Abstract
Background
Air pollution increases the morbidity and mortality of cardiovascular disease (CVD). Atherosclerosis (AS) is the pathological basis of most CVD, and the progression of atherosclerosis and the increase of fragile plaque rupture are the mechanism basis of the relationship between atmospheric particulate pollution and CVD. The aim of the present study was to investigate the effects of coal-fired fine particulate matter (PM2.5) on the expression levels of atherosclerosis-related proteins (von Willebrand factor (vWF), Endothelin-1 (ET-1), intercellular adhesion molecule-1 (ICAM-1), and E-selectin, and to explore the role and mechanism of the progression of atherosclerosis induced by coal-fired PM2.5 via the mitogen-activated protein kinase (MAPK) signaling pathways.
Methods
Different concentrations of PM2.5 were given to apolipoprotein-E knockout (ApoE−/−) mice via intratracheal instillation for 8 weeks. Enzyme-linked immunosorbent assay (ELISA) was used to detect the levels of vWF, ET-1 in serum of mice. Immunohistochemistry was used to observe the expression and distribution of ICAM-1 and E-selectin in the aorta of mice. Western blot was used to investigate the phosphoylation of proteins relevant to MAPK signaling pathways.
Results
Coal-fired PM2.5 exacerbated atherosclerosis induced by a high-fat diet. Fibrous cap formation, foam cells accumulation, and atherosclerotic lesions were observed in the aortas of PM2.5-treated mice. Coal-fired PM2.5 increased the protein levels of ET-1, ICAM-1, and E-selectin, but there was no significant difference in the vWF levels between the PM2.5-treatment mice and the HFD control mice. Coal-fired PM2.5 promoted the phosphorylation of p38, c-Jun N-terminal kinase (JNK), extracellular signal-regulated kinase (ERK) in aortic tissues of mice.
Conclusion
Coal-derived PM2.5 exacerbated the formation of atherosclerosis in mice, increased the expression levels of atherosclerosis-related proteins in mice serum, and promoted the phosphorylation of proteins relevant to MAPK signaling pathway. Thus, MAPK signaling pathway may play a role in the atherosclerosis pathogenesis induced by Coal-derived PM2.5.
Similar content being viewed by others
Background
Air pollution caused 4.1 million deaths globally in 2016 alone and is the sixth highest-ranking risk factor for global mortality [1]. Air pollution increases the morbidity and mortality of cardiovascular disease (CVD) [2,3,4,5]. According to a report of the World Health Organization (WHO), around 17.3 million people die of CVD each year, which accounts for 30% of all deaths [6]. Fine particulate matter (PM2.5) is the main toxic component of atmospheric particulate matter and primarily derives from coal-fired emission and automobile exhaust [7]. Moreover, an estimated 2.9 million deaths was attributed to PM2.5 in 2013 alone, which is considered as a leading risk factor for global disease [8]. PM2.5 is one of the primary causes of death in China and accounted for 11.1% of all deaths in China in 2016 [1]. Since the PM2.5 pollution is mainly caused by coal-burning emission in China [9, 10], it is important for future research to further elucidate the effects and mechanisms of coal-fired PM2.5 on cardiovascular diseases.
Atherosclerosis (AS) is a type of CVD [11] and is one of the leading causes of death around the world [12,13,14]. AS is also the pathological basis of most CVD, and the progression of atherosclerosis and the increase of fragile plaque rupture are the mechanism basis of the relationship between atmospheric particulate pollution and CVD [15,16,17]. PM2.5 increased mortality in individuals with CVD [18] via its contribution to the development of atherosclerosis [19]. Additionally, exposure to PM2.5 is a fundamental cause of cardiovascular diseases [20].
PM2.5 has short-term and long-term effect on cardiovascular system [14, 21]. Animal studies have suggested that PM2.5 exposure increases both the area of atherosclerotic plaques and plaque vulnerability in apolipoprotein-E knockout (ApoE−/−) mice and rats [19, 22, 23]. Similar results have been found from epidemiological studies, which have revealed that exposure to PM2.5 increases the development of atherosclerosis in humans [24,25,26]. PM2.5 presumably exerts atherogenic effects by inducing endothelial damage, mitochondrial injury, inflammatory responses, and oxidative stress [23, 27, 28]. However, the underlying molecular processes and potential mechanisms remain to be fully elucidated due to the etiological complexity of the atherogenesis [29, 30].
Mitogen-activated protein kinase (MAPK) signaling pathways are a series of parallel cascades of serine/threonine kinase, including extracellular signal-regulated kinase (ERK), c-Jun N-terminal kinase (JNK), and p38 MAPK [31]. MAPK signaling pathways play a key role in the atherosclerosis development [32], and it deserves further investigation in PM2.5-induced atherosclerosis. Thus, the present study aimed at exploring the mechanisms of atherosclerosis induced by coal-fired PM2.5 and the role of MAPK signaling pathways in this disease progression.
Methods
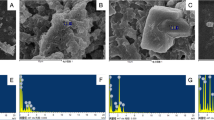
Coal-fired PM2.5 collection and extraction
Raw coal from a typical coal field (Yinchuan) in China was purchased from state-owned coal mines. The coal samples were broken into pieces and ignited in the stove. PM2.5 emitted from coal combustion was sampled by the dilution tunnel system, and dilution and sampling continued until the combustion finished [33].
The PM2.5 filters were extracted with ultra-pure water in an ultrasonic bath. After ultrasonic elution and freeze-drying, coal-fired PM2.5 suspensions were prepared and stored at − 20 °C until they were used for exposure to mice.
Animals and experimental groups
ApoE−/− C57BL/6 J mice represent a common experimental model for atherosclerosis research. Forty ApoE−/− male mice (7–8 weeks old, weight ranged from 18 g to 20 g) were obtained from Beijing Vital River Laboratory Animal Technology Co., Ltd. Mice were housed in a barrier system at a controlled temperature (22 ± 2 °C) and a relative humidity 40–70%, with a 12 h:12 h light:dark cycle. All animals were given free access to food and water. Atherosclerosis model groups were fed with a high-fat diet (HFD) consisting of 54% regular chow, 20% sugar, 15% lard oil, 7.8% casein, 1.7% calcium hydrogen phosphate, 1.2% cholesterol, and 0.2% bile salt.
