Abstract
The powder of root bark of Malva parviflora (Malvaceae) was successively extracted with petroleum ether (b.p. 60–80 °C), chloroform and ethanol. The chloroform extract showed antibacterial activity against Staphylococcus aureus and Escherichia coli, whereas the ethanolic extract showed antibacterial activity against only S. aureus. The chloroform extract, after column chromatographic separation on silica gel using petroleum ether:chloroform (3:1) as eluent, furnished 98 mg of white crystalline compound. The yield of the compound is 0.316 % (w/w). The compound has a melting point of 134–136 °C and the Rf value 0.56 in benzene:chloroform:acetone (1:15:1) on silica gel TLC. The compound was characterized as β-sitosterol by physical properties, chemical test, spectral analysis (FTIR, NMR and MS) and comparing the data obtained from the literature.
Similar content being viewed by others
Background
Populations throughout Africa, Asia and Latin America use traditional medicine to meet their primary healthcare needs (WHO 2002). Although animal parts and minerals have been used, the primary source of traditional medication is herbal medicines (WHO 2000). The majority of Ethiopians depend on herbal medicines as their only source of healthcare, especially in rural areas. Medicinal plants and knowledge of their use provide a vital contribution to human and livestock healthcare needs throughout the country areas (World Bank 2004). Malva parviflora is one of the most widely used herbs in Ethiopia.
Malva parviflora (family: Malvaceae) is native to Northern Africa, Europe and Asia. In Ethiopia, the plant is commonly known as Lit (in Amharic), Lita (in Afaan Oromo), Enkefteha (in Tigrigna) and Uka (in Wolaitta) languages. It often grows in waste places and agricultural farmlands. Malva parviflora is an annual, a biennial or a perennial herb plant. The plant is growing up to 40 in., has a deep strong tap root system and the leaves are dark green and have 5–7 toothed, rounded lobes (Fig. 1).
Malva parviflora has been widely used in many parts of the world for curing various diseases. In South Africa, Xhosa people use a poultice made from the whole plant parts of the plant to treat boils, inflammed purulent wounds and swellings (Afolayan et al. 2008). A hot poultice of leaf is used to treat wounds and swellings in La Reunion, and tea of the leaf is taken as a nervine tonic and used as a taenicide and for profuse menstruation (Sharma and Ali 1999). A dried powder or an infusion of the leaves and roots is used to clean wounds and sores in Lesotho (Afolayan et al. 2008). Tea of the leaf is used for treating dry, irritative cough and bronchitis (Ishtiaq et al. 2012). A decoction of the leaves and roots is also used as a hair rinse to remove dandruff and to soften the hair, and tea of the leaf is also used to clean out the mother’s system after childbirth (Mukul 2012). Seeds are demulcent, used to treat cough and ulcers in the bladder (Sharma and Ali 1999). In Ethiopia, the fresh root bark of M. parviflora is chopped into small pieces and applied on the damaged skin surfaces to treat furuncles, carbuncles, wound infections and other related ailments.
The skin infections such as furuncles and carbuncles are universally caused by Staphylococcus aureus (McCaig et al. 2006). The most common bacteria causing wound infection is S. aureus followed by Escherichia coli (Shittu et al. 2002; Ahmed et al. 2007). Staphylococcus aureus (S. aureus) is a Gram-positive bacterium that can live as a commensal organism on the skin and in the nose and throat (Ryu et al. 2014). Human beings are a natural reservoir for S. aureus; and asymptomatic colonization is far more common than infection (Chambers 2001). Approximately 30 % of healthy people are asymptomatically colonized by S. aureus (Ryu et al. 2014). A transmission of S. aureus may occur by direct contact to a colonized carrier (Chambers 2001). Escherichia coli is a Gram-negative bacillus that belongs to the Escherichia genus which is made up of species present in the human and other animal intestine. When eliminated in the environment together with feces, E. coli contaminates water, soil and food. E. coli strains may cause various infections including infections of the skin wounds (Moş et al. 2010).
Although M. parviflora plays a significant role in traditional medicine in many countries including Ethiopia, only a limited study has been done to scientifically explore antibacterial activity, and there have been no previous reports on the isolation and structural characterization of the bioactive compounds present in this plant. Thus, the present study aimed to evaluate antibacterial activity of root bark of M. parviflora for further structural characterization of bioactive compound(s).
