Abstract
Allergic rhinitis (AR) is an IgE-mediated inflammatory disease of the nasal mucosa with well described local immune responses during allergen exposure. The frequent association of AR with general extra-nasal symptoms and other allergic conditions, such as conjunctivitis and asthma, however, support a more systemic disease impact. In addition to acute elevation of soluble inflammatory mediators in periphery blood, a growing number of studies have reported changes in circulating blood cells after specific nasal allergen challenge or environmental allergen exposure. These findings imply an involvement of specific blood leukocyte subsets, thrombocytes and recently, erythrocytes. This review summarizes the circulating blood cell dynamics associated with allergen exposure in AR subjects reported so far. Additionally, the impact of therapy, particularly allergen-specific immunotherapy (AIT), the only currently available causal treatment reducing AR-related symptoms, is further considered in this context.
Similar content being viewed by others
Background
Allergic rhinitis (AR) refers to nasal mucosa inflammation upon repeated aeroallergen exposure in susceptible subjects [1]. The underlying early inflammatory response is characterized by IgE-mediated release of preformed histamine from activated mast cells, leading to up-regulation of pro-inflammatory cytokines and adhesion molecules. The late phase reaction is based on the release of newly generated mediators, such as leukotrienes (LT), and a wave of effector cells recruited from lymphatic tissue and circulating blood [2,3,4]. Indeed, circulating leukocytes and their subsets markedly differ in blood of symptomatic AR patients compared to healthy controls [5] and even an activation of platelets has been reported [6, 7]. Recently, we further described a rapid decrease in circulating erythrocytes after allergen exposure in AR [8, 9]. Thus, local nasal inflammation upon allergen exposure induces systemic inflammatory responses [10] and, in the context of effector cell recruitment, activation of bone marrow. This raises the question if changes in circulating blood cell numbers are indicative of the allergic nasal inflammatory response. The aim of this review was to summarize previously described effects of allergen exposure on complete and differential blood counts in adult patients suffering from AR and the observed impact of allergen-immunotherapy (AIT).
Blood cells in AR
T cells
T helper cells are the main players in the allergic airway inflammatory response. CD4+ T cells are characterized by specific surface molecules expression and cytokine secretion profiles [11]. Th1 cells result from an IL-12 and IFN-γ driven polarization of naïve CD4+ T cells (Th0) towards a Th1 phenotype. Lower Th1 numbers and thus, lower Th1-derived IFN-γ levels were found in nasal lavage fluids of AR patients compared to controls [12]. A higher IL-4 and lower IFN-γ production in cultured blood Th cells from pollen-sensitized seasonal AR patients is found compared to controls implying a Th2 skewing in allergic disease [13]. Th2 cell polarization in Th0 is mainly promoted by IL-4, but may also be induced by epithelium-damage associated release of TSLP, IL-25 and IL-33. Main effector cytokines of Th2 cells are IL-4, IL-5, and IL-13, supporting B cell-derived IgE production, eosinophil activation and mast cells-derived histamine and LT release. Th2 cytokines further suppress Th1 cell differentiation. Ratios of Th1/Th2 and Treg/Th2 are reduced in the nasal mucosa of AR patients during allergen season [14]. A relative predominance of Th2 cytokine profiles, except for IL-4 levels, was found in nasal fluid of olive-sensitized AR patients compared to healthy controls [12]. In circulating blood, Th2 cells are increased in AR patients while AIT has been shown to lower Th2 cell numbers in grass-pollen sensitized AR patients [15]. The Th9 cell subsets produce IL-9, IL-10 and IL-21 and are associated with eosinophil survival during allergic airway inflammation. In a recent murine model, a greater Th9 cell percentage, higher Th9 cell transcription factor mRNA and higher IL-9 levels were found in nasal mucosa of AR mice compared to controls. Further, after intranasal application of anti-IL-9 antibodies less eosinophil nasal mucosa infiltration was described [16]. Higher Th9 numbers were found in Chinese AR patients compared to controls. Further, IL-9 levels correlated with circulating eosinophil numbers and clinical symptom scores [17]. Another study did not observe different Th9 levels in HDM sensitized AR and controls [18]. AIT resulted in a lower frequency of Th2, Th9 and Th17 and higher values of Th1 and Treg cells and their respective cytokines [19]. Th17 cells are generated upon TGFβ, IL-6 and IL-21 co-stimulation and produce IL-17A, IL-17F, IL-22 and IL-26, but also IL-6 and IL-21 as positive feed-back loop cytokines. IL-17 directly promotes neutrophil recruitment and indirectly supports neutrophil generation via GM-CSF production. In a murine AR model, antibody mediated neutralization of IL-17 resulted in less eosinophil and neutrophil infiltration and lower Th2 and Th17 cytokine levels in nasal mucosa [16]. Elevated Th17 percentages and serum IL-17A levels have been reported in AR patients compared to controls [18, 20, 21] and a reduction of circulating Th17 cells after successful AIT has been reported [19]. A more recent study did not observe changes in Th17 numbers and function in AR patients during pollen season [22]. Tfh cells and their main effector cytokine IL-21 induce generation of B memory cells and isotype class switching in plasma cells. Tfh cells produced IL-4 and induced effector Th2 cell responses after allergen challenge in HDM allergic subjects; further Th2 responses were shown to be impaired in Tfh cell absence [23]. IL-4-committed Tfh were described to be Th2 cell precursors in HDM associated allergic airway disease [24], indicating their role in supplying new effector cells after allergen encounter as memory Th cell reservoirs in secondary lymphoid organs [25]. However, while one study found reduced circulating Tfh in human AR [26], they did not differ in another study compared to healthy controls [27]. Th22 cells and their main effector cytokine IL-22, were higher in peripheral blood of HDM sensitized AR patients compared to controls correlating with clinical symptom scores [18]. yδT cells, secreting IFN-γ, IL-17A, IL-17F and IL-22, are usually enriched at epithelial surfaces and manifest both innate and adaptive immunity characteristics; they release IL-4 and IL-13 and induce B cell IgE synthesis. [28] In AR, yδT cells support IL-5, IL-13 and IFN-γ release in the Th2 inflammatory response [29]. Nasal yδT cells (Vg1/Vd1-Jd1 TCR+) seem to differ from those in peripheral blood (Vg2/Vd2 TCR+) [30], implying that nasal mucosa yδT cells are organ specific and proliferate locally in an oligoclonal fashion upon allergen exposure [28]. Still, higher yδT cell percentages were described in circulating blood of AR patients, correlating with Th17 numbers and levels of IL-17 [20]. A Chinese study found increased circulating yδT numbers in AR patients with higher IL-17 and lower TGF-ß1 levels during pollen season [31], while yδT cells correlated negatively with Treg cell percentages and TGF-ß1 levels. Tregs are immune-modulatory cells secreting TGF-ß and IL-10; they suppress Th2 activation by inhibiting IL-4, IL-5, IL-9 and IL-13 production, block effector T cell migration to inflammation sites and further induce IgG4 instead of IgE production by B cells. In nasal fluid of AR patients, lower Treg cell numbers and slightly lower Treg derived TNF-ß levels were found compared to controls [12]. Treg cell-derived IL-10 levels were higher before compared to baseline values after AIT in the same study. Circulating Treg numbers did not differ between healthy subjects and in AR outside of allergen exposure [32], with an increase of Treg cells in nasal mucosa after allergen challenge and during allergen season [33, 34]. Another study described higher circulating Tregs numbers in AR patients compared to healthy controls; in the same study Treg numbers remained unchanged after 1 year of AIT compared to baseline values. The FoxP3- IL-10 producing Tr1 cells, usually associated with tumor immunity and immune tolerance after organ transplant [35], were reduced in circulating blood and inversely correlated with symptom scores in AR compared to healthy individuals [36]. Naïve CD8+ T cytotoxic cells (Tc) have the capacity to produce cytokines involved in allergic inflammation (e.g. IL-4 and IL-5) and stimulate IgE class switching in B cells [37, 38]; successful AIT reduces the IL-4 producing Tc subtype [39]. Recently, an involvement of Tcs in nasal mucosa inflammation of atypical AR patients was also proposed. [40] However, an active role for circulating Tcs in AR has not yet been established. Several studies report reduced blood Tc numbers [41, 42] in allergic airway disease potentially associated with a hyper-releasability of Tc granules [43]. A recent study reported no changes in circulating CD4/CD8 cell ratio in AR patients before or during allergen season compared to controls [22].
