Abstract
Background
Epidemiologic evidence suggested that remnant cholesterol (RC) is associated with the occurrence of cardiovascular disease (CVD). In recent years, RC has been connected with different types of cardiometabolic disorders. We aim to clarify the relationship among RC, metabolic syndrome (MetS) and subsequent CVD.
Methods
We enrolled 7471 individuals into our study from China Health and Nutrition Survey in 2009 and followed participants till 2015. RC was calculated as total cholesterol minus low-density lipoprotein cholesterol minus high-density lipoprotein cholesterol. CVD was defined as myocardial infarction and stroke. Multivariate logistic regression and Cox regression models were used to evaluate the association between RC and MetS as well as CVD. We further investigated whether the association between RC and CVD was mediated by MetS.
Results
Of all subjects, 24.73% were diagnosed with MetS and 2.74% developed CVD. Multivariate logistic regression analysis elucidated that per-tertile-increase in RC was associated with MetS after adjusting all the confounder factors, (odds ratio: 3.49, 95% confidence interval CI 3.21–3.79, P for trend < 0.001). And per-tertile-increase RC had a significant increased risk of CVD (hazard ratio: 1.26, 95% CI 1.06–1.50, P for trend = 0.008). Meanwhile, we found that RC level is associated with the prevalence of all the components of MetS. Significant indirect effects of RC between MetS and CVD were found, with the index mediated at 48.46% of the association.
Conclusions
Our study provides the evidence that RC level is independently associated with the prevalence of MetS and each component of MetS. MetS partially mediated the association between RC level and CVD risk.
Similar content being viewed by others
Background
According to the World Health Organization (WHO) data, cardiovascular disease (CVD) are the leading cause of death globally taking an estimated 17.9 million lives each year, with heart attacks and strokes accounting for 85% of deaths [1]. Metabolic syndrome (MetS) is a constellation of many cardio-metabolic risk factors and is associated with increased all-cause and CVD mortality risk, and as such has been arising peoples’ attention as a serious public health issue [2]. Meanwhile, the prevalence of MetS has increased in recent decades, independent of any kind of criteria for diagnosis, keeping pace with the epidemic of CVD [3]. According to previous research, the pathogenesis of MetS is not only attributable to neurohormonal activation, but also insulin resistance and chronic low-grade inflammation as well [4]. Moreover, elevated inflammatory cytokines are considered a high risk factor for the development of CVDs, and insulin resistance is regarded as one of the earliest demonstrations of CVD [5,6,7].
Remnant cholesterol (RC), a novel atherogenic lipoprotein, is the cholesterol content within triglyceride-rich lipoproteins, consisting primarily of very low-density lipoproteins, intermediate-density lipoproteins and chylomicron remnants. Based on a standard lipid profile, RC is usually calculated as total cholesterol minus low-density lipoprotein cholesterol (LDL-C) minus high-density lipoprotein cholesterol (HDL-C) [8]. According to a study by Johns Hopkins Medicine researchers, RC is as a stand-alone risk for CVD such as myocardial infarction and stroke [9]. Additionally, an epidemical study showed that with the level of RC increasing, the prevalence of diabetes mellitus (DM), lipid disorders and even hypertension is higher [10,11,12,13], which means that RC may act as a representative factor in a state of cardio-metabolic disorder. Interestingly, mechanistic evidence revealed that high concentrations of RC is related to low-grade inflammation and is genetically mediated by insulin resistance [14,15,16]. RC and MetS are linked by a positive feedback loop involving insulin resistance, chronic inflammation, abnormal lipid metabolism, and hypertension. RC affects these factors and is also affected by them, leading to faster MetS progression [17,18,19,20]. Such findings suggest significant similarities between concomitant alterations of RC and MetS in the underlying pathogenesis. Although RC was proposed as a new agent of cardiovascular risk factor, with association of many cardiometabolic disorders, the relationship between RC and MetS still unclear. Furthermore, the role of MetS played in the association between RC and CVD remains unknown.
