Abstract
Immune checkpoint inhibitors (ICIs) targeting PD-1 or PD-L1 have emerged as a revolutionary treatment strategy for human cancer patients. However, as the response rate to ICI therapy varies widely among different types of tumours, we are beginning to gain insight into the mechanisms as well as biomarkers of therapeutic response and resistance. Numerous studies have highlighted the dominant role of cytotoxic T cells in determining the treatment response to ICIs. Empowered by recent technical advances, such as single-cell sequencing, tumour-infiltrating B cells have been identified as a key regulator in several solid tumours by affecting tumour progression and the response to ICIs. In the current review, we summarized recent advances regarding the role and underlying mechanisms of B cells in human cancer and therapy. Some studies have shown that B-cell abundance in cancer is positively associated with favourable clinical outcomes, while others have indicated that they are tumour-promoting, implying that the biological function of B cells is a complex landscape. The molecular mechanisms involved multiple aspects of the functions of B cells, including the activation of CD8+ T cells, the secretion of antibodies and cytokines, and the facilitation of the antigen presentation process. In addition, other crucial mechanisms, such as the functions of regulatory B cells (Bregs) and plasma cells, are discussed. Here, by summarizing the advances and dilemmas of recent studies, we depicted the current landscape of B cells in cancers and paved the way for future research in this field.
Graphical Abstract

Similar content being viewed by others
Introduction
Immune checkpoint inhibitor (ICI) therapy has now been established as a first-line treatment for multiple types of metastatic cancers. Many of these promising therapeutic strategies, which can lead to strong antitumour responses and even long-term tumour remission, are based on the blockade of the activation of immune inhibitory receptors such as programmed cell death protein 1 (PD-1), programmed cell death ligand 1 (PD-L1) and cytotoxic T lymphocyte–associated protein 4 (CTLA-4) [1, 2]. Unfortunately, only a minority of patients showed satisfactory responses to ICIs. Therefore, it is urgent to expand the understanding of the potential mechanisms leading to resistance to ICI therapy [3].
The tumour microenvironment (TME) is the environment in which tumours form and develop. It consists of stromal cells (including mesenchymal cells and endothelial cells), extracellular matrix, various cytokines and chemokines, and most importantly, various components of immune cells [4]. Accumulating evidence has suggested that the interaction between cancer cells and the TME reshapes the immune phenotype of cancers and thereby has profound effects on cancer initiation, progression, and therapeutic efficacy [5]. TME-mediated ICI resistance can be induced by cytokines secreted by tumour or stromal cells [6, 7]. Additionally, the interaction of tumour cells with stromal cells or components of the extracellular matrix can also blunt the therapeutic response [2]. Combinations of therapies targeting TME components and chemotherapy, radiation, or ICIs now appear to offer new approaches for cancer treatment. Driven by recently developed techniques such as single-cell sequencing and spatial transcriptomics, new subsets of immune cells in the TME have been defined and located [8, 9].
Tumour-infiltrating B cells are often colocalized with T cells or other immune cells, such as dendritic cells, in organized lymphoid aggregates known as tertiary lymphoid structures (TLSs). Substantial evidence suggests that the response to ICIs is positively correlated with the presence of B cells, particularly in TLSs [10]. Mechanistically, B cells secrete an array of cytokines (including TNF, interleukin (IL)-2, IL-6 and IFN-γ), through which they recruit other immune effector cells, including T cells [11, 12]. Memory B cells may act as antigen-presenting cells, driving the expansion of both memory and naive tumour-associated T-cell responses, and potentially contribute to the antitumour response by producing antibodies against tumours [13]. Moreover, B cells probably cooperate with the other key immune contexture within the TLS. However, recent studies have reported that B cells dampen the tumour immune response by producing certain cytokines, such as IL-10, IL-35, TGF-β and even gamma-aminobutyric acid (GABA) [14]. All these results indicate that B cells have heterogeneous subpopulations with distinct functions, contributing to pros as well as cons in antitumour immune responses. In this review, we summarized and updated recent findings pertaining to the classifications, functions, and mechanisms of B cells in cellular and humoral immune responses to cancer and their potential relevance to immunotherapy.
Phenotypes and functions of B cells in the TME
B-cell development and recruitment
B cells are derived from the bone marrow and then circulate and move to the spleen and lymph nodes. They participate in immune responses in the peripheral blood and immune zone. Naive B cells are activated in response to specific antigens during development and then differentiate and proliferate into plasma blasts or plasma cells (PCs), which are known as activated B cells. Depending on the function of differentiation, other B cells become memory B cells, follicular B cells or regulatory B cells (Bregs) [15, 16]. The epitopes of B cells change with the transformation and maturation of B cells, and the method of labelling B cells depends on the cluster of differentiation (CD), such as the well-known CD19, CD20, CD21, CD40, and CD79b. Furthermore, single-cell RNA sequencing (scRNA-seq) can be used to analyse the distributions and types of B cells in tissues, which is especially applicable to the heterogeneity of B cells in tumours [8]. We can define a richer B-cell phenotype to reveal the key mechanisms of tumour immunology.
B cells mainly exist in the form of a scattered distribution or TLSs in the TME and directly and indirectly exert effects on tumour cells through antigen presentation, antibody production or cytokine production. According to previous concepts, the infiltration of B cells in the TME can also be divided into the immune inflammatory type, immune excluded type and immune desert type [17]. The factors that influence B-cell recruitment are not fully understood. What is clear is that in addition to receiving antigen stimulation and BCR signalling, many cytokines are also involved in the regulation of the B-cell population and status. For example, IL-17 and CXCL12 can induce pro-B progenitor cells to grow into B cells and participate in the evolution of B cells [18]. INF-α, -β, and -γ produced by other immune cells, such as T cells, can also promote B-cell activation and plasma cell differentiation to produce antibodies [19, 20]. B cells are recruited to the mouse intestinal epithelium in response to CCL20 and CCL28 [21]. Moreover, B cells can transform into antigen-presenting cells (APCs) through the membrane-binding molecule CD40/CD40L induced by IL-4 and IL-21 [22, 23]. In the TME, the cytokine recruitment of B cells represented by CXCL13 is different from that in the normal immune environment [24].
APC
Acting as professional APCs is the crucial function of B cells in the TME. Compared with other APCs, antigens are recognized more sensitively by the BCR [25]. B cells enhance the density and response of T cells in the TME by activating T cells, especially CD4+ T cells [26]. On the one hand, B cells transform CD4+ T cells into an activated state, which enhances the density of T cells in the TME. On the other hand, B cells mediate the transformation of CD4+ T cells and CD8+ T cells to different functional subsets after receiving antigen stimulation and then strengthen the specific response of T cells [27]. In addition, B cells tend to be actively converted into effector B cells. Some subsets of B cells express surface markers, including MHCII, CD80 and CD86, and can maintain additional T-cell population expansion after dendritic cell (DC)-induced initial activation by acting as APCs [28]. B cells also affect other APCs and enhance their ability to present antigens, such as in DCs and macrophage antigen presentation. B cells affect the state of both and develop in the direction of promoting immunity [29]. The mechanism of B-cell recognition of cancer cell antigens is the focus of current research in B-cell treatment.