Methods
Collection of the plant material and description the study area
Fresh plant material was collected at the agricultural farmlands area, around Shanto Town (latitude 07°01′28.2″N and longitude 037°55′09.9″E), Damot Pulassa Woreda, Wolaitta Zone, SNNPR, Ethiopia, in October 2012 towards the end of the rainy season. A voucher specimen (083488) has been deposited at the National Herbarium, Addis Ababa University, Addis Ababa, Ethiopia.
Preparation of the plant material
The root parts were washed with tap water followed by distilled water. The bark part was then separated from the root and dried under shade. The dried samples were powdered using a local coffee grinder.
Extraction
The powdered root bark of M. parviflora was successively extracted by Soxhlet extraction with petroleum ether (b.p. 60–80 °C), chloroform and ethanol using standard procedure as described by Jones and Kinghorn (2006). Fifteen grams of the powder was extracted in 300 mL of the solvents. The extractions were carried out for 6 h by petroleum ether, 10 h by chloroform and 15 h by ethanol. The solvents in the filtrates were then evaporated completely using water bath at their boiling points. The dried crude extracts were weighed, and the percentage (%) yields of the extractions process were calculated. The processes were repeated a total of three extractions.
Preparation of extracts solution for antibacterial activity assay
The solutions (each 30 mg/mL) of the ethanolic and chloroform extracts were prepared by dissolving their crude extracts in sterile distilled water and dimethylsulfoxide (DMSO) respectively. The solvents were hence used as a negative control. Serial twofold dilution of each extract was prepared in a concentration ranging from 25 to 2.5 mg/mL for the determination of minimum inhibitory concentration (MIC) value. The antibacterial activity of the root bark of M. parviflora was compared to gentamicin (Ivee Aqua Epz Ltd, Kenya) which is a commercial synthetic antibiotic to S. aureus and E. coli pathogens (Ghalem 2014).
Test bacteria
Two bacterial species namely S. aureus (ATCC 25923) and E. coli (ATCC 20922) were used for antibacterial activity assay. The bacteria pathogens were obtained from Ethiopian Health and Nutrition Research Institute (EHNRI), Addis Ababa, Ethiopia.
Antibacterial activity assay
The antibacterial activity of the extracts was evaluated by Agar Well Diffusion method as described by Mattana et al. (2010) with little modification. Both bacteria strains were inoculated into 10 mL of sterile nutrient broth [Bulux Laboratories (P) Ltd, India] in respective conical flasks and incubated at 37 °C for 24 h. Nutrient agar (Merck KGaA, Germany) medium was prepared, poured into sterilized Petri dishes and allowed to solidify inside the biological safety cabinet. The cultures were then swabbed on the surface of sterile nutrient agar plates using a sterile cotton swab. Three wells (6 mm in diameter) were drilled into each plate, and the solutions of the extracts were added, until wells were filled. After in upright position incubation at 37 °C for 24 h, the diameter of inhibition zones were measured in millimeter (mm). The antibacterial activity assay was determined as the MIC value, which is the minimum concentration of the extract that could inhibit the growth of tested bacteria.
Isolation and purification
The chloroform extract was chromatographed on silica gel 60 (0.063–0.200 mm particle size, Merck KGaA, Germany) column (11 cm length and 2 cm cross section). The silica gel was weighed using a ratio of 10 g of the adsorbent to 1 g of the extract. First, the slurry of weighed silica gel (8 g) was prepared using 100 % petroleum ether and poured into the column. The crude extract (1 g) was dissolved in 2 mL of chloroform in a beaker and adsorbed in 2 g of the silica gel. The mixture was stirred at room temperature until all the chloroform was evaporated off, and put on top of a column of previously packed. Initially, it was eluted with 100 % petroleum ether, and the polarity was gradually increased by adding chloroform at various ratios (Table 1). Totally, 118 fractions were collected (10 mL each) until the compounds were completely eluted from the column. The fractions were monitored by TLC, and then similar fractions having the same Rf values were combined together (Table 1).
Fractions (80–89), showed a major spot with two faint spots, were kept in a fridge at 4 °C for 4 h after addition of a little methanol. The crystals were formed at the bottom of the flask and separated from the mother liquor. The light yellow crystals were further purified by crystallization from methanol (white crystal, 98 mg). The yield of the compound is 0.316 % (w/w). The purity of isolated compound was determined by TLC and melting point before submitting to the spectral analysis.
