Abstract
Background
Oxidative stress plays an important role in the occurrence and development of malignancy. However, the relationship between oxidative stress and upper urinary tract urothelial carcinoma (UTUC) prognosis remains elusive. This study aimed to evaluate the prognostic value of systematic oxidative stress indices as a predictor of patient outcomes in UTUC after radical nephroureterectomy.
Methods
Clinical data for 483 patients with UTUC who underwent radical nephroureterectomy were analyzed. Patients were categorized according to an optimal value of systematic oxidative stress indices (SOSIs), including fibrinogen (Fib), gamma-glutamyl transpeptidase (γ-GGT), creatinine (CRE), lactate dehydrogenase (LDH) and albumin (ALB). Kaplan–Meier analyses were used to investigate associations of SOSIs with overall survival (OS) and progression-free survival (PFS). Moreover, associations between SOSIs and OS and PFS were assessed with univariate and multivariate analyses.
Results
High values of Fib, γ-GGT, CRE, and LDH, and low values of ALB were associated with reduced OS. SOSIs status correlated with age, tumor site, surgical approach, hydronephrosis, tumor size, T stage, and lymph node status. The Kaplan–Meier survival analysis showed a significant discriminatory ability for death and progression risks in the two groups based on SOSIs. Multivariate Cox proportional hazards models showed that SOSIs were an independent prognostic indicator for OS (p = 0.007) and PFS (p = 0.021). SOSIs and clinical variables were selected to establish a nomogram for OS. The 1-, 3-, and 5-year AUC values were 0.77, 0.78, and 0.81, respectively. Calibration curves of the nomogram showed high consistencies between the predicted and observed survival probability. Decision curve analysis curves showed that the nomogram could well predict the 1‐year, 3-year, and 5‐year OS.
Conclusions
SOSIs are an independent unfavorable predictor of OS and PFS in patients diagnosed with UTUC undergoing RNU. Therefore, incorporating SOSIs into currently available clinical parameters may improve clinical decision-making.
Similar content being viewed by others
Introduction
Upper urinary tract urothelial carcinomas (UTUCs), which are derived from the urothelium along the urinary tract, are located in the upper (pyelocaliceal cavities and ureter) urinary tract. UTUCs account for only 5–10% of all urothelial carcinomas (UCs) [1]. Radical nephroureterectomy (RNU) with bladder cuff excision remains the gold standard treatment for localized upper urinary tract urothelial carcinoma (UTUC). Because 60% of UTUCs are invasive at diagnosis, they usually have very poor prognosis [1, 2]. The 5-year specific survival is < 50% for pT2/pT3 and < 10% for pT4 [3,4,5]. European Association of Urology guidelines indicate that postoperative prognostic factors, such as lymph node involvement, tumor stage, and grade, are related to oncological outcomes. However, postoperative information might not contribute to making pretreatment assessments. Thus, identification of preoperatively available prognostic factors may enable physicians to determine preoperative treatment strategies concerning clinically valuable decisions in UTUC.
Oxidative stress is defined as a relative excess of reactive oxygen species (ROS) compared with antioxidants. ROS have been linked to a whole range of diseases, including cardiovascular disease, neurodegenerative disorders, autoimmune disease, and many cancers. Previous studies have revealed that intricate crosstalk between myeloid cell-derived ROS, oxidative DNA damage, and tumor necrosis factor α-mediated signaling can initiate cancer and contribute to tumor promotion and progression [6]. In addition, ROS can damage DNA, leading to genetic lesions that initiate tumorigenicity and subsequent tumor progression [7]. TBARS (thiobarbituric acid reactive substances) represents a good indicator of oxidative stress. A retrospective analysis revealed that metastatic urothelial carcinoma patients with increased TBARS had worse prognosis [8]. In addition, Chang et al. indicated that underexpression of glutathione peroxidase 2 (GPX2), a gene associated with oxidative stress, is a significant independent prognostic factor of urothelial carcinoma [9]. These findings provide evidence that oxidative stress is closely related to urothelial carcinoma.
In recent years, considerable evidence has demonstrated that several plasma biomarkers are associated with increased oxidative stress [10,11,12]. Higher levels of serum albumin (ALB) and lactate dehydrogenase (LDH) were observed in patients with trauma compared with the Antiox group. Decreasing the OS level with antioxidant substances correlated significantly with better prognosis and outcome [12]. Creatinine (CRE) and blood urea nitrogen (BUN) were significantly increased in a sleep-deprived mouse model associated with increased oxidative stress [11]. The serum-level of gamma-glutamyl transferase (γ-GGT) was found to decrease after antioxidant therapy [13]. Some previous results demonstrate that fibrinogen during acute inflammatory states may be affected by oxidative stress and can be used as a marker to reflect the status of systematic oxidative stress [14,15,16]. Systematic oxidative stress has been proven to be useful as a predictor of prognosis in many cancers, including breast cancer, colorectal cancer, and T lymphoblastic lymphoma/leukemia [17,18,19]. However, the feasibility of oxidative stress for UTUC has not been evaluated to date.