In order to fill the knowledge gap, we investigated the correlation of RC with the prevalence of MetS and subsequent CVD based on the China Health and Nutrition Survey (CHNS). And whether the presence of MetS mediates the effect of RC on CVD.
Methods
Study setting and population
This study used data from the CHNS, an ongoing longitudinal community-based cohort study carried out by the national and local governments of China. The study includes data for more than 12,000 individuals across approximately nine provinces. Trained researchers conducted household surveys, using standard questionnaires and face-to-face interviews to obtain information about participants. Each participant provided written informed consent. Study details are described in our previous article [21], and the relevant protocol is published elsewhere [22]. The inclusion criteria were: (1) age ≥ 18 years old, (2) measurement of RC level. The exclusion criteria were: (1) pregnant women, (2) without sufficient information to diagnose MetS. We first removed 2466 participants that lacked fasting blood samples, then we excluded 1054 participants without RC measurement, 741 participants who were under 18 years of age, 57 pregnant women, 226 participants without sufficient information to diagnose MetS (Fig. 1). Based on the aforementioned criteria, 7471 eligible participants were identified. We also presented demographic information, health behaviors, health status and laboratory examinations of study participants. After six years follow-up, 205 patients diagnosed with CVD, with 1041 individuals loss follow-up.
This manuscript was written in strict accordance with the STROBE statement [23].
Measures
RC (mmol/L) was calculated as total cholesterol (TC) (mmol/L) minus LDL-C (mmol/L) minus HDL-C (mmol/L) and blood sample were obtained in the fasting state [24]. MetS was diagnosed according to the International Diabetes Federation as individuals with central obesity (waist circumference ≥ 90 cm in men or ≥ 80 cm in women) plus any two of the following: (1) raised TG (> 1.7 mmol/L) or specific treatment for TG abnormality; (2) reduced HDL-C in men (< 1.03 mmol/L) and in women (< 1.29 mmol/L) or specific treatment for TG abnormality; (3) raised blood pressure (SBP ≥ 130 mm Hg or DBP ≥ 85 mmHg) or treatment of previously diagnosed hypertension; (4) raised fasting plasma glucose (fasting plasma glucose ≥ 5.6 mmol/L) or previously diagnosed type 2 DM [25]. CVD was defined as myocardial infarction or stroke and was derived by medical diagnosis [26]from doctors.
Definition
Height and weight were measured while the subjects were wearing light clothing and standing without shoes. We calculated body mass index (BMI) as weight (kg)/height (m)2. Health behaviors (smoking and alcohol consumption), education background and residence were self-reported. Smoking was defined as any previous smoking (yes/no), and alcohol consumption was defined as imbibition greater than three times per week (yes/no). Renal function was presented as eGFR using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [27]. Nutrition intake was assessed through questionnaire that included 24 h diet recalls about the food on the same 3 days (2 week days and 1 weekend day). Energy intake, carbohydrate intake, fat intake and protein intake were calculated by multiplying the intake of each food from the average dietary intake for 3 days by the standard serving size (100 g). Physical activity was defined as more than 150 min of moderate exercise or more than 75 min of vigorous exercise per week [28]. Creatinine, uric acid, fasting blood glucose, HDL-C, LDL-C, TG, TC,were measured using a Hitachi 7600 machine (Randox, UK and Kyowa, Japan). HbA1c was detected by HLC-723 G7/D10/PDQ A1c (Tosoh, Japan/Bio-Rad, USA/Primus, USA). Insulin was detected by Gamma counter XH-6020,China (North Institute of Bio-Tech,China). High-sensitivity C-reactive protein (Hs-CRP) was measured by Hitachi 7600 machine (Denka Seiken, Japan).
Homeostatic model assessment of insulin resistance (HOMA-IR) was calculated by: fasting insulin (µIU/mL) × fasting glucose (mmol/L)/22.5.