Choosing 6 to 10 mice for each group in general mice experiments to meet the statistical requirements, and we chose the median 8. It not only avoided sample size reduction caused by accidental death during the experiment, but also followed the rules of 3R which contain the reduction of animal usage. After 1 week of acclimatization, mice were divided into the following five groups randomly by using random number table (n = 8) and treated with PM2.5 or phosphate buffer saline (PBS): (1) normal control group (normal diet + PBS); (2) HFD control group (HFD + PBS); (3) low-dose group (HFD + PM2.5 0.05 mg/kg of body weight [bw]/week); (4) middle-dose group (HFD + PM2.5 0.50 mg/kg of bw/week); and (5) high-dose group (HFD + PM2.5 5.00 mg/kg of bw/week). Basing on previously reported study [34] and our laboratory former work, different concentrations of coal-fired PM2.5 (0, 0.05, 0.50, and 5.00 mg/kg of bw) were given to ApoE−/− mice once a week (at 8.00–11.00 a.m. of Tuesday) via intratracheal instillation. After 8 weeks treatment [21], mice were sacrificed by cervical dislocation under isoflurane anaesthesia. Whole-blood samples kept at room temperature for 30 min after they were collected through aortas, and then they were centrifuged at 3000 g for 10 min. Sera were collected and stored at − 80 °C. Aortic root samples were fixed in 4% paraformaldehyde and embedded in paraffin, after which they were used for histopathological and immunohistochemical analyses.
Histopathology
As previously reported [35, 36], aortas isolated from all groups were fixed in 4% paraformaldehyde for 48 h and subsequently embedded in paraffin. For histopathological assessment, all samples of aorta root were processed into serial sections with 6-μm thick, and stained with hematoxylin and eosin (H&E).
Immunohistochemistry
Immunohistochemistry was performed as previously described [37]. The paraffin-embedded tissue sections were dewaxed, then immersed in 0.01 mol/L citric acid buffer and heated to boiling in an autoclave for 2 min. After treated with 0.3% hydrogen peroxide solution for 10 min, the tissue sections were blocked with 5% bovine serum albumin (BSA) for 1 h at 37 °C. Then they were washed three times with tris buffered saline (TBS), and were then incubated with primary antibodies (rat anti-mouse intercellular adhesion molecule-1 [ICAM-1] [dilution 1:100] and rabbit anti-mouse E-selectin [dilution 1:25], both purchased from Abcam, UK) for 2 h at 37 °C. The tissue sections were then washed three times with TBS, and treated with appropriate horseradish peroxidase (HRP)- conjugated secondary antibodies for 2 h at 37 °C. Then they were then rinsed three times with TBS again. Antigen-antibody reactions were stained with diaminobenzidine (DAB), and sections were also counterstained with H&E. The expression levels of ICAM-1 and E-selectin were observed with a Nikon E400 microscope under high-power (400×) fields.
Enzyme-linked immunosorbent assays (ELISAs)
The concentrations of Endothelin-1 (ET-1) and von Willebrand factor (vWF) in the mice sera were determined by ELISA kits according to the manufacturer’s recommendations (Abcam, UK).
Western blotting
As previously described [38], proteins were extracted with protein lysate, and a BCA protein assay reagent kit (Beyotime Biotechnology, Shanghai, China) was used to detect their concentrations. Proteins were subjected to electrophoresis on sodium dodecyl sulfate (SDS)– polyacrylamide gels and then the target proteins were transferred onto nitrocellulose membranes. Subsequently, the membranes were blocked for 2 h at room temperature with 5% (wt/vol) milk in TBS with 0.05% (wt/vol) Tween-20. Next, The membranes were washed in tris buffered saline with Tween 20 (TBST) for three times and incubated overnight at 4°Cwith specific primary antibodies. Antibodies for p-p38 (4511S), p38 (9212S), p-JNK (4668S), JNK (9252S), p-ERK (9101S), ERK (9102S), and β-Tubulin (2146S) were obtained from Cell Signaling Technology (Danvers, MA, USA). Then the membranes were washed with TBST three times and were incubated for 2 h at room temperature with horseradish peroxidase-conjugated secondary antibody. After being washed in TBST, protein bands were detected with an enhanced chemiluminescence (ECL) detection kit (GE Health, USA), and quantified by densitometry (Tanon-4500).
Statistical analysis
All data were presented as the mean ± standard deviation (SD). Statistical analyses were performed with SPSS 18.0 software. One-way analysis of variance was used to analyze the differences among multiple groups. P value < 0.05 was considered to be statistically significant.
Results
Body weights and organ coefficients
After 8 weeks of PM2.5 exposure, there was no significant difference in body weights among the experimental groups (Fig. 1). There were also no significant differences in the mediastinal lymph-node weights or coefficients between the normal control group and the HFD control group. However, after 8 weeks of treatment with PM2.5, HFD-fed ApoE−/− mice had significantly increased mediastinal lymph-node weights and coefficients compared with those of HFD control mice (Fig. 2). Compared with the measured parameters in HFD control mice, PM2.5-treatment did not induce any changes in thymus, spleen, liver, or kidney weights—or in their corresponding organ coefficients—in HFD-fed ApoE−/− mice (not shown).
Histopathology
To examine whether coal-fired PM2.5 promotes the formation of atherosclerosis in ApoE−/− mice, we exposed them to coal-fired PM2.5 or PBS for 8 weeks. Cross-sections of aortas were stained with H&E (Fig. 3). In the normal control group, the intimal structure was well-organized and intact. However, the intima was markedly thickened in the HFD control group, and some foam cells were located in the subendothelial layer. Moreover, PM2.5 treatment exacerbated HFD-induced atherosclerosis. Cross-sections of the PM2.5-treated mouse aortas showed atherosclerotic lesions, intimal thickening, fibrous cap formation, and accumulation of foam cells, indicating that coal-fired PM2.5 promoted the formation of atherosclerosis in mice.
