Abstract
Objective
The study investigated the feasibility and potential outcome measures during acute hyperoxia in type 2 diabetes patients (DM2).
Methods
Eleven DM2 patients (7 men and 4 women) were included in the study. The patients cycled (30 min at 20 % Wmax) whilst breathing three different supplemental oxygen flows (SOF, 5, 10, 15 L min−1). During hyperoxic exercise, arterial blood gases and intra-arterial blood pressure measurements were obtained.
Results
Arterial pO2 levels increased significantly (ANOVA, p < 0.05) with SOF: 13.9 ± 1.2 (0 L min−1); 18.5 ± 1.5 (5 L min−1); 21.7 ± 1.7 (10 L min−1); 24.0 ± 2.3 (15 L min−1). Heart rate (HR) and pH increased significantly after terminating administration of hyperoxic air.
Conclusions
An SOF of 15 L min−1 appears to be more effective than 5 or 10 L min−1. Moreover, HR, blood pressure, blood lactate and pH are not recommended as primary outcome measures.
Similar content being viewed by others
Background
Breathing a hyperoxic gas mixture has been shown to acutely enhance power output (W) by 8–13 % [1–6], increase oxygen uptake (\(\dot{V}{\text{O}}_{ 2}\)) by 10–14 % [2, 3, 6–10], decrease blood lactate level [11] and lower perceived exertion [7] during aerobic type of exercise. Both healthy subjects and COPD patients show improved exercise performance with hyperoxia [12–14]. These findings suggest that certain other clinical populations with impaired cardiovascular and/or pulmonary fitness levels might benefit from exercise under hyperoxic conditions as well. Patients with type 2 diabetes (DM2) might be good candidates for hyperoxic exercise training as previous research indicated that DM2 patients frequently have a reduced diffusion capacity of the lungs (8–25 %), inversely related to blood glucose levels as well as duration and severity of DM2 [15–17]. Pathophysiological mechanisms explaining the impaired pulmonary function may be micro-angiopathy, chronic inflammation and autonomic neuropathy [16, 18] resulting in a diminished alveolar micro-vascular reserve [15, 17, 19–21]. Impaired alveolar gas exchange in DM2 patients has been shown to correlate with a lower \(\dot{V}{\text{O}}_{ 2}\) and workload capacity during aerobic type of exercise [22].
Although beneficial effects of exercise under hyperoxic conditions have been reported for different types of chronic disease populations [1, 4, 8, 23–26], experimental data on an effective dose of hyperoxic air during exercise in DM2 patients are still lacking. Despite the ongoing debate on oxygen transport and consumption [50], increased oxygen availability in arterial blood may improve intracellular transport and uptake of active muscle tissue, and subsequently improve exercise performance. In accordance, the aim of the present feasibility study was to establish an effective dose of supplemental oxygen in DM2 population as a basis to guide and optimise future hyperoxic exercise training protocols.
Methods
Subjects
Eleven patients diagnosed with DM2 for at least 2 years and not taking anti-hypertensive medication were screened and included at the outpatient clinic at Erasmus University Medical Center in Rotterdam, the Netherlands. The characteristics of the eligible patients are presented in Table 1. Out of 22 screened patients, a total of six patients were not willing to participate in the hyperoxic exercise intervention following the maximal exercise test. Four patients were excluded from the hyperoxic experiment because it was not possible to introduce an intra-arterial catheter in the radial artery. One patient was excluded from our study because of abnormally high lactate levels during exercise and was diagnosed with mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes (MELAS) syndrome afterwards. Baseline characteristics of excluded patients were not different from the experimental group. Included subjects gave their informed consent to participate in the study, approved by the medical ethical committee of the Erasmus University Medical Center in Rotterdam (ISRCTN number: NTR2299).
