s disease, 4R tau predominantly in progressive supranuclear palsy (PSP) and corticobasal degeneration (CBD), and a mixture of 3R and 4R (3R/4R) tau in Alzheimer’s disease (AD).
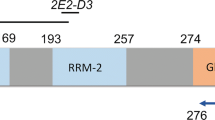
Tuberous Sclerosis Complex (TSC) is a neurodevelopmental disorder arising primarily from mutations in TSC1 (hamartin) and TSC2 (tuberin) (TSC1/2) [8]. These mutations promote the growth of benign masses involving several organ systems. In addition to the physical manifestations of TSC, these patients frequently suffer from behavioral, cognitive and psychiatric difficulties collectively termed Tuberous Sclerosis Complex Associated Neuropsychiatric disorders (TAND) [14]. Our work published in 2019 suggested a significant overlap between TSC and a group of neurodegenerative disorders named Frontotemporal Dementias (FTD) based on neuropsychological testing, however, TSC subjects scored significantly worse on memory when compared to FTD subjects [5]. Cerebrospinal fluid (CSF) results showed elevated phosphorylated tau (pTau-181) levels with an average of 32 pg/mL in TSC subjects when compared to healthy controls [5]. Furthermore, AV1451 (Flortaucipir)-PET/CT scans were completed in 3 adult patients with TSC. Intriguingly, focal uptake of AV1451in the frontal and temporal regions was seen in all 3 of these patients. Collectively, based on the significant memory loss and elevated CSF pTau-181 levels, it was hypothesized that TSC may represent a novel genetic tauopathy similar to that seen in AD.
AV1451 has a high affinity for pTau-181 related to Alzheimer’s disease by PET imaging [6]; however, AV1451 also displays significant off-target binding [1]. As a result, we could not definitively conclude that the focal binding of AV1451 in adult patients with TSC was due to the accumulation of pTau-181. Our current study investigates whether the AV1451 signal corresponds to tau pathology in adult patients with TSC by comparing AV1451 staining and immunohistochemical staining of various tau antibodies on brain tissue from adult patients with TSC, AD, FTLD-tau, and healthy controls. This is based on prior studies which have shown that TSC is an infantile tauopathy accumulating phosphorylated tau [10]. The isoform of phosphorylated tau in infantile tauopathies is still an area of active investigation. Here we show that AV1451 labels sparse neurofibrillary tangles in the entorhinal cortex, dorsolateral prefrontal cortex (Brodmann area 8) and inferior frontal cortex (Brodmann area 11) of adult patients with TSC. The tangles are also labeled by AT8 (which detects pTau-202/205) and GT-38 (which detects a conformation-specific mixture of 3R- and 4R-tau). Amyloid plaques were not detected in any of the brains from adult patients with TSC. These results suggest that TSC is a genetic 3R/4R tauopathy that develops independent of amyloid plaques seen in AD.
Materials and methods
Antibodies and PET ligand
The antibodies used for this study were AT8 (ThermoScientific cat # MN1020), GT-38 (ABCAM cat # ab254274), and 4G8 (BioLegend Cat#: 800,702). Unlabeled AV1451 was generously provided by Avid Radiopharmaceuticals.
Brain tissue
Tissue from cognitively healthy controls (HC), and from patients with AD, FTLD-tau, and TSC were obtained from the NIH biobank. Brain tissue was age and gender matched to HCs. AD brain tissue was requested with Braak stage 4 and above. Three subjects carried a clinical diagnosis of Down Syndrome (DS) and were included in the AD cohort. FTD brain tissue demonstrating FTLD-tau pathology was requested. Since patients with TAND showed executive function, behavioral and memory difficulties, three brain areas involving these functions, the dorsolateral prefrontal cortex (Brodmann area 8), inferior Frontal Cortex (Brodmann area 11) and the entorhinal cortex were selected for neuropathological analysis. Formalin fixed paraffin embedded (FFPE) tissue was sectioned at eight microns on a Leica microtome.