The levels of atherosclerosis-related proteins
Compared with the HFD control group, the vWF levels in blood plasma of PM2.5-treatment groups were not increased, but were significantly increased in the normal control group (Fig. 4a). This finding indicated that HFD inhibited the level of vWF in ApoE−/− mice.
The levels of ET-1 in the plasma were significantly increased in PM2.5-treatment groups compared with the HFD control group, whereas they were lower in normal control group compared to the HFD control group (Fig. 4b). This finding indicated that PM2.5 increased the expression of ET-1 in ApoE−/− mice.
Immunohistochemistry revealed a slight increase in the expression of ICAM-1 in the HFD control group relative to that in the normal control group. In addition, PM2.5 treatment significantly increased ICAM-1 expression compared with that in the HFD group (Fig. 4c).
E-selectin expression was also examined by immunohistochemistry (Fig. 4d). There were no visible E-selectin-positive cells in aortas from normal control mice, while HFD significantly increased E-selectin expression. Treatment with PM2.5 plus HFD markedly increased E-selectin expression in mouse aortas.
Phosphorylation levels of components of MAPK signaling pathways
To further investigate the mechanism of PM2.5-induced atherosclerosis, activation of MAPK signaling pathways was examined. As shown in Fig. 5, the phosphorylation levels of p38 MAPK, ERK1/2, and JNK in PM2.5-treatment ApoE−/− mice were significantly increased compared with those in HFD control mice. This finding indicated that coal-fired PM2.5 increased the phosphorylation levels of p38, ERK1/2, and JNK in mouse aortas.
Discussion
PM2.5 presumably exerts atherogenic effects by inducing endothelial damage, mitochondrial injury, inflammatory responses, and oxidative stress [21, 23, 28, 39, 40]. In our present study, PM2.5-treatment significantly increased lymph-node weights and coefficients compared with those of HFD control group. It indicated that in the process of inflammation induced by coal-fired PM2.5 immunocytes might be involved in and play role in injury or recovery. So further studies are needed to elucidate potential mechanisms underlying this phenomenon.
Epidemiological and experimental studies have suggested that PM2.5 exposure is a risk factor which promotes the development of AS [41], and lipids accumulation and fibrous plaques formation in arteries are characters of AS [42, 43]. In our present study, cross-sections of PM2.5-treated mouse aortas exhibited atherosclerotic lesions, intima thickening, fibrous cap formation, and foam cell accumulation, indicating that coal-fired PM2.5 promoted the formation of atherosclerosis in mice.
The expression of adhesion molecules on the endothelium increased during the progression of AS, which involve the recruitment of monocytes into the circulation and trans-endothelial migration [44]. Moreover, eficiencies of adhesion molecules would inhibit monocyte migration and AS formation in mice [36].
vWF is a large glycoprotein [45] that can be produced in endothelial cells and megakaryocytes [46,47,48]. vWF involves the adhesion of platelets to endothelial cells [47], which is associated with the formation of thrombus and atherosclerosis [49, 50]. But It is still controversial whether vWF plays a key regulatory role in the AS formation induced by coal-fired PM2.5. A study showed PM2.5 could increase vWF in old people, but another stuy showed PM2.5 could decrease vWF level in rats [51]. In our study, there was no significant difference in the vWF levels between the PM2.5-treatment mice and the HFD control mice. Our result was consisted with those in the previous study [52], which showed PM2.5 could not increase vWF in young adults. Different results may caused by different species and different physical conditions. Therefore, further studies are needed to elucidate whether vWF is really involved in the process of AS formation induced by PM2.5 or not.
ET-1 is a vasoconstrictor peptide that is synthesized by endothelial cells of the vascular wall [53] and by macrophages [54], and has been demonstrated to be a potent vasoconstrictor [55,56,57,58]. ET-1 directly affects blood vessels and the heart [59] and is implicated in many forms of cardiovascular disease [60,61,62,63]. Studies have demonstrated that the overexpression of ET-1 exacerbates HFD-induced AS in ApoE−/− mice [64, 65]. However, it remains unclear how increased ET-1 expression exacerbates atherosclerotic progression in HFD-fed ApoE−/− mice [64]. In the present study, we found that coal-fired PM2.5 elevated the expression of ET-1 in mice plasma. We can not obtain a very ideal dose-response relationship for this index, there are two reasons may induce such condition. The first is that in the experiment only several mice were used for each group and there must be some sampling error which may influence the representativeness of mean for the population. Second, there is no liner relationship between the dose and the response for this index.
ICAM-1 is a transmembrane glycoprotein [66] and is typically expressed on the surface of endothelial and immune cells [67]. Cell-adhesion molecules, such as ICAM-1, involve in binding and recruitment of circulating leukocytes to the vascular endothelial cells and further migration into subendothelial spaces, which are primary processes of AS [68, 69]. Hence, ICAM-1 may play a key role at the initial stage of AS [70,71,72,73]. In the present study, we found that coal-fired PM2.5 increased the expression of ICAM-1 in ApoE−/− mouse aortas. In addition, a soluble form of ICAM-1 has been found in plasma, which may be involved in the progression of AS [74].