“Helper” of T cells
Elimination of B cells abrogates the activation of cytotoxic and helper T cells (CTL and Th) upon antigen stimulation, indicating that antigen-specific interactions between T cells and CD20+ B cells in the TME seem to be crucial to the protective role of T cells [30]. Intriguingly, activated CTLs can also engage with soluble CD27 secreted by CD19+ B cells, which promotes their survival and proliferation, suggesting a ‘helper’ role of B cells in the tumour immune response [31].
In several recent studies on TLSs in cancer, TLSs have been found to be strongly associated with a favourable prognosis. B cells, as the major component in TLSs, contribute significantly to T-cell immunity. Two major functions of TLSs are the mediation of T cells to enhance antitumour effects and the crosstalk of T and B cells to promote the maturation and development of TLSs. Corresponding to the abovementioned enhanced immunity to fight tumours is the anti-immune regulatory function of Bregs. Bregs suppress the immune activity of T cells and other immune cells by secreting related cytokines such as IL-10 and IL-35 [32]. B cells from the TME have the ability to play distinct roles by differentiating groups to affect the immune balance of the tumour.
The production of immune substances
B cells regulate immune function and the immune microenvironment by producing immune substances, including antibodies and cytokines. For cytokines produced by B cells, it has been clearly confirmed that IL-2 and IL-4 produced by B cells can induce Th cells to differentiate into Th1 and Th2 cells [33, 34], and IL-6 can induce the activation of regulatory T cells (Tregs) and promote the production of plasma cell antibodies [35]. B cells can produce IFN-α and IFN-γ to activate the cell-killing effect of NK cells [36]. In addition, Bregs produce cytokines to suppress immune function, including the secretion of IL-10, IL-35, and TGF-β by Bregs to inhibit T cell, DC, and macrophage function. In addition, Bregs can also exert inhibitory effects by the membrane-bound molecules CD39, CD73 and PD1 [37]. A higher proportion of Bregs is often found in advanced hepatocellular cancer (HCC), gastric cancer and prostate cancer, indicating that Bregs may influence tumour development and progression [38,39,40]. Moreover, Bregs also secrete cytokines such as TGF-β, which may differentiate naive CD4+ T cells into Tregs and transform macrophages into an M2 immunosuppressive phenotype, leading to remodelling of the TME [41, 42].
Antibody production is a specific ability of B cells, and increasing research points to the role of antibodies in tumours. During tumorigenesis, frequent missense mutations or alternative splicing events often result in the exposure of tumour-specific neoantigens that can drive the B-cell-mediated humoral immune response. With B-cell maturation confirmed, they perform clonal proliferation, selection for high-affinity antibodies and isotype switching within tumour-associated TLSs and in less organized structures, ultimately converting to effector or memory B cells and PCs [16, 43]. Furthermore, PCs and memory B cells themselves produce high titres of tumour-specific antibodies, inducing opsonization, complement-mediated lysis of cancer cells, antibody-dependent cell cytotoxicity (ADCC) executed by T cells or NK cells and antibody-mediated phagocytosis of tumour cells by macrophages in TLSs of the TME [10, 28]. Moreover, the IgG-type antibodies secreted by PCs can be directed to tumour-associated antigens, induce ADCC in bound tumour cells and enhance the complement pathway through FcγR activation, reflecting the role of B cells as the 'defender' [44,45,46,47]. These results confirm that B cells produce an emerging antitumour response that increases with TLSs and the TME.
Crosstalk of B cells with other immune cells in the TME
Obvious antitumour effects
Both B cells and other immune cell subsets in the TME interact with each other through multiple pathways to influence oncogenesis and might determine the response to immunotherapy. Substantial evidence suggests that B cells are the main partners of T cells in antitumour immunity. B-cell and T-cell aggregation in the TME has traditionally been considered a favourable prognostic feature, which has also been validated using single-cell techniques [48]. B cells can provide T cells with stronger signals, such as the inducible costimulator (ICOS) ligands CD80 and CD86, to support the function of T cells in immune killing [49, 50]. The aggregation of CD20+ B cells and CD8+ T cells plays a crucial role in the tumour immune response through costimulatory signalling, such as CD40/CD40L, which triggers the tumour-killing effect of T cells [51]. Different subsets of T cells are recruited into the TME to exert antitumour effects by the secretion of cytokines from B cells. CD20+ B cells recruit CD8+ T cells by releasing chemokines, and then B-cell populations attract T cells in inflammatory responses and immune cell interactions, including common chemokines such as CCL3, CCL4, CCL5, CXCL10, and CXCL13. In particular, CXCL13 is a core chemokine that recruits tumour-infiltrating B and T cells [52,53,54].
Correspondingly, helper T cells also prompt B cells to differentiate PCs and switch antibodies that exhibit antitumour responses [55]. Another recent research advance points to T follicular helper (Tfh) cells. Interactions between CD4+ T cells and B cells within tumours induce tumour-specific Tfh cell generation; afterwards, Tfh cells can enhance the antitumour effect of CD8+ T cells by secreting IL-21 [27] In addition, CD86+ B cells induce T-cell responses by localizing heavily in the TME through the presentation of tumour-associated antigens, particularly in TLSs of various cancer types, and B cells have also been found to promote the formation of TLSs by secreting CXCL13 and cytotoxic factors [28]. These results indicate that B cells in the TME achieve antitumour immunity by activating and inducing various T-cell subsets.
Crosstalk between T cells and B cells in the immune microenvironment is the backbone of tumour immunity, and other immune components also closely contact B cells. B cells are converted from naive B cells to memory B cells and PCs in TLSs of the TME [56]. Memory B cells have been detected in the peripheral blood of patients with various tumours, which may be related to the role of B cells in the microcirculation to help fight metastatic tumour cells [44, 57, 58]. Furthermore, PCs express IgA, IL-10, and PD-L1, resulting in immunosuppressive effects [59]. Recent studies have also shown the potential ability of B cells located in TLSs to respond to immunotherapy in multiple cancers [28, 60, 61]. With the help of Tfh cells, memory B cells and PCs are generated during the maturation of TLSs [62]. IgG-secreting PCs can also enhance the immune responses of Th1/Th17 cells [63]. A fraction of DCs expressing FcγR have affinity for PC-secreted IgG and enhance the immune response. Therefore, the utilization of the affinity of tumour-specific IgG antibodies to further improve the effect of antibody therapy for cancer is one of the current research directions in cancer immunotherapy [64, 65]. Effector B cells can affect the migration of DCs and produce antibodies to induce M1 macrophages to undergo ADCC or antibody-dependent cellular phagocytosis (ADCP) to kill tumour cells [66]. In addition, B cells crosstalk with other cells in the TME. Fibroblasts from tumours express higher levels of CXCL13, BAFF, and APRIL and are dependent on the CXCR5-CXCL13 axis to promote the accumulation of B cells in tumours and increase the proliferation of fibroblasts and TLS expansion in the TME [67]. These results suggest that B cells positively affect the TME and antitumour responses through the combined action of B cells and multiple immune cells (Fig. 1).