Therefore, this study aimed to explore correlations of systematic oxidative stress indices (SOSIs) with clinicopathologic parameters and to validate the prognostic value of SOSIs as a predictor of patient outcome in UTUC after radical nephroureterectomy.
Materials and methods
Study population
This retrospective analysis evaluated data from patients without evidence of distant metastases who underwent RNU between March 1996 and June 2021 at Beijing Hospital, National Center of Gerontology, Institute of the Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing. Patients who had not undergone RNU, had evidence of metastatic disease at the time of surgery, or had incomplete preoperative medical information on hematologic indicators; patients who were lost to follow-up; patients with autoimmune diseases; and patients who had received preoperative adjuvant chemotherapy, radiotherapy, or any other antitumor therapy were excluded from the study. Finally, we assessed data for a final total of 483 patients who underwent open or laparoscopic RNU.
Data collection and evaluation
Data regarding sex, age, symptoms, tumor location, tumor side, tumor size, presence of preoperative hydronephrosis, multifocality, pathologic T and N stage, appearance of lymphovascular invasion, chemotherapy, tumor grade, positive surgical margin, surgical approach, and the presence of concomitant carcinoma in situ (CIS) were obtained from the Beijing Hospital Information System. Biochemical information, including fibrinogen (Fib), gamma-glutamyl transpeptidase (γ-GGT), creatinine (CRE), lactate dehydrogenase (LDH), albumin (ALB), blood urea nitrogen (BUN), and alkaline phosphatase (ALP), was obtained within 7 days before RNU. Progression-free survival (PFS), and overall survival (OS) were obtained from medical records. Surgical specimens were processed by an experienced pathologist, who confirmed the T stage (based on the American Joint Committee on Cancer TNM Classification, 7th edition), tumor grade (based on 1998 WHO classification), lympho-vascular invasion (LVI), and presence of variant histology.
Follow-up regimen
Postoperative follow-up included routine urine tests, urine pathology chest radiography, computed tomography, and cystoscopy. Patients were generally assessed postoperatively every 3–4 months in the first year after RNU, every 6 months from the second year to the fifth year, and annually thereafter. PFS (measured from RNU until the date of last follow-up or date of disease progression (including local recurrence or distant metastasis or death) and OS (measured from RNU until the date of last follow-up or date of death from any cause) were selected as primary endpoints.
Statistical analysis
Comparisons between the clinicopathological characteristics of the patients were performed using the chi-square test and Mann–Whitney U test, as appropriate. Seven plasma biomarkers associated with increased oxidative stress, including Fib, CRE, GGT, ALB, LDH, ALP, and BUN, were identified for calculating SOSIs, which were determined by the lowest Akaike information criterion (AIC) value. The value was defined as 1 if the plasma biomarker value was above the cutoff level; the value was defined as 0 if the plasma biomarkers value was below the cutoff level. Survival curves were generated using the Kaplan–Meier method with the log-rank test. Univariate and multivariate Cox proportional hazard models were conducted to evaluate the impact of variables on OS and PFS after RNU. Time-dependent receiver operating characteristic (ROC) analysis and decision curve analysis (DCA) were used to assess the prognostic capacity of the nomogram. A P value lower than 0.05 was considered statistically significant. Data analysis was completed with R software, version 4.2.1.
Results
Basic information of selected patients
The clinical and pathologic characteristics of the patients are shown in Table 1. In this cohort, males accounted for 51.1% (247 patients) and females for 48.9% (236 patients), with a median age of 70 years (interquartile range: 62–76). The cutoff values of Fib, CRE, GGT, ALB, BUN, ALP, and LDH derived from the ROC curves were 3.978 g/L, 83.5 μmol/L, 43.5 U/L, 39.5 g/L,9.07 mg/dL, 83.5 UL/L, and 170.5 U/L, respectively. During the median follow-up of 36.8 (interquartile range [IQR]: 22.0–68.5) months, a total of 182 (37.7%) patients died, and 224 (46.4%) had progressive disease.