Thin layer chromatography (TLC)
A small amount of crystals was dissolved in chloroform and spotted on the TLC plate using pre-coated aluminium with 0.20 mm thick silica gel 60 F254 (20 × 20 cm, Merck KGaA, Germany). Then the TLC plate was run by the solvent system of benzene:chloroform:acetone (1:15:1), respectively. After drying at room temperature, the spot was visualized by placing the plate in iodine vapor. The retardation factor (Rf) value was then measured.
Melting point measurement
A melting point (m.p.) measurement was performed by procedure as described by Brittain (2009) on a SA-300H digital melting point apparatus. A few crystals of the compound were placed in a thin walled glass capillary tube and then inserted into the side of the heating block via the hole provided in the apparatus. The compound was then heated until it was melted. The temperature at which the solid began to melt, and that at which it was completely liquid, was recorded as the melting point range of the compound.
Spectra measurement
FTIR spectrum was recorded on a Perkin Elmer 1330 spectrometer with KBr pellets. 1H and 13C NMR spectra were measured on a Bruker DPX 400 MHz and 100.06 MHz spectrometer respectively. High-resolution electrospray ionization mass spectrometry (HR–ESI–MS) measurement was carried out on a Q-Tof Micro YA263 spectrometer in the positive ion mode.
Test for steroid
The test for steroid was performed by Liebermann–Burchard reaction as described by Rajput and Rajput (2012). A few crystals of isolated solid compound were dissolved in chloroform, and a few drops of concentrated sulfuric acid were added to the solution followed by the addition of 3 drops of acetic anhydride. The solution turned violet blue and finally green.
Statistical analysis
The extraction efficiency of the solvents and the zones of inhibition induced by the plant extracts against tested bacteria were given as mean ± SD (where SD is standard deviation) of three replicates. Difference between means zones of inhibition and the standard was determined using students’ test (t-test). The level of statistical significance was set at P ≤ 0.05.
Results and discussion
Extraction
Petroleum ether gave light yellow coloured solid (1.18 ± 0.07 %), chloroform yielded light brown coloured solid (3.22 ± 0.42 %) and ethanol resulted yellow coloured amorphous solid (9.62 ± 0.84 %) crude extracts. The results revealed that different solvents have been found to extract different active principles depending on their polarity, and ethanol could extract the highest amount of materials present in the plant which indicates that the root bark of M. parviflora contains the largest proportion of polar components. The percent yield of petroleum ether is very low and could not allow further chemical study. In the present study, we conducted only the antibacterial activity evaluation on chloroform and ethanolic crude extracts.
Antibacterial activity assay
The chloroform extract showed antibacterial activity against S. aureus (Fig. 2b) and E. coli (Fig. 3a) with the same diameter of zones of inhibition (15 ± 0.41 mm) and MIC value of 20 mg/mL, whereas the ethanolic extract showed antibacterial activity against only S. aureus (Fig. 2a) with diameter of zone of inhibition (18 ± 3.20 mm) and MIC value of 15 mg/mL. The results revealed that S. aureus more sensitive to ethanolic extract than chloroform extract. This is due to stronger extraction capacity of ethanol could have produced greater number of active constituents responsible for antibacterial activity against S. aureus. However, only chloroform extract showed antibacterial activity against E. coli. The fact that the root bark of M. parviflora showed antibacterial activity against S. aureus and E. coli might justify the use of this plant in traditional medicine for the treatment of the diseases caused by tested bacteria pathogens.
It was observed that S. aureus (Gram positive bacterium) is highly susceptible to inhibition by ethanolic extract, whereas E. coli (Gram negative bacterium) did not show growth of inhibition. This may probably be due the morphological differences particularly cell wall composition between the two bacteria species. The Gram-positive bacteria have only an outer peptidoglycan layer which is not effective permeability barrier, whereas the most of the Gram-negative bacteria possess an outer multilayered peptidoglycan and a phospholipidic bilayer. This makes the cell wall impermeable to most of the drugs (Ghansar et al. 2012). Gentamicin (a positive control) caused zones of inhibition 24 ± 1.21 mm (Fig. 2c) and 25 ± 1.04 mm (Fig. 3b) against S. aureus and E. coli respectively. The statistical evaluation revealed that the root bark of M. parviflora showed significantly lower inhibitory activity against both tested bacteria than the standard antibiotic. Sterile distilled water (Fig. 4a) and DMSO (Fig. 4b) did not show any antibacterial activity against tested bacteria.