Crosstalk of B cells with other immune cells in the tumour microenvironment. Tumour-infiltrating B cells can activate CD4+ T cells, recruit CD8+ T cells and regulate the polarization of macrophages. In addition, B cells transform into plasma cells and effector B cells in the TME. Plasma cells can influence dendritic cells to present antigens to CD8+ T cells and produce antibodies to inhibit tumours. Plasma cells secrete antibodies to combine with the ligand of macrophages and transform macrophages into the M1 type to kill tumour cells. Effector B cells travel into the blood circulation to defend against potential tumour cells. However, Bregs can produce cytokines that are immunosuppressive and ultimately promote cancer development
Hidden protumor efforts
Overall, the antitumour effects of B cells are indisputable, but in fact, not all B cells have antitumour effects, and Bregs are the first to bear the brunt. Bregs negatively regulate the immune response by producing anti-inflammatory factors such as IL-10, IL-35 and TGF-β, which has been confirmed in several related tumour studies [32]. In the immunomodulation of pancreatic cancer, Bregs cause the depletion of CD8+ T cells in the TME through the IL-35- and IL-10-mediated STST2 pathway [68]. Bregs have been detected in the peripheral blood of gastric cancer patients and mediate tumour cell escape through IL-10 signalling [69]. In a clinical study of chronic myeloid leukaemia, tumour-produced TGF-β induced an immunosuppressive phenotype in Bregs, resulting in accelerated tumour progression [70]. These results are predictable considering the immunoregulatory function of Bregs, and reasonable elimination of the tumour-promoting effect of Bregs is the main point of current attention.
On the other hand, it is the tumour-promoting effect of antibodies produced by PCs, mainly including IgG variants and IgA. IgG4 subclass antibodies have been shown to be highly correlated with tumour malignancy and poor prognosis in oesophageal cancer patients, and the same results have been found in mouse models of breast cancer, colorectal cancer and carcinogen-induced skin papilloma [71]. In a colorectal cancer study, IgG4 induced the activation of M2 macrophages, impairing anticancer effects and promoting tumour development [72]. Regarding the tumour-promoting effect of IgA, it has been found that the concentration of IgA is positively correlated with a poor prognosis in both melanoma and HCC [73, 74]; it may regulate the immune function of T cells and cause a decrease in antitumour ability. These studies roughly suggest the opposite roles of antitumour immunity in human tumours and mouse tumours. In some animal experiments in mice, as ‘promoters’, B cells mostly promote tumour survival through specific cytokines. The conclusions of this part also require continuous attention and research.
B cells as biomarkers in cancer
Prognostic markers in cancer
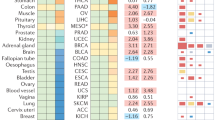
Multiple phenotypes of B cells have been shown to infiltrate various tumour tissues and are associated with a favourable prognosis (Table 1). These B cells perform complex functions in the TME. On the one hand, they can activate and connect with other immune cells to enhance the killing of tumour cells; on the other hand, different types of B cells produce various cytokines and antibodies and remodel the TME. The following characteristics of B cells as biomarkers can generally be found in patients with tumours: (i) The main types of infiltrating B cells are naive B cells, PCs and memory B cells, and the number of infiltrating B cells in tumours is positively correlated with the prognosis of patients. To a certain extent, the heterogeneity of populations and types of B cells in tumours determines the degree of antitumour effect. (ii) The spatiotemporal heterogeneity of B cells in tumours also affects the prognosis of cancer. Patients with advanced tumours have a low number of effector B cells and a high proportion of naive B cells. In tumour tissues, PCs and memory B cells are more relevant than naive B cells for the positive prognosis of tumours. In peripheral blood, there is also some degree of variation in the composition of B cells. (iii) TLSs are an important form of tumour-infiltrating B cells. The presence or absence of TLSs, the number of TLSs in the tumour and the degree of TLS maturation have been shown to be valuable prognostic markers. (iv) Antibodies produced by PCs can also be used as a prognostic indicator.
Some tumour-infiltrating B cells secrete antibodies against breast cancer antigens to promote humoral immunity. IgG and IgA are the primary antibodies, and they show different responses, with IgG usually representing a positive prognosis and IgA representing the opposite [72]. By initiating self-activation, B cells achieve class switching and affinity maturation in the immune aggregation zone and act as 'helpers' and 'defenders', thereby expanding the antibody library that matches adaptive immunity [16, 62]. In vitro studies have demonstrated that B cells from melanoma patients can produce IgG, which can eliminate cancer cells by triggering ADCC and ADCP. IgG can enhance antigen presentation and phagocytosis to promote antitumour effects [66]. Variants of IgG have also been detected in the peripheral blood of patients with non-small cell lung cancer (NSCLC) and breast cancer (BC), which is usually associated with a better clinical prognosis. In contrast, IgA has been detected in the TME and blood and has been associated with tumour-promoting mechanisms in some animal experiments [86, 87]. For example, TGF-β and some interleukins can induce IgA production, resulting in immunosuppression [59]. Consistently, tumour-specific antibodies have been detected in the serum of cancer patients in many studies [88]. Furthermore, the detection of serum levels of antibodies against tumour-associated antigens has been proposed for the early detection of cancer. In addition, the role of BCR in immunotherapy should not be overlooked. The killing effect of BCR and some costimulatory molecules, such as CD40 and CD86, on the surface of B cells in response to external antigen stimulation or enhancement of costimulatory signals of CD4+ T cells in tumours can also be used as markers for clinical prognostic monitoring [28, 89, 90].
Several recent heavyweight studies have shown that B-cell localization in the TME is a predictor of a favourable response in patients treated with ICIs in melanoma, sarcoma and clear cell renal cell carcinoma. Multicolour fluorescence immunohistochemical staining of some tumour tissues also revealed that there are many different lineages of B cells localized in TLSs, such as CD19, CD20, CD21, and CD138 [46, 58, 76]. Different B-cell lineages and tumour backgrounds have also shown different roles in various cancer types.
The role of B cells in immunotherapy and chemoradiotherapy
After changing the ecology of tumour immunity, B cells also respond positively to immunotherapy. This finding has been confirmed to varying degrees in different cancers. In addition to the involvement of B cells in tumour immune responses and influencing patient prognosis, B cells can also be used to predict the response to immunotherapy. From the classic classification, activated B cells, represented by PCs and memory B cells, enriched in tumour tissue usually predicts a favourable prognosis [91]. They adjust T-cell states to make them more sensitive to tumour cells in the TME. In melanoma patients receiving CTLA-4 inhibitor therapy, a lack of B cells is a predictor of a poor response to ICIs [92]. The signatures of B cells and PCs show a high immune enrichment status and a strong response to anti-PD-1 antibody therapy in soft tissue sarcoma [76]. In the immunotherapy of breast cancer, B-cell activation by T follicular helper cells and the secretion of antibodies is a key reflection of the response to immunotherapy. The response can also be checked by screening antibodies [93]. CD20+ B lymphocytes in colorectal cancer (CRC) are correlated with other immune cells and support a beneficial prognostic impact, even as prognostic biomarkers in metastatic CRC. Related B-cell subtypes are becoming hot targets for research [80, 94]. In addition, B cells can be used as biomarkers for immunotherapy, and B-cell-based immunotherapeutic strategies are discussed, including the stimulation of B-cell ligands to enhance B-cell immunity and activation of B cells in vitro and in vivo [95].