Calculation of systematic oxidative stress indices (SOSIs) and baseline characteristics of UTUC patients in different SOSI groups
First, we divided the seven plasma biomarkers into 2 groups using the cutoff value. Values of “0” and “1” were used for scoring according to the algorithm mentioned above. Univariate and multivariate Cox regression analyses were used to explore whether the above seven plasma biomarkers are independent prognostic factors for UTUC. According to univariate Cox regression analysis, we found that Fib, GGT, CRE, BUN, LDH, and ALB correlated significantly with overall survival (OS) (all p < 0.05) (Fig. 1a). Multivariate Cox regression analysis indicated that Fib, GGT, CRE, LDH, and ALB were associated with OS (Fig. 1b). Then, the SOSIs prognostic model was generated based on the lowest AIC value: SOSIs = Fib*0.3141 + GGT*0.6059 + CRE*0.3582 + LDH*0.7149–ALB*0.3600. The cutoff value of SOSIs based on the median value was set as 0.3582 and used to divide the patients into high-risk (272 with SOSIs of 0.3582 or above) and low-risk groups (211 with a SOSIs level less 0.3582). The clinical characteristics of all the patients grouped by SOSIs are presented in Table 2. Patients in the high-risk group had higher incidences of ≥ pT3 stage and pN + . In the high-risk patient group, tumor size, hydronephrosis, and positive urine pathology were significantly higher than those in the low-risk patient group. There was an obvious difference between the two groups in terms of age, tumor site, and surgical approach. However, no significant difference was found for sex, BMI, tumor side, previous ureteroscopic surgical margin status, multifocality, presence of lymphovascular invasion, chemotherapy, lymph node stage, presence of CIS in surgical specimens, or tumor grade.
Relationship between SOSIs and clinical features
The Kaplan–Meier curve showed that the patients in the high-risk group had worse overall survival (OS) (Fig. 2a) and progression-free survival (PFS) (Fig. 2b) than those in the low-risk group. We also found that OS was worse in the high-risk group than in the low-risk group in subgroup analysis performed by age (Fig. 2c) and T stage (Fig. 2d). In the size ≤ 5 and pN0&Nx groups, the high-risk group had worse prognosis, but there was no significant difference in the size > 5 and pN + groups between the two groups (Fig. 2e, f). Subgroup analyses suggested a significant difference in PFS between the two risk groups for the two T-stage groups (Fig. 2g). In size ≤ 5 (Fig. 2h), age ≥ 65 (Fig. 2i) and pN0&Nx (Fig. 2j) subgroups, survival analysis showed that patients with low-risk had significantly favorable PFS compared with patients with high-risk.
Kaplan–Meier curves for OS and PFS based on SOSIs. OS (a) and PFS (b) in the cohort; Subgroup analysis based on age (c), T stage (d), size (e) and pN (f), Kaplan–Meier curves for OS stratified according to SOSIs for UTUC patients receiving RNU; Subgroup analysis based on T stage (g), size (h), age (i) and pN (j), Kaplan–Meier curves for PFS stratified according to SOSIs for UTUC patients receiving RNU
Evaluation of SOSIs as an independent prognostic factor in patients with UTUC
Univariate and multivariate analyses were performed to determine predictors of OS (Table 3). In univariate analyses,we found that age (HR = 1.681, p = 0.003), tumor site at the ureter (HR = 1.413, p = 0.029), use of ureteroscopy (HR = 1.620, p = 0.014), hydronephrosis (HR = 1.904, p = 0.001), size ≥ 5 (HR = 1.744, p = 0.005), LVI (HR = 3.766, p < 0.001), T stage (T2, HR = 2.507, p < 0.001; T3, HR = 3.404, p < 0.001; T4, HR = 12.446, p < 0.001), margin (HR = 5.062, p < 0.001), N stage (HR = 5.344, p < 0.001), grade (HR = 2.013, p = 0.001), chemotherapy (HR = 2.241, p < 0.001), and SOSIs (HR = 2.217, p < 0.001) were significantly associated with OS. Those significant and potential risk factors were evaluated in multivariate analyses, in which OS (all p < 0.05)was independently predicted by age, LVI, T stage, N stage, margin, and SOSIs.
Interestingly, sex (HR = 1.335, p = 0.030), age (HR = 1.435, p = 0.018), tumor site at the ureter (HR = 1.617, p = 0.001), use of ureteroscopy (HR = 1.489, p = 0.025), hydronephrosis (HR = 1.544, p = 0.010), LVI (HR = 2.467, p < 0.001), T stage (T2, HR = 1.832, p = 0.002; T3, HR = 2.098, p < 0.001; T4, HR = 5.538, p < 0.001), margin (HR = 2.308, p = 0.021), N stage (HR = 4.302, p < 0.001), grade (HR = 1.809, p = 0.001), and SOSI (HR = 1.721, p < 0.001) were all highly significantly different in univariate PFS analysis. Next, age, tumor site at the ureter, LVI, T stage, N stage, and SOSIs were all significantly identified in PFS multivariate analysis (Table 4).