There have been a few previous reports on the antibacterial activity of M. parviflora. The root of M. parviflora inhibited the growth of S. aureus and E. coli with the zones of inhibition ranged between 0.20 and 0.43 mm (Shale et al. 2005). According to Tadeg et al. (2005) report, the root of M. parviflora showed zone of inhibition (20 ± 0.0 mm) against S. aureus, but no zone of inhibition was noted against E. coli. Furthermore, Kalayou et al. (2012) performed antibacterial activity on the leaves of M. parviflora, and the zones of inhibition were 9.70 ± 1.10 mm for S. aureus and 10.25 ± 2.20 mm for E. coli. In general, the zones of inhibition obtained in the present study are different from results in the previous reports. This is due to several variables which influence the bioactive plant constituents against tested bacteria such as the environmental and climatic conditions under which the plant grow, choice of plant extracts, choice of extraction methods and antimicrobial test method as well (Ncube et al. 2008).
TLC, melting point and steroid test
The isolated compound showed a single spot with Rf value 0.56 and has m.p. of 134–136 °C. A sharp m.p. (just a narrow range of 1–2 °C) indicates that the high purity of the isolated compound (Brittain 2009). The m.p. result of the compound is very close to the literature value (134–135 °C) for β-sitosterol (Hang and Dussault 2010). In steroid test, the compound showed a violet-blue colour, which finally turned into green in Liebermann–Burchard reaction indicating the presence of steroid (Rajput and Rajput 2012).
Spectra analysis
The FTIR spectrum (Fig. 5) showed absorptions band (cm−1) for OH at 3427.85, CH3 at 2959.64 and 2868.72, CH2 at 2868.72 and 2852.27, unconjugated olefinic (C=C) at 1641.91, cyclic methylene groups (CH2)n at 1464.59, gem-dimethyl (–CH(CH3)2) group at 1382.09 and C–OH of secondary alcohol at 1052.35.
The integration of 1H NMR spectrum (Fig. 6) showed the presence of fifty hydrogens: six CH 3 , eleven CH 2 , nine CH and one OH groups (Table 2). The appearance the singlets at δ 0.70 and 1.03 confirming the presence of two CH 3 attached to quaternary carbons. The appearance of the complex multiplets at δ 2.29 and 2.32 is revealed that the two CH 2 adjacent to carbon attached to OH group. The multiplet at δ 3.54 is due to a proton connected to the carbon which attached with OH group. The overlapping triplet signal also appeared for CH at δ 5.37 indicated that the presence of one olefinic proton.
The 13C NMR spectrum (Fig. 7) exhibited the existence of 29 carbons. The carbons could be classified as representing CH 3 , CH 2 , CH or quaternary carbon (QC) by DEPT-135. The DEPT-135 spectrum (Fig. 8) indicated the presence of 26 carbons: six peaks appeared up due CH 3 groups, nine peaks up for CH groups and peaks appeared down indicated the presence of eleven CH 2 groups (Table 2). The absence of three signals in the DEPT-135 spectrum confirmed the presence of three QC atoms. In 13C NMR spectrum, the recognizable signals at 140.77 and 121.73 are assigned for double bond between carbon atoms in position 5 and 6 (C5 = C6), respectively. The signal at δ 71.8 is assigned for C3 β-OH group, and the signals at δ 11.89 and 19.42 are assigned for angular methyl carbons for C19 and C18, respectively. The chemical shift value for C18 is lower due to γ-gauche interaction that increases the screening of the C18. However, the loss of H-atom in C6 results in decrease in screening of the C19 leading to increase in 13C NMR chemicals shift to higher frequency (Pateh et al. 2009).
The mass molecular ion of the compound appeared in HR–ESI–MS spectrum (Fig. 9) at m/z 437.3521 which is approximately 23 higher than the expected because the compound was ionized under positive mode HR–ESI by addition of Na atom. This indicated that the isolated compound with molecular weight of 414.3521, in good agreement with the theoretical value (calculated for C29H50O, 414.7066). The characteristic peak was given at m/z 413.2449 that corresponds to (M‐1) or loss of H. The spectrum showed the most intense peak at m/z 301.1362 that corresponds to (M‐113) or loss of (–C8H17). Other ion peak at m/z 231.1145 is due to the loss of side-chain and ring D fragment, –C13H27 that corresponds to the M-183.
The observed chemical shift values (Table 2) in NMR spectra are very close to values reported in the literature for β-sitosterol (Patra et al. 2010).