In 1995 Pawankar et al. described that T cells in nasal mucosa of AR patients were distinct and did not reflect circulating subsets [44]. The authors concluded that inflammatory cells are compartmentalized in nasal mucosa and circulating blood [45]. Comparison of reported findings regarding circulating lymphocytes is difficult based on differences in study design and heterogeneity of allergen exposure settings. While allergen contact does seem to impact circulating lymphocytes subtypes, particularly on a Th cell subset level, changes in differential blood lymphocyte count are not always observed.
Innate lymphoid cells
Innate Lymphoid Cells (ILCs), also referred to as natural helper cells, innate helper type 2 cells and nuocytes, are immune cells of the lymphoid lineage, which do not express T or B cell surface markers. Group 2 ILCs (ILC2s) secrete IL-5, IL-9 and IL-13 linking adaptive and innate immune responses in allergic disease. Allergen-associated release of IL-25, IL-33, and TSLP by airway epithelial cells induces ILC2 cytokine secretion and promotion of a Th2 inflammatory response and memory T cell reactivation [46]. In the presence of IL-2, IL-7 or TLSP, ILC2s were also shown to release IL-5 and IL-13 upon stimulation with IL-33 or IL-25 without antigen contact. Their expression of MHC class II molecules and costimulatory signals suggests a role in Th cell activation by antigen presentation [25]. Upon CysLTs and PGD2 stimulation ILC2-derived Th2 cytokines promote airway eosinophilia and mucus hypersecretion [47].
Higher ILC2 numbers in nasal tissue correlated with severity of AR in one study [48]. Dhariwal et al. showed an ILC2 accumulation in the nasal mucosa of AR after allergen challenge; these findings were particularly striking in patients with elevated IgE levels and airway eosinophilia outside of allergy season [49].
Increased ILC2 percentages in circulating blood have been described 4 h after allergen challenge in cat-sensitized AR patients. Allergen challenge in AR rapidly induces increased peripheral blood ILC2s that express CD84 [50]. Similarly, another study described higher circulating ILC2 levels in AR during pollen season, compared to AR subjects after AIT and non-atopic individuals [47, 51]. Interestingly, circulating ILC2s were also higher in HDM sensitized, but not in mugwort sensitized AR patients during allergen season and compared to healthy controls [52]. Circulating ILC2 percentages were similar in AR and in healthy subjects outside of allergen season [53].
Circulating ILC2s are involved in the AR immune reaction and appear to increase in circulation upon allergen exposure, possibly dependent on allergen type.
B cells
B lymphocytes are activated directly by antigen presenting interaction with T cells, promoting Th2 development by inducing IL-2 cytokine production [54], or indirectly by antigen contact. In AR, nasal mucosa residing IgE-positive B cells can produce IgE [55] and undergo class switch to IgE production upon allergen challenge [56]. IgE also binds on low affinity receptors FcεRII expressed on B cells, further upregulating IgE synthesis.
In blood of AR pollen patients a proportion of allergen-specific B cells showed adaptive memory B-cell responses making them potential sources of allergen-specific IgE upon subsequent allergen exposure [57]. However, the difficult quantification of circulating IgE+ B cells in allergic disease implies a B cell isotype switching to IgE+ B cells in the nasal mucosa through interactions with dendritic cells (DCs) and T cells [58]. A decreased in IgE+ B cells proportion was found in AR patients after AIT without correlation between blood IgE+ B cells and circulating IgE levels [59]. There is evidence that IL-21 regulates IgE levels by binding to B cells in the AR associated immune response [60]. Regulatory B cells (Bregs) modulate inflammation by IL-10, IL-35 and TGF-ß secretion and are associated with allergen tolerance [61]. Percentages of Breg cells were decreased in AR [26, 61], especially in cases with comorbid allergic asthma.
In summary, in AR circulating B cells appear to be recruited into the nasal mucosa, where class switching to IgE is induced, however, without significantly impact on overall blood B cell numbers.
Natural killer cells (NK)
NK cells play an important role in mediation between innate and acquired immunity, such as interaction with DCs leading to a selection of antigen-presenting cells. Since the description of subtypes by Wei et al. [62], NK cells are classified into IFN-γ secreting NK1 and IL-4, IL-5 and IL-13 secreting NK2 cells. In AR, higher circulating NK cell percentages and cytotoxicity was shown for IL-4+ NK2 cells but not for IFN-γ + NK1 cells compared with non-atopic controls, correlating with elevated IgE levels [5].
In a murine AR model, depletion of NK cells induced more mucosal and peripheral blood eosinophilia and higher IL-5 levels [63]. In AR patients, NK cells were shown to secrete IL-8 after treatment with IL-15 further indicating a link between NK cells and eosinophils in humans [64]. Circulating NK cells expressing the chemotactant CX3CR1 were increased after nasal allergen challenge in AR, but their relative percentage among lymphocytes remained the same [65].
Reports on circulating NK numbers in AR are scarce; however, the NK2 type appears to be involved in the allergic inflammatory response.
Monocytes
Depending on their surface receptor expression, circulating monocytes are classified as classical (CD14++CD16−), intermediate (CD14++CD16+) and non-classical monocytes (CD14 + CD16++) [66]. In particular, classical monocytes are shown to differentiate into macrophages or DCs upon homing into tissues.
Most airway macrophages are derived by proliferation of local embryonic precursors; they have homeostatic functions and their numbers remain unchanged after allergen challenge. Blood-derived monocytes, however, can promote allergic inflammation as interstitial macrophages. Macrophages can be subjected to classical activation (M1 cells), induced by IFN-α or lipopolysaccharide (LPS), or alternative activation (M2 cells), induced by IL-4 and IL-13, but also by IL-10, depending on the required pro- or anti-inflammatory cell functions. M2a cells produce pro-allergenic cytokines IL-4 and IL-13 and are involved in different stages of allergic airway disease [67]. In a murine model of AR, lymph node macrophages were associated with IL-4 and IgE production, as well as IgG to IgE immunoglobulin class switching [68]. In human allergic inflammation, gene expression of Th2-related chemokines from recruited CD14+ monocytes in the nasal mucosa was observed simultaneously with accumulation of both mucosal Th2 cells and eosinophils [69]. The authors suggested that recruited monocytes are regulated by IL-4/IL-13 signaling and are directly involved in Th2 pro-inflammatory chemokine production attracting effector cells. Circulating monocytes from atopic patients have a higher FcεRI surface expression correlating with serum IgE levels [70]. Further, higher levels of circulating monocytes have been described in AR compared to healthy controls [71]. Moniuszko et al. reported that circulating monocytes phenotypes differ in HDM AR patients and healthy individuals [72]; CD14++CD16+ and CD14 + CD16++ monocytes subtypes were pronounced in AR patients compared to healthy controls and associated with decreased CD4 + CD25high T cells frequencies. In AR, CD141 monocytes were recruited to the nasal mucosa within hours and DCs accumulated after several days of continued allergen challenge. During allergen season, blood CD14 + monocytes in AR subjects showed higher integrin adhesion molecule (CD11c) surface density compared to asymptomatic but also non-atopic subjects. Glucocorticoids were shown to deplete these subsets potentially limiting allergic inflammation by decreasing antigen presentation [11]. Immune modulating effects have also been described for monocytes. In mice, FcεRI-mediated IgE endocytosis by monocytes induces IgE clearance from serum [73]. After AIT, an increased IL-10 production by monocytes was reported in human AR subjects [74]. Further, a downregulation of monocytes-derived IL-10 by Th2 cytokines has been described in nasal mucosa of AR patients [75].
Circulating monocytes are a source for macrophages and DCs recruited to the nasal mucosa in AR associated inflammation; however, reports on elevated circulating monocyte numbers in AR appear inconsistent.
Dendritic cells
Antigen-presenting dendritic cells (DCs) in in allergic inflammation are on the one hand involved in pro-allergenic activation of effector T cells, and on the other hand in tolerance induction via activation of Tregs cells, such as during allergen immunotherapy. In circulating blood, the two main DC subtypes are CD11c − CD123+ plasmacytoid (pDCs) and CD11c + CD123− myeloid (mDCs) cells; blood DCs are typically without dendrites and less mature compared to tissue DCs. Allergen challenge leads to recruitment of circulating mDCs through chemotactic factors, such as IL-8, RANTES, macrophage inflammatory protein (MIP)-3α and epithelial β-defensins, leading to an increase of mucosal DCs within hours after allergen exposure. In allergic patients, epithelial cells can promote DCs maturation and induction of Th2 polarization by release of TSLP, IL-25 and IL-33 [76].