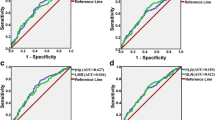
Development and validation of the nomogram prediction model
The independent predictors were used to construct a nomogram (Fig. 3). The areas under the curve (AUCs) of the nomogram for predicting 1-year, 3-year, and 5-year survival rates were 0.77, 0.78, and 0.81, respectively (Fig. 4a). The time‐dependent AUC was > 0.7 for prediction of OS within 10 years, indicating favorable discrimination by the nomogram (Fig. 4b). As shown in Fig. 4c, calibration curves indicated good agreement between the predicted and observed probabilities. Furthermore, in decision curve analysis, the nomogram consistently achieved a greater net benefit than traditional prognostic indicators (Fig. 4d). Collectively, these results indicate that the nomogram has good concordance and accuracy.
Discussion
In the present study, we investigated systematic oxidative stress indices levels in 483 patients undergoing RNU for localized UTUC. Elevated preoperative SOSIs levels were associated with higher incidences of ≥ pT3 stage and pN + . Kaplan–Meier analysis showed that patients with high SOSIs levels were predicted to have poor overall survival and progression-free survival. Furthermore, results from multivariate analysis confirmed SOSIs levels to be an independent predictor of OS and PFS. Using SOSIs and clinical–pathological features, we developed a nomogram to predict survival outcomes for patients with UTUC. To the best of our knowledge, this is the first report to describe an association of combined SOSIs with prognosis in upper urinary tract urothelial carcinoma after radical nephroureterectomy. The results suggest that SOSIs levels are a strong biomarker for predicting oncological outcomes preoperatively in localized UTUC.
The concept of oxidative stress was first proposed in 1985 for redox biology and medicine research, approximately 40 years ago [20]. Since then, redox biology as a field of study has exploded in a wide range of disciplines. Imbalance between oxidants (so-called reactive oxygen species, ROS) and antioxidants is the core of oxidative stress [21]. This imbalance leads to damage to important biomolecules and cells, with a potential impact on the whole organism [22]. In recent years, considerable evidence has demonstrated that ROS may increase the risk of cancer when the balance between the relative abundance of ROS and antioxidants is broken. Sod1-deficient mice develop liver cancer, as marked by extensive oxidative and DNA damage. Mice heterozygous for a null allele of Sod2 also exhibit increased levels of oxidative damage to DNA and form tumors, particularly lymphoma and pituitary adenoma [23,24,25]. Many studies have shown the significant role of oxidative stress in the development and progression of malignancies, such as breast cancer, hepatocellular carcinoma, and prostate cancer, through excessive production of reactive oxygen species [26,27,28]. As one of the key antioxidant enzymes, GPX2 plays an important role in catalyzing reduction of hydrogen peroxide or organic hydroperoxides [29]. Chang et al. found that underexpression of GPX2 in UTUC correlated strongly with more advanced and more aggressive disease. In addition, GPX2 underexpression and downregulation are predictive of poor prognosis in patients with UTUC [9].
Increasing evidence has consistently shown the role of SOSIs in predicting patient outcomes in multiple malignant tumors [17,18,19]. Our findings are consistent with those of previous studies, as SOSIs are considered an independent predictor. Fib is an adhesive plasma protein that plays a central role in hemostasis. Previous work has revealed that Fib is targeted for oxidative modifications in vivo, and that it can reflect the status of systematic oxidative stress [15, 30]. Fib and its related fragments are involved in tumor angiogenesis and metastasis [31]. Evidence has shown the association of elevated Fib levels with worse survival outcomes in gastrointestinal stromal tumors, pancreatic ductal adenocarcinoma, the coronavirus disease-19 (COVID-19), and colon cancer [32,33,34,35]. Similarly, in patients with UTUC, elevated plasma Fib levels are an independent predictor of poor survival [36]. In the present study, we found that Fib was a significant independent prognostic factor of UTUC following curative resection. Creatinine, the end product of creatine and creatine phosphate metabolism, is excreted mainly by the kidney [37,38,39]. Accumulating evidence indicates that oxidative stress plays a central role in the pathogenesis of chronic kidney disease [40]. In the case of renal dysfunction, the daily creatinine produced is not completely excreted, resulting in increased blood creatinine levels. Thus, values of CRE can reflect the oxidative stress injury of an organism. In this research, serum creatinine level was identified as an independent risk factor for mortality.