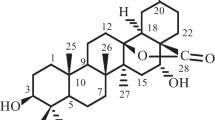
Based on 1H NMR, 13C NMR, DEPT-135 and HR–ESI–MS data, molecular formula of the isolated compound was determined to be C29H50O. Since the isolated compound gave positive test for steroids, all of the other structures other than steroids were rejected. Based upon the functional group analysis, it was found that the nature of oxygen was hydroxyl which is supported by FTIR data. The FTIR spectrum also showed the presence of one C=C in the structure. So, the steroids with other functional groups were rejected. In general, based on the physical properties (crystal with white color and m.p.), steroid test and spectroscopic data (IR, NMR and MS) and comparing the data in the scientific literature, the structure of the isolated compound was determined to be β-sitosterol (Fig. 10).
β-Sitosterol is a natural micronutrient found in the cells and membranes of all oil producing plants, fruit, vegetables, grains, seeds and trees (Sen et al. 2012). It is commercially available in preparative amounts only as mixtures with other phytosterols typically stigmasterol and campesterol (Hang and Dussault 2010). β-Sitosterol has been proven to be a safe, nontoxic, effective nutritional supplement and has amazing potential health benefits in many diverse applications including antibacterial activity (Sen et al. 2012). Earlier experimental studies have shown that β-sitosterol has antibacterial activity against different bacteria species including S. aureus and E. coli. According to Sen et al. (2012) and Joy et al. (2012) reports, β-sitosterol inhibited the growth of S. aureus (17.83 ± 0.58 mm) and E. coli (14.5 ± 1.84 mm) and S. aureus (13 mm) and E. coli (14 mm) respectively. So, the study suggested that the presence of β-sitosterol in chloroform extract of the root bark M. parviflora might contribute to its potency of growth inhibition against tested bacteria.
Conclusions
The antibacterial activity assay showed that the ethanolic and chloroform extracts of the root bark M. parviflora possess active compound to inhibit the growth of bacteria species: S. aureus and E. coli. This is in agreement with the use of this plant in traditional medicine for the treatment of furuncles, carbuncles, wound infections and other related ailments. In chromatographic separation, β-sitosterol was isolated from chloroform extract of the root bark of M. parviflora. Although β-sitosterol is a known natural product, this is the first report of the isolation from this plant and its structural characterization.
References
Afolayan AJ, Aboyade OM, Sofidiya MO (2008) Total phenolic content and free radical scavenging activity of Malva parviflora L. (Malvaceae). J Biol Sci 8(5):945–949
Ahmed M, Alam SN, Khan O, Manzar S (2007) Post-operative wound infection: a surgeon’s dilemma. Pak J Surg 23(1):41–47
Brittain CG (2009) Using melting point to determine purity of crystalline solids. https://www.chm.uri.edu/mmcgregor/chm228/use_of_melting_point_apparatus.pdf. Accessed 10 Apr 2016
Chambers HF (2001) The changing epidemiology of Staphylococcus aureus? Emerg Infect Dis 7(2):178–182
Ghalem BR (2014) Effect of essential oils of Artemisia arborescens on Escherichia coli, Staphylococcus aureus and Pseudomonas aeruginosa. J Plant Sci 2(6–1):1–4
Ghansar NH, Bhopale SU, Prabhune VS (2012) In Vitro studies of antimicrobial properties of extracts from Unani medicinal plants. Int J Pharm Bio Sci 3(1):B-240–B-249
Hang J, Dussault P (2010) A concise synthesis of β-sitosterol and other phytosterols. Steroids 75(12):879–883
Ishtiaq S, Saeed-Ul-Hassan S, Niaz U, Saeed MA (2012) Identification and evaluation of counter-irritant potential of crude extract of Malva parviflora L. by WHO recommended methods. Pak J Pharm Sci 25(3):589–594
Jones WP, Kinghorn AD (2006) Extraction of plant secondary metabolites. In: Sarker SD, Latif Z, Gray AI (eds) Natural products isolation, 2nd edn. Humana Press, Totowa
Joy HH, Krishna V, Jignesh S, Sanjay ST, Roshan A, Vijay S (2012) In-Silico drug designing using β-sitosterol isolated from Flaveria trinervia against peptide deformylase protein to hypothesize bactericidal effect. Int J Pharm Pharm Sci 4(2):192–196