E-selectin is a transmembrane glycoprotein [75] and expressed exclusively on the surface of endothelial cells [76, 77]. E-selectin is important for the initial rolling interaction [78,79,80] and subsequent adhesion [81] of leukocytes in the inflamed endothelium, as well as for the transmigration of inflammatory cells to inflammation sites [76], which are critical events in the initiation of AS [82]. Moreover, monocytes are recruited to lipid-rich plaques mediated by E-selectin during the progression of AS [83]. E-selectin is a hallmark of atherogenesis [84,85,86] and is implicated in the destabilization of atherosclerotic plaques [87]. It has been reported that E-selectin is mostly absent in the healthy endothelial cells but is apparently upregulated in aberrant endothelia that are covered with atherosclerotic plaques in mice and humans [86]. E-selectin is associated with PM2.5 measurements at the day of blood drawing [88]. Our present study found that coal-fired PM2.5 promoted E-selectin expression, indicating that PM2.5 may aggravate arteriosclerosis by inducing upregulation of E-selectin. Taken together, the PM2.5-induced the changes of multiple proteins expression in the present study suggest that these proteins may link coal-fired PM2.5 exposure with the formation of atherosclerosis.
MAPK signaling pathways are a series of parallel cascades of serine/threonine kinases [31] that transduce extracellular signals into cells and induce cellular biological responses [89]. MAPK signaling pathways play an important role in regulating the cardiovascular system [90], and they also influence the formation and development of atherosclerosis [91, 92]. PM2.5 increases ET-1 levels and markedly upregulates p-p38 MAPK expression in vascular smooth muscle cells [93]. Studies have shown that cigarette-smoke extracts upregulate the ICAM-1 and E-selectin expressions via phosphorylation of JNK and ERK pathways [94, 95]. Moreover, a study demonstrated that PM2.5 increases the expression of ICAM-1 in human endothelial cells via ERK pathway [96]. In the present study, western blotting showed that coal-fired PM2.5 induced phosphorylation of p38, JNK, and ERK kinases in mouse aortas. Hence, MAPK signaling pathways may partially link coal-fired PM2.5 exposure with upregulation of ET-1, ICAM-1 and E-selectin.
Conclusion
Coal-derived PM2.5 exacerbated the formation of atherosclerosis in mice, increased the expression levels of atherosclerosis-related proteins (ET-1, ICAM-1 and E-selectinin) in mice serum and promoted the phosphorylation of proteins relevant to MAPK signaling pathway. Therefore, We postulate that MAPK signaling pathway may play a role in the atherosclerosis pathogenesis induced by coal-derived PM2.5. More researches need to be conducted on the relationship between atherosclerosis-related proteins and MAPK signaling pathway and the underlying mechanism needs to be elucidated further in the future.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- AS:
-
Atherosclerosis
- ApoE-/-:
-
Apolipoprotein-E knockout
- BSA:
-
Bovine serum albumin
- CVD:
-
Cardiovascular disease
- DAB:
-
Diaminobenzidine
- ECL:
-
Enhanced chemiluminescence
- ELISA:
-
Enzyme-linked immunosorbent assay
- ERK:
-
Extracellular signal-regulated kinase
- ET-1:
-
Endothelin-1
- FBS:
-
Fetal bovine serum
- H&E:
-
Hematoxylin and eosin
- HFD:
-
High-fat diet
- HRP:
-
Horseradish peroxidase
- ICAM-1:
-
Intercellular adhesion molecule-1
- JNK:
-
c-Jun N-terminal kinase
- MAPK:
-
Mitogen-activated protein kinase
- PBS:
-
Phosphate buffer saline
- PM2.5:
-
Fine particulate matter
- SD:
-
Standard deviation
- SDS:
-
Sodium dodecyl sulfate
- SLE:
-
Systemic lupus erythematosus
- TBS:
-
Tris buffered saline
- TBST:
-
Tris buffered saline with Tween 20
- vWF:
-
von Willebrand factor
- WHO:
-
World Health Organization
References
Gakidou E, Afshin A, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abdulle AM, Abera SF, Aboyans V. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1345–422..
Clark J, Gregory CC, Matthews IP, Hoogendoorn B. The biological effects upon the cardiovascular system consequent to exposure to particulates of less than 500 nm in size. Biomarkers. 2016;21(1):1–47.
Newby DE, Mannucci PM, Tell GS, Baccarelli AA, Brook RD, Donaldson K, Forastiere F, Franchini M, Franco OH, Graham I. Expert position paper on air pollution and cardiovascular disease. Eur Heart J. 2015;36(2):83–93.
Cai X, Li Z, Scott EM, Li X, Tang M. Short-term effects of atmospheric particulate matter on myocardial infarction: A cumulative meta-analysis. Environ Sci Pollut R. 2016;23(7):6139–48.
Pun VC, Kazemiparkouhi F, Manjourides J, Suh HH. Long-term PM2.5 exposure and respiratory, cancer, and cardiovascular mortality in older US adults. Am J Epidemiol. 2017;186(8):961–9.
Chenchen W, Yifan T, Zongliang Y, Rongzhu L. PM2.5 and cardiovascular diseases in the elderly: An overview. Int J Environ Res Public Health. 2015;12(7):8187–97.
Wang FF, Wang XL, Liu FY, Lv ZL, Qian Y, Peng LL. Oxidative injury effect of different compositions of coal-fired PM2.5 on vascular endothelial cells. China Environ Sci. 2014;34:780–5.
Brauer M, Freedman G, Frostad J, van Donkelaar A, Martin RV, Dentener F, van Dingenen R, Estep K, Amini H, Apte JS. Ambient air pollution exposure estimation for the global burden of disease 2013. Environ Sci Technol. 2016;50(1):79–88.
Andersson A, Deng J, Du K, Zheng M, Yan C, Sköld M, Gustafsson Ö. Regionally-varying combustion sources of the January 2013 severe haze events over eastern China. Environ Sci Technol. 2015;49(4):2038–43.
Wang P, Cao J, Shen Z, Han Y, Lee S, Huang Y, Zhu C, Wang Q, Xu H, Huang R. Spatial and seasonal variations of PM2.5 mass and species during 2010 in Xi’an, China. Sci Total Environ. 2015;508:477–87.
Kojima M, Ozawa N, Mori Y, Takahashi Y, Watanabe-Kominato K, Shirai R, Watanabe R, Sato K, Matsuyama T, Ishibashi-Ueda H. Catestatin prevents macrophage-driven atherosclerosis but not arterial injury-induced neointimal hyperplasia. Thromb Haemost. 2018;118(01):182–94.