It is noteworthy that the characteristics of B cells in the TME change after ICI treatment, which has been demonstrated in different cancers (Table 2). After ICI therapy, responders were found to have the following characteristics: (1) B cells were significantly more abundant in the TME of responders than nonresponders, and the types were mainly memory B cells and plasma cells [46, 75, 85, 96,97,98]. (2) A variety of specific BCRs and antibodies closely related to B cells were also found to be abundant in the TME, with the type of antibodies being mainly immune-promoting IgG [46, 75, 93, 96]. (3) Increasing numbers of memory B cells, antibodies and cytokines were also detected in the peripheral blood of responders [98, 99]. Thus, these results confirmed not only the strong association between altered B-cell characteristics in the TME and the response to ICI treatment but also that B cells are likely to be necessary players in the role of ICIs in the TME.
For some patients receiving chemotherapy, there was an increase in the number of B cells, especially naive B cells and PCs, in patients who responded to treatment. These patients eventually had improved disease-free survival (DFS) and overall survival (OS). The number of B cells can be used as a prognostic indicator for cancer patients after radiotherapy or chemotherapy [101,102,103]. In other studies, dabrafenib plus trametinib in melanoma patients increased the density of tumour-infiltrating B cells in responders and may induce TLS formation [104]. The phenotype of tumour-infiltrating B cells changed to ICOSL+ B cells after chemotherapy in breast cancer patients and was associated with an improved prognosis. A positive correlation was also found between the response to chemotherapy in mice and the B cells infiltrating the tumour [105]. In ovarian cancer patients who responded to neoadjuvant chemotherapy, the density of CD20+ B cells was increased [106]. These results suggest that the density of B cells is closely related to the chemotherapy response. The number of B cells and TLSs in tumours can be increased with the addition of chemotherapy to enhance the immune response and improve tumour treatment by synergistic immunotherapy.
The future direction of B-cell clinical research
As the only immune cells that can produce antibodies, B cells can be expected to become a force in immunotherapy and targeted therapy. At present, the clinical application of cancer-targeting B cells is being attempted. We focus on these studies and summarize current advances (Fig. 2).
Predictive role
Prognostic prediction and treatment evaluation based on the surface markers of B cells have made distinct progress in B-cell clinical research at present. CD19, CD20, CD38, CD86 and CD138 detected in tumour tissues were used as markers for positive prognosis [28, 58, 84, 85]. These markers mainly correspond to naive B cells, switch B cells, PCs and memory B cells. In addition, the presence of B cells in tumours, especially fully mature TLSs, also plays a crucial role in cancer prediction. B cells can better exert antitumour effects by producing antitumour antibodies and cooperating with other immune cells in mature TLSs [61, 107]. The changes in IgG, IgM, and IgA produced by B cells in tumour tissues or peripheral blood can also reflect the prognosis of cancer. Moreover, the detection of Bregs is important for predicting cancer. The corresponding markers were mainly IL-10, IL-35 and PD-L1. In addition, some B-cell markers sometimes correspond to a poorer prognosis, such as CD19 (which was found to be associated with a poor prognosis in studies of breast and gastric cancers) and CD79a expression on immature myeloid cells, contributing to their tumour-promoting effects [39, 108, 109]. This suggests that the link between these B-cell biomarkers and prognosis remains a focus of research. B cells are also good predictors of the response to immunotherapy and chemoradiotherapy. In addition to the above biomarkers, targeting the B-cell transcriptome can be used to construct effective prognostic models for cancer patients.
Targeted therapy
It is valuable to look for antitumour or tumour-promoting signals of cytokines and antibodies associated with B cells to find some targets for targeted therapy. Cytokine-based signalling pathways, such as the CXCL13/CXCR5 axis and the CCL19,21/CCR7 axis, mediate the recruitment of B cells and TLSs in tumours [62]. CXCR5 is the target molecule of CXCL13, which induces the aggregation of CXCR5-expressing B cells and other immune cells in the TME, and it is also highly correlated with the expression and formation of TLSs. CCL19,21/CCR7 can mediate the homing of immune cells to lymphoid tissues, leading to enhanced immune infiltration in the TME and ultimately to a positive survival outcome. In addition, cytokines such as IL-17 and CXCL12 can contribute to the maturation of B cells [110]. These results suggest that B-cell-related cytokines and pathways are available as targets for tumour-targeted therapy to inhibit tumour growth. The main goal is to enhance the infiltration of B cells or TLSs in the TME and obtain a better immune benefit. However, the above cytokines also showed opposite results in some studies. For instance, CXCL13 elevation was related to a poor prognosis in breast cancer, and CCR7 upregulation in some cancer cells enhanced lymph node metastasis [111,112,113]. This may be closely related to the heterogeneity of different tumour types. It is important to note that when enhancing B-cell-based immunity, attention needs to be paid to its hidden protumor effects as well as the massive production of antibodies and cytokines causing immune storms and autoimmune diseases. In contrast to the antitumour effects of B cells, Bregs are also a potential target, and Breg-produced IL-10 and IL-35 can have inhibitory effects on a variety of immune cells promoting tumour development. This demonstrates that tumour development can be inhibited in tumours by suppressing Breg-secreted cytokines.
Immunotherapy
B cells in the TME of patients who have responded to ICI treatment tend to be more active. This state is mainly characterized by differentiation towards specific functional subpopulations and possibly increased expression of immune checkpoints [114, 115]. Therefore, the identification of developmental trajectories and specific subpopulations of tumour-infiltrating B cells using single-cell technology is an important future direction [116, 117]. On the one hand, a better prognosis could be achieved by promoting the differentiation of B cells into specific subpopulations. On the other hand, novel immunotherapeutic drugs could be designed based on new surface markers and potential immune checkpoints of B cells.
Recently, CD40/CD40L was identified as a potential immune checkpoint for B cells and may play a role in immunotherapy [118]. CD40 agonist antibodies have been shown to make a difference in the clinical treatment of different cancers and are closely related to B cells [119]. CD40 expressed by B cells generates signalling to stimulate the formation of immune tissue generative centres, promotes antibody isotype switching and enhances antigen affinity, and then creates long-lasting PCs and memory B cells [120]. Targeting CD40/CD40L is still in clinical trials in some solid tumours, but it gives us the idea to further search for B-cell immune checkpoints for immunotherapy, which is an important research direction for B-cell immunotherapy.