Kalayou S, Haileselassie M, Gebre-egziabher G, Tiku’e T, Sahle S, Taddele H, Ghezu M (2012) In-vitro antimicrobial activity screening of some ethnoveterinary medicinal plants traditionally used against mastitis, wound and gastrointestinal tract complication in Tigray Region, Ethiopia. Asian Pac J Trop Biomed 2(7):512–522
Mattana CM, Satorres SE, Sosa A, Fusco M, Alcaráz LE (2010) Antibacterial activity of extracts of Acacia aroma against methicillin-resistant and methicillin-sensitive Staphylococcus. Braz J Microbiol 41:581–587
McCaig LF, McDonald LC, Mandal S, Jernigan DB (2006) Staphylococcus aureus-associated skin and soft tissue infections in ambulatory care. Emerg Infect Dis 12(11):1715–1723
Moş I, Micle O, Zdrâncă M, Mureşan M, Vicaş L (2010) Antibiotic sensitivity of the Escherichia coli strains isolated from infected skin wounds. Farmacia 58(5):637–645
Mukul (2012) Malva parviflora | Find Me A Cure www.findmeacure.com/2012/08/06/malva-parviflora/. Accessed 5 Sept 2012
Ncube NS, Afolayan AJ, Okoh AI (2008) Assessment techniques of antimicrobial properties of natural compounds of plant origin: current methods and future trends. Afr J Biotechnol 7(12):1797–1806
Pateh UU, Haruna AK, Garba M, Iliya I, Sule IM, Abubakar MS, Ambi AA (2009) Isolation of stigmasterol, β-sitosterol and 2-hydroxyhexadecanoic acid methyl ester from the rhizomes of Stylochiton lancifolius Pyer and Kotchy (Araceae). Niger J Pharm Sci 8(1):19–25
Patra A, Jha S, Murthy PN, Manik Sharone A (2010) Isolation and characterization of stigmast-5-en-3β-ol (β-sitosterol) from the leaves of Hygrophila spinosa T. Anders. Int J Pharma Sci Res 1(2):95–100
Rajput AP, Rajput TA (2012) Isolation of stigmasterol and β-sitosterol from chloroform extract of leaves of Corchorus fascicularis Lam. Int J Biol Chem 6(4):130–135
Ryu S, Song PI, Seo CH, Cheong H, Park Y (2014) Colonization and infection of the skin by S. aureus: immune system evasion and the response to cationic antimicrobial peptides. Int J Mol Sci 15:8753–8772
Sen A, Dhavan P, Shukla KK, Singh S, Tejovathi G (2012) Analysis of IR, NMR and antimicrobial activity of β-sitosterol isolated from Momordica charantia. Sci Secure J Biotech 1(1):9–13
Shale TL, Stirk WA, van Staden J (2005) Variation in antibacterial and anti-inflammatory activity of different growth forms of Malva parviflora and evidence for synergism of the anti-inflammatory compounds. J Ethnopharmacol 96:325–330
Sharma SK, Ali M (1999) A new stigmastane derivative isolated from root of Malva parviflora. Ind J Chem 38B:746–748
Shittu AO, Kolawole DO, Oyedepo EAR (2002) A study of wound infections in two health institutions in Ile-Ife, Nigeria. Afr J Biomed Res 5:97–102
Tadeg H, Mohammed E, Asres K, Gebre-Mariam T (2005) Antimicrobial activities of some selected traditional Ethiopian medicinal plants used in the treatment of skin disorders. J Ethnopharmacol 100:168–175
WHO (2000) General guidelines for methodologies on research and evaluation of traditional medicine. World Health Organization, Geneva
WHO (2002) Policy perspectives on medicines-traditional medicine-growing needs and potential. No. 2. World Health Organization, Geneva
World Bank (2004) Indigenous knowledge-local pathways to global development. Knowledge and Learning Group, Africa Region, The World Bank, Washington
Authors’ contributions
MMO collected and prepared the sample, designed experiments, interpreted the data and prepared the manuscript. MKC and AHD are supervisors of this research and guided the progress of the work. All authors read and approved the final manuscript.
Acknowledgements
This work was financially supported by Ministry of Education of the Federal Democratic Republic of Ethiopia.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ododo, M.M., Choudhury, M.K. & Dekebo, A.H. Structure elucidation of β-sitosterol with antibacterial activity from the root bark of Malva parviflora . SpringerPlus 5, 1210 (2016). https://doi.org/10.1186/s40064-016-2894-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40064-016-2894-x