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C. Heart disease and stroke statistics-2017 update: A report from the american heart association. Circulation. 2017;135(10):e146–603.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, De Ferranti S, Després J, Fullerton HJ. Heart disease and stroke statistics-2016 update: A report from the american heart association. Circulation. 2016;133(4):e38–e360.
Zhang H, Zhao Z, Pang X, Yang J, Yu H, Zhang Y, Zhou H, Zhao J. Genistein protects against ox-LDL-induced inflammation through MicroRNA-155/SOCS1-mediated repression of NF-ĸB signaling pathway in HUVECs. Inflammation. 2017;40(4):1450–9.
Sun Q, Hong X, Wold LE. Cardiovascular effects of ambient particulate air pollution exposure. Circulation. 2010;121(25):2755–65.
Schneider A, Neas L, Herbst MC, Case M, Williams RW, Cascio W, Hinderliter A, Holguin F, Buse JB, Dungan K. Endothelial dysfunction: associations with exposure to ambient fine particles in diabetic individuals. Environ Health Perspect. 2008;116(12):1666–74.
Yatera K, Hsieh J, Hogg JC, Tranfield E, Suzuki H, Shih C, Behzad AR, Vincent R, van Eeden SF. Particulate matter air pollution exposure promotes recruitment of monocytes into atherosclerotic plaques. Am J Physiol Heart Circ Physiol. 2008;294(2):H944–53.
Chen H, Burnett RT, Copes R, Kwong JC, Villeneuve PJ, Goldberg MS, Brook RD, van Donkelaar A, Jerrett M, Martin RV. Ambient fine particulate matter and mortality among survivors of myocardial infarction: population-based cohort study. Environ Health Perspect. 2016;124(9):1421–8.
Geng J, Liu H, Ge P, Hu T, Zhang Y, Zhang X, Xu B, Wang B, Xie J. PM2.5 promotes plaque vulnerability at different stages of atherosclerosis and the formation of foam cells via TLR4/MyD88/NFκB pathway. Ecotoxicol Environ Saf. 2019;176:76–84.
Du X, Jiang S, Zeng X, Zhang J, Pan K, Zhou J, Xie Y, Kan H, Song W, Sun Q. Air pollution is associated with the development of atherosclerosis via the cooperation of CD36 and NLRP3 inflammasome in ApoE −/− mice. Toxicol Lett. 2018;290:123–32.
Pei Y, Jiang R, Zou Y, Wang Y, Zhang S, Wang G, Zhao J, Song W. Effects of fine particulate matter (PM2.5) on systemic oxidative stress and cardiac function in ApoE−/− Mice. Int J Environ Res Public Health. 2016;13(5):484.
Yao H, Lv J. Statin attenuated myocardial inflammation induced by PM2.5 in rats. Acta Cardiol Sin. 2017;33(6):637–45.
Zhu X, Zhao P, Lu Y, Huo L, Bai M, Yu F, Tie Y. Potential injurious effects of the fine particulate PM2.5 on the progression of atherosclerosis in apoE-deficient mice by activating platelets and leukocytes. Arch Med Sci. 2019;15(1):250–61.
Allen RW, Criqui MH, Diez Roux AV, Allison M, Shea S, Detrano R, Sheppard L, Wong ND, Stukovsky KH, Kaufman JD. Fine particulate matter air pollution, proximity to traffic, and aortic atherosclerosis. Epidemiology. 2009;20(2):254–64.
Bauer M, Moebus S, Möhlenkamp S, Dragano N, Nonnemacher M, Fuchsluger M, Kessler C, Jakobs H, Memmesheimer M, Erbel R. Urban particulate matter air pollution is associated with subclinical atherosclerosis: results from the HNR (Heinz Nixdorf recall) study. J Am Coll Cardiol. 2010;56(22):1803–8.
Barbara H, Susanne M, Knut KG, Andreas S, Stefan MH, Nico D, Axel S, Michael M, Raimund E, Karl-Heinz JC. Residential exposure to urban air pollution, ankle-brachial index, and peripheral arterial disease. Epidemiology. 2009;20(2):280–8.
Feng S, Gao D, Liao F, Zhou F, Wang X. The health effects of ambient PM2.5 and potential mechanisms. Ecotoxicol Environ Saf. 2016;128:67–74.
Meng X, Zhang Y, Yang K, Yang Y, Zhou X. Potential harmful effects of PM2.5 on occurrence and progression of acute coronary syndrome: epidemiology, mechanisms, and prevention measures. Int J Environ Res Public Health. 2016;13(8):748.
Hicken MT, Adar SD, Hajat A, Kershaw KN, Do DP, Barr RG, Kaufman JD, Diez Roux AV. Air pollution, cardiovascular outcomes, and social disadvantage: the multi-ethnic study of atherosclerosis. Epidemiology. 2016;27(1):42.
Vargas JD, Manichaikul A, Wang XQ, Rich SS, Rotter JI, Post WS, Polak JF, Budoff MJ, Bluemke DA. Common genetic variants and subclinical atherosclerosis: the multi-ethnic study of atherosclerosis (MESA). Atherosclerosis. 2015;245:230–6.
Zhang H, Zhang R, Chen J, Shi M, Li W, Zhang X. High mobility group box 1 inhibitor glycyrrhizic acid attenuates kidney injury in Streptozotocin-induced diabetic rats. Kidney Blood Press Res. 2018;42(5):894–904.
Hopkins PN. Molecular biology of atherosclerosis. Physiol Rev. 2013;93(3):1317–542.
Wang FF, Geng CM, Hao WD, Zhao YD, Li Q, Wang HM, Qian Y. The cellular toxicity of PM2.5 emitted from coal combustion in human umbilical vein endothelial cells. Biomed Environ Sci. 2016;29(2):107–16.