Immunohistochemistry (IHC)
IHC was performed on formalin fixed paraffin embedded (FFPE) sections that were deparaffinized in xylene and washed in absolute ETOH and 95% ETOH. Endogenous peroxidase activity was blocked with 1.875% H2O2 in methanol for 8 min. Samples were then washed and hydrated in DH2O. GT38 (ABCAM: cat#ab254274) required antigen retrieval with a boiling citrate buffer at pH6 for 30 min. A second blocking step was applied by submerging the sections in a dish containing 200 mL of 5% w/v nonfat dry milk in 0.05 M Tris buffer, pH7.6, for 20 min at room temperature. Primary antibodies were applied to each slide (1:500 for AT8 and GT-38) and allowed to incubate for 45 min at 37–40°C. Secondary antibodies were applied using the Dako EnVision™ Dual Link System-HRP (Agilent Technologies, Cat# K406189-2) and incubated for 30 min at 37–40°C. The slides were then developed with Dako DAB solution (Agilent Technologies, Cat# K346811-2) for 5 min and counterstained with Fisherfinest Hematoxylin + (ThermoFisher, Cat#220-100) for 15–25 sec. The slides were dehydrated through graded alcohols, cleared in xylene, and coverslipped in Permount mounting medium.
AV1451 staining
The AV1451 PET Ligand is autofluorescent and was applied to FFPE sections. The sections were first deparaffinized in xylene and washed with absolute ETOH, 95% and 70% ETOH. Endogenous autofluorescence was blocked using 0.1% Sudan Black B solution made with 70% ETOH. The AV1451 PET Ligand was supplied as a powder in a 1 mg vial. Then 380 µL of DMSO was added to the powder and allowed to dissolve to make a 10 mM stock solution. The working solution of AV1451 was a 1:100 dilution applied for 1 h at room temp. The sections were rinsed in 50% ETOH for 10 min prior to rinsing in DH2O for 10 min. The sections were coverslipped using Vectashield Hardset(Vector Laboratories; Cat#H1400).
Imaging and data analysis
AV1451 signal was analyzed using a digital Revolve R3 fluorescent microscope (ECHO, San Diego, CA) using the DAPI channel. AT8 and GT-38 immunohistochemistry was analyzed using an Olympus bright field microscope. Five 1mm2 fields with the highest number of tangles were chosen from each slide. The average number of tangles was quantified and converted to a semi-quantitative score as follows, 0: no tangles, 1: < 1 tangle per 1mm2 field, 2: 1–2 tangles per 1mm2 field, 3: 3–5 tangles per 1mm2 field, 4: 6–10 tangles per 1mm2 field, and 5: > 10 tangles per 1mm2 field.
Results
Patient characteristics
Patient characteristics are summarized in Table 1. Thirty-five patients were included in the study, including 11 healthy control patients, 9 patients with AD, 10 patients with TSC, and 5 patients neuropathologically diagnosed with FTLD-tau. Notably, no HC patients or patients with FTLD-tau had epilepsy, whereas 50% of patients with TSC had epilepsy and 22% of patients with AD had epilepsy. Similarly, no control patients, patients with AD, or patients with FTD had intellectual or developmental disability (IDD), but 55% of patients with TSC had Intellectual or Developmental Disability (IDD).
Qualitative immunohistochemistry findings
Patients with TSC exhibited sparsely positive AT8 staining in the entorhinal cortex and BA8 but not BA11. AT8 staining in patients with TSC was considerably sparser than in patients with DS/AD patients or FTLD-tau. HC patients did not show appreciable AT8 staining in any region (Fig. 1). Patients with TSC exhibited more strongly positive GT38 (3R tau + 4R tau) staining in all three brain regions studied, although the density was still sparse compared to patients with DS/AD or FTLD-tau (Fig. 2). AV1451 staining was positive for neurofibrillary tangles in patients with TSC, FTLD-tau, and DS/AD. AV1451 also labeled neuritic plaques from patients with DS/AD, but no glial tau lesions were observed (Fig. 3). No patients with TSC exhibited glial-tau lesions such as coiled bodies, tufted astrocytes, or astrocytic plaques (Figs. 1, 2, 3). Furthermore, no patients with TSC had amyloid-beta plaques (Fig. 4). The percentage of patients from each cohort positive for AT8, GT38, and AV1451 in the studied brain regions is sunmmarized in Table 2.