In allergic asthma, mDCs have increased surface FcɛRI expression levels compared to non-asthmatics, mediate pulmonary inflammation through T-cell and eosinophil activation, and nourish local IgE and Th2 cytokine production [77]. Further, a significant increase of tissue pDC are found in AR after allergen exposure skewing naïve T-cells towards a Th2 phenotype [78] or potentially inducing antigen-specific T-cell subset depletion by selective inhibition [79]. In AR, increased mDCs and pDCs numbers have been demonstrated in nasal mucosa after allergen challenge; further, tissue and blood DCs were shown to express less IL-10, IL-12 and IFN-α in these patients [80]. The authors concluded that these impaired DCs responses in AR patients promote Th2/Th17-cell polarization in vivo, since the IL-6/IL-17 pathway was also upregulated by blood mDCs. Another study showed impaired expression of costimulatory molecules by circulating mDCs promoting IL-5 and IL-13 derived Th2 cell responses [81].
AIT promotes DC-mediated naïve T-cells skewing towards an IL-10-producing Treg phenotype and subsequent Th1 response [82]. Indeed, AIT has been shown to result in an increase in IFN-α production from pDCs and elevated circulating IgG4 antibody levels after stimulation with a TLR9 agonist in AR patients [83]. Additionally, local corticosteroids inhibit the production of DC chemotactants in the nasal mucosa disrupting allergen presentation of tissue DCs to effector T cells [79].
While a significant mDCs and slight pDCs decrease was reported in circulating blood 24 h after allergen challenge in allergic asthma patients [84], suggesting their recruitment into the airway mucosa [85], little is known about circulating DCs dynamics after allergen challenge in AR.
Neutrophils
Migration of neutrophils is dependent on blood IL-8 concentration in AR [86]. While baseline circulating IL-8 levels in AR patients are similar to healthy controls, they were shown to significantly increase after allergen challenge [86]. Further, an increase in circulating IL-6 after allergen challenge has been associated with neutrophil trafficking in atopic AR subjects [49]. IL-17 from Th17 cells was also associated with neutrophil recruitment in AR, probably by inducing IL-8 and CXCL1Groα release by airway fibroblasts. Neutrophils express multiple mediators which mediate airway inflammation such as MMP-9, neutrophil elastase, α-defensin, TGF-ß1 and ROS, supporting eosinophil migration and priming of T cells [87]. The prolonged release of neutrophil elastase and free radicals damage the epithelium and are most likely responsible for vasomotor symptoms characterizing AR. Further, function alterations in ROS generation by circulating blood neutrophils potentially induce (anti)oxidant imbalance resulting in tissue damage [86].
A recent study of nasal cytology in 468 AR patients described a neutrophils dominated (≥90%) inflammatory cell response in 14.32% and a mixed eosinophil/neutrophil (10% ≤ eosinophil < 50%) response in 23.93% of all cases. [88]. Compared to healthy controls higher neutrophil numbers are generally observed in nasal fluid of AR patients [49]. Upon allergen exposure in intermittent AR, particularly early-phase responses are dominated by neutrophil accumulation in nasal mucosa, with positively correlating neutrophil numbers and nasal symptom scores in nasal lavage fluid 1 hour after allergen challenge [89]. Challenge with IL-8 lead to a fast influx of neutrophils into the nasal mucosa measured 30mins and 3 h after challenge [90]. In HDM allergic AR patients late-phase mucosal inflammation also induced circulating neutrophils activation and neutrophils increased in nasal fluid 6 h after allergen challenge [89]. Neutrophils accumulation in nasal mucosa seems partially LT dependent, since montelukast was shown to significantly lower neutrophil numbers 30 min and 6 h after allergen challenge [91].
Blood neutrophils, particularly segmented neutrophils, increase upon allergen challenge [8, 9] and show altered functions in AR. For example, circulating blood neutrophils from AR patients produced more LTB2 after stimulation with calcium ionophore than controls. Also, phagocytic activity of neutrophils was lower in AR subjects compared to healthy controls, but was increased at 7 h and 24 h after allergen compared to baseline. Further, increased ROS generation by circulating neutrophils was found in 24 h after allergen challenge in AR patients [89]. However in the late phase (7 h and 24 h) after allergen challenge neutrophil numbers were not elevated in AR [86].
In summary, circulating neutrophils increase in the early phase after nasal allergen challenge but return to baseline in the late phase. These findings possibly reflect a rapid recruitment of these innate immune cells to the nasal mucosa, where they support effector cell recruitment, but also induce tissue damage in AR.
Eosinophils
Eosinophils are innate immune system inflammatory cells with a well-known role in allergic inflammation. Their maturation, activation and survival are mainly mediated by IL-5 and eosinophil trafficking by Th2 cytokines, such as IL-5 and IL-13. In allergic inflammation, eosinophils promote Th2 polarization by IL-4, IL-25 and IDO release, but also B cell proliferation and antibody induction. Eosinophils also promote recruitment of Th2 cells by chemotactants such as CCL17/CCL22 and interactions with DCs. Tissue ILC2s have been shown to regulate blood eosinophils by IL-5 secretion [48, 92].
Atopic AR subjects show significantly increased eosinophil numbers in the nasal mucosa compared to healthy subjects [93]. Increased nasal mucosa eosinophils were found days after but not in the first 24 h post allergen challenge in pollen sensitized AR subjects, whereas placebo airway challenge did not induce nasal eosinophilia in AR [33]. Eotaxin levels increased after nasal allergen challenge in AR subjects and were associated with eosinophil and macrophage elevation in nasal fluid and sputum [94]. Eotaxin challenge alone was also shown to induce eosinophilia in nasal fluid of AR [95], without changes in lymphocyte, basophil, and macrophage numbers [96].
Elevated circulating eosinophils have been reported in AR patients during allergen season [97] with positive correlation to clinical symptoms and nasal inflammation. A study in HDM sensitized AR patients revealed a significant increase of eosinophil percentages 24 h after allergen challenge compared to baseline, which was not as pronounced as in allergic asthma [86]. However, this increase in circulating blood eosinophils and their progenitors was not consistently significant, despite regular elevation of plasma IL-5 [98, 99]. Interestingly, in symptomatic AR patients granules of circulating eosinophils were found mostly intact, implying that circulating eosinophils retain their granule contents until they home in target tissues [100]. Also, blood eosinophil chemotaxis and spontaneous ROS production did not significantly differ between AR patients and healthy controls [101].
The role of eosinophils in atopic disease is well known; numbers of circulating blood eosinophils increase in the inflammatory late phase response after allergen exposure in AR, but to a much lesser extent compared to allergic asthma.
Basophils
Basophils are equipped with surface IgE receptors and release histamine, lipid mediators and cytokines from intracellular vesicles upon IgE cross-linking. In the early phase of the allergic inflammatory response two pathways enable Th2 skewing by basophils: IgE-dependent IL-3, IL-4 and IL-13 secretion after allergen contact and direct stimulation by epithelial cell-derived IL-3, TSLP and IL-33. The late phase of IgE mediated AR responses is mainly induced by basophil-derived LTC4 and histamine following IL-3, IL-5 and GM-CSF activation [102]. IL-17RB expression on ex vivo allergen-challenged basophils from AR patients is IL-3 dependent and was shown to inhibit apoptosis, promoting IgE-mediated basophil degranulation [103]. Allergen-specific reactivity of circulating basophils was found to exhibit a Clock dependent circadian variability in seasonal AR [104].
In AR patients, basophil accumulation in nasal mucosa was described [105, 106], associated with subsequent histamine release 11 h after allergen challenge [105]. An increase in IL-18 levels was shown 4 h after nasal allergen challenge and correlated with basophil proportions after 24 h. [57] Another study found increased nasal mucosa basophils 1 hour after allergen challenge which persisted up to 1 week [107]. IL-33 protein was expressed by AR nasal epithelial cells in response to ragweed pollen exposure; IL-33 supported mucosal accumulation of eosinophils and basophils along with chemoattractant production from FcεRI1 expressing mast cells and basophils [108]. Further, nasal challenge with RANTES induced an allergic mucosal response with eosinophils and basophils infiltration [109].