B-cell engineering and vaccines
A number of studies are underway using CAR-T and cancer vaccines as important tools for cell engineering to treat cancer [121, 122]. However, B cells and their interactions with T cells have been much less studied in cancer cell engineering and vaccines than T cells. Although B cells are highly sensitive to tumour cell-specific antigens, these antigens require antigen-antibody interactions mediated by CD4+ T cells with the help of MHC-II molecules. Subsequently, B cells are triggered to produce antibodies upon contact with tumour cell-specific antigens and completely destroy the target antigen. This requires determining the structure and form of the processed antigen of the B-cell-recognized MHC molecule as the basis for in vitro processing and loading and applying it in the form of a vaccine to cancer patients to induce adaptive immunity in B cells [123]. Current single-cell omics technology is a reliable means of classifying subpopulations of tumour-infiltrating B cells and identifying B cells with better antitumour effects.
Discussion
Studies on immune cells in tumorigenesis and development raise concern and indicate the need for more effective immune treatments. B cells are gaining attention as an emerging prognostic factor and immunotherapy direction. We discuss that different subsets of B cells exhibit different immune functions against cancer. In the TME, B cells interact with other immune cells in a variety of ways in different states, mainly by inhibiting the occurrence and development of tumours and killing tumour cells to a certain extent. Overall, the favourable prognosis of tumour patients is closely related to the infiltration of B cells. We have listed various cancer types to prove this hypothesis. Moreover, B-cell density and B-cell activity were significantly increased in tumour patients who responded well to immunotherapy. These results imply that B cells are the key immune cells associated with a favourable tumour prognosis. However, in the practice of translating the immune ability of B cells to tumour immunotherapy, a large number of issues still need to be addressed. First, B cells recognize tumour cell antigens and then act as APCs, which is particularly vital for whether the recognized ones are endogenous or exogenous, which can explore what pathways B cells utilize to enhance the inhibitory effect of immune components on tumours, including endogenous or exogenous antigenic stimuli and related immune signals for induced responses. The relationship between the production of antibodies by PCs and tumours is another hot topic. In addition to enhancing antigen presentation and promoting the killing of other immune cells, the role of different antibody types and their subtypes in different tumours is also worth discussing. It is a potential research direction to explain how B cells respond to tumour cell heterogeneity to achieve the corresponding immune response.
In addition, the relationship between B cells and other immune cells or lymphoid structures is particularly important in different cancer models. In the TME, B cells interact with a variety of immune cells and play a role in tumorigenesis through synergy or antagonism. Among them, B-cell-related cytokines are particularly significant. Core cytokines such as CXCL13, CXCL10 and IL-10 are involved in the recruitment, activation or inhibition of various immune cells. B cells can also reshape the immune microenvironment to provide beds more suitable for T cells to exert their effects and control tumour growth. Of course, these linkages are particularly pronounced in TLSs, where both the degree of B-cell activation and TLS maturation are good indicators of response to ICI therapy. Moreover, some immune complexes have also been found to be associated with inflammatory responses and activation of immune components. In that way, does immune-active individuals or the immune storm after infectious immunization have a positive effect on tumour immunity and its treatment?
Finally, the role of different subsets of B cells in tumours is different in multiple studies. PCs and Bregs are the focus of attention. The functions and phenotypes of various B-cell subsets are complex, and it is necessary to carry out comprehensive marker determination and prognostic analysis of the TME and circulating B cells in various cancers currently relying on single-cell technology. Therefore, in studies of B-cell tumour immunotherapy, it is still necessary to further explore the relationship between its immune mechanisms, changes in the TME with ICI therapy, and the clinical prognosis of various subpopulations. Cancer immunotherapy relying on B cells will undergo a great shift in the near future.
Availability of data and materials
Not applicable.
Abbreviations
- ICI:
-
Immune checkpoint inhibitor
- PD-1:
-
Programmed cell death protein 1
- PD-L1:
-
Programmed cell death ligand 1
- Bregs:
-
Regulatory B cells
- PCs:
-
Plasma cells
- CTLA-4:
-
Cytotoxic T lymphocyte–associated protein 4
- TME:
-
Tumour microenvironment
- TLS:
-
Tertiary lymphoid structure
- IL:
-
Interleukin
- CD:
-
Cluster of differentiation
- scRNA-seq:
-
Single-cell RNA sequencing
- CXCL:
-
Chemokine interferon-inducible protein
- CCL:
-
Chemokine (C-C motif) ligand
- APC:
-
Antigen-presenting cell
- MHC:
-
Major histocompatibility complex
- DC:
-
Dendric cell
- CTL:
-
Cytotoxic T cell
- Th:
-
Helper T cell
- ADCC:
-
Antibody-dependent cell cytotoxicity
- ADCP:
-
Antibody-dependent cellular phagocytosis
- ICOS:
-
Inducible costimulatory
- Tregs:
-
Regulatory T cells
- HCC:
-
Hepatocellular carcinoma
- CAR:
-
Chimeric antigen receptor
- NSCLC:
-
Non-small cell lung cancer
- BC:
-
Breast cancer
- CRC:
-
Colorectal cancer
- RCC:
-
Renal cell cancer
- SCC:
-
Squamous cell carcinoma
- GC:
-
Germinal centre
- OS:
-
Overall survival
- DFS:
-
Disease-free survival
- DSS:
-
Disease specific survival
- PFS:
-
Progression-free survival
- RFS:
-
Recurrence free survival
References
Nishino M, et al. Monitoring immune-checkpoint blockade: response evaluation and biomarker development. Nat Rev Clin Oncol. 2017;14(11):655–68.
Sharma P, Allison JP. The future of immune checkpoint therapy. Science. 2015;348(6230):56–61.
Morad G, et al. Hallmarks of response, resistance, and toxicity to immune checkpoint blockade. Cell. 2021;184(21):5309–37.
Quail DF, Joyce JA. Microenvironmental regulation of tumor progression and metastasis. Nat Med. 2013;19(11):1423–37.
Hinshaw DC, Shevde LA. The Tumor Microenvironment Innately Modulates Cancer Progression. Cancer Res. 2019;79(18):4557–66.
Farhood B, Najafi M, Mortezaee K. CD8(+) cytotoxic T lymphocytes in cancer immunotherapy: A review. J Cell Physiol. 2019;234(6):8509–21.
Liao W, et al. KRAS-IRF2 Axis Drives Immune Suppression and Immune Therapy Resistance in Colorectal Cancer. Cancer Cell. 2019;35(4):559-572 e7.
Papalexi E, Satija R. Single-cell RNA sequencing to explore immune cell heterogeneity. Nat Rev Immunol. 2018;18(1):35–45.
Veldman-Jones MH, et al. Evaluating Robustness and Sensitivity of the NanoString Technologies nCounter Platform to Enable Multiplexed Gene Expression Analysis of Clinical Samples. Cancer Res. 2015;75(13):2587–93.
Sautes-Fridman C, et al. Tertiary lymphoid structures in the era of cancer immunotherapy. Nat Rev Cancer. 2019;19(6):307–25.