Zhang Y, Hu H, Shi Y, Yang X, Cao L, Wu J, Asweto CO, Feng L, Duan J, Sun Z. 1 H NMR-based metabolomics study on repeat dose toxicity of fine particulate matter in rats after intratracheal instillation. Sci Total Environ. 2017;589:212–21.
Cheng Z, Chu H, Wang S, Huang Y, Hou X, Zhang Q, Zhou W, Jia L, Meng Q, Shang L. TAK1 knock-down in macrophage alleviate lung inflammation induced by black carbon and aged black carbon. Environ Pollut. 2019;253:507–15.
Cybulsky MI, Iiyama K, Li H, Zhu S, Chen M, Iiyama M, Davis V, Gutierrez-Ramos JC, Connelly PW, Milstone DS. A major role for VCAM-1, but not ICAM-1, in early atherosclerosis. J Clin Invest. 2001;107(10):1255–62.
Kim S, Roh J, Park C. Immunohistochemistry for pathologists: protocols, pitfalls, and tips. J Pathol Transl Med. 2016;50(6):411–8.
Wang S, Jin H, Tang Q, Fu J, Ren Z, Peng C, Shang L, Hao W, Wei X. The effect of ethephon on immune system in male offspring of mice. Environ Toxicol Pharmacol. 2017;49:119–23.
Guan L, Geng X, Stone C, Cosky EEP, Ji Y, Du H, Zhang K, Sun Q, Ding Y. PM2.5 exposure induces systemic inflammation and oxidative stress in an intracranial atherosclerosis rat model. Environ Toxicol. 2019;34(4):530–8.
Pope CA, Bhatnagar A, McCracken JP, Abplanalp W, Conklin DJ, O’Toole T. Exposure to fine particulate air pollution is associated with endothelial injury and systemic inflammation. Circ Res. 2016;119(11):1204–14.
Neill MSO, Diez-Roux AV, Auchincloss AH, Shen M, Lima JA, Polak JF, Barr RG, Kaufman J, David R, Jacobs J. Long-term exposure to airborne particles and arterial stiffness: the multi-ethnic study of atherosclerosis (MESA). Environ Health Perspect. 2011;119:844–51.
Bai Y, Sun Q. Fine particulate matter air pollution and atherosclerosis: mechanistic insights. Biochim Biophys Acta. 2016;1860(12):2863–8.
Dutta P, Hoyer FF, Sun Y, Iwamoto Y, Tricot B, Weissleder R, Magnani JL, Swirski FK, Nahrendorf M. E-Selectin inhibition mitigates splenic HSC activation and myelopoiesis in hypercholesterolemic mice with myocardial infarction. Arterioscler Thromb Vasc Biol. 2016;36(9):1802–8.
Yoon JJ, Lee YJ, Han BH, Choi ES, Kho MC, Park JH, Ahn YM, Kim HY, Kang DG, Lee HS. Protective effect of betulinic acid on early atherosclerosis in diabetic apolipoprotein-E gene knockout mice. Eur J Pharmacol. 2017;796:224–32.
Van Galen K, Tuinenburg A, Smeets EM, Schutgens REG. Von Willebrand factor deficiency and atherosclerosis. Blood Rev. 2012;26(5):189–96.
Doddapattar P, Dhanesha N, Chorawala MR, Tinsman C, Jain M, Nayak MK, Staber JM, Chauhan AK. Endothelial cell-derived von willebrand factor, but not platelet-derived, promotes atherosclerosis in apolipoprotein E-deficient mice. Arterioscler Thromb Vasc Biol. 2018;38:520–8.
Fiodorenko-Dumas Z, Dumas I, Mastej K, Adamiec R. Physical activity – related changes in ADMA and vWF levels in patients with type 2 diabetes – a preliminary study. Adv Clin Exp Med. 2017;26(4):601–8.
Gragnano F, Sperlongano S, Golia E, Natale F, Bianchi R, Crisci M, Fimiani F, Pariggiano I, Diana V, Carbone A. The role of von willebrand factor in vascular inflammation: from pathogenesis to targeted therapy. Mediat Inflamm. 2017;2017:1–13.
Dhanesha N, Prakash P, Doddapattar P, Khanna I, Pollpeter MJ, Nayak MK, Staber JM, Chauhan AK. Endothelial cell-derived von willebrand factor is the major determinant that mediates von willebrand factor-dependent acute ischemic stroke by promoting postischemic Thrombo-inflammation. Arterioscler Thromb Vasc Biol. 2016;36(9):1829–37.
Libby P. Inflammation in atherosclerosis. Arterioscler Thromb Vasc Biol. 2012;32(9):2045–51.
Liang S, Zhao T, Hu H, Shi Y, Xu Q, Miller MR, Duan J, Sun Z. Repeat dose exposure of PM2.5 triggers the disseminated intravascular coagulation (DIC) in SD rats. Sci Total Environ. 2019;663:245–53.
Hassanvand MS, Naddafi K, Kashani H, Faridi S, Kunzli N, Nabizadeh R, Momeniha F, Gholampour A, Arhami M, Zare A. Short-term effects of particle size fractions on circulating biomarkers of inflammation in a panel of elderly subjects and healthy young adults. Environ Pollut. 2017;223:695–704.
Freeman BD, Machado FS, Tanowitz HB, Desruisseaux MS. Endothelin-1 and its role in the pathogenesis of infectious diseases. Life Sci. 2014;118(2):110–9.
Hao L, Wang X, Cheng J, You S, Ma S, Zhong X, Quan L, Luo B. The up-regulation of endothelin-1 and down-regulation of miRNA-125a-5p, −155, and -199a/b-3p in human atherosclerotic coronary artery. Cardiovasc Pathol. 2014;23(4):217–23.
Anunciato IF, Lobo RR, Coelho EB, Verri WAJ, Eckeli AL, Evora PRB, Nobre F, Moriguti JC, Ferriolli E, Lima NK. Big endothelin-1 and nitric oxide in hypertensive elderly patients with and without obstructive sleep apnea-hypopnea syndrome. Arq Bras Cardiol. 2013;101(4):344–51.