Nasal allergen challenge was associated with increased blood basophil activation marked by peaks in circulating basophil activation markers up until 24 h after challenge [110] and spontaneous secretion of IL-13 [4]. Blood basophil sensitivity correlated with allergen-specific IgE fraction and was associated with clinical symptoms during grass pollen season [111]. In an early pioneer study, Pedersen et al. found that rhG-CSF treatment increases circulating basophils numbers, but reduces average basophil histamine content and releasability [112]. Persistent suppression of basophil response was associated with lower clinical symptoms years after successful grass pollen AIT [112, 113]. Reduced basophil responsiveness after AIT was confirmed by another study, implying that IgG antibodies compete with allergen for blocking of basophil surface FcεRIIb receptors [114]; However, whole blood basophils did not prove to be sufficient biomarker for adverse effects or early clinical responses onset in AIT [115].
Despite reports of circulating basophil decrease in allergic asthma [104, 116], possibly due to recruitment to the airway mucosa in the late phase response, changes in blood basophil numbers are not consistent in AR. However, basophil responsiveness seems to be associated with allergic inflammatory responses in AR and therapeutic success of AIT.
Thrombocytes
Beside their established role in coagulation, findings from animal studies with induced platelet depletion have shown that thrombocytes are also clearly involved in allergic disease [117, 118]. In human subjects, low-affinity and high-affinity IgE receptors on the membrane of platelets, as well as TLR2, TLR4, TLR9 innate immune receptors provide a potential link to allergic inflammatory responses. [119]. Platelets form complexes with leukocytes, supporting their recruitment into tissues in response to inflammatory stimuli; circulating platelet-leukocyte complexes, displaying α-M subunits (CD11b), which promote leukocyte attachment to the vascular epithelium, have been described [117]. A similar finding has been reported for platelet P-selectin associated promoting of endothelial eosinophil attachment [120]. CD40 ligand on activated platelets promotes antigen presentation to the adaptive immune response inducing DCs maturation and Th2 polarization responses following allergen challenge [121]. In allergic asthma, platelets have been shown to undergo chemotaxis after allergen exposure in vitro [122] and also contribute to acute bronchoconstriction, bronchial hyper-reactivity, immune cell infiltration and airway remodeling [6]. In lethal status asthmaticus increased megakaryocytes numbers were found in lung circulation [123].
Data on circulating thrombocyte dynamics during allergen challenge in AR are lacking, but an impairment of platelet aggregation correlating with IgE levels was previously shown [124]. Serum PF-4 and β-TG levels in HDM AR patients appear to be comparable to those in healthy controls [125]. Incidentally, we found a significant increase in circulating thrombocytes after 2 h of continuous allergen challenge compared to baseline values [8, 9]; however, 4 h after allergen challenge, no significant changes in circulating thrombocyte numbers were observed (data not published). During AIT in grass pollen AR, no changes in platelet activation marker β-TG levels were observed in plasma, even with during administration of the highest vaccine dose [126].
Little is known about circulating platelets in AR. Analogous to findings in allergic asthma, recruitment of circulating platelets to airway mucosa in the early phase of AR with subsequent support of effector cell adhesion and extravasation into the inflammation site is possible, but remains to be evaluated.
Erythrocytes
While the main role of red blood cells (RBC) is oxygen transportation, their crosstalk with immune cells has recently gained interest. DAMPs such as heme, Hsp70 and IL-33 have been identified in RBCs [127, 128], which are released into circulation upon intravascular hemolysis. If not neutralized by scavenger proteins, RBC-derived DAMPs can potentiate systemic inflammatory responses. In a model of allergy-induced anaphylaxis [129] a decrease in circulating RBCs was observed as a potential result of aggregation of erythrocytes, leucocytes and platelets; RBC adhesion to activated neutrophils and platelets might cause thrombosis in lowered blood flow settings and hypoxia [129, 130]. Anaphylaxis-associated hypoxia has been shown to result in a H2O2 release from RBCs leading to neutrophils chemotaxis [131].
An involvement of erythrocytes in the allergic immune response has not yet been established. In AR subjects, free hemoglobin has been found in nasal lavage after allergen challenge (micro-epistaxis), possibly as a result of increased vascular permeability [132]. We recently reported significant decreases of circulating RBCs and hematocrit in AR after 2 h, 4 h and 6 h of continuous allergen exposure in a specialized challenge chamber [8, 9]. Due to the concomitant increase in segmented neutrophils, we hypothesized a mechanical trapping of circulating erythrocytes in the airway capillaries by NETs. LT-induced eryptosis during the acute allergic inflammatory response could potentially contribute to this highly significant circulating RBC decrease after allergen challenge.
Taken together, decrease of erythrocytes during the early allergic immune response in AR has been observed. A contribution of RBCs to inflammation by release of DAMPs and ROS for neutrophil chemotaxis remains to be evaluated in mechanistic studies.
The cellular orchestra in AR
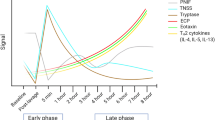
Upon allergen encounter there is a pull of circulating blood cells to the local allergic reaction site in the nasal mucosa in AR (Fig. 1). Neutrophils are recruited to the nasal mucosa in the early phase of the inflammatory response as first-line defense of the innate immune system; beside direct damage induced by certain allergens (e.g. with enzymatic properties), neutrophil-derived cytokines and release of cytotoxic mediators support epithelia damage and nerve ending disturbance (edema, rhinorrhea, vasomotor symptoms). Specific circulating lymphocyte subtypes (e.g. ILC2) accumulate in the nasal mucosa based on cytokines released by damaged epithelial cells (e.g. TSLP, IL-25, IL-33) and Th2 cytokines, which further lead to eosinophil maturation, recruitment and survival in the late phase contributing to further epithelial damage and microvascular leaking. Basophils influx amplifies IgE-mediated mediator release (e.g. histamine, leukotrienes) supporting symptomatic inflammation along with local mast cells. Blood monocytes functionally differentiate into DCs and tissue macrophages, thus participating in the promotion but also in the resolution of the Th2 inflammatory response. After allergen immunotherapy, Bregs and Tregs access the nasal mucosa and initiate immune-modulation via IL-10 release and induction of antibody class switching from IgE to IgG.
How circulating blood cells participate in allergic rhinitis (AR). Allergen exposure initiates a local inflammatory response involving recruitment of circulating blood cells to the nasal mucosa. In the early phase, neutrophils are mobilized as first-line responders of the innate immune system and contribute to epithelial and nerve damage via cytotoxic mediator release. Damaged epithelial cells release DAMPs and cytokines (e.g. TSLP, IL-25, IL-33) recruiting circulating lymphocyte subtypes (e.g. ILC2), which accumulate in the nasal mucosa and promote the Th2 inflammatory response. In the late phase, mediator release from recruited eosinophils and basophils further contributes to AR symptoms via epithelial damage and microvascular leaking. Blood-derived monocytes participate in promotion and resolution of the allergic response by differentiation into DCs and tissue macrophages. Boxes below the cartoon illustrate different blood cells and their reported changes after allergen exposure. DC, dendritic cell; ECP, eosinophil cationic protein; ILC, Innate Lymphoid Cell; MBP, major basic protein; MMP, matrix metalloprotease; NET, neutrophil extracellular trap; RBC, red blood cell; ROS, reactive oxygen species; for simplicity, IgE-mediated mechanisms are not illustrated
Conclusions
For all of the reasons discussed above, the view on the nasal mucosa as an isolated organ has to be corrected. Multiple evidence for the involvement of circulating blood cells is provided for all phases of the allergic inflammatory response (Table 1). Overall, in vivo reports are consistently reporting an early increase in circulating segmented neutrophils followed by a delayed elevation in peripheral ILC2 and eosinophils numbers upon allergen exposure in AR, implying their recruitment in the nasal mucosa. Besides the resulting elevation in circulating leukocytes, a rapid decrease in erythrocytes and, to a lesser extent, changes in thrombocyte numbers reflect a systemic impact of the acute inflammatory AR reaction. Regarding the effects of AIT, the most striking associations between blood cell numbers and therapy success seem to be changes in circulating T cell subsets and their respective cytokines, namely lower Th2, Th9 and Th17 in favor of higher Th1 and Treg cell numbers.