Semi-quantitative immunohistochemistry quantification
Semi-quantitative analysis was utilized to provide more formal assessment of qualitative findings. For AT8 (Fig. 1B), we observed that control patients and patients with TSC had no AT8 staining in BA11, whereas the median scores for patients with DS/AD and FTLD respectively were 5 (> 10 tangles/1 mm2 field). In BA8, however, patients with TSC had a median score of 0.5 (< 1 tangle/1 mm2 field, but tangles present), compared to controls which lacked AT8 staining. The median AT8 score for patients with TSC was also 0.5 in the entorhinal cortex, but the 75th percentile score was 1.75, as more patients had AT8 scores of 2 (1–2 tangles/1 mm2 field) or 3 (3–5 tangles/1 mm2 field). Median AT8 scores were high in all three brain regions for patients with DS/AD and FTLD-tau.
For GT38 scoring (Fig. 2B), while the median GT38 score in BA11 for patients with TSC was 0, the 75th percentile score was 1 (< 1 tangle/1 mm2 field), as several patients had scores of 1 or 2 (1–2 tangles/1mm2 field). The median GT38 score in BA8 was 0.5, and the 75th percentile score was 1; the median GT38 score in entorhinal cortex was 0.5, whitle the 75th percentile score was 2, as some patients had scores up to 4 (6–10 tangles /1mm2 field). Patients with AD and FTLD had high median GT38 scores in all three brain regions. Control patients had minimal to no appreciable GT38 scoring in all three brain regions.
Finally, AV1451 scores (Fig. 3B) also varied across groups. Patients with TSC had median scores of 0.5, 1, and 1 in BA11, BA8, and the entorhinal cortex respectively, compared to control patients with a median score of 0 in all regions. Patients with AD and FTLD-tau had median AV1451 scores greater than 2 in all three brain regions.
Discussion
The etiology of TAND behaviors remains unknown and has been hypothesized to be related to seizures, structural changes, and intellectual disability [12,13,14]. Our study suggests an additional neuropathological etiology. Future studies are needed to elucidate if the neuropathological phenotypes correlate with previously described neuroradiologic phenotypes and clinically meaningful TAND clusters [11, 13].
Our study provides the first compelling evidence that TAND is a novel amyloid-independent 3R/4R tauopathy. Our finding that patients with TSC had elevated density of AT8 staining, which identifies tau phosphorylated at Ser202 and/or Thr205, compared to control patients, but less than patients with AD or FTLD suggests that phosphorylated tau accumulates to some extent in patients with TSC. Additionally, our finding that the density of GT38 positive tangles was higher in patients with TSC than control patients, and again lower than patients with AD/FTLD, suggests that TSC is a mixed 3R/4R tauopathy. Patients with TSC notably lacked amyloid plaques and glial-tau lesions, distinguishing the pathology underlying TAND from other neurodegenerative conditions.
It is not entirely clear why patients with TAND had a lower density of GT38 positive tangles than FTLD patients; one possible explanation is that TSC causes a diminished extent of pathological 3R/4R tau accumulation compared with classic FTLD due to a different underlying causative mechanism. Prior research has suggested that TSC1/2 mutations, excessive mTOR signaling, and dementias may be linked mechanistically [9]. A recent case–control study likewise suggested that pTau-181 was elevated in patients with TAND and that these patients had symptoms consistent with a neurodegenerative condition [5]. Our study extends this body of literature by describing the precise underlying neuropathological phenotype of patients with TAND. In particular, the hyperactivation of mTOR signaling seen in TSC could contribute to increased tau protein aggregation and the development of 3R/4R positive tangles. This finding, if true, would have broad implications for research into other neurodegenerative conditions, as it would imply that mTOR signaling pathway could be causally related to the formation of neurofibrillary tangles, but not neuritic plaques [3, 7]. Additional characterization between pTau distribution (and density) and clinical phenotypes has major implications both for the diagnosis and management of TAND in patients with TSC and for the pathogenesis of 3R/4R tau commonly seen in Alzheimer’s disease.