Fillatreau S. Cytokine-producing B cells as regulators of pathogenic and protective immune responses. Ann Rheum Dis. 2013;72 Suppl 2:ii80-4.
Bao Y, et al. Identification of IFN-gamma-producing innate B cells. Cell Res. 2014;24(2):161–76.
Sarvaria A, Madrigal JA, Saudemont A. B cell regulation in cancer and anti-tumor immunity. Cell Mol Immunol. 2017;14(8):662–74.
Zhang B, et al. B cell-derived GABA elicits IL-10(+) macrophages to limit anti-tumour immunity. Nature. 2021;599(7885):471–6.
Shahaf G, et al. B Cell Development in the Bone Marrow Is Regulated by Homeostatic Feedback Exerted by Mature B Cells. Front Immunol. 2016;7:77.
LeBien TW, Tedder TF. B lymphocytes: how they develop and function. Blood. 2008;112(5):1570–80.
Hegde PS, Chen DS. Top 10 Challenges in Cancer Immunotherapy. Immunity. 2020;52(1):17–35.
Zehentmeier S, Pereira JP. Cell circuits and niches controlling B cell development. Immunol Rev. 2019;289(1):142–57.
Giordani L, et al. IFN-alpha amplifies human naive B cell TLR-9-mediated activation and Ig production. J Leukoc Biol. 2009;86(2):261–71.
Barnas JL, et al. B Cell Activation and Plasma Cell Differentiation Are Promoted by IFN-lambda in Systemic Lupus Erythematosus. J Immunol. 2021;207(11):2660–72.
Shang L, et al. Toll-like receptor signaling in small intestinal epithelium promotes B-cell recruitment and IgA production in lamina propria. Gastroenterology. 2008;135(2):529–38.
Possamai D, et al. CD40L-Stimulated B Lymphocytes Are Polarized toward APC Functions after Exposure to IL-4 and IL-21. J Immunol. 2021;207(1):77–89.
Franke F, et al. IL-21 in Conjunction with Anti-CD40 and IL-4 Constitutes a Potent Polyclonal B Cell Stimulator for Monitoring Antigen-Specific Memory B Cells. Cells. 2020;9(2):433.
Gao SH, et al. CXCL13 in Cancer and Other Diseases: Biological Functions, Clinical Significance, and Therapeutic Opportunities. Life (Basel). 2021;11(12):1282.
Bolger-Munro M, et al. Arp2/3 complex-driven spatial patterning of the BCR enhances immune synapse formation, BCR signaling and B cell activation. Elife. 2019;8:e44574.
Bruno TC, et al. Antigen-Presenting Intratumoral B Cells Affect CD4(+) TIL Phenotypes in Non-Small Cell Lung Cancer Patients. Cancer Immunol Res. 2017;5(10):898–907.
Cui C, et al. Neoantigen-driven B cell and CD4 T follicular helper cell collaboration promotes anti-tumor CD8 T cell responses. Cell. 2021;184(25):6101-6118 e13.
Wennhold K, et al. CD86(+) Antigen-Presenting B Cells Are Increased in Cancer, Localize in Tertiary Lymphoid Structures, and Induce Specific T-cell Responses. Cancer Immunol Res. 2021;9(9):1098–108.
Yuseff MI, et al. How B cells capture, process and present antigens: a crucial role for cell polarity. Nat Rev Immunol. 2013;13(7):475–86.
Chen Z, et al. Landscape and dynamics of single tumor and immune cells in early and advanced-stage lung adenocarcinoma. Clin Transl Med. 2021;11(3):e350.
Deola S, et al. Helper B cells promote cytotoxic T cell survival and proliferation independently of antigen presentation through CD27/CD70 interactions. J Immunol. 2008;180(3):1362–72.
Rosser EC, Mauri C. Regulatory B cells: origin, phenotype, and function. Immunity. 2015;42(4):607–12.
Wojciechowski W, et al. Cytokine-producing effector B cells regulate type 2 immunity to H. polygyrus. Immunity. 2009;30(3):421–33.
Linton PJ, et al. Costimulation via OX40L expressed by B cells is sufficient to determine the extent of primary CD4 cell expansion and Th2 cytokine secretion in vivo. J Exp Med. 2003;197(7):875–83.
Barr TA, et al. TLR and B cell receptor signals to B cells differentially program primary and memory Th1 responses to Salmonella enterica. J Immunol. 2010;185(5):2783–9.
Pang Y, et al. Interferon-gamma gene expression in human B-cell lines: induction by interleukin-2, protein kinase C activators, and possible effect of hypomethylation on gene regulation. Blood. 1992;80(3):724–32.
Jansen K, et al. Regulatory B cells. A to Z Allergy. 2021;76(9):2699–715.
Shao Y, et al. Regulatory B cells accelerate hepatocellular carcinoma progression via CD40/CD154 signaling pathway. Cancer Lett. 2014;355(2):264–72.
Murakami Y, et al. Increased regulatory B cells are involved in immune evasion in patients with gastric cancer. Sci Rep. 2019;9(1):13083.
Roya N, et al. Frequency of IL-10+CD19+ B cells in patients with prostate cancer compared to patients with benign prostatic hyperplasia. Afr Health Sci. 2020;20(3):1264–72.
Olkhanud PB, et al. Tumor-evoked regulatory B cells promote breast cancer metastasis by converting resting CD4(+) T cells to T-regulatory cells. Cancer Res. 2011;71(10):3505–15.
Mantovani A, et al. Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol. 2002;23(11):549–55.
Fridman WH, et al. B cells and tertiary lymphoid structures as determinants of tumour immune contexture and clinical outcome. Nat Rev Clin Oncol. 2022;19(7):441–57.
Germain C, et al. Presence of B cells in tertiary lymphoid structures is associated with a protective immunity in patients with lung cancer. Am J Respir Crit Care Med. 2014;189(7):832–44.
Montfort A, et al. A Strong B-cell Response Is Part of the Immune Landscape in Human High-Grade Serous Ovarian Metastases. Clin Cancer Res. 2017;23(1):250–62.
Meylan M, et al. Tertiary lymphoid structures generate and propagate anti-tumor antibody-producing plasma cells in renal cell cancer. Immunity. 2022;55(3):527-541 e5.
Roumenina LT, et al. Context-dependent roles of complement in cancer. Nat Rev Cancer. 2019;19(12):698–715.
Chung W, et al. Single-cell RNA-seq enables comprehensive tumour and immune cell profiling in primary breast cancer. Nat Commun. 2017;8:15081.
Lane P. Regulation of T and B cell responses by modulating interactions between CD28/CTLA4 and their ligands, CD80 and CD86. Ann N Y Acad Sci. 1997;815:392–400.
Greenwald RJ, Freeman GJ, Sharpe AH. The B7 family revisited. Annu Rev Immunol. 2005;23:515–48.