Statistical methods
Participant characteristics were described based on tertiles of RC. Continuous variables are expressed as means ± standard deviation for normal distributions or medians and interquartile range (25% to 75%) for skewed distributions. Categorical variables are presented as relative frequencies (percentages). Each tertile of RC was taken as a unit and p-values for trends were calculated using linear-regression analyses for continuous variables and Cochran-Armitage test for categorical variables. We used an upset and correlation plot to show the distribution of different combinations of MetS components and the relationships between the MetS components. Generalized additive models were then used to identify relationships between RC and the prevalence of each MetS component, since RC was a continuous variable. The independent association of RC with MetS and CVD were evaluated using logistic models with odds ratios (ORs) and 95% confidence intervals (CIs), and Cox regression models with hazard ratios (HRs) and 95% CIs. Potential covariates that were significant in the baseline comparison, or that we considered to be of clinical importance were included in the multivariate models. We established two main models for covariate adjustment: crude model; adjusted model for age, sex, education, residence, smoking, alcohol consumption, protein intake, carbohydrate intake, fat intake, daily energy intake and physical activity. Subgroup analyses and effect modification were performed considering age (< 60/ ≥ 60 years old), sex (male/female), education levels (middle school and below/high school and above), alcohol consumption (yes/no), smoking(yes/no) and residence(urban/rural). Finally, given that the MetS has been identified as a way through which RC may affect the CVD, we investigated whether the association between RC and CVD was mediated by MetS. The bootstrap test was used to assess the effects of these mediators [29].
The sensitivity analysis was conducted by adopting the WHO criterion to diagnose MetS [26]. The proportion of missing data in the analytic sample did not exceed 2%. Missing data were interpolated using the method of last observation carried forward or using the means and medians for continuous variables and skewed variables. Comparisons where P was < 0.05 (two-sided) were considered to be statistically significant. We performed all analyses with Stata 15.0, R (version 3.4.3) and EmpowerStats (http://www.empowerstats.com, X and Y Solutions, Inc., Boston, MA).
Results
Baseline information
Demographic characteristics of the study population are summarized in Tables 1 and 2. Among the 7471 participants, there were 1848 individuals (24.74%) who had MetS and 205 individuals (2.74%) with CVD. Urban residents accounted for the majority of subjects across the different RC groups. Subjects with MetS exhibited statistically higher RC levels and had significantly higher BMI, uric acid, creatinine, LDL-C, TG, TC, HOMA-IR, Hb1Ac, fasting blood glucose, and insulin levels. Conversely eGFR and HDL-C levels were significantly lower within the elevated RC tertile. Compared with lower-level RC group, subjects within higher tertiles of RC were older, more educated, and engaged in smoking and alcohol consumption more frequently, and their protein intake was also higher. Participants were spilt into two groups, according to whether MetS was present. Female and urban residents accounted for the majority of subjects in the group with MetS. These subjects were statistically significant higher in age, BMI, uric acid, Hs-CRP, LDL-C, TG, TC, RC, HOMA-IR, HbA1c, fasting blood glucose, carbohydrate intake, daily energy intake and insulin levels. Subjects with MetS also had statistically significantly lower HDL-C and eGFR when compared to participants without MetS.
The intersection distribution of different metabolic disorders
By analyzing the upset plot (Fig. 2), we observed that among the general metabolic disorders, individuals with expanded waist circumference were the most prevalent in the general population, and participants with low HDL-C were relatively rare by contrast. Corresponding to the diagnosis of MetS, the population with all five factors coexisting accounted for the majority of MetS cases, while the proportion of the participants with the combination of expanded waist circumference, high blood glucose and low HDL-C was comparatively small.
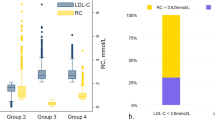
The association of RC and MetS
Table 3 shows the association between RC tertiles and prevalence of MetS. By using logistic regression models, per-tertile-increase in RC were associated with 317% increasing risk for MetS (OR: 3.17, 95% CI 2.93–3.43, P for trend < 0.001). After adjusting for age, sex, education, residence, alcohol consumption, protein intake, carbohydrate intake, fat intake, daily energy intake and physical activity, the result remained significant (OR: 3.49, 95% CI 3.21–3.79, P for trend < 0.001). As shown in Fig. 3, with rising concentration of RC, the prevalence of MetS, abdominal obesity, elevated triglycerides, reduced HDL-C, elevated blood pressure, and abnormal glucose metabolism simultaneously increased. After analyzing the correlation between RC and each component of MetS in Fig. 4, we found out that RC level had a positive correlation with waist circumference, abnormal glucose metabolism, raised blood pressure and triglyceride levels, with the triglycerides serving as the most relevant factor for RC. All components were correlated with each other positively except for reduced HDL-C, which has negative correlation with RC, triglyceride, abnormal glucose metabolism and waist circumference. Though, HDL-C is irrelevant to raised blood pressure.