Procedures
Prior to the hyperoxic exercise session all subjects performed a maximal exercise test on a cycle ergometer (Jaeger ER800) using an incremental workload (1.85 W/6 s for men, 1.2 W/6 s for women). The oxygen uptake (\(\dot{V}{\text{O}}_{ 2}\)) (Oxycon Pro, Viasys, Houten, Netherlands) and heart rate (HR) (Polar wear-link, Finland) were measured continuously. A second visit was scheduled within 1–3 weeks following a maximal exercise test. During the second visit subjects performed a hyperoxic exercise session. The bout consisted of 25 min of submaximal cycling at 20 % of the maximal workload capacity (W max). The workload was chosen to ensure that the subjects reach steady state, based on the assumption that the anaerobic threshold is at least 40 % W max in DM2 patients. After calibration patients underwent the Allen’s test, and subsequently beat-to-beat blood pressure was obtained through a percutaneous intra-articular catheter in the radial artery of the non-dominant hand [51]. Data were registered in a computer and analysed using specialised software (Beat scope, Finapres Medical Systems, Amsterdam, the Netherlands). It was performed to minimise the risk of ischaemia of the hand. The exercise protocol consisted of 6 phases: 5 min of rest without supplemental oxygen flow (SOF), 10 min without SOF, 5 min with 5 L min−1 SOF, 5 min with 10 L min−1 SOF, 5 min with 15 L min−1 SOF, 5 min without SOF (Fig. 1). A stage duration of 5 min was chosen to reach steady state during, at least, the last 2 min of each stage [27, 28]. The last stage was added to assess the effect of cessation of SOF.
The SOF was administered directly into a face mask (without a reservoir bag, Teleflex Inc. Hudson RCI adult Multi-Vent air entrainment mask), allowing the inhalation of room air to meet the subjects’ ventilatory demands. In our study, we chose to dose oxygen as a fixed flow quantity, instead of a fixed inspirational fraction with a maximum of 15 L min−1. This design was chosen to match the possibilities of the standard facilities for supplemental oxygen available in most primary and secondary healthcare settings. During the last min of each phase arterial blood gas and the rate of perceived exertion (Borg score) [29] were obtained.
Statistical analysis
An independent sample T test was used to analyse the baseline characteristics and maximal exercise test. We used a single-factor ANOVA with repeated measures to compare the means of the given variables during different hyperoxic exercise phases. Differences with a p value <0.05 were considered significant. The Bonferroni adjustment was applied. Data were presented as mean ± SD.
Results
Participants
The characteristics of the included participants are presented in Table 1.
Maximal exercise test
The average maximal oxygen uptake (VO2max) of the subjects was 1.83 ± 0.59 L min−1. The mean VO2max was on average ~24 % (p < 0.05) below the average of a healthy population of the same age, weight, length and sex based on the regression equations by Fairbarn et al. [30]. Maximal HR was not significantly different form the predicted values according to the Tanaka regression equation [31]. The results of the maximal exercise test are presented in Table 2.
Hyperoxic exercise: blood gas analysis
All included subjects were able to complete 25 min of submaximal hyperoxic exercise. Arterial pO2 levels (Fig. 2a) did not change immediately after starting the exercise (T1–2). The arterial pO2 increased significantly with increased SOF (T2–T5) in a dose-dependent manner and returned to baseline after cessation of the SOF administration (T5–T6). The arterial pCO2 (Fig. 2b) did not change significantly in response to exercise under different SOF.
Blood gas analysis a pO2 levels during hyperoxic exercise. *T3–5 are significantly different from T1, T2 and T6, and each other (p < 0.05). b pCO2 levels during hyperoxic exercise. No significant changes (p < 0.05). c pH levels during hyperoxic exercise. *T6 is significantly higher than T2 and T3 (p < 0.05). d Lactate levels during hyperoxic exercise. No significant changes (p < 0.05)
There was a decreasing trend of the pH (Fig. 2c) at the onset of the exercise bout (T1–T2), while pH increased significantly (p value) during the last step when the supplemental oxygen flow administration was stopped (T5–T6).
Hyperoxic exercise: HR, blood pressure and rate of perceived exertion
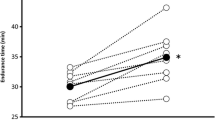
The HR (Fig. 3a) increased significantly after the onset of the exercise bout (T1–T2), and remained unchanged during the SOF phases (T2–T5) and increased after stopping the SOF (T5–T6). After an initial increase of systolic and diastolic blood pressure after starting the exercise (T1–2), systolic, diastolic and mean arterial blood pressure (Fig. 3b–d) did not change during the SOF. Furthermore, the rate pressure product (Fig. 3e) showed a significant increase after stopping the SOF (T5–T6). The rate of perceived exertion (Fig. 3f) increased with the start of exercise (T1–2) and did not increase significantly during exercise (T2–T6).