γ-GGT is a ubiquitous cell surface enzyme that plays a crucial role in antioxidant defense systems [41]. Based on epidemiological and experimental studies, elevated serum γ-GGT might be an early and sensitive marker for oxidative stress [42, 43]. γ-GGT levels have been shown to have independent prognostic value in various types of cancer, including non-small lung cancer, colorectal cancer, and hepatocellular carcinoma [44,45,46]. In line with previous studies, we found that a high serum γ-GGT level was an independent prognostic factor for OS in UTUC patients. LDH is a tetrameric enzyme comprising two major subunits, A and/or B. Lactate dehydrogenase A (LDHA) is a key enzyme in aerobic glycolysis that preferentially converts pyruvate to lactic acid [47]. Tumor cells overexpress LDHA to obtain energy through aerobic glycolysis [48]. Le et al. reported that a reduction in LDHA level or activity triggers oxidative stress and cell death [49]. In the current study, we showed that LDH is an effective indicator for predicting prognosis in UTUC patients. ALB is the most abundant plasma protein and has important antioxidant activities [50]. Our results were consistent with a previous report that ALB is an independent survival risk factor [51]. In summary SOSIs which consists of Fib, CRE, γ-GGT, ALB, and LDH, is a newly established scoring tool for representing the status of systematic oxidative stress. Our results demonstrate that high SOSIs correlates significantly with decreased OS and PFS in patients with UTUC.
Currently, the standard of care for patients with nonmetastatic MIBC is platinum-based neoadjuvant chemotherapy in combination with radical cystectomy [52]. However, there is currently no high-level evidence to support use of neoadjuvant chemotherapy for high-risk UTUC, given the significant bias and heterogeneity. A recent randomized controlled trial assessing the benefit of adjuvant gemcitabine–platinum combination chemotherapy initiated within 90 days after RNU reported significant improvement in disease-free survival for patients. In this study, we found no significant difference between oxidative stress and use of chemotherapy; chemotherapy did not improve survival. The possible explanation is that the number of people who received chemotherapy was small, and the treatment plan was not uniform due to the long-time span of this study. In addition, immune checkpoint inhibitors have been used in treatment of urothelial carcinoma to improve overall survival and reduce morbidity and mortality [53]. We hope to collect immunotherapy data for analysis in a future study.
There are some limitations to our study. First, as with all retrospective studies, the limitations of our study are inherent to the design. There was also a limited number of patients; thus a high risk of selection bias may exist in the findings. Randomized controlled trials with a larger population are warranted to validate the prognostic ability of SOSIs in patients with UTUC. Moreover, it was difficult to guarantee the consistency of the pathologic outcomes, because the patients in our study were treated by multiple surgeons. In this study, no information on the inflammatory status of patients was analyzed, which may affect the SOSIs level. In addition, all patients enrolled in this study were Chinese, and the influence of ethnic diversity cannot be ignored. The findings must be further explored in future studies. Finally, there is currently a lack of data on immunotherapy, and we could not compare levels of oxidative stress in patients with immune checkpoint inhibitors. Of course, we intend to continue this line of inquiry in a follow-up study.
Conclusion
To our knowledge, this is the first study to explore the prognostic value of SOSIs for survival in patients with UTUC who underwent RNU. We confirmed that SOSIs can sever as an independent predictor of OS and PFS in patients with UTUC. The nomogram also showed good predictive performance in UTUC patients. We thus believe that use of the SOSIs may facilitate preintervention risk stratification in UTUC.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Change history
21 December 2023
A Correction to this paper has been published: https://doi.org/10.1186/s40001-023-01582-w
References
Rouprêt M, Babjuk M, Burger M, Capoun O, Cohen D, Compérat EM, Cowan NC, Dominguez-Escrig JL, Gontero P, Hugh Mostafid A, et al. European association of urology guidelines on upper urinary tract urothelial carcinoma: 2020 update. Eur Urol. 2021;79(1):62–79.
Vitaly M, Shahrokh FS, Surena FM, Kamat MA, Zigeuner R, Kikuchi E, Lotan Y, Weizer A, Raman JD, Wood CG. Outcomes of radical nephroureterectomy: a series from the upper tract urothelial carcinoma collaboration. Cancer. 2009;115(6):1224–33.
Lughezzani G, Burger M, Margulis V, Matin SF, Novara G, Roupret M, Shariat SF, Wood CG, Zigeuner R. Prognostic factors in upper urinary tract urothelial carcinomas: a comprehensive review of the current literature. Eur Urol. 2012;62(1):100–14.
Abouassaly R, Alibhai SMH, Shah N, Timilshina N, Fleshner N, Finelli A. Troubling outcomes from population-level analysis of surgery for upper tract urothelial carcinoma. Urology. 2010;76(4):895–901.
Jeldres C, Sun M, Isbarn H, Lughezzani G, Budäus L, Alasker A, Shariat SF, Lattouf J-B, Widmer H, Pharand D, et al. A population-based assessment of perioperative mortality after nephroureterectomy for upper-tract urothelial carcinoma. Urology. 2010;75(2):315–20.