Abbreviations
- AIT:
-
Allergen-specific immunotherapy
- AR:
-
Allergic rhinitis
- BCR:
-
B cell receptor
- Breg :
-
Regulatory B cell
- CSF:
-
Colony stimulating factor
- CysLT:
-
Cysteinyl leukotriene
- DAMPs:
-
Damage-associated molecular patterns
- DCs:
-
Dendritic cells
- HDM:
-
House dust mite
- IFN:
-
Interferon
- IL:
-
Interleukin
- ILC :
-
Innate lymphoid cell
- LT:
-
Leukotriene
- NET:
-
Neutrophil extracellular trap
- NK:
-
Natural killer cell
- RBC:
-
Red blood cell
- ROS:
-
Reactive oxygen species
- Tc:
-
T cytotoxic cell
- TCR:
-
T cell receptor
- Tfh:
-
T follicular helper cell
- TGF:
-
Transforming growth factor
- Th:
-
T helper cell
- Th0:
-
Naïve T helper cell
- Treg :
-
Regulatory T cell
- TSLP:
-
Thymic stromal lymphopoietin
References
Scarupa MD, Kaliner MA. In-Depth Review of Allergic rhinitis [http://www.worldallergy.org/education-and-programs/education/allergic-disease-resource-center/professionals/in-depth-review-of-allergic-rhinitis].
Braunstahl GJ, Hellings PW. Nasobronchial interaction mechanisms in allergic airways disease. Curr Opin Otolaryngol Head Neck Surg. 2006;14:176–82.
Denburg JA. The origins of basophils and eosinophils in allergic inflammation. J Allergy Clin Immunol. 1998;102:S74–6.
Saini S, Bloom DC, Bieneman A, Vasagar K, Togias A, Schroeder J. Systemic effects of allergen exposure on blood basophil IL-13 secretion and FcepsilonRIbeta. J Allergy Clin Immunol. 2004;114:768–74.
Zhang H, Cardell LO, Bjorkander J, Benson M, Wang H. Comprehensive profiling of peripheral immune cells and subsets in patients with intermittent allergic rhinitis compared to healthy controls and after treatment with glucocorticoids. Inflammation. 2013;36:821–9.
Page C, Pitchford S. Platelets and allergic inflammation. Clin Exp Allergy. 2014;44:901–13.
Pitchford SC. Defining a role for platelets in allergic inflammation. Biochem Soc Trans. 2007;35:1104–8.
Jordakieva G, Kundi M, Lemell P, Zieglmayer R, Zieglmayer P, Godnic-Cvar J, Jensen-Jarolim E. Sublingual house dust mite immunotherapy has no impact on decrease of circulating erythrocytes upon airway allergen challenge in allergic rhinitis. Sci Rep. 2017;7:2555.
Jordakieva G, Wallmann J, Schmutz R, Lemell P, Wegmann M, Nittke T, Mittlbock M, Fehrenbach H, Godnic-Cvar J, Zieglmayer R, Jensen-Jarolim E. Peripheral erythrocytes decrease upon specific respiratory challenge with grass pollen allergen in sensitized mice and in human subjects. PLoS One. 2014;9:e86701.
Hansen I, Klimek L, Mosges R, Hormann K. Mediators of inflammation in the early and the late phase of allergic rhinitis. Curr Opin Allergy Clin Immunol. 2004;4:159–63.
Kratzer B, Pickl WF. Years in review: recent progress in cellular Allergology. Int Arch Allergy Immunol. 2016;169:1–12.
Kirmaz C, Ozenturk Kirgiz O, Bayrak P, Yilmaz O, Vatansever S, Ozbilgin K, Onur E, Celik O, Sogut A, Ay G, Yuksel H. Effects of allergen-specific immunotherapy on functions of helper and regulatory T cells in patients with seasonal allergic rhinitis. Eur Cytokine Netw. 2011;22:15–23.
Imada M, Simons FE, Jay FT, Hayglass KT. Allergen-stimulated interleukin-4 and interferon-gamma production in primary culture: responses of subjects with allergic rhinitis and normal controls. Immunology. 1995;85:373–80.
Sogut A, Yilmaz O, Kirmaz C, Ozbilgin K, Onur E, Celik O, Pinar E, Vatansever S, Dinc G, Yuksel H. Regulatory-T, T-helper 1, and T-helper 2 cell differentiation in nasal mucosa of allergic rhinitis with olive pollen sensitivity. Int Arch Allergy Immunol. 2012;157:349–53.
Francis JN, Lloyd CM, Sabroe I, Durham SR, Till SJ. T lymphocytes expressing CCR3 are increased in allergic rhinitis compared with non-allergic controls and following allergen immunotherapy. Allergy. 2007;62:59–65.
Gu ZW, Wang YX, Cao ZW. Neutralization of interleukin-17 suppresses allergic rhinitis symptoms by downregulating Th2 and Th17 responses and upregulating the Treg response. Oncotarget. 2017;8:22361–9.
Wang XQ, Hu GH, Kang HY, Shen Y, Ke X, Hong SL. High frequency of T helper type 9 cells in Chinese patients with allergic rhinitis. Asian Pac J Allergy Immunol. 2015;33:301–7.
Tang J, Xiao P, Luo X, Bai J, Xia W, Chen W, Li J, Yu Q, Shi S, Xu Y, et al. Increased IL-22 level in allergic rhinitis significantly correlates with clinical severity. Am J Rhinol Allergy. 2014;28:197–201.
Gomez E, Fernandez TD, Dona I, Rondon C, Campo P, Gomez F, Salas M, Gonzalez M, Perkins JR, Palomares F, et al. Initial immunological changes as predictors for house dust mite immunotherapy response. Clin Exp Allergy. 2015;45:1542–53.
Xuekun H, Qintai Y, Yulian C, Gehua Z. Correlation of gammadelta-T-cells, Th17 cells and IL-17 in peripheral blood of patients with allergic rhinitis. Asian Pac J Allergy Immunol. 2014;32:235–9.
Huang X, Chen Y, Zhang F, Yang Q, Zhang G. Peripheral Th17/Treg cell-mediated immunity imbalance in allergic rhinitis patients. Braz J Otorhinolaryngol. 2014;80:152–5.
Schramm A, Jasiewicz-Honkisz B, Osmenda G, Wilk G, Siedlinski M, Sagan A, Matusik PT, Maciag J, Sliwa T, Czesnikiewicz-Guzik M, Mikolajczyk TP. Th17 responses are not altered by natural exposure to seasonal allergens in pollen-sensitive patients. Allergy Asthma Clin Immunol. 2016;12:55.
Okubo K, Kurono Y, Ichimura K, Enomoto T, Okamoto Y, Kawauchi H, Suzaki H, Fujieda S, Masuyama K. Japanese guidelines for allergic rhinitis 2017. Allergol Int. 2017;66:205–19.
Ballesteros-Tato A, Randall TD, Lund FE, Spolski R, Leonard WJ, Leon B. T follicular helper cell plasticity shapes pathogenic T helper 2 cell-mediated immunity to inhaled house dust mite. Immunity. 2016;44:259–73.
Leomicronn B. T cells in allergic asthma: key players beyond the Th2 pathway. Curr Allergy Asthma Rep. 2017;17:43.
Kim AS, Doherty TA, Karta MR, Das S, Baum R, Rosenthal P, Beppu A, Miller M, Kurten R, Broide DH. Regulatory B cells and T follicular helper cells are reduced in allergic rhinitis. J Allergy Clin Immunol. 2016;138:1192–5. e1195
Akiyama M, Suzuki K, Yamaoka K, Yasuoka H, Takeshita M, Kaneko Y, Kondo H, Kassai Y, Miyazaki T, Morita R, et al. Number of circulating follicular helper 2 T cells correlates with IgG4 and Interleukin-4 levels and Plasmablast numbers in IgG4-related disease. Arthritis Rheumatol. 2015;67:2476–81.
Pawankar R. Gammadelta T cells in allergic airway diseases. Clin Exp Allergy. 2000;30:318–23.
Korematsu S, Tanaka Y, Nagakura T, Minato N, Izumi T. Human gammadelta T cells modulate the mite allergen-specific T-helper type 2-skewed immunity. Clin Exp Allergy. 2007;37:1681–7.
Vercelli D, Jabara HH, Arai K, Geha RS. Induction of human IgE synthesis requires interleukin 4 and T/B cell interactions involving the T cell receptor/CD3 complex and MHC class II antigens. J Exp Med. 1989;169:1295–307.
Huang XK, Yang QT, Chen YL, Zhang FC, Zhang GH: [expression of peripheral blood gammadelta T cells, treg cells and cytokines IL-17 and TGF-beta1 in patients with allergic rhinitis]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2013, 48:544–548.
Seddiki N, Santner-Nanan B, Martinson J, Zaunders J, Sasson S, Landay A, Solomon M, Selby W, Alexander SI, Nanan R, et al. Expression of interleukin (IL)-2 and IL-7 receptors discriminates between human regulatory and activated T cells. J Exp Med. 2006;203:1693–700.