Cardiovascular response and rate of perceived exertion a HR during hyperoxic exercise. *T1 is significantly lower than T2–6. T6 is significantly higher than T1, T3, and T4 (p < 0.05). b Systolic blood pressure during hyperoxic exercise. *T1 is significantly lower than T2, T3 and T6 (p < 0.05). c Diastolic blood pressure during hyperoxic exercise. No significant changes (p < 0.05). d Mean arterial blood pressure during hyperoxic exercise. No significant changes (p < 0.05). e Rate pressure product during hyperoxic exercise. *T1 is significantly lower than T2–6. T6 is significantly higher than T1 and T3 (p < 0.05). f Rate of perceived exertion (Borg score) during hyperoxic exercise. *T1 is significantly lower T2–T6 (p < 0.05)
Discussion
We tested the feasibility of hyperoxic exercise and dose–response in type 2 diabetes patients. The main finding of this feasibility study was that exercise under SOF 15 L min−1 increased pO2 more effectively than lower doses (5 and 10 L min−1) in DM2 patients (Table 3).
Technical feasibility
From a technical perspective, our results demonstrate that supplemental oxygen, applied with a standard open facemask (5–15 L min−1), results in significant increases in arterial pO2 levels during exercise. Higher pO2 at increased SOF (i.e. 5, 10 and 15 L min−1) suggests a dose-dependent effect. The pO2 levels obtained from the radial artery during hyperoxic exercise in the present study (24.0 ± 2.3 kPa) were comparable with the arterial pO2 levels measured by Plet et al. in healthy subjects. Administration of 55 % of oxygen improved maximal oxygen uptake by 12 % during cycle-ergometry in comparison with normoxic exercise [9]. Other studies investigating the influence of hyperoxia during exercise found slightly higher pO2 levels of approximately 40 kPa obtained from the femoral artery with an inspired oxygen fraction of 60 % [32–34]. Taken together, our data show that supplemental oxygen applied during submaximal exercise via a standard open face mask increases arterial pO2 levels. Additional oxygen availability could compensate for the diminished diffusion capacity, endothelial function and low aerobic capacity seen in most DM2 patients [15, 17, 19–21]. The latter suggests that a hyperoxic training study in DM2 patients could be a potential solution in a medical fitness centre, since no special equipment is needed other than an open facemask and standard gas cylinders with O2. However, before investigating training effects under hyperoxic conditions, this warrants further controlled trials on cardiovascular and pulmonary function in DM2 patients. The results will improve our understanding on whether additional oxygen during exercise may improve oxidative metabolism in populations such as DM2 with deficient cardiovascular and respiratory function.
Patient recruitment and study population
Despite the invasive nature of our study and the fact that use of antihypertensive medication was an exclusion criterion for the present study, the majority (=76 %) of the eligible DM2 patients that were approached in our outpatient clinic were willing to participate in our feasibility study. Although, a training study requires a more long-term commitment, the willingness to participate in our feasibility study indicates that it might be possible to recruit a sufficient and representative proportion of subjects for a randomized clinical trial on the medium-term effects of hyperoxic exercise training.
In accordance with previous studies [35–38], the mean VO2max of the investigated patient sample is well below the average of the healthy population, even when corrected for a high BMI. High HbA1c and fasting glucose levels showed that our overweight subjects had poorly regulated DM2. As such, the present study population may not be representative for the general well-controlled DM2 population. Long-term adherence has been reported to vary substantially (10–80 %) in conventional exercise programs for DM2 patients [39–44]. However, effects of hyperoxic exercise training in other patient populations, with a reduced alveolar and capillary diffusion capacity [12–14], showed the anticipated increase in exercise capacity. Less perceived exercise intensity and improvement of exercise performance will also motivate overweight and with poorly regulated DM2 patients to adhere to hyperoxic exercise training.
Potential outcome measures
In contrast with previous hyperoxic exercise studies [8, 9, 33, 45–47], we observed no change in HR, blood pressure or rate of perceived exertion during exercise while increasing the supplemental oxygen flow during exercise. However, after stopping administration of SOF we observed a significant increase in HR and rate pressure product [HR * systolic blood pressure (SBP)]. The cardiovascular response during phase 6 indicates that hyperoxia lowers the cardiovascular burden during submaximal steady-state exercise in patients with DM2. A number of physiological mechanisms might explain why, in comparison with previous hyperoxic exercise studies, SOF did not lower HR and systemic blood pressure during phases 3–5 in our experimental setup. First, it is possible that even at an exercise intensity of 20 % \(\dot{V}{\text{O}}_{{ 2 {\text{ max}}}}\) max, our patients were not completely in a steady-state condition during phases 3–5. Second, in comparison with previous hyperoxic exercise studies, the absolute exercise intensity may have been too low to cause a significant drop in HR, blood pressure or the rate of perceived exertion (Borg score). Third, the arterial wall stiffening in combination with the diabetes-related endothelial dysfunction may have impaired a normal vascular response to hyperoxia [48, 49].