Hladikova K, et al. Tumor-infiltrating B cells affect the progression of oropharyngeal squamous cell carcinoma via cell-to-cell interactions with CD8(+) T cells. J Immunother Cancer. 2019;7(1):261.
Griss J, et al. B cells sustain inflammation and predict response to immune checkpoint blockade in human melanoma. Nat Commun. 2019;10(1):4186.
Workel HH, et al. A Transcriptionally Distinct CXCL13(+)CD103(+)CD8(+) T-cell Population Is Associated with B-cell Recruitment and Neoantigen Load in Human Cancer. Cancer Immunol Res. 2019;7(5):784–96.
Zhang QF, et al. CDK4/6 inhibition promotes immune infiltration in ovarian cancer and synergizes with PD-1 blockade in a B cell-dependent manner. Theranostics. 2020;10(23):10619–33.
Pillozzi S, et al. Soft Tissue Sarcoma: An Insight on Biomarkers at Molecular, Metabolic and Cellular Level. Cancers (Basel). 2021;13(12):3044.
Gundeson AJ, et al. Germinal center reactions in tertiary lymphoid structures associate with neoantigen burden, humoral immunity and long-term survivorship in pancreatic cancer. Oncoimmunology. 2021;10(1):1900635.
Kohli K, Pillarisetty VG. Dendritic Cells in the Tumor Microenvironment. Adv Exp Med Biol. 2020;1273:29–38.
Cabrita R, et al. Tertiary lymphoid structures improve immunotherapy and survival in melanoma. Nature. 2020;577(7791):561–5.
Shalapour S, et al. Immunosuppressive plasma cells impede T-cell-dependent immunogenic chemotherapy. Nature. 2015;521(7550):94–8.
Kroeger DR, Milne K, Nelson BH. Tumor-Infiltrating Plasma Cells Are Associated with Tertiary Lymphoid Structures, Cytolytic T-Cell Responses, and Superior Prognosis in Ovarian Cancer. Clin Cancer Res. 2016;22(12):3005–15.
Ruffin AT, et al. B cell signatures and tertiary lymphoid structures contribute to outcome in head and neck squamous cell carcinoma. Nat Commun. 2021;12(1):3349.
Tokunaga R, et al. B cell and B cell-related pathways for novel cancer treatments. Cancer Treat Rev. 2019;73:10–9.
Liu RX, et al. Chemokine (C-X-C motif) receptor 3-positive B cells link interleukin-17 inflammation to protumorigenic macrophage polarization in human hepatocellular carcinoma. Hepatology. 2015;62(6):1779–90.
Guilliams M, et al. The function of Fcgamma receptors in dendritic cells and macrophages. Nat Rev Immunol. 2014;14(2):94–108.
Nimmerjahn F, Ravetch JV. Translating basic mechanisms of IgG effector activity into next generation cancer therapies. Cancer Immun. 2012;12:13.
Gul N, van Egmond M. Antibody-Dependent Phagocytosis of Tumor Cells by Macrophages: A Potent Effector Mechanism of Monoclonal Antibody Therapy of Cancer. Cancer Res. 2015;75(23):5008–13.
Rodriguez AB, et al. Immune mechanisms orchestrate tertiary lymphoid structures in tumors via cancer-associated fibroblasts. Cell Rep. 2021;36(3):109422.
Mirlekar B, et al. B cell-Derived IL35 Drives STAT3-Dependent CD8(+) T-cell Exclusion in Pancreatic Cancer. Cancer Immunol Res. 2020;8(3):292–308.
Wei X, et al. Regulatory B cells contribute to the impaired antitumor immunity in ovarian cancer patients. Tumour Biol. 2016;37(5):6581–8.
Bodogai M, et al. Anti-CD20 antibody promotes cancer escape via enrichment of tumor-evoked regulatory B cells expressing low levels of CD20 and CD137L. Cancer Res. 2013;73(7):2127–38.
Wang H, et al. An immune evasion mechanism with IgG4 playing an essential role in cancer and implication for immunotherapy. J Immunother Cancer. 2020;8(2):e000661.
Jordakieva G, et al. IgG4 induces tolerogenic M2-like macrophages and correlates with disease progression in colon cancer. Oncoimmunology. 2021;10(1):1880687.
Bosisio FM, et al. Plasma cells in primary melanoma. Prognostic significance and possible role of IgA. Mod Pathol. 2016;29(4):347–58.
Shalapour S, et al. Inflammation-induced IgA+ cells dismantle anti-liver cancer immunity. Nature. 2017;551(7680):340–5.
Helmink BA, et al. B cells and tertiary lymphoid structures promote immunotherapy response. Nature. 2020;577(7791):549–55.
Petitprez F, et al. B cells are associated with survival and immunotherapy response in sarcoma. Nature. 2020;577(7791):556–60.
Mahmoud SM, et al. The prognostic significance of B lymphocytes in invasive carcinoma of the breast. Breast Cancer Res Treat. 2012;132(2):545–53.
Garaud S, et al. Tumor infiltrating B-cells signal functional humoral immune responses in breast cancer. JCI Insight. 2019;5:e129641.
Kuroda H, et al. Prognostic value of tumor-infiltrating B lymphocytes and plasma cells in triple-negative breast cancer. Breast Cancer. 2021;28(4):904–14.
Edin S, et al. The Prognostic Importance of CD20(+) B lymphocytes in Colorectal Cancer and the Relation to Other Immune Cell subsets. Sci Rep. 2019;9(1):19997.
Berntsson J, et al. Expression of programmed cell death protein 1 (PD-1) and its ligand PD-L1 in colorectal cancer: Relationship with sidedness and prognosis. Oncoimmunology. 2018;7(8):e1465165.
Yamakoshi Y, et al. Immunological potential of tertiary lymphoid structures surrounding the primary tumor in gastric cancer. Int J Oncol. 2020;57(1):171–82.
Shi JY, et al. Margin-infiltrating CD20(+) B cells display an atypical memory phenotype and correlate with favorable prognosis in hepatocellular carcinoma. Clin Cancer Res. 2013;19(21):5994–6005.
Garnelo M, et al. Interaction between tumour-infiltrating B cells and T cells controls the progression of hepatocellular carcinoma. Gut. 2017;66(2):342–51.
Patil NS, et al. Intratumoral plasma cells predict outcomes to PD-L1 blockade in non-small cell lung cancer. Cancer Cell. 2022;40(3):289-300 e4.
Tan Q, et al. Anti-PD1/PDL1 IgG subclass distribution in ten cancer types and anti-PD1 IgG4 as biomarker for the long time survival in NSCLC with anti-PD1 therapy. Cancer Immunol Immunother. 2022;71(7):1681–91.
Garaud S, et al. Antigen Specificity and Clinical Significance of IgG and IgA Autoantibodies Produced in situ by Tumor-Infiltrating B Cells in Breast Cancer. Front Immunol. 2018;9:2660.
Chen W, Yuan Y, Jiang X. Antibody and antibody fragments for cancer immunotherapy. J Control Release. 2020;328:395–406.