Guddeti RR, Prasad A, Matsuzawa Y, Aoki T, Rihal C, Holmes D, Best P, Lennon RJ, Lerman LO, Lerman A. Role of endothelin in microvascular dysfunction following percutaneous coronary intervention for non-ST elevation acute coronary syndromes: A single-Centre randomised controlled trial. Open Heart. 2016;3(2):e428.
Mian MOR, Idris-Khodja N, Li MW, Leibowitz A, Paradis P, Rautureau Y, Schiffrin EL. Preservation of endothelium-dependent relaxation in atherosclerotic mice with endothelium-restricted endothelin-1 overexpression. J Pharmacol Exp Ther. 2013;347(1):30–7.
Soewondo P, Suyono S, Sastrosuwignyo MK, Harahap AR, Sutrisna B, Makmun LH. Prediction of wound healing in diabetic foot ulcers: An observational study in tertiary hospital in Indonesia. Acta Med Indones. 2017;49(1):41–51.
Ju C, Ye M, Li F. Plasma brain natriuretic peptide, endothelin-1, and matrix metalloproteinase 9 expression and significance in type 2 diabetes mellitus patients with ischemic heart disease. Med Sci Monit. 2015;21:2094–9.
Qin Q, Chen M, Yi B, You X, Yang P, Sun J. Orphan nuclear receptor Nur77 is a novel negative regulator of endothelin-1 expression in vascular endothelial cells. J Mol Cell Cardiol. 2014;77:20–8.
Rautureau Y, Schiffrin EL. Endothelin in hypertension: An update. Curr Opin Nephrol Hypertens. 2012;21(2):128–36.
Sánchez A, Martínez P, Muñoz M, Benedito S, García-Sacristán A, Hernández M, Prieto D. Endothelin-1 contributes to endothelial dysfunction and enhanced vasoconstriction through augmented superoxide production in penile arteries from insulin-resistant obese rats: role of ETA and ETB receptors. Brit J Pharmacol. 2014;171(24):5682–95.
Vignon-Zellweger N, Heiden S, Miyauchi T, Emoto N. Endothelin and endothelin receptors in the renal and cardiovascular systems. Life Sci. 2012;91(13–14):490–500.
Li MW, Mian MOR, Barhoumi T, Rehman A, Mann K, Paradis P, Schiffrin EL. Endothelin-1 overexpression exacerbates atherosclerosis and induces aortic aneurysms in apolipoprotein e knockout mice. Arterioscler Thromb Vasc Biol. 2013;33(10):2306–15.
Simeone SMC, Li MW, Paradis P, Schiffrin EL. Vascular gene expression in mice overexpressing human endothelin-1 targeted to the endothelium. Physiol Genomics. 2011;43(3):148–60.
Li T, Liu X, Zhao Z, Ni L, Liu C. Sulodexide recovers endothelial function through reconstructing glycocalyx in the balloon-injury rat carotid artery model. Oncotarget. 2017;8(53):91350–61.
Yang M, Fu Z, Zhang Q, Xin Y, Chen Y, Tian Y. Association between the polymorphisms in intercellular adhesion molecule-1 and the risk of coronary atherosclerosis: A case-controlled study. PLoS One. 2014;9(10):e109658.
Shalini V, Pushpan CK, Sindhu G, Jayalekshmy A, Helen A. Tricin, flavonoid from Njavara reduces inflammatory responses in hPBMCs by modulating the p38MAPK and PI3K/Akt pathways and prevents inflammation associated endothelial dysfunction in HUVECs. Immunobiology 2016;221(2):137–144.
Woollard KJ, Geissmann F. Monocytes in atherosclerosis: subsets and functions. Nat Rev Cardiol. 2010;7(2):77–86.
Chang HH, Chien CY, Chen KH, Huang SC, Chien CT. Catechins blunt the effects of oxLDL and its primary metabolite phosphatidylcholine hydroperoxide on endothelial dysfunction through inhibition of oxidative stress and restoration of eNOS in rats. Kidney Blood Press Res. 2017;42(5):919–32.
Hur HJ, Lee AS. Protective effect of Allium tuberosum extract on vascular inflammation in tumor necrosis factor-α-induced human vascular endothelial cells. J Cancer Prev. 2017;22(4):228–33.
Khodabandehlou K, Masehilano JJ, Poon C, Wang J, Chung EJ. Targeting cell adhesion molecules with nanoparticles using in vivo and flow-based in vitro models of atherosclerosis. Exp Biol Med. 2017;242(8):799–812.
Kim YH, Noh JR, Hwang JH, Kim KS, Choi DH, An JP, Oh WK, Lee CH. Sicyos angulatus ameliorates atherosclerosis through downregulation of aortic inflammatory responses in apolipoprotein E-deficient mice. Exp Ther Med. 2017;14(6):5863–70.
Lawson C, Wolf S. ICAM-1 signaling in endothelial cells. Pharmacol Rep. 2009;61(1):22–32.
Wang Y, Blessing F, Walli AK, Überfuhr P, Fraunberger P, Seidel D. Effects of heparin-mediated extracorporeal low-density lipoprotein precipitation beyond lowering proatherogenic lipoproteins—reduction of circulating proinflammatory and procoagulatory markers. Atherosclerosis. 2004;175(1):145–50.
Skeoch S, Haque S, Pemberton P, Bruce IN. Cell adhesion molecules as potential biomarkers of nephritis, damage and accelerated atherosclerosis in patients with SLE. Lupus. 2014;23(8):819–24.
Winkler IG, Barbier V, Nowlan B, Jacobsen RN, Forristal CE, Patton JT, Magnani JL, Lévesque JP. Vascular niche E-selectin regulates hematopoietic stem cell dormancy, self renewal and chemoresistance. Nat Med. 2012;18(11):1651–7.