Limitations of the study
Unfortunately, for medical ethical reasons (invasive study) it was difficult to add a healthy control group or different oxygen conditions. Because of this limitation, we can only speculate about the physiological reason for this abnormal response to hyperoxic exercise. Arterial blood gas collection (arterial blood withdrawal) was vastly limited because of impaired structure of arterial walls in the DM2 patients. These invasive methods may be replaced by non-invasive study measures in the future studies such as bio-impedance cardiography and near-infrared spectroscopy. Nevertheless, the present feasibility study suggests that HR, blood pressure and rate of perceived exertion may not be suitable primary outcome measures for a hyperoxic training study in unfit DM2 patients. Instead, direct assessment of the VO2max should be considered in a hyperoxic training study to monitor and document change in exercise performance.
Conclusions
Based on arterial pO2 measurements, a supplemental oxygen flow of 15 L min−1 appears sufficient to compensate for impaired alveolar and capillary oxygen transport and/or consumption in DM2 patients. Based on this feasibility study, we propose to first investigate acute effects of various inspiratory oxygen fractions on the cardio-respiratory system and speed of oxygen uptake kinetics. This will improve our understanding on potential exercise performance enhancement benefits of supplementary oxygen. This would warrant future studies to investigate the medium- and long-term benefits of hyperoxic exercise training in patients with DM2.
References
Morris DM, Kearney JT, Burke ER. The effects of breathing supplemental oxygen during altitude training on cycling performance. J Sci Med Sport. 2000;3:165–75.
Peltonen JE, Ritola JJ, Ahotupa, et al. Oxygen uptake response during maximal cycling in hyperoxia, normoxia and hypoxia. Aviat Space Environ Med. 2001;72:904–11.
Peltonen JE, Tikkanen HO, Rusko HK. Cardiorespiratory responses to exercise in acute hypoxia, hyperoxia and normoxia. Eur J Appl Physiol. 2001;85:82–8.
Ploutz-Snyder LL, Simoneau JA, Gilders RM, et al. Cardiorespiratory and metabolic adaptations to hyperoxic training. Eur J Appl Physiol Occup Physiol. 1996;73:38–48.
Vanhatalo A, Fulford J, DiMenna FJ, et al. Influence of hyperoxia on muscle metabolic responses and the power-duration relationship during severe-intensity exercise in humans: a 31P magnetic resonance spectroscopy study. Exp Physiol. 2010;95:528–40.
Wilber RL, Holm PL, Morris DM, et al. Effect of F(I)O(2) on physiological responses and cycling performance at moderate altitude. Med Sci Sports Exerc. 2003;35:1153–9.
Ekblom B, Huot R, Stein EM, et al. Effect of changes in arterial oxygen content on circulation and physical performance. J Appl Physiol. 1975;39:71–5.
Perry CG, Talanian JL, Heigenhauser GJ, et al. The effects of training in hyperoxia vs. normoxia on skeletal muscle enzyme activities and exercise performance. J Appl Physiol. 2007;102:1022–7.
Plat J, Pedersen PK, Jensen FB, et al. Increased working capacity with hyperoxia in humans. Eur J Appl Physiol Occup Physiol. 1992;65:171–7.
Welch HG. Hyperoxia and human performance: a brief review. Med Sci Sports Exerc. 1982;14:253–62.
Maeda T, Yasukouchi A. Blood lactate disappearance during breathing hyperoxic gas after exercise in two different physical fitness groups–on the workload fixed at 130 % AT. Appl Human Sci. 1998;17:33–40.
Emtner M, Porszasz J, Burns M, et al. Benefits of supplemental oxygen in exercise training in nonhypoxemic chronic obstructive pulmonary disease patients. Am J Respir Crit Care Med. 2003;168:1034–42.
