Abstract
Background
The purpose of the present study was to investigate the influence of the pronator quadratus (PQ) muscle repair following volar plate fixation of distal radius fractures with special regards to the forearm pronation strength. During the early recovery period of 3 months, an improvement of pronation strength and functional scorings was hypothesized for the PQ repair when compared to no repair.
Methods
The inclusion criteria were (1) men or women between 18 and 80 years, (2) isolated, closed fractures of the distal radius, (3) A2 to B2 types of fracture according to the AO fracture classification system, (4) primary volar locking plate osteosynthesis. Patients were randomized to group A = PQ repair and group B = no repair. Follow-up examinations after 6 and 12 weeks included bilateral isometric pronation strength measurement, range of motion, the QuickDASH and the Mayo-Wrist-Score, and a visual analog scale (VAS).
Results
60 patients (n = 31 in group A and n = 29 in group B) with an average age of 54 years (range 22–77 years) returned for both follow-up visits. The pronation strength measurements showed no significant differences between groups (PQ repair vs. no repair) neither at 6 weeks nor at 12 weeks. Additionally, no statistical significant differences were noted for ROM, QuickDASH-Score or Mayo-Wrist-Score. The VAS scoring revealed a significant decreased pain level after PQ repair at 6 weeks postoperatively (p = 0.017).
Conclusion
An improved pronation strength after PQ repair in the early rehabilitation period could not be confirmed. However, the PQ repair might reduce pain in the early postoperative period.
Trial registration number: NCT02595229 (ClinicalTrials.gov, registered 02 November 2015)
Similar content being viewed by others
Background
Distal radius fractures account for the most common fractures (up to 25 %) and their incidence is increasing in an aging population [1, 2]. The volar locking plate osteosynthesis has become the treatment of choice for distal radius fractures in recent years. This technique enables good functional results with high fragment stability and a lower complication rate than alternative procedures as external fixation, closed reduction and casting, percutaneous pin fixation or dorsal plating [3, 4]. During the volar approach the release of the pronator quadratus muscle (PQ) from its radial insertion is required for visualization and fixation of the fracture at the distal radius [5, 6]. In this context, the suturing of the PQ muscle following plate fixation is controversially discussed. According to the current literature the assumed benefits of this muscle repair include restoration of the pronation strength, protection of the flexor tendons, and stability of the distal radioulnar joint [7–9]. However, a sufficient repair of the PQ muscle can often be difficult due to the poor tissue quality [10]. It is described that a tight repair might even lead to ischemic contractures with a subsequently decreased range of motion [11]. A number of studies evaluated the efficacy of PQ repair in patients with repair of the PQ muscle versus no repair and reported no differences in terms of functional outcome [12, 13]. However, these studies lacked objective strength testing in forearm pronation.
The main purpose of this prospective trial was to determine the influence of PQ repair on forearm pronation strengths during the initial rehabilitation period of 3 months after surgery. The hypothesis was that a repair of the PQ muscle after volar plating of distal radius fractures leads to higher isometric pronation strengths when compared to no PQ repair. Moreover, an improved functional outcome based on validated upper extremity scores was assumed with PQ repair following volar plate osteosynthesis.
Methods
Study population
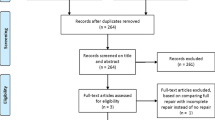
The present survey was performed as a prospective, randomized controlled single-center study. The local institutional ethics committee approved the study protocol (study number 2759/10), trial registration number NCT02595229 (ClinicalTrials.gov, registered 02 November 2015). From May 2010 to March 2013, 72 consecutive patients were included in the study. The inclusion criteria were (1) male or female patient with an age between 18 and 80 years, (2) isolated, closed fractures of the distal radius, (3) A2 to B2 types of fracture according to the AO fracture classification system (4), primary volar locking plate osteosynthesis within 7 days after trauma. For exclusion the following criteria were determined: (1) concomitant fractures of the affected upper extremity, (2) intra-articular distal radius fractures (type C), (3) concomitant neurovascular injuries or preexisting neurological illnesses, (4) initial external fixation. The study was performed as a single-blinded, controlled randomized trial. Randomization into group A = repair of the PQ muscle and group B = without PQ repair was performed by an independent member of the institutional study center. Written informed consent was obtained from each patient when initially presented at the emergency room.
Surgical procedure and postoperative management
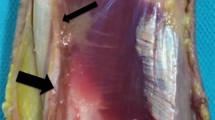
All operations were performed by experienced upper extremity surgeons under regional or general anaesthesia. Following standard volar approach, a complete longitudinal incision of the PQ muscle at the radial third with a subsequent careful elevation of the muscle from the bone was performed for visualization of the distal radius in all cases (Fig. 1).