The association of RC and new-onset CVD
After a median follow-up of 6 years, we identified 205 (2.74%) subjects who developed CVD. By using the Cox regression analysis in Table 4, RC had a significant correlation with risk of CVD in crude model (HR: 1.22, 95% CI 1.03–1.45, P for trend = 0.021). After adjusting for age, sex, education, residence, alcohol consumption, protein intake, carbohydrate intake, fat intake, daily energy intake and physical activity, the result remained significant (HR: 1.26, 95% CI 1.06–1.50, P for trend = 0.008).
Subgroup analysis
Subgroup analyses of the asocciation between RC, MetS and CVD was listed in Table 5 and Table 6. There was an interaction between age and RC for MetS, as people under 60 years old at high RC levels were significantly associated with MetS (OR: 3.84, 95%CI 3.45–4.29, P for interaction < 0.001). However, other stratification factors such as sex, education, alcohol consumption, smoking and residence had no interaction with RC regarding the incidence of metabolic syndrome. No interaction were found of all subgroups in the relationship between RC and CVD.
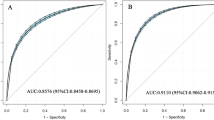
Mediation analysis
Potential mediation effects of RC in the correlation between MetS and CVD are presented in Fig. 5. We observed significant indirect effects of RC between MetS and CVD with mediation at 48.46% of the association.
Sensitivity analysis
To consolidate our result, we conducted the sensitivity analysis base on the different diagnostic criterion of MetS (WHO standard) and the results were listed below in Table 7 and Fig. 6. We re-did the mediation analysis and logistic regression. The results were similar to the main results.
Discussion
In this nationwide study, we found that RC was significantly associated with the prevalence of MetS and incidence of CVD. RC was also positively related with the each component of MetS, which was most relevant to elevated triglycerides and has minimal correlation with raised blood pressure. Additionally, MetS partially mediates the relationships between RC and CVD.
A remarkable increase in the prevalence of obesity is garnering greater the attention from the public [30]. Obesity is a predominant contributor to MetS, and the presence of the obesity elevates the risk of dyslipidemia by raising the concentration of TG levels and lowering concentration of the HDL-C [31, 32]. In the present study, with increasing tertile of RC, the prevalence of elevated triglycerides and reduced HDL-C were higher, which was consistent with previous studies. Besides, the correlation between RC and TG was the highest compared to RC and other components of MetS, which was in line with previous research which pointed out that TG was primarily carried by the remnants and the concentration of TG was highly increased with the elevated levels of RC [12, 33]. At the same time, levels of the HDL-C decreased as levels of the RC increased because of the exchange of the TGs and cholesterol between the HDL-C and remnants in plasma [11, 34]. The reverse correlation between the HDL-C and RC was in line with our results. Previous epidemiological studies found that elevated RC along with a higher prevalence of DM, as such RC may be a predictor of diabetes or prediabetes and hypertension [35, 36]. Additionally, a study of a population of 7308 individuals recruited from CHNS showed that the concentration of RC was associated with DM beyond the LDL-C [37]. Besides, RC also had a substantial connection with the prediction or diagnosis of hypertension, and could be used as a blood marker for screening [38, 39]. A recent study, which included more than 8 million Korean adults, found that RC provide additional information in predicting future progression of type 2 DM, independent of the conventional lipid parameters [40]. All of the above evidence indicated that RC level was highly relevant to cardiometabolic disorders.