Another amyloid independent 3R/4R tauopathy named Primary Age Related Tauopathy (PART) was considered to explain the findings in the TSC cohort. What makes PART less likely is the age at which the pTau was found. The mean age of the TSC cohort was 49 (Table 1). In an autopsy study, 20–25% of patients age 90 or older were found to have PART [2]. More importantly, PART is defined by the accumulation of 3R/4R pTau in the mesial temporal lobes. The TSC cohort from this study displayed 3R/4R pTau in both the frontal and temporal lobes. For these reasons, PART is unlikely to explain our findings in the TSC cohort. Future research is needed to determine the precise mechanism through which mTOR signaling pathway may be related to the development of neurofibrillary tangles.
Strengths of this study include its comparison to age and gender matched healthy controls, as well as its simultaneous evaluation of multiple neuropathologies, including AD, TSC, FTLD-tau, and other neurodegenerative disorders. Additional strengths include detailed, semi-quantitative neuropathological evaluation of various tau isoforms, allowing for precise definition of the specific tauopathy seen in patients with TAND.
This study has limitations. First and foremost, its sample size was small, as TAND is a rare condition, which prevented us from utilizing formal tests of statistical significance for the associations observed. Additionally, this study was unable to control for intellectual ability/cognitive status, which has been suggested to be a major risk factor for the clinical presentation of TAND [12]. Despite these limitations, this study suggests that TAND is a novel 3R/4R tauopathy independent of amyloid plaque formation, and points to promising new directions for research into the mechanism of TAND symptoms and novel anti-tau therapies in AD.
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
References
Baker SL, Harrison TM, Maass A, La JR, Jagust WJ (2019) Effect of off-target binding on 18F-flortaucipir variability in healthy controls across the life span. J Nucl Med 60:1444–1451. https://doi.org/10.2967/jnumed.118.224113
Bell WR, An Y, Kageyama Y, English C, Rudow GL, Pletnikova O, Thambisetty M, O’Brien R, Moghekar AR, Albert MS, Rabins PV, Resnick SM, Troncoso JC (2019) Neuropathologic, genetic, and longitudinal cognitive profiles in primary age-related tauopathy (PART) and Alzheimer’s disease. Alzheimers Dement J Alzheimers Assoc 15:8–16. https://doi.org/10.1016/j.jalz.2018.07.215
Cai Z, Chen G, He W, Xiao M, Yan L-J (2015) Activation of mTOR: a culprit of Alzheimer’s disease? Neuropsychiatr Dis Treat 11:1015–1030. https://doi.org/10.2147/NDT.S75717
Iqubal K, Liu F, Gong CXG-II (2010) Tau in Alzheimer disease and related tauopathies. Curr Alzheimers Res 7:656–664. https://doi.org/10.2174/156720510793611592
Liu AJ, Staffaroni AM, Rojas-Martinez JC, Olney NT, Alquezar-Burillo C, Ljubenkov PA, La Joie R, Fong JC, Taylor J, Karydas A, Ramos EM, Coppola G, Boxer AL, Rabinovici GD, Miller BL, Kao AW (2019) Association of cognitive and behavioral features between adults with tuberous sclerosis and frontotemporal dementia. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2019.4284
Mattsson N, Schöll M, Strandberg O, Smith R, Palmqvist S, Insel PS, Hägerström D, Ohlsson T, Zetterberg H, Jögi J, Blennow K, Hansson O (2017) 18 F-AV-1451 and CSF T-tau and P-tau as biomarkers in Alzheimer’s disease. EMBO Mol Med 9:1212–1223. https://doi.org/10.15252/emmm.201707809