Skrindo I, Scheel C, Johansen FE, Jahnsen FL. Experimentally induced accumulation of Foxp3(+) T cells in upper airway allergy. Clin Exp Allergy. 2011;41:954–62.
Radulovic S, Jacobson MR, Durham SR, Nouri-Aria KT. Grass pollen immunotherapy induces Foxp3-expressing CD4+ CD25+ cells in the nasal mucosa. J Allergy Clin Immunol. 2008;121:1467–72. 1472 e1461
Zeng H, Zhang R, Jin B, Chen L. Type 1 regulatory T cells: a new mechanism of peripheral immune tolerance. Cell Mol Immunol. 2015;12:566–71.
Han D, Wang C, Lou W, Gu Y, Wang Y, Zhang L. Allergen-specific IL-10-secreting type I T regulatory cells, but not CD4(+)CD25(+)Foxp3(+) T cells, are decreased in peripheral blood of patients with persistent allergic rhinitis. Clin Immunol. 2010;136:292–301.
Li L, Sad S, Kagi D, Mosmann TR. CD8Tc1 and Tc2 cells secrete distinct cytokine patterns in vitro and in vivo but induce similar inflammatory reactions. J Immunol. 1997;158:4152–61.
Sad S, Marcotte R, Mosmann TR. Cytokine-induced differentiation of precursor mouse CD8+ T cells into cytotoxic CD8+ T cells secreting Th1 or Th2 cytokines. Immunity. 1995;2:271–9.
Gluck J, Rogala B, Rogala E, Oles E. Allergen immunotherapy in intermittent allergic rhinitis reduces the intracellular expression of IL-4 by CD8+ T cells. Vaccine. 2007;26:77–81.
Qiu S, Du Y, Duan X, Geng X, Xie J, Gao H, Yang PC. Cytotoxic T lymphocytes mediate chronic inflammation of the nasal mucosa of patients with atypical allergic rhinitis. N Am J Med Sci. 2011;3:378–83.
Bratke K, Haupt F, Kuepper M, Bade B, Faehndrich S, Luttmann W, Virchow JC Jr. Decrease of cytotoxic T cells in allergic asthma correlates with total serum immunglobulin E. Allergy. 2006;61:1351–7.
Kus J, Tse KS, Enarson D, Grzybowski S, Chan-Yeung M. Lymphocyte subpopulations in patients with allergic rhinitis. Allergy. 1984;39:509–14.
Ambach A, Bonnekoh B, Gollnick H. Perforin hyperreleasability and depletion in cytotoxic T cells from patients with exacerbated atopic dermatitis and asymptomatic rhinoconjunctivitis allergica. J Allergy Clin Immunol. 2001;107:878–86.
Pawankar RU, Okuda M, Okubo K, Ra C. Lymphocyte subsets of the nasal mucosa in perennial allergic rhinitis. Am J Respir Crit Care Med. 1995;152:2049–58.
Pawankar R, Ra C. Heterogeneity of mast cells and T cells in the nasal mucosa. J Allergy Clin Immunol. 1996;98:S248–62.
Scanlon ST, McKenzie AN. The messenger between worlds: the regulation of innate and adaptive type-2 immunity by innate lymphoid cells. Clin Exp Allergy. 2015;45:9–20.
Karta MR, Broide DH, Doherty TA. Insights into group 2 innate lymphoid cells in human airway disease. Curr Allergy Asthma Rep. 2016;16:8.
Ho J, Bailey M, Zaunders J, Mrad N, Sacks R, Sewell W, Harvey RJ. Group 2 innate lymphoid cells (ILC2s) are increased in chronic rhinosinusitis with nasal polyps or eosinophilia. Clin Exp Allergy. 2015;45:394–403.
Dhariwal J, Cameron A, Trujillo-Torralbo MB, Del Rosario A, Bakhsoliani E, Paulsen M, Jackson DJ, Edwards MR, Rana BMJ, Cousins DJ, et al. Mucosal type 2 innate lymphoid cells are a key component of the allergic response to aeroallergens. Am J Respir Crit Care Med. 2017;195:1586–96.
Doherty TA, Scott D, Walford HH, Khorram N, Lund S, Baum R, Chang J, Rosenthal P, Beppu A, Miller M, Broide DH. Allergen challenge in allergic rhinitis rapidly induces increased peripheral blood type 2 innate lymphoid cells that express CD84. J Allergy Clin Immunol. 2014;133:1203–5.
Lao-Araya M, Steveling E, Scadding GW, Durham SR, Shamji MH. Seasonal increases in peripheral innate lymphoid type 2 cells are inhibited by subcutaneous grass pollen immunotherapy. J Allergy Clin Immunol. 2014;134:1193–5. e1194
Fan D, Wang X, Wang M, Wang Y, Zhang L, Li Y, Fan E, Cao F, Van Crombruggen K, Zhang L. Allergen-dependent differences in ILC2s frequencies in patients with allergic rhinitis. Allergy Asthma Immunol Res. 2016;8:216–22.
Bartemes KR, Kephart GM, Fox SJ, Kita H. Enhanced innate type 2 immune response in peripheral blood from patients with asthma. J Allergy Clin Immunol. 2014;134:671–8. e674
Leon B, Ballesteros-Tato A, Lund FE. Dendritic cells and B cells: unexpected partners in Th2 development. J Immunol. 2014;193:1531–7.
De Schryver E, Devuyst L, Derycke L, Dullaers M, Van Zele T, Bachert C, Gevaert P. Local immunoglobulin e in the nasal mucosa: clinical implications. Allergy Asthma Immunol Res. 2015;7:321–31.
Cameron L, Gounni AS, Frenkiel S, Lavigne F, Vercelli D, Hamid Q. S epsilon S mu and S epsilon S gamma switch circles in human nasal mucosa following ex vivo allergen challenge: evidence for direct as well as sequential class switch recombination. J Immunol. 2003;171:3816–22.
Wong KJ, Timbrell V, Xi Y, Upham JW, Collins AM, Davies JM. IgE+ B cells are scarce, but allergen-specific B cells with a memory phenotype circulate in patients with allergic rhinitis. Allergy. 2015;70:420–8.
Perez-Andres M, Paiva B, Nieto WG, Caraux A, Schmitz A, Almeida J, Vogt RF Jr, Marti GE, Rawstron AC, Van Zelm MC, et al. Human peripheral blood B-cell compartments: a crossroad in B-cell traffic. Cytometry B Clin Cytom. 2010;78(Suppl 1):S47–60.
Henriques A, Nunes R, Loureiro G, Martinho A, Pais M, Segorbe-Luis A, Trindade H, Pereira C, Paiva A. Alterations on peripheral blood B cell subsets induced by allergic rhinitis. Inflamm Res. 2015;64:145–9.
Jen HY, Yang YH, Chiang BL, Chuang YH. Upregulated interleukin-21 receptor on B cells associated with the downregulation of IgE in patients with allergic rhinitis. J Interf Cytokine Res. 2015;35:42–8.
Kamekura R, Shigehara K, Miyajima S, Jitsukawa S, Kawata K, Yamashita K, Nagaya T, Kumagai A, Sato A, Matsumiya H, et al. Alteration of circulating type 2 follicular helper T cells and regulatory B cells underlies the comorbid association of allergic rhinitis with bronchial asthma. Clin Immunol. 2015;158:204–11.
Mesdaghi M, Vodjgani M, Salehi E, Hadjati J, Sarrafnejad A, Bidad K, Berjisian F. Natural killer cells in allergic rhinitis patients and nonatopic controls. Int Arch Allergy Immunol. 2010;153:234–8.
Kim JH, Gong CH, Choi GE, Kim SA, Kim HS, Jang YJ. Natural killer cell deficits aggravate allergic rhinosinusitis in a murine model. ORL J Otorhinolaryngol Relat Spec. 2016;78:199–207.
El-Shazly AE, Lefebvre PP. Modulation of NK cell autocrine-induced eosinophil chemotaxis by interleukin-15 and vitamin D(3): a possible NK-eosinophil crosstalk via IL-8 in the pathophysiology of allergic rhinitis. Mediat Inflamm. 2011;2011:373589.
El-Shazly AE, Doloriert HC, Bisig B, Lefebvre PP, Delvenne P, Jacobs N. Novel cooperation between CX3CL1 and CCL26 inducing NK cell chemotaxis via CX3CR1: a possible mechanism for NK cell infiltration of the allergic nasal tissue. Clin Exp Allergy. 2013;43:322–31.
Ziegler-Heitbrock L. The CD14+ CD16+ blood monocytes: their role in infection and inflammation. J Leukoc Biol. 2007;81:584–92.