Furthermore, our study found that MetS mediated the association between RC and new-onset CVD. Previous study found that RC levels of ≥ 1 mmol/L (39 mg/dL) was presented in 22% of the population, which was associated with a two-fold increase in mortality from cardiovascular and other causes [41]. High levels of both RC and LDL-C were associated with a higher risk of CVD than either one indicator alone [42]. Elevated RC levels, independent of LDL-C levels, were also associated with an increased risk of incident CVD. Thses findings were novel and similar to our findings. In recent years, RC had attracted a lot of attention as a residual cardiovascular risk factor in many large cohort studies, and was highly instrumental due to its great atherogenic capacity [43, 44]. Unlike LDL-C, RC is free to enter the intima and become trapped in the connective tissue matrix, and could also be taken up by macrophages without modification. Furthermore, it is difficult for RC to diffuse back to blood stream, since RC has larger scales compared to LDL-C [45, 46]. Our study suggested that the association between RC and CVD may be related not only to RC causing systemic low-level inflammation and insulin resistance, but also due to RC causing a series of abnormal manifestations of cardiovascular metabolism represented by MetS which accelerated the development of CVD. However, more studies are required to support this mechanistic correlation.
Therefore, the monitoring of RC, as a simple method, could further facilitate the prevention of CVD. Special attention needs to be paid to the cardiometabolic disorders when we studied RC, in order to early identify its related metabolic risks. Future studies are needed to provide evidence that whether a reduction in RC could reduce the risk of CVD by improving metabolic status.
Limitations
Several limitations of the current study should be taken into consideration. First, due to the nature of cross-sectional design of the current study, we can only determine the associations between RC and MetS, rather than causality. Future prospective studies are needed to identify the mechanism by which elevated RC is associated with increased risk of MetS. Second, in the current study we calculated the concentration of RC from a standard lipid profile as total cholesterol minus LDL-C minus HDL-C, which was not as accurate as direct approaches like ultracentrifugation or nuclear magnetic resonance spectroscopy. However, owing to the side effects of using such laborious methods like cost and time-consumption, it is not appropriate for their use to be widespread. Third, although our analysis utilized different approaches to support our discovery, we must be cautious when explaining these results as some observed associations may be accidental. For instance, family history of CVD and other chronic diseases may influence the current findings, but this information was not provided by CHNS. Finally, repeated analysis across different ethnic groups may enhance the extrapolation of conclusions.
Conclusions
In summary, our study provided the evidence that RC level was independently associated with the prevalence of MetS and incidence of CVD, and was also primarily connected with each component of MetS. Insulin resistance and inflammation need to be considered as intermediate pivotal links between RC, MetS and CVD. Ultimately, MetS partially mediated the association between RC level and CVD risk, and the intrinsic mechanism by which this occurs needs further investigation.
Availability of data and materials
The data analyzed in this study can be available at: https://www.cpc.unc.edu/projects/china.
Abbreviations
- BMI:
-
Body mass index
- CHNS:
-
China Health and Nutrition Survey
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetes mellitus
- eGFR:
-
Estimated glomerular filtration rate
- HbA1c:
-
Hemoglobin A1c
- HDL-C:
-
High-density lipoprotein cholesterol
- HOMA-IR:
-
Homeostatic model assessment for insulin resistance
- Hs-CRP:
-
High-sensitivity C-reactive protein
- LDL-C:
-
Low-density lipoprotein cholesterol
- MetS:
-
Metabolic syndrome
- OR:
-
Odds ratio
- RC:
-
Remnant cholesterol
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- 95% CI:
-
95% confidence interval
References
Cardiovascular diseases (CVDs) n.d. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) Accessed 22 Aug 2023.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56:1113–32. https://doi.org/10.1016/j.jacc.2010.05.034.
Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018;20:12. https://doi.org/10.1007/s11906-018-0812-z.
Fahed G, Aoun L, Bou Zerdan M, Allam S, Bou Zerdan M, Bouferraa Y, et al. Metabolic syndrome: updates on pathophysiology and management in 2021. Int J Mol Sci. 2022;23:786. https://doi.org/10.3390/ijms23020786.