Canli Ö, Nicolas AM, Gupta J, Finkelmeier F, Goncharova O, Pesic M, Neumann T, Horst D, Löwer M, Sahin U, et al. Myeloid cell-derived reactive oxygen species induce epithelial mutagenesis. Cancer Cell. 2017. https://doi.org/10.1016/j.ccell.2017.11.004.
Srinivas US, Tan BWQ, Vellayappan BA, Jeyasekharan AD. ROS and the DNA damage response in cancer. Redox Biol. 2019;25: 101084.
Slopovsky J, Kucharska J, Obertova J, Mego M, Kalavska K, Cingelova S, Svetlovska D, Gvozdjakova A, Furka S, Palacka P. Plasma thiobarbituric acid reactive substances predicts survival in chemotherapy naïve patients with metastatic urothelial carcinoma. Transl Oncol. 2021;14(1): 100890.
Chang IW, Lin VC-H, Hung C-H, Wang H-P, Lin Y-Y, Wu W-J, Huang C-N, Li C-C, Li W-M, Wu J-Y, et al. GPX2 underexpression indicates poor prognosis in patients with urothelial carcinomas of the upper urinary tract and urinary bladder. World J Urol. 2015;33(11):1777–89.
Teixeira-Gomes A, Laffon B, Valdiglesias V, Gostner JM, Felder T, Costa C, Madureira J, Fuchs D, Teixeira JP, Costa S. Exploring early detection of frailty syndrome in older adults: evaluation of oxi-immune markers, clinical parameters and modifiable risk factors. Antioxidants. 2021. https://doi.org/10.3390/antiox10121975.
Periasamy S, Hsu D-Z, Fu Y-H, Liu M-Y. Sleep deprivation-induced multi-organ injury: role of oxidative stress and inflammation. EXCLI J. 2015;14:672–83.
Sandesc M, Rogobete AF, Bedreag OH, Dinu A, Papurica M, Cradigati CA, Sarandan M, Popovici SE, Bratu LM, Bratu T, et al. Analysis of oxidative stress-related markers in critically ill polytrauma patients: an observational prospective single-center study. Bosn J Basic Med Sci. 2018;18(2):191–7.
Ahmed S, Zahoor A, Ibrahim M, Younus M, Nawaz S, Naseer R, Akram Q, Deng C-L, Ojha SC. Enhanced efficacy of direct-acting antivirals in hepatitis C patients by coadministration of black cumin and ascorbate as antioxidant adjuvants. Oxid Med Cell Longev. 2020;2020:7087921.
Becatti M, Marcucci R, Bruschi G, Taddei N, Bani D, Gori AM, Giusti B, Gensini GF, Abbate R, Fiorillo C. Oxidative modification of fibrinogen is associated with altered function and structure in the subacute phase of myocardial infarction. Arterioscler Thromb Vasc Biol. 2014;34(7):1355–61.
McLarnon JG. A leaky blood-brain barrier to fibrinogen contributes to oxidative Damage in Alzheimer’s Disease. Antioxidants. 2021. https://doi.org/10.3390/antiox11010102.
White NJ, Wang Y, Fu X, Cardenas JC, Martin EJ, Brophy DF, Wade CE, Wang X, St John AE, Lim EB, et al. Post-translational oxidative modification of fibrinogen is associated with coagulopathy after traumatic injury. Free Radic Biol Med. 2016;96:181–9.
Cao Y, Deng S, Yan L, Gu J, Mao F, Xue Y, Zheng C, Yang M, Liu H, Liu L, et al. An oxidative stress index-based score for prognostic prediction in colorectal cancer patients undergoing surgery. Oxid Med Cell Longev. 2021;2021:6693707.
Ping L, Gao Y, He Y, Wang X, Bai B, Huang C, Huang H. Systematic oxidative stress indexes associated with the prognosis in patients with t lymphoblastic lymphoma/leukemia. Oxid Med Cell Longev. 2022;2022:2679154.
Zhang K, Ping L, Du T, Wang Y, Sun Y, Liang G, Wang X, Xie X, Wei W, Xiao X, et al. A novel systematic oxidative stress score predicts the prognosis of patients with operable breast cancer. Oxid Med Cell Longev. 2021;2021:9441896.
Sies H, editor. Oxidative Stress. London: Academic Press; 1985. p. 1–507.
Sies H. Oxidative stress: a concept in redox biology and medicine. Redox Biol. 2015;4:180–3.
Ďuračková Z. Some current insights into oxidative stress. Physiol Res. 2010;59(4):459–69.