Jiang Z, Zhu L. Update on the role of alternatively activated macrophages in asthma. J Asthma Allergy. 2016;9:101–7.
Hirano M, Ogita-Nakanishi H, Miyachi W, Hannya N, Yamamoto-Kimoto Y, Sakurai K, Miyoshi-Higashino M, Tashiro-Yamaji J, Kato R, Ijiri Y, et al. Essential role of macrophages in the initiation of allergic rhinitis in mice sensitized intranasally once with cedar pollen: regulation of class switching of immunoglobulin in B cells by controlling interleukin-4 production in T cells of submandibular lymph nodes. Microbiol Immunol. 2012;56:392–405.
Eguiluz-Gracia I, Bosco A, Dollner R, Melum GR, Lexberg MH, Jones AC, Dheyauldeen SA, Holt PG, Baekkevold ES, Jahnsen FL. Rapid recruitment of CD14(+) monocytes in experimentally induced allergic rhinitis in human subjects. J Allergy Clin Immunol. 2016;137:1872–81. e1812
Sihra BS, Kon OM, Grant JA, Kay AB. Expression of high-affinity IgE receptors (fc epsilon RI) on peripheral blood basophils, monocytes, and eosinophils in atopic and nonatopic subjects: relationship to total serum IgE concentrations. J Allergy Clin Immunol. 1997;99:699–706.
Melewicz FM, Zeiger RS, Mellon MH, O'Connor RD, Spiegelberg HL. Increased peripheral blood monocytes with fc receptors for IgE in patients with severe allergic disorders. J Immunol. 1981;126:1592–5.
Moniuszko M, Kowal K, Jeznach M, Rusak M, Dabrowska M, Bodzenta-Lukaszyk A. Phenotypic correlations between monocytes and CD4+ T cells in allergic patients. Int Arch Allergy Immunol. 2013;161:131–41.
Greer AM, Wu N, Putnam AL, Woodruff PG, Wolters P, Kinet JP, Shin JS. Serum IgE clearance is facilitated by human FcepsilonRI internalization. J Clin Invest. 2014;124:1187–98.
Yamanaka K, Yuta A, Kakeda M, Kitagawa H, Ogihara H, Gabazza EC, Okubo K, Kurokawa I, Takeuchi K, Mizutani H. SLIT improves cedar pollinosis by restoring IL-10 production from Tr1 and monocytes approximately IL-10 productivity is critical for becoming allergic approximately. Allergol Int. 2011;60:45–51.
Luo X, Han M, Liu J, Wang Y, Luo X, Zheng J, Wang S, Liu Z, Liu D, Yang PC, Li H. Epithelial cell-derived micro RNA-146a generates interleukin-10-producing monocytes to inhibit nasal allergy. Sci Rep. 2015;5:15937.
Bellinghausen I, Brand U, Steinbrink K, Enk AH, Knop J, Saloga J. Inhibition of human allergic T-cell responses by IL-10-treated dendritic cells: differences from hydrocortisone-treated dendritic cells. J Allergy Clin Immunol. 2001;108:242–9.
Novak N, Allam JP, Betten H, Haberstok J, Bieber T. The role of antigen presenting cells at distinct anatomic sites: they accelerate and they slow down allergies. Allergy. 2004;59:5–14.
Jahnsen FL, Lund-Johansen F, Dunne JF, Farkas L, Haye R, Brandtzaeg P. Experimentally induced recruitment of plasmacytoid (CD123high) dendritic cells in human nasal allergy. J Immunol. 2000;165:4062–8.
Lambrecht BN. The dendritic cell in allergic airway diseases: a new player to the game. Clin Exp Allergy. 2001;31:206–18.
Pilette C, Jacobson MR, Ratajczak C, Detry B, Banfield G, VanSnick J, Durham SR, Nouri-Aria KT. Aberrant dendritic cell function conditions Th2-cell polarization in allergic rhinitis. Allergy. 2013;68:312–21.
Shen C, Hupin C, Froidure A, Detry B, Pilette C. Impaired ICOSL in human myeloid dendritic cells promotes Th2 responses in patients with allergic rhinitis and asthma. Clin Exp Allergy. 2014;44:831–41.
Akdis CA, Akdis M. Mechanisms of allergen-specific immunotherapy and immune tolerance to allergens. World Allergy Organ J. 2015;8:17.
Tversky JR, Bieneman AP, Chichester KL, Hamilton RG, Schroeder JT. Subcutaneous allergen immunotherapy restores human dendritic cell innate immune function. Clin Exp Allergy. 2010;40:94–102.
Bratke K, Lommatzsch M, Julius P, Kuepper M, Kleine HD, Luttmann W, Christian Virchow J. Dendritic cell subsets in human bronchoalveolar lavage fluid after segmental allergen challenge. Thorax. 2007;62:168–75.
Upham JW, Denburg JA, O'Byrne PM. Rapid response of circulating myeloid dendritic cells to inhaled allergen in asthmatic subjects. Clin Exp Allergy. 2002;32:818–23.
Lavinskiene S, Jeroch J, Malakauskas K, Bajoriuniene I, Jackute J, Sakalauskas R. Peripheral blood neutrophil activity during Dermatophagoides pteronyssinus-induced late-phase airway inflammation in patients with allergic rhinitis and asthma. Inflammation. 2012;35:1600–9.
Arebro J, Ekstedt S, Hjalmarsson E, Winqvist O, Kumlien Georen S, Cardell LO. A possible role for neutrophils in allergic rhinitis revealed after cellular subclassification. Sci Rep. 2017;7:43568.
Chen J, Zhou Y, Zhang L, Wang Y, Pepper AN, Cho SH, Kong W. Individualized treatment of allergic rhinitis according to nasal cytology. Allergy Asthma Immunol Res. 2017;9:403–9.
Fransson M, Benson M, Wennergren G, Cardell LO. A role for neutrophils in intermittent allergic rhinitis. Acta Otolaryngol. 2004;124:616–20.
Bochenska-Marciniak M, Kupczyk M, Gorski P, Kuna P. The effect of recombinant interleukin-8 on eosinophils' and neutrophils' migration in vivo and in vitro. Allergy. 2003;58:795–801.
Braido F, Riccio AM, Rogkakou A, Massacane P, Guerra L, Fumagalli F, Stagi E, Balestracci S, Porcu A, Canonica GW. Montelukast effects on inflammation in allergic rhinitis: a double blind placebo controlled pilot study. Eur Ann Allergy Clin Immunol. 2012;44:48–53.
Nussbaum JC, Van Dyken SJ, von Moltke J, Cheng LE, Mohapatra A, Molofsky AB, Thornton EE, Krummel MF, Chawla A, Liang HE, Locksley RM. Type 2 innate lymphoid cells control eosinophil homeostasis. Nature. 2013;502:245–8.
Canonica GW, Compalati E. Minimal persistent inflammation in allergic rhinitis: implications for current treatment strategies. Clin Exp Immunol. 2009;158:260–71.
Semik-Orzech A, Barczyk A, Wiaderkiewicz R, Pierzchala W. Eotaxin, but not IL-8, is increased in upper and lower airways of allergic rhinitis subjects after nasal allergen challenge. Allergy Asthma Proc. 2011;32:230–8.
Górski P, Wittczak T, Walusiak J, Pałczyński C, Ruta U, Kuna P, Alam R. Eotaxin but not MCP−3 induces eosinophil influx into nasal fluid in allergic patients. Allergy. 2002;57:519–28.
Hanazawa T, Antuni JD, Kharitonov SA, Barnes PJ. Intranasal administration of eotaxin increases nasal eosinophils and nitric oxide in patients with allergic rhinitis. J Allergy Clin Immunol. 2000;105:58–64.
Ciprandi G, Vizzaccaro A, Cirillo I, Tosca M, Massolo A, Passalacqua G. Nasal eosinophils display the best correlation with symptoms, pulmonary function and inflammation in allergic rhinitis. Int Arch Allergy Immunol. 2005;136:266–72.
Wilson AM, Duong M, Crawford L, Denburg J. An evaluation of peripheral blood eosinophil/basophil progenitors following nasal allergen challenge in patients with allergic rhinitis. Clin Exp Allergy. 2005;35:39–44.
Beeh KM, Beier J, Kornmann O, Meier C, Taeumer T, Buhl R. A single nasal allergen challenge increases induced sputum inflammatory markers in non-asthmatic subjects with seasonal allergic rhinitis: correlation with plasma interleukin-5. Clin Exp Allergy. 2003;33:475–82.