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377:1119–31. https://doi.org/10.1056/NEJMoa1707914.
James DE, Stöckli J, Birnbaum MJ. The aetiology and molecular landscape of insulin resistance. Nat Rev Mol Cell Biol. 2021;22:751–71. https://doi.org/10.1038/s41580-021-00390-6.
Laakso M, Kuusisto J. Insulin resistance and hyperglycaemia in cardiovascular disease development. Nat Rev Endocrinol. 2014;10:293–302. https://doi.org/10.1038/nrendo.2014.29.
Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet. 2014;384:626–35. https://doi.org/10.1016/S0140-6736(14)61177-6.
Quispe R, Martin SS, Michos ED, Lamba I, Blumenthal RS, Saeed A, et al. Remnant cholesterol predicts cardiovascular disease beyond LDL and ApoB: a primary prevention study. Eur Heart J. 2021;42:4324–32. https://doi.org/10.1093/eurheartj/ehab432.
Ye X, Kong W, Zafar MI, Chen L-L. Serum triglycerides as a risk factor for cardiovascular diseases in type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Cardiovasc Diabetol. 2019;18:48. https://doi.org/10.1186/s12933-019-0851-z.
Nordestgaard BG, Tybjærg-Hansen A. Genetic determinants of LDL, lipoprotein(a), triglyceride-rich lipoproteins and HDL: concordance and discordance with cardiovascular disease risk. Curr Opin Lipidol. 2011;22:113–22. https://doi.org/10.1097/MOL.0b013e32834477d2.
Varbo A, Benn M, Nordestgaard BG. Remnant cholesterol as a cause of ischemic heart disease: evidence, definition, measurement, atherogenicity, high risk patients, and present and future treatment. Pharmacol Ther. 2014;141:358–67. https://doi.org/10.1016/j.pharmthera.2013.11.008.
de Graaf J, van der Vleuten GM, ter Avest E, Dallinga-Thie GM, Stalenhoef AFH. High plasma level of remnant-like particles cholesterol in familial combined hyperlipidemia. J Clin Endocrinol Metab. 2007;92:1269–75. https://doi.org/10.1210/jc.2006-1973.
Basu D, Bornfeldt KE. Hypertriglyceridemia and atherosclerosis: using human research to guide mechanistic studies in animal models. Front Endocrinol. 2020;11:504. https://doi.org/10.3389/fendo.2020.00504.
Varbo A, Benn M, Tybjærg-Hansen A, Nordestgaard BG. Elevated remnant cholesterol causes both low-grade inflammation and ischemic heart disease, whereas elevated low-density lipoprotein cholesterol causes ischemic heart disease without inflammation. Circulation. 2013;128:1298–309. https://doi.org/10.1161/CIRCULATIONAHA.113.003008.
Nordestgaard BG. Triglyceride-rich lipoproteins and atherosclerotic cardiovascular disease: new insights from epidemiology, genetics, and biology. Circ Res. 2016;118:547–63. https://doi.org/10.1161/CIRCRESAHA.115.306249.
Lewis GF, Carpentier A, Adeli K, Giacca A. Disordered fat storage and mobilization in the pathogenesis of insulin resistance and type 2 diabetes. Endocr Rev. 2002;23:201–29. https://doi.org/10.1210/edrv.23.2.0461.
Arner P, Bernard S, Salehpour M, Possnert G, Liebl J, Steier P, et al. Dynamics of human adipose lipid turnover in health and metabolic disease. Nature. 2011;478:110–3. https://doi.org/10.1038/nature10426.
Xiao C, Hsieh J, Adeli K, Lewis GF. Gut-liver interaction in triglyceride-rich lipoprotein metabolism. Am J Physiol Endocrinol Metab. 2011;301:E429-446. https://doi.org/10.1152/ajpendo.00178.2011.
Jin J, Meng X, Wang D, Han B, Wu T, Xie J, et al. Association between ambient temperature and cardiovascular diseases related hospital admissions in Lanzhou China. Heliyon. 2023;9:e12997. https://doi.org/10.1016/j.heliyon.2023.e12997.