Gill JG, Piskounova E, Morrison SJ. Cancer, oxidative stress, and metastasis. Cold Spring Harb Symp Quant Biol. 2016;81:163–75.
Elchuri S, Oberley TD, Qi W, Eisenstein RS, Jackson Roberts L, Van Remmen H, Epstein CJ, Huang T-T. CuZnSOD deficiency leads to persistent and widespread oxidative damage and hepatocarcinogenesis later in life. Oncogene. 2005;24(3):367–80.
Van Remmen H, Ikeno Y, Hamilton M, Pahlavani M, Wolf N, Thorpe SR, Alderson NL, Baynes JW, Epstein CJ, Huang T-T, et al. Life-long reduction in MnSOD activity results in increased DNA damage and higher incidence of cancer but does not accelerate aging. Physiol Genomics. 2003;16(1):29–37.
McLoughlin MR, Orlicky DJ, Prigge JR, Krishna P, Talago EA, Cavigli IR, Eriksson S, Miller CG, Kundert JA, Sayin VI, et al. TrxR1, Gsr, and oxidative stress determine hepatocellular carcinoma malignancy. Proc Natl Acad Sci U S A. 2019;116(23):11408–17.
Papachristodoulou A, Rodriguez-Calero A, Panja S, Margolskee E, Virk RK, Milner TA, Martina LP, Kim JY, Di Bernardo M, Williams AB, et al. NKX3.1 localization to mitochondria suppresses prostate cancer initiation. Cancer Disc. 2021;11(9):2316–33.
Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB. Oxidative stress, inflammation, and cancer: how are they linked? Free Radic Biol Med. 2010;49(11):1603–16.
Margis R, Dunand C, Teixeira FK, Margis-Pinheiro M. Glutathione peroxidase family - an evolutionary overview. FEBS J. 2008;275(15):3959–70.
Heffron SP, Parastatidis I, Cuchel M, Wolfe ML, Tadesse MG, Mohler ER, Ischiropoulos H, Rader DJ, Reilly MP. Inflammation induces fibrinogen nitration in experimental human endotoxemia. Free Radic Biol Med. 2009;47(8):1140–6.
Wang M, Zhang G, Zhang Y, Cui X, Wang S, Gao S, Wang Y, Liu Y, Bae JH, Yang W-H, et al. Fibrinogen alpha chain knockout promotes tumor growth and metastasis through integrin-AKT signaling pathway in lung cancer. Mol Cancer Res. 2020;18(7):943–54.
Guo Y, Liu J, Zhang W, Xiao S, Zheng G, Liu S, Guo M, Zhang H, Feng F. Prognostic value of fibrinogen and lymphocyte count in intermediate and high risk gastrointestinal stromal tumors. Cancer Manag Res. 2020;12:8149–57.
Sui J, Noubouossie DF, Gandotra S, Cao L. Elevated plasma fibrinogen is associated with excessive inflammation and disease Severity in COVID-19 patients. Front Cell Infect Microbiol. 2021;11: 734005.
Papila Kundaktepe B, Papila C. The clinical significance of preoperative plasma fibrinogen levels and platelet counts in resectable colon cancer. World J Surg Oncol. 2021;19(1):69.
Chung KH, Lee J-C, Lee J, Cho I-K, Kim J, Jang W, Yoo BC, Hwang J-H. Serum fibrinogen as a diagnostic and prognostic biomarker for pancreatic ductal adenocarcinoma. Pancreatology. 2020;20(7):1465–71.
Xu H, Ai J-Z, Tan P, Lin T-H, Jin X, Gong L-N, Lei H-R, Yang L, Wei Q. Pretreatment elevated fibrinogen level predicts worse oncologic outcomes in upper tract urothelial carcinoma. Asian J Androl. 2020;22(2):177–83.
Brosnan JT, Brosnan ME. Creatine metabolism and the urea cycle. Mol Genet Metab. 2010;100(Suppl 1):S49–52.
Wyss M, Kaddurah-Daouk R. Creatine and creatinine metabolism. Physiol Rev. 2000;80(3):1107–213.
Kashani K, Rosner MH, Ostermann M. Creatinine: from physiology to clinical application. Eur J Intern Med. 2020. https://doi.org/10.1016/j.ejim.2019.10.025.
Irazabal MV, Torres VE. Reactive oxygen species and redox signaling in chronic kidney disease. Cells. 2020. https://doi.org/10.3390/cells9061342.
Whitfield JB. Gamma glutamyl transferase. Crit Rev Clin Lab Sci. 2001;38(4):263–355.
Lee D-H, Blomhoff R, Jacobs DR. Is serum gamma glutamyltransferase a marker of oxidative stress? Free Radic Res. 2004;38(6):535–9.