Malm-Erjefalt M, Greiff L, Ankerst J, Andersson M, Wallengren J, Cardell LO, Rak S, Persson CG, Erjefalt JS. Circulating eosinophils in asthma, allergic rhinitis, and atopic dermatitis lack morphological signs of degranulation. Clin Exp Allergy. 2005;35:1334–40.
Lavinskiene S, Malakauskas K, Jeroch J, Hoppenot D, Sakalauskas R. Functional activity of peripheral blood eosinophils in allergen-induced late-phase airway inflammation in asthma patients. J Inflamm (Lond). 2015;12:25.
Knol EF, Mul FP, Lie WJ, Verhoeven AJ, Roos D. The role of basophils in allergic disease. Eur Respir J Suppl. 1996;22:126s–31s.
Wang H, Mobini R, Fang Y, Barrenas F, Zhang H, Xiang Z, Benson M. Allergen challenge of peripheral blood mononuclear cells from patients with seasonal allergic rhinitis increases IL-17RB, which regulates basophil apoptosis and degranulation. Clin Exp Allergy. 2010;40:1194–202.
Ando N, Nakamura Y, Ishimaru K, Ogawa H, Okumura K, Shimada S, Nakao A. Allergen-specific basophil reactivity exhibits daily variations in seasonal allergic rhinitis. Allergy. 2015;70:319–22.
Bascom R, Wachs M, Naclerio RM, Pipkorn U, Galli SJ, Lichtenstein LM. Basophil influx occurs after nasal antigen challenge: effects of topical corticosteroid pretreatment. J Allergy Clin Immunol. 1988;81:580–9.
Gorski P, Krakowiak A, Ruta U. Nasal and bronchial responses to flour-inhalation in subjects with occupationally induced allergy affecting the airway. Int Arch Occup Environ Health. 2000;73:488–97.
KleinJan A, McEuen AR, Dijkstra MD, Buckley MG, Walls AF, Fokkens WJ. Basophil and eosinophil accumulation and mast cell degranulation in the nasal mucosa of patients with hay fever after local allergen provocation. J Allergy Clin Immunol. 2000;106:677–86.
Haenuki Y, Matsushita K, Futatsugi-Yumikura S, Ishii KJ, Kawagoe T, Imoto Y, Fujieda S, Yasuda M, Hisa Y, Akira S, et al. A critical role of IL-33 in experimental allergic rhinitis. J Allergy Clin Immunol. 2012;130:184–94. e111
Kuna P, Alam R, Ruta U, Gorski P. RANTES induces nasal mucosal inflammation rich in eosinophils, basophils, and lymphocytes in vivo. Am J Respir Crit Care Med. 1998;157:873–9.
Shamji MH, Bellido V, Scadding GW, Layhadi JA, Cheung DK, Calderon MA, Asare A, Gao Z, Turka LA, Tchao N, et al. Effector cell signature in peripheral blood following nasal allergen challenge in grass pollen allergic individuals. Allergy. 2015;70:171–9.
Zidarn M, Kosnik M, Silar M, Grahek A, Korosec P. Rhinitis symptoms caused by grass pollen are associated with elevated basophile allergen sensitivity and a larger grass-specific immunoglobulin E fraction. Clin Exp Allergy. 2012;42:49–57.
Pedersen M, Kristensen KS, Clementsen P, Olsen OT, Skov PS, Permin H, Norn S: Increased numbers of circulating basophils with decreased releasability after administration of rhG-CSF to allergic patients. Agents Actions 1994, 41 Spec No:C24–C25.
Zidarn M, Kosnik M, Silar M, Bajrovic N, Korosec P. Sustained effect of grass pollen subcutaneous immunotherapy on suppression of allergen-specific basophil response; a real-life, nonrandomized controlled study. Allergy. 2015;70:547–55.
Shamji MH, Layhadi JA, Scadding GW, Cheung DK, Calderon MA, Turka LA, Phippard D, Durham SR. Basophil expression of diamine oxidase: a novel biomarker of allergen immunotherapy response. J Allergy Clin Immunol. 2015;135:913–21. e919
Van Overtvelt L, Baron-Bodo V, Horiot S, Moussu H, Ricarte C, Horak F, Zieglmayer P, Zieglmayer R, Montagut A, Galvain S, et al. Changes in basophil activation during grass-pollen sublingual immunotherapy do not correlate with clinical efficacy. Allergy. 2011;66:1530–7.
Dijkstra D, Hennig C, Hansen G, Biller H, Krug N, Hohlfeld JM. Identification and quantification of basophils in the airways of asthmatics following segmental allergen challenge. Cytometry A. 2014;85:580–7.
Pitchford SC, Yano H, Lever R, Riffo-Vasquez Y, Ciferri S, Rose MJ, Giannini S, Momi S, Spina D, O'Connor B, et al. Platelets are essential for leukocyte recruitment in allergic inflammation. J Allergy Clin Immunol. 2003;112:109–18.
Lellouch-Tubiana A, Lefort J, Simon MT, Pfister A, Vargaftig BB. Eosinophil recruitment into Guinea pig lungs after PAF-acether and allergen administration. Modulation by prostacyclin, platelet depletion, and selective antagonists. Am Rev Respir Dis. 1988;137:948–54.
Idzko M, Pitchford S, Page C. Role of platelets in allergic airway inflammation. J Allergy Clin Immunol. 2015;135:1416–23.
Pitchford SC, Momi S, Giannini S, Casali L, Spina D, Page CP, Gresele P. Platelet P-selectin is required for pulmonary eosinophil and lymphocyte recruitment in a murine model of allergic inflammation. Blood. 2005;105:2074–81.
Tian J, Zhu T, Liu J, Guo Z, Cao X. Platelets promote allergic asthma through the expression of CD154. Cell Mol Immunol. 2015;12:700–7.
Pitchford SC, Momi S, Baglioni S, Casali L, Giannini S, Rossi R, Page CP, Gresele P. Allergen induces the migration of platelets to lung tissue in allergic asthma. Am J Respir Crit Care Med. 2008;177:604–12.
Slater D, Martin J, Trowbridge A. The platelet in asthma. Lancet. 1985;1:110.
Gallagher JS, Bernstein IL, Maccia CA, Splansky GL, Glueck HI. Cyclic platelet dysfunction in IgE-mediated allergy. J Allergy Clin Immunol. 1978;62:229–35.
Kasperska-Zajac A, Rogala B. Markers of platelet activation in plasma of patients suffering from persistent allergic rhinitis with or without asthma symptoms. Clin Exp Allergy. 2005;35:1462–5.
Kasperska-Zajac A, Brzoza Z, Rogala B. Effect of allergen-specific immunotherapy on platelet secretory activity in patients with grass-pollen allergy. Vaccine. 2006;24:6990–3.
Buttari B, Profumo E, Rigano R. Crosstalk between red blood cells and the immune system and its impact on atherosclerosis. Biomed Res Int. 2015;2015:616834.
Mendonca R, Silveira AA, Conran N. Red cell DAMPs and inflammation. Inflamm Res. 2016;65:665–78.
Zimmerman GA. Hypoxic erythrocytes spark lung leukocyte adhesion. Blood. 2008;111:4831–2.
Goel MS, Diamond SL. Adhesion of normal erythrocytes at depressed venous shear rates to activated neutrophils, activated platelets, and fibrin polymerized from plasma. Blood. 2002;100:3797–803.
Kiefmann R, Rifkind JM, Nagababu E, Bhattacharya J. Red blood cells induce hypoxic lung inflammation. Blood. 2008;111:5205–14.
Park YJ, Repka-Ramirez MS, Naranch K, Velarde A, Clauw D, Baraniuk JN. Nasal lavage concentrations of free hemoglobin as a marker of microepistaxis during nasal provocation testing*. Allergy. 2002;57:329–35.
Acknowledgments
The authors thank Amelia Wein for proof reading.
Authors’ contribution
GJ designed the concept of the review, wrote the article and searched the literature. EJJ contributed to the scientific concept of this review and critically revised the manuscript. Both authors read and approved the final manuscript.
Funding
This study was supported by the Austrian Science Fund FWF, grant SFB F4606-B28 to EJJ.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Jordakieva, G., Jensen-Jarolim, E. The impact of allergen exposure and specific immunotherapy on circulating blood cells in allergic rhinitis. World Allergy Organ J 11, 19 (2018). https://doi.org/10.1186/s40413-018-0197-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40413-018-0197-0