Hu X, Appleton AA, Ou Y, Zhang Y, Cai A, Zhou Y, et al. Abdominal volume index trajectories and risk of diabetes mellitus: results from the China Health and nutrition survey. J Diabetes Investig. 2022;13:868–77. https://doi.org/10.1111/jdi.13733.
Zhang B, Zhai FY, Du SF, Popkin BM. The China health and nutrition survey 1989–2011. Obes Rev. 2014;15:2–7. https://doi.org/10.1111/obr.12119.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007. https://doi.org/10.1136/bmj.39335.541782.AD.
Qian S, You S, Sun Y, Wu Q, Wang X, Tang W, et al. Remnant cholesterol and common carotid artery intima-media thickness in patients with ischemic stroke. Circulation Cardiovasc Imaging. 2021;14:010953. https://doi.org/10.1161/CIRCIMAGING.120.010953.
Alberti KGMM, Zimmet P, Shaw J, IDF Epidemiology Task Force Consensus Group. The metabolic syndrome–a new worldwide definition. Lancet. 2005;366(1059):62. https://doi.org/10.1016/S0140-6736(05)67402-8.
Kassi E, Pervanidou P, Kaltsas G, Chrousos G. Metabolic syndrome: definitions and controversies. BMC Med. 2011;9:48. https://doi.org/10.1186/1741-7015-9-48.
Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S. Modification of the CKD epidemiology collaboration (CKD-EPI) equation for japanese: accuracy and use for population estimates. Am J Kidney Dis. 2010;56:32–8. https://doi.org/10.1053/j.ajkd.2010.02.344.
Global recommendations on physical activity for health n.d. https://www.who.int/publications-detail-redirect/9789241599979 (Accessed 24 Aug 2023).
Alfons A, Ates NY, Groenen PJF. A robust bootstrap test for mediation analysis. ERIM Rep Series Res Manage. 2018;25(3):591.
Neeland IJ, Turer AT, Ayers CR, Powell-Wiley TM, Vega GL, Farzaneh-Far R, et al. Dysfunctional adiposity and the risk of prediabetes and type 2 diabetes in obese adults. JAMA. 2012;308:1150–9. https://doi.org/10.1001/2012.jama.11132.
Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen M-R, European Association for Cardiovascular Prevention & Rehabilitation, et al. ESC/EAS guidelines for the management of dyslipidaemias: the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European atherosclerosis society (EAS). Eur Heart J. 2011;32(1769):818. https://doi.org/10.1093/eurheartj/ehr158.
Berglund L, Brunzell JD, Goldberg AC, Goldberg IJ, Sacks F, Murad MH, et al. Evaluation and treatment of hypertriglyceridemia: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2012;97:2969–89. https://doi.org/10.1210/jc.2011-3213.
Varbo A, Benn M, Tybjærg-Hansen A, Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Coll Cardiol. 2013;61:427–36. https://doi.org/10.1016/j.jacc.2012.08.1026.
Nordestgaard BG, Langsted A, Freiberg JJ. Nonfasting hyperlipidemia and cardiovascular disease. Curr Drug Targets. 2009;10:328–35. https://doi.org/10.2174/138945009787846434.
Hadi Alijanvand M, Aminorroaya A, Kazemi I, Amini M, Aminorroaya Yamini S, Mansourian M. Prevalence and predictors of prediabetes and its coexistence with high blood pressure in first-degree relatives of patients with type 2 diabetes: a 9-year cohort study. J Res Med Sci. 2020;25:31. https://doi.org/10.4103/jrms.JRMS_472_18.
Xie G, Zhong Y, Yang S, Zou Y. Remnant cholesterol is an independent predictor of new-onset diabetes: a single-center cohort study. Diabetes Metab Syndr Obes. 2021;14:4735–45. https://doi.org/10.2147/DMSO.S341285.