Palange P, Crimi E, Pellegrino R, et al. Supplemental oxygen and heliox: ‘new’ tools for exercise training in chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2005;11:145–8.
van Helvoort HA, Heijdra YF, Heunks LM, et al. Supplemental oxygen prevents exercise-induced oxidative stress in muscle-wasted patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;173:1122–9.
Chance WW, Rhee C, Yilmaz C, et al. Diminished alveolar microvascular reserves in type 2 diabetes reflect systemic microangiopathy. Diabetes Care. 2008;31:1596–601.
Hsia CC, Raskin P. Lung function changes related to diabetes mellitus. Diabetes Technol Ther. 2007;9:73–82.
Klein OL, Krishnan JA, Glick S, et al. Systematic review of the association between lung function and Type 2 diabetes mellitus. Diabet Med. 2010;27:977–87.
Sandler M. Is the lung a ‘target organ’ in diabetes mellitus? Arch Intern Med. 1990;150:1385–8.
Klein OL, Smith LJ, Tipping M, et al. Reduced diffusion lung capacity in patients with type 2 diabetes mellitus predicts hospitalization for pneumonia. Diabetes Res Clin Pract. 2011;92:12–5.
Ozşahin K, Tuğrul A, Mert S, et al. Evaluation of pulmonary alveolo-capillary permeability in Type 2 diabetes mellitus: using technetium 99mTc-DTPA aerosol scintigraphy and carbon monoxide diffusion capacity. J Diabetes Complications. 2006;20:205–9.
Saler T, Cakmak G, Saglam ZA, et al. The assessment of pulmonary diffusing capacity in diabetes mellitus with regard to microalbuminuria. Intern Med. 2009;48:1939–43.
Cooper BG, Taylor R, Alberti KG, et al. Lung function in patients with diabetes mellitus. Respir Med. 1990;84:235–9.
Grataloup O, Prieur F, Busso T, et al. Effect of hyperoxia on maximal O2 uptake in exercise-induced arterial hypoxaemic subjects. Eur J Appl Physiol. 2005;94:641–5.
Izdebska E, Izdebski J, Trzebski A. Hemodynamic responses to brief hyperoxia in healthy and in mild hypertensive human subjects in rest and during dynamic exercise. J Physiol Pharmacol. 1996;47:243–56.
Karlsen T, Hoff J, Støylen A, et al. Aerobic interval training improves VO2 peak in coronary artery disease patients; no additional effect from hyperoxia. Scand Cardiovasc J. 2008;42:303–9.
Stray-Gundersen J, Chapman RF, Levine BD. “Living high-training low” altitude training improves sea level performance in male and female elite runners. J Appl Physiol. 2001;91:1113–20.
Baron B, Dekerle J, Robin S, et al. Maximal lactate steady state does not correspond to a complete physiological steady state. Int J Sports Med. 2003;24:582–7.
Macsween A. The reliability and validity of the Astrand nomogram and linear extrapolation for deriving VO2 max from submaximal exercise data. J Sports Med Phys Fitness. 2001;41:312–7.
Borg G, Linderholm H. Exercise performance and perceived exertion in patients with coronary insufficiency, arterial hypertension and vasoregulatory asthenia. Acta Med Scand. 1970;187:17–26.
Fairbarn MS, Blackie SP, McElvaney NG, et al. Prediction of HR and oxygen uptake during incremental and maximal exercise in healthy adults. Chest. 1994;105:1365–9.
Tanaka H, Monahan KD, Seals DR. Age-predicted maximal HR revisited. J Am Coll Cardiol. 2001;37:153–6.
Mourtzakis M, González-Alonso J, Graham TE, et al. Hemodynamics and O2 uptake during maximal knee extensor exercise in untrained and trained human quadriceps muscle: effects of hyperoxia. J Appl Physiol. 2004;97:1796–802.
Pedersen PK, Kiens B, Saltin B. Hyperoxia does not increase peak muscle oxygen uptake in small muscle group exercise. Acta Physiol Scand. 1999;166:309–18.
Stellingwerff T, Leblanc PJ, Hollidge MG, et al. Hyperoxia decreases muscle glycogenolysis, lactate production, and lactate efflux during steady-state exercise. Am J Physiol Endocrinol Metab. 2006;290:1180–90.
Brun JF, Bordenave S, Mercier J, et al. Cost-sparing effect of twice-weekly targeted endurance training in type 2 diabetics: a one-year controlled randomized trial. Diabetes Metab. 2008;34:258–65.