Tamagawamineoka R. Important roles of platelets as immune cells in the skin. J Dermatol Sci. 2015;77(2):93–101.
Turan Ç, Kesebir S, Süner Ö. Are ICAM, VCAM and E-selectin levels different in first manic episode and subsequent remission? J Affect Disord. 2014;163:76–80.
Velázquez F, Grodeckipena A, Knapp A, Salvador AM, Nevers T, Croce K, Alcaide P. CD43 functions as an E-selectin ligand for Th17 cells in vitro and is required for rolling on the vascular endothelium and Th17 cell recruitment during inflammation in vivo. J Immunol. 2016;196(3):1305–16.
Zarbock A, Ley K, Mcever RP, Hidalgo A. Leukocyte ligands for endothelial selectins: specialized glycoconjugates that mediate rolling and signaling under flow. Blood. 2011;118(26):6743–51.
Herbin O, Regelmann AG, Ramkhelawon B, Weinstein EG, Moore KJ, Alexandropoulos K. Monocyte adhesion and plaque recruitment during atherosclerosis development is regulated by the adapter protein chat-H/SHEP1. Arterioscler Thromb Vasc Biol. 2016;36(9):1791–801.
Moore KJ, Tabas I. Macrophages in the pathogenesis of atherosclerosis. Cell. 2011;145(3):341–55.
Hadzijusufovic E, Albrecht-Schgoer K, Huber K, Hoermann G, Grebien F, Eisenwort G, Schgoer W, Herndlhofer S, Kaun C, Theurl M. Nilotinib-induced vasculopathy: identification of vascular endothelial cells as a primary target site. Leukemia. 2017;31(11):2388–97.
Jalaly L, Sharifi G, Faramarzi M, Nematollahi A, Rafieian-Kopaei M, Amiri M, Moattar F. Comparison of the effects of Crataegus oxyacantha extract, aerobic exercise and their combination on the serum levels of ICAM-1 and E-Selectin in patients with stable angina pectoris. Daru J Pharma Sci. 2015;23(1):54.
Ma S, Tian XY, Zhang Y, Mu C, Shen H, Bismuth J, Pownall HJ, Huang Y. Wong WT. E-selectin-targeting delivery of microRNAs by microparticles ameliorates endothelial inflammation and atherosclerosis. Sci Rep 2016;6(1):22910.
Hoke M, Winter MP, Wagner O, Exner M, Schillinger M, Arnold Z, Mlekusch W, Maurer G, Koppensteiner R, Minar E. The impact of selectins on mortality in stable carotid atherosclerosis. Thromb Haemost. 2015;114(3):632–8.
Hajat A, Allison M, Diez-Roux AV, Jenny NS, Jorgensen NW, Szpiro AA, Vedal S, Kaufman JD. Long-term exposure to air pollution and markers of inflammation, coagulation, and endothelial activation: A repeat-measures analysis in the multi-ethnic study of atherosclerosis (MESA). Epidemiology. 2015;26(3):310–20.
Yang L, Liu J, Qi G. Mechanism of the effect of saikosaponin on atherosclerosis in vitro is based on the MAPK signaling pathway. Mol Med Rep. 2017;16(6):8868–74.
Madonna R, Massaro M, Pandolfi A, Consoli A, De Caterina R. The prominent role of p38 mitogen-activated protein kinase in insulin-mediated enhancement of VCAM-1 expression in endothelial cells. Int J Immunopathol Pharmacol. 2007;20(3):539–55.
Guo J, Liang W, Li J, Long J. Knockdown of FSTL1 inhibits oxLDL-induced inflammation responses through the TLR4/MyD88/NF-κB and MAPK pathway. Biochem Biophys Res Commun. 2016;478(4):1528–33.
Pan JX. LncRNA H19 promotes atherosclerosis by regulating MAPK and NF-kB signaling pathway. Eur Rev Med Pharmacol Sci. 2017;21(2):322–8.
Wan Q, Liu Z, Yang Y. Puerarin inhibits vascular smooth muscle cells proliferation induced by fine particulate matter via suppressing of the p38 MAPK signaling pathway. BMC Complement Altern Med. 2018;18(1):146.
Cao L, Xu C, Zhang Y, Cao Y, Edvinsson L. Secondhand smoke exposure induces Raf/ERK/MAPK-mediated upregulation of cerebrovascular endothelin ETA receptors. BMC Neurosci. 2011;12(1):109.
Chen H, Lii C, Ku H, Wang T. Cigarette smoke extract induces expression of cell adhesion molecules in HUVEC via actin filament reorganization. Environ Mol Mutagen. 2009;50(2):96–104.
Rui W, Guan L, Zhang F, Zhang W, Ding W. PM2.5-induced oxidative stress increases adhesion molecules expression in human endothelial cells through the ERK/AKT/NF-κB-dependent pathway. J Appl Toxicol. 2016;36(1):48–59.
Acknowledgements
We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Funding
The present study was supported by the National Natural Science Foundation of China (Grant No. 21507122). It is a government fund without any commercial object. The whole grant was spent on experiment reagents. The funding had no role in the design of present study, data collection, analysis and interpretation, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
SW has made contributions to the acquisition, analysis and interpretation of data, drafted the work and substantively revised it. FW has made substantial contributions to the conception, design and revised the work. LY and QL have made contributions to the design of the work. YH, ZC, YS, and LS have made contributions to the acquisition of data. HC has made contributions to the creation of new software used in the work. WH has revised the work. XW has made contributions to the conception, the interpretation of data, and substantively revised the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All animal protocols were approved by the local-research ethics review board of the Animal Ethics Committee of Peking University Health Science Center (ethic code LA2015066).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Highlights
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, S., Wang, F., Yang, L. et al. Effects of coal-fired PM2.5 on the expression levels of atherosclerosis-related proteins and the phosphorylation level of MAPK in ApoE−/− mice. BMC Pharmacol Toxicol 21, 34 (2020). https://doi.org/10.1186/s40360-020-00411-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40360-020-00411-8