Hu X, Liu Q, Guo X, Wang W, Yu B, Liang B, et al. The role of remnant cholesterol beyond low-density lipoprotein cholesterol in diabetes mellitus. Cardiovasc Diabetol. 2022;21:117. https://doi.org/10.1186/s12933-022-01554-0.
Palmu J, Tikkanen E, Havulinna AS, Vartiainen E, Lundqvist A, Ruuskanen MO, et al. Comprehensive biomarker profiling of hypertension in 36 985 Finnish individuals. J Hypertens. 2022;40:579–87. https://doi.org/10.1097/HJH.0000000000003051.
Chen M-M, Huang X, Xu C, Song X-H, Liu Y-M, Yao D, et al. High remnant cholesterol level potentiates the development of hypertension. Front Endocrinol. 2022;13:830347. https://doi.org/10.3389/fendo.2022.830347.
Huh JH, Roh E, Lee SJ, Ihm S-H, Han K-D, Kang JG. Remnant cholesterol is an independent predictor of type 2 diabetes: a nationwide population-based cohort study. Diabetes Care. 2023;46:305–12. https://doi.org/10.2337/dc22-1550.
Wadström BN, Pedersen KM, Wulff AB, Nordestgaard BG. Elevated remnant cholesterol, plasma triglycerides, and cardiovascular and non-cardiovascular mortality. Eur Heart J. 2023;44:1432–45. https://doi.org/10.1093/eurheartj/ehac822.
Lee SJ, Kim S-E, Go T-H, Kang DR, Jeon H-S, Kim Y-I, et al. Remnant cholesterol, low-density lipoprotein cholesterol, and incident cardiovascular disease among Koreans: a national population-based study. Eur J Prev Cardiol. 2023;30:1142–50. https://doi.org/10.1093/eurjpc/zwad036.
Salinas CAA, Chapman MJ. Remnant lipoproteins: are they equal to or more atherogenic than LDL? Curr Opin Lipidol. 2020;31:132–9. https://doi.org/10.1097/MOL.0000000000000682.
Langsted A, Madsen CM, Nordestgaard BG. Contribution of remnant cholesterol to cardiovascular risk. J Intern Med. 2020;288:116–27. https://doi.org/10.1111/joim.13059.
Whitman SC, Miller DB, Wolfe BM, Hegele RA, Huff MW. Uptake of type III hypertriglyceridemic VLDL by macrophages is enhanced by oxidation, especially after remnant formation. Arterioscler Thromb Vasc Biol. 1997;17:1707–15. https://doi.org/10.1161/01.atv.17.9.1707.
Rutledge JC, Mullick AE, Gardner G, Goldberg IJ. Direct visualization of lipid deposition and reverse lipid transport in a perfused artery. Circ Res. 2000;86:768–73. https://doi.org/10.1161/01.RES.86.7.768.
Acknowledgements
We thank the investigators who worked hard for the CHNS, and the CHNS participants and their families for the data provided.
Funding
Our research was supported by the National Natural Science Foundation of China (82074295, 82373529, 81903287), the Science and Technology Program of Tibet Grant (No. XZ202201ZY0051G).
Author information
Authors and Affiliations
Contributions
JGJ, XMH and Melissa Francois contributed to the manuscript preparation and wrote the main manuscript text; XMH contributed to the data analysis and prepared tables; WMW and BYY prepared figures; PZ provided critical revisions of the manuscript; YLZ and HJD contributed to the research ideas and approved the final version of the manuscript for submission; All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Study protocols and ethics approval were derived from the Institutional Review Committees of the University of North Carolina at Chapel Hill, USA, and the National Institute for Nutrition and Health (NINH, former National Institute of Nutrition and Food Safety) at the Chinese Center for Disease Control and Prevention (CCDC) at Beijing, China. Each participant signed an informed consent form.
Consent for publication
All the authors gave their consent to publication.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jin, J., Hu, X., Francois, M. et al. Association between remnant cholesterol, metabolic syndrome, and cardiovascular disease: post hoc analysis of a prospective national cohort study. Eur J Med Res 28, 420 (2023). https://doi.org/10.1186/s40001-023-01369-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-01369-z