Mueed Z, Tandon P, Maurya SK, Deval R, Kamal MA, Poddar NK (2019) Tau and mTOR: the hotspots for multifarious diseases in Alzheimer’s development. Front Neurosci 12:1017. https://doi.org/10.3389/fnins.2018.01017
Northrup H, Krueger DA, Roberds S, Smith K, Sampson J, Korf B, Kwiatkowski DJ, Mowat D, Nellist M, Povey S, de Vries P, Byars A, Dunn D, Ess K, Hook D, Jansen A, King B, Sahin M, Whittemore V, Thiele E, Bebin EM, Chugani HT, Crino P, Curatolo P, Holmes G, Nabbout R, O’Callaghan F, Wheless J, Wu J, Darling TN, Cowen EW, Gosnell E, Hebert A, Mlynarczyk G, Soltani K, Teng J, Wataya-Kaneda M, Witman PM, Kingswood C, Bissler J, Budde K, Hulbert J, Guay-Woodford L, Sauter M, Zonneberg B, Jóźwiak S, Bartels U, Berhouma M, Franz DN, Koenig MK, Roach ES, Roth J, Wang H, Weiner H, McCormack FX, Almoosa K, Brody A, Burger C, Cottin V, Finlay G, Glass J, Henske EP, Johnson S, Kotloff R, Lynch D, Moss J, Rhu J, Da Silva AT, Young LR, Knilans T, Hinton R, Prakash A, Romp R, Singh AD, Debroy A, Chen PL, Sparagana S, Frost MD (2013) Tuberous sclerosis complex diagnostic criteria update: Recommendations of the 2012 international tuberous sclerosis complex consensus conference. Pediatr Neurol 49:243–254. https://doi.org/10.1016/j.pediatrneurol.2013.08.001
Olney NT, Alquezar C, Ramos EM, Nana AL, Fong JC, Karydas AM, Taylor JB, Stephens ML, Argouarch AR, Van Berlo VA, Dokuru DR, Sherr EH, Jicha GA, Dillon WP, Desikan RS, De May M, Seeley WW, Coppola G, Miller BL, Kao AW (2017) Linking tuberous sclerosis complex, excessive mTOR signaling, and age-related neurodegeneration: a new association between TSC1 mutation and frontotemporal dementia. Acta Neuropathol (Berl) 134:813–816. https://doi.org/10.1007/s00401-017-1764-0
Sarnat HB, Flores-Sarnat L (2015) Infantile tauopathies: Hemimegalencephaly; tuberous sclerosis complex; focal cortical dysplasia 2; ganglioglioma. Brain Dev 37:553–562. https://doi.org/10.1016/j.braindev.2014.08.010
Sidira C, Vargiami E, Anastasiou A, Talimtzi P, Kyriazi M, Dragoumi P, Spanou M, Ntinopoulos A, Dalpa E, Evangeliou A, Zafeiriou DI (2021) The complex interplay of cortex, cerebellum, and age in a cohort of pediatric patients with tuberous sclerosis complex. Pediatr Neurol 123:43–49. https://doi.org/10.1016/j.pediatrneurol.2021.06.009
de Vries PJ, Belousova E, Benedik MP, Carter T, Cottin V, Curatolo P, Dahlin M, D’Amato L, Beaure d’ Augères G, Ferreira JC, Feucht M, Fladrowski C, Hertzberg C, Jozwiak S, Lawson JA, Macaya A, Marques R, Nabbout R, O’Callaghan F, Qin J, Sander V, Sauter M, Shah S, Takahashi Y, Touraine R, Youroukos S, Zonnenberg B, Kingswood JC, Jansen AC, Investigators T, Shinohara N, Horie S, Kubota M, Tohyama J, Imai K, Kaneda M, Kaneko H, Uchida Y, Kirino T, Endo S, Inoue Y, Uruno K, Serdaroglu A, Yapici Z, Anlar B, Altunbasak S, Lvova O, Belyaev OV, Agranovich O, Levitina EV, Maksimova YV, Karas A, Jiang Y, Zou L, Xu K, Zhang Y, Luan G, Zhang Y, Wang Y, Jin M, Ye D, Liao W, Zhou L, Liu J, Liao J, Yan B, Deng Y, Jiang L, Liu Z, Huang S, Li H, Kim K, Chen P-L, Lee H-F, Tsai J-D, Chi C-S, Huang C-C, Riney K, Yates D, Kwan P, Likasitwattanakul S, Nabangchang C, Chomtho LTK, Katanyuwong K, Sriudomkajorn S, Wilmshurst J, Segel R, Gilboa T, Tzadok M, Fattal-Valevski A, Papathanasopoulos P, Papavasiliou AS, Giannakodimos S, Gatzonis S, Pavlou E, Tzoufi M, Vergeer AMH, Dhooghe M, Verhelst H, Roelens F, Nassogne MC, Defresne P, Waele LD, Leroy P, Demonceau N, Legros B, Bogaert PV, Ceulemans B, Dom L, Castelnau P, Martin ADS, Riquet A, Milh M, Cances C, Pedespan J-M, Ville D, Roubertie A, Auvin S, Berquin