Hordern MD, Cooney LM, Beller EM, et al. Determinants of changes in blood glucose response to short-term exercise training in patients with Type 2 diabetes. Clin Sci (Lond). 2008;115:273–81.
Leite SA, Monk AM, Upham PA, et al. Low cardiorespiratory fitness in people at risk for type 2 diabetes: early marker for insulin resistance. Diabetol Metab Syndr. 2009;1:8.
Lindegaard B, Hansen T, Hvid T, et al. The effect of strength and endurance training on insulin sensitivity and fat distribution in human immunodeficiency virus-infected patients with lipodystrophy. J Clin Endocrinol Metab. 2008;93:3860–9.
Balducci S, Leonetti F, Di Mario U, et al. Is a long-term aerobic plus resistance training program feasible for and effective on metabolic profiles in type 2 diabetic patients? Diabetes Care. 2004;27:841–2.
Dunstan DW, Vulikh E, Owen N, et al. Community center-based resistance training for the maintenance of glycemic control in adults with type 2 diabetes. Diabetes Care. 2006;29:2586–91.
Kirk A, Mutrie N, MacIntyre P, et al. Effects of a 12-month physical activity counselling intervention on glycaemic control and on the status of cardiovascular risk factors in people with Type 2 diabetes. Diabetologia. 2004;47:821–32.
Praet SF, van Rooij ES, Wijtvliet A, et al. Brisk walking compared with an individualised medical fitness programme for patients with type 2 diabetes: a randomised controlled trial. Diabetologia. 2008;51:736–46.
Schneider SH, Khachadurian AK, Amorosa LF, et al. Ten-year experience with an exercise-based outpatient life-style modification program in the treatment of diabetes mellitus. Diabetes Care. 1992;15:1800–10.
Shinji S, Shigeru M, Ryusei U, et al. Adherence to a home-based exercise program and incidence of cardiovascular disease in type 2 diabetes patients. Int J Sports Med. 2007;28:877–9.
Byrnes WC, Mihevic PM, Freedson PS, et al. Submaximal exercise quantified as percent of normoxic and hyperoxic maximum oxygen uptakes. Med Sci Sports Exerc. 1984;16:572–7.
Graham TE, Wilson BA. Effects of hypercapnia and hyperoxia on metabolism during exercise. Med Sci Sports Exerc. 1983;15:514–9.
Rousseau A, Bak Z, Janerot-Sjöberg B, et al. Acute hyperoxaemia-induced effects on regional blood flow, oxygen consumption and central circulation in man. Acta Physiol Scand. 2005;183:231–40.
Jansson PA. Endothelial dysfunction in insulin resistance and type 2 diabetes. J Intern Med. 2007;262:173–83.
Tabit CE, Chung WB, Hamburg NM, et al. Endothelial dysfunction in diabetes mellitus: molecular mechanisms and clinical implications. Rev Endocr Metab Disord. 2010;11:61–74.
Crecelius AR, Kirby BS, Dinenno FA. Intravascular ATP and the regulation of blood flow and oxygen delivery in humans. Exerc Sport Sci Rev. 2015;43(1):5–13.
Limberg JK, Kellawan JM, Harrell JW, Johansson RE, Eldridge MW, Proctor LT, Sebranek JJ, Schrage WG. Exercise-mediated vasodilation in human obesity and metabolic syndrome: effect of acute ascorbic acid infusion. Am J Physiol Heart Circ Physiol. 2014;307(6):H840–7.
Authors’ contributions
RR and SP designed the study protocol, obtained an approval from the medical ethical committee, performed the experiments and took significant part in writing this manuscript. RM assisted during the experiments and significantly contributed in writing the manuscript. JL, ES and AM advised on the contents of the protocol and contributed inclusion of type 2 diabetes patients. HS and LL advised on the contents of the protocol and chosen methods and contributed significantly by revising a manuscript. All authors read and approved the final manuscript.
Acknowledgements
This study was supported by the Dutch Research Foundation 2008.11.007. The authors would like to thank Ashraf Fagirzada and Mery Arevalo de Weever for their assistance with patient recruitment and experimental procedures.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Rozenberg, R., Mankowski, R.T., van Loon, L.J.C. et al. Hyperoxia increases arterial oxygen pressure during exercise in type 2 diabetes patients: a feasibility study. Eur J Med Res 21, 1 (2016). https://doi.org/10.1186/s40001-015-0194-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-015-0194-5