Constant SL. B lymphocytes as antigen-presenting cells for CD4+ T cell priming in vivo. J Immunol. 1999;162(10):5695–703.
Huffman AP, et al. CCL5 mediates CD40-driven CD4+ T cell tumor infiltration and immunity. JCI Insight. 2020;5(10):e137263.
Wouters MCA, Nelson BH. Prognostic Significance of Tumor-Infiltrating B Cells and Plasma Cells in Human Cancer. Clin Cancer Res. 2018;24(24):6125–35.
Selitsky SR, et al. Prognostic value of B cells in cutaneous melanoma. Genome Med. 2019;11(1):36.
Hollern DP, et al. B Cells and T Follicular Helper Cells Mediate Response to Checkpoint Inhibitors in High Mutation Burden Mouse Models of Breast Cancer. Cell. 2019;179(5):1191-1206 e21.
Hof J, et al. B Cells as Prognostic Biomarker After Surgery for Colorectal Liver Metastases. Front Oncol. 2020;10:249.
Wang SS, et al. Tumor-infiltrating B cells: their role and application in anti-tumor immunity in lung cancer. Cell Mol Immunol. 2019;16(1):6–18.
Anagnostou V, et al. Integrative Tumor and Immune Cell Multi-omic Analyses Predict Response to Immune Checkpoint Blockade in Melanoma. Cell Rep Med. 2020;1(8):100139.
Chen R, et al. Effect of immunotherapy on the immune microenvironment in advanced recurrent cervical cancer. Int Immunopharmacol. 2022;106:108630.
Ho WJ, et al. Neoadjuvant Cabozantinib and Nivolumab Converts Locally Advanced HCC into Resectable Disease with Enhanced Antitumor Immunity. Nat Cancer. 2021;2(9):891–903.
Xia L, et al. Predictable Roles of Peripheral IgM Memory B Cells for the Responses to Anti-PD-1 Monotherapy Against Advanced Non-Small Cell Lung Cancer. Front Immunol. 2021;12:759217.
Wu Z, et al. CD20(+)CD22(+)ADAM28(+) B Cells in Tertiary Lymphoid Structures Promote Immunotherapy Response. Front Immunol. 2022;13:865596.
Kim SS, et al. B Cells Improve Overall Survival in HPV-Associated Squamous Cell Carcinomas and Are Activated by Radiation and PD-1 Blockade. Clin Cancer Res. 2020;26(13):3345–59.
Han L, et al. Gene signature based on B cell predicts clinical outcome of radiotherapy and immunotherapy for patients with lung adenocarcinoma. Cancer Med. 2020;9(24):9581–94.
Singh S, et al. Chemotherapy Coupled to Macrophage Inhibition Induces T-cell and B-cell Infiltration and Durable Regression in Triple-Negative Breast Cancer. Cancer Res. 2022;82(12):2281–97.
Brase JC, et al. Role of Tumor-Infiltrating B Cells in Clinical Outcome of Patients with Melanoma Treated With Dabrafenib Plus Trametinib. Clin Cancer Res. 2021;27(16):4500–10.
Lu Y, et al. Complement Signals Determine Opposite Effects of B Cells in Chemotherapy-Induced Immunity. Cell. 2020;180(6):1081-1097 e24.
Lo CS, et al. Neoadjuvant Chemotherapy of Ovarian Cancer Results in Three Patterns of Tumor-Infiltrating Lymphocyte Response with Distinct Implications for Immunotherapy. Clin Cancer Res. 2017;23(4):925–34.
Xia J, et al. Single-cell landscape and clinical outcomes of infiltrating B cells in colorectal cancer. Immunol. 2023;168(1):135-51.
Luger D, et al. Expression of the B-cell receptor component CD79a on immature myeloid cells contributes to their tumor promoting effects. PLoS One. 2013;8(10):e76115.
Guan H, et al. PD-L1 mediated the differentiation of tumor-infiltrating CD19(+) B lymphocytes and T cells in Invasive breast cancer. Oncoimmunology. 2016;5(2):e1075112.
Ferretti E, et al. IL-17 superfamily cytokines modulate normal germinal center B cell migration. J Leukoc Biol. 2016;100(5):913–8.
Mehner C, et al. Tumor cell-produced matrix metalloproteinase 9 (MMP-9) drives malignant progression and metastasis of basal-like triple negative breast cancer. Oncotarget. 2014;5(9):2736–49.
Xia X, et al. Correlation between CCR7 expression and lymph node metastatic potential of human tongue carcinoma. Oral Dis. 2015;21(1):123–31.
Muller A, et al. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001;410(6824):50–6.
Kim SS, et al. Role of B Cells in Responses to Checkpoint Blockade Immunotherapy and Overall Survival of Cancer Patients. Clin Cancer Res. 2021;27(22):6075–82.
Willsmore ZN, et al. B Cells in Patients With Melanoma: Implications for Treatment With Checkpoint Inhibitor Antibodies. Front Immunol. 2020;11:622442.
Morgan D, Tergaonkar V. Unraveling B cell trajectories at single cell resolution. Trends Immunol. 2022;43(3):210–29.
Gu S, et al. Significance of intratumoral infiltration of B cells in cancer immunotherapy: From a single cell perspective. Biochim Biophys Acta Rev Cancer. 2021;1876(2):188632.
Enell Smith K, et al. Rationale and clinical development of CD40 agonistic antibodies for cancer immunotherapy. Expert Opin Biol Ther. 2021;21(12):1635–46.
Vonderheide RH. CD40 Agonist Antibodies in Cancer Immunotherapy. Annu Rev Med. 2020;71:47–58.
Elgueta R, et al. Molecular mechanism and function of CD40/CD40L engagement in the immune system. Immunol Rev. 2009;229(1):152–72.
Brudno JN, Kochenderfer JN. Recent advances in CAR T-cell toxicity: Mechanisms, manifestations and management. Blood Rev. 2019;34:45–55.
Sellars MC, Wu CJ, Fritsch EF. Cancer vaccines: Building a bridge over troubled waters. Cell. 2022;185(15):2770–88.
Beg S, et al. Nanomedicinal strategies as efficient therapeutic interventions for delivery of cancer vaccines. Semin Cancer Biol. 2021;69:43–51.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81802933 to Xiao Yang, No. 82072614 to Minhua Zheng, and No. 81871984 to Jing Sun), Shanghai Municipal Key Clinical Specialty (shslczdzk00102 to Minhua Zheng), Science and Technology Commission of Shanghai Municipality (under Grant 22ZR1439700), and Guangci Distinguished Young Scholars Training Program (under Grant GCQN-2019-A07).
Author information
Authors and Affiliations
Contributions
X.Y, MH.Z and J.S designed this study. EK.Z, CS.D and SC.L drafted the manuscript. XL.Z, B.A, XD.F revised manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, E., Ding, C., Li, S. et al. Roles and mechanisms of tumour-infiltrating B cells in human cancer: a new force in immunotherapy. Biomark Res 11, 28 (2023). https://doi.org/10.1186/s40364-023-00460-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40364-023-00460-1