P, Richelme C, Allaire C, Gueden S, Tich SNT, Godet B, Rojas MLRF, Planas JC, Bermejo AM, Dura PS, Aparicio SR, Gonzalez MJM, Pison JL, Barca MOB, Laso EL, Luengo OA, Rodriguez FJA, Dieguez IM, Salas AC, Carrera IM, Salcedo EM, Petri MEY, Candela RC, da Carrilho IC, Vieira JP, da Monteiro JPSO, de Leao MJSOF, Luis CSMR, Mendonca CP, Endziniene M, Strautmanis J, Talvik I, Canevini MP, Gambardella A, Pruna D, Buono S, Fontana E, Bernardina BD, Burloiu C, Cosma ISB, Vintan MA, Popescu L, Zitterbart K, Payerova J, Bratsky L, Zilinska Z, Gruber-Sedlmayr U, Baumann M, Haberlandt E, Rostasy K, Pataraia E, Elmslie F, Johnston CA, Crawford P, Uldall P, Uvebrant P, Rask O, Bjoernvold M, Brodtkorb E, Sloerdahl A, Solhoff R, Jaatun MSG, Mandera M, Radzikowska EJ, Wysocki M, Fischereder M, Kurlemann G, Wilken B, Wiemer-Kruel A, Budde K, Marquard K, Knuf M, Hahn A, Hartmann H, Merkenschlager A, Trollmann R (2020) Tuberous sclerosis complex-associated neuropsychiatric disorders (TAND): new findings on age, sex, and genotype in relation to intellectual phenotype. Front Neurol. https://doi.org/10.3389/fneur.2020.00603
de Vries PJ, Belousova E, Benedik MP, Carter T, Cottin V, Curatolo P, D’Amato L, Beure d’Augères G, Ferreira JC, Feucht M, Fladrowski C, Hertzberg C, Jozwiak S, Lawson JA, Macaya A, Marques R, Nabbout R, O’Callaghan F, Qin J, Sander V, Sauter M, Shah S, Takahashi Y, Touraine R, Youroukos S, Zonnenberg B, Kingswood JC, Jansen AC, TOSCA Consortium and TOSCA Investigators (2020) Natural clusters of tuberous sclerosis complex (TSC)-associated neuropsychiatric disorders (TAND): new findings from the TOSCA TAND research project. J Neurodev Disord 12:24. https://doi.org/10.1186/s11689-020-09327-0
De Vries PJ, Whittemore VH, Leclezio L, Byars AW, Dunn D, Ess KC, Hook D, King BH, Sahin M, Jansen A (2015) Tuberous sclerosis associated neuropsychiatric disorders (TAND) and the TAND checklist. Pediatr Neurol 52:25–35. https://doi.org/10.1016/j.pediatrneurol.2014.10.004
Acknowledgements
We would like to thank Avid Radiopharmacheuticals for providing the AV1451 radioligand for this study. We would like to thank the NIH NeuroBiobank for supplying the brain tissue. Lastly, we thank Nikki Steinsiek for her input on this paper.
Funding
Funding for this project was provided by the Duke University, Department of Neurology.
Author information
Authors and Affiliations
Contributions
AJL substantially contributed to the conception, design, analysis, interpretation and draft of this work. JBL substantially contributed to the acquisition, interpretation and draft of this work. JE made substantial contributions to the acquisition and interpretation of this work. JB substantially contributed to the conception, design, analysis, interpretation of data and draft of this work. RO made substantial contributions to the analysis, interpretation and draft of this work. SHW made substantial contributions to the conception, acquisition, analysis, interpretation and draft of this work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Duke University IRB approved protocol (protocol ID: Pro00105057) was completed prior to obtaining brain tissue from the NIH biobank.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, A.J., Lusk, J.B., Ervin, J. et al. Tuberous sclerosis complex is a novel, amyloid-independent tauopathy associated with elevated phosphorylated 3R/4R tau aggregation. acta neuropathol commun 10, 27 (2022). https://doi.org/10.1186/s40478-022-01330-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40478-022-01330-x