Zhang H, Forman HJ. Redox regulation of gamma-glutamyl transpeptidase. Am J Respir Cell Mol Biol. 2009;41(5):509–15.
Yang D, Wu H, Nong W, Zheng M, Li A, Wang Y, Li M, Chen Q, Yuan S, Yu J, et al. A new model based on gamma-glutamyl transpeptidase to platelet ratio (GPR) predicts prognostic outcome after curative resection of solitary hepatocellular carcinoma. Clin Res Hepatol Gastroenterol. 2021;45(5): 101509.
Bozkaya Y, Yazıcı O. Prognostic significance of gamma-glutamyl transferase in patients with metastatic non-small cell lung cancer. Expert Rev Mol Diagn. 2019;19(3):267–72.
Xiao B, Peng J, Tang J, Deng Y, Zhao Y, Wu X, Ding P, Lin J, Pan Z. Serum Gamma Glutamyl transferase is a predictor of recurrence after R0 hepatectomy for patients with colorectal cancer liver metastases. Therap Adv Med Oncol. 2020;12:1758835920947971.
Ždralević M, Brand A, Di Ianni L, Dettmer K, Reinders J, Singer K, Peter K, Schnell A, Bruss C, Decking S-M, et al. Double genetic disruption of lactate dehydrogenases A and B is required to ablate the “Warburg effect” restricting tumor growth to oxidative metabolism. J Biol Chem. 2018;293(41):15947–61.
Li X, Zhang C, Zhao T, Su Z, Li M, Hu J, Wen J, Shen J, Wang C, Pan J, et al. Lysine-222 succinylation reduces lysosomal degradation of lactate dehydrogenase a and is increased in gastric cancer. J Exp Clin Cancer Res. 2020;39(1):172.
Le A, Cooper CR, Gouw AM, Dinavahi R, Maitra A, Deck LM, Royer RE, Vander Jagt DL, Semenza GL, Dang CV. Inhibition of lactate dehydrogenase A induces oxidative stress and inhibits tumor progression. Proc Natl Acad Sci U S A. 2010;107(5):2037–42.
Roche M, Rondeau P, Singh NR, Tarnus E, Bourdon E. The antioxidant properties of serum albumin. FEBS Lett. 2008;582(13):1783–7.
Pradere B, D’Andrea D, Schuettfort VM, Foerster B, Quhal F, Mori K, Abufaraj M, Margulis V, Deuker M, Briganti A, et al. Pre-therapy serum albumin-to-globulin ratio in patients treated with neoadjuvant chemotherapy and radical nephroureterectomy for upper tract urothelial carcinoma. World J Urol. 2021;39(7):2567–77.
Iacovino ML, Miceli CC, De Felice M, Barone B, Pompella L, Chiancone F, Di Zazzo E, Tirino G, Della Corte CM, Imbimbo C, et al. Novel therapeutic opportunities in neoadjuvant setting in urothelial cancers: a new horizon opened by molecular classification and immune checkpoint inhibitors. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms23031133.
Barone B, Calogero A, Scafuri L, Ferro M, Lucarelli G, Di Zazzo E, Sicignano E, Falcone A, Romano L, De Luca L, et al. Immune checkpoint inhibitors as a neoadjuvant/adjuvant treatment of muscle-invasive bladder cancer: a systematic review. Cancers. 2022. https://doi.org/10.3390/cancers14102545.
Acknowledgements
Not applicable.
Funding
The study was funded by China's National Key R&D Program (Grant Numbers: 2018YFC2002202) and the Chinese Academy of Medical Sciences (Grant Numbers: BJ-2022-237).
Author information
Authors and Affiliations
Contributions
JL: project development, data collection, data analysis, manuscript writing. SL: project development, data collection, data analysis, manuscript writing. PW: project development, data collection, data analysis, manuscript writing. JW: data collection, data analysis. JW: project development, data analysis, manuscript editing. JW: project development, data analysis, manuscript editing. YZ: project development, data analysis, manuscript editing.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The current research was approved by the Research Ethics Committee of Beijing Hospital. The study was conducted in accordance with the declaration of Helsinki. Informed consent was obtained from all subjects/participants and/or legal guardian(s).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The affiliation 1 which was incorrectly published has been corrected as “Department of Urology, Beijing Hospital, National Center of Gerontology, Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, No. 1 DaHua Road, Dong Dan, Beijing 100730, People’s Republic of China".
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, J., Lai, S., Wu, P. et al. Systematic oxidative stress indices predicts prognosis in patients with urothelial carcinoma of the upper urinary tract after radical nephroureterectomy. Eur J Med Res 28, 469 (2023). https://doi.org/10.1186/s40001-023-01295-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-01295-0