After fracture reduction and consecutive volar plate fixation, in group A the PQ muscle was sutured with three to five U-shaped stitches using a polyfilament, absorbable synthetic suture (3.0 Vicryl, Ethicon Norderstedt, Germany). In the control group (group B), the PQ was just placed to its anatomic position but without suture repair. For plate osteosynthesis, in three cases a 2.4 mm unidirectional locking plate (Synthes, Umkirch, Germany) was used. The remaining included patients had received a 2.5 mm multidirectional fixed-angle plate (Distal Radius 2.5, Medartis, Basel, Switzerland).
All the patients underwent the same postoperative management irrespective of the study arm. Within the first 2 weeks the wrist was immobilized in a cast for active motion. Passive exercises started under physiotherapist’s supervision the day after surgery. After 4 weeks the cast was removed and physiotherapy with unrestricted active range of motion was allowed. Weight bearing was restricted for 6 weeks postoperatively.
Outcome parameters
Patients returned 6 and 12 weeks after surgery for follow-up visits. Personal interviews and physical examinations were carried out by an independent investigator (SH) not involved in the initial surgical procedure.
As primary outcome parameter the isometric pronation strength was measured using the IsoForce-Control EVO 2 dynamometer (MDS AG, Oberburg, Switzerland) on a self-built measurement apparatus (Fig. 2). With the flexed forearm (in 90°) in neutral position, the operated arm was tested with three isometric effort trials (5 s/trial) while recording the maximum and mean pronation strength of every trial. The averaged values were used for evaluation.
Secondary outcome parameters included the range of motion (ROM) of both wrists, the shortened Disabilities of the Arm, Shoulder and Hand questionnaire (QuickDASH), the Mayo-Wrist-Score, and a visual analog scale (VAS) (range 0 points = no pain to 10 points = maximum pain) [14–16].
Moreover, postoperative radiographs were reviewed for maintenance of fracture reduction and implant-related complications.
Statistical analysis
Continuous variables are presented as mean ± standard deviation (SD) or median and range in case of skewed distributions. Categorical variables are presented as absolute and relative frequencies. Differences between groups were assessed using a two sample t test, a Mann–Whitney U test, or a Fisher’s exact test, as appropriate. For the comparison of different time points within a group, paired t test or Wilcoxon signed rank test was used. All reported P values are two sided, with a significance level of 0.05 and have not been adjusted for multiple testing. Statistical analysis was performed using IBM SPSS Statistics for Windows, version 22 (Armonk, NY, USA: IBM Corp.).
Results
From the 72 included patients, 60 patients (47 females, 13 males) with an average age of 54 years (range 22–77 years) returned for both follow-up visits.
31 patients (group A) with a mean age of 52 years (range 22–77 years; 24 females and 7 males) had a PQ repair, whereas 29 patients (group B) with a mean age of 56 years (range 25–76 years; 24 females and 5 males) had no PQ muscle repair. In both groups all fractures were A-type distal radius fractures according to the AO classification. There were two A2-type and 29 A3-type fractures in group A, and five A2-type and 25 A3-type fractures in group B, respectively.
Two patients dropped out of the study. One patient (group B) needed to be revised due to loss of fracture reduction 15 days after index surgery and another patient (group A) has developed a carpal tunnel syndrome 6 weeks postoperatively and resulted in reoperation. 10 patients were not available for both follow-up examinations and were, therefore, secondarily excluded.
Isometric pronation strength
At 6 weeks postoperatively, higher values for the PQ repair (±30 %) were seen for the maximum pronation strength (F max) but without significant differences between groups [group A—median 52.1 N (range 22.0–232.9 N); group B—median 40.2 N (range 23.1–92.0 N); p = 0.112]. Accordingly, the median of the mean pronation strength (F mean) was 44.8 N (range 19.4–172.7 N) for group A (±19.5 %) and 37.5 N (range 21.2–82.6 N) in group B (p = 0.169) (Figs. 3, 4). For further analysis, the ratio (ΔF) between the operated and non-operated hand was evaluated for maximum and medium strengths. There could also not be found any significant differences between group A and B (for F max p = 0.599 and for F mean p = 0.610).
12 weeks after surgery, increased pronation strengths were found in both groups with F max of median 65.9 N (range 28.5–210.0 N) in group A (±7.9 %) and 61.1 N (range 38.3–123.4 N) in group B, but without statistical significance between groups (p = 0.333). The median of F mean was 63.6 N (range 27.2–203.3 N) in group A (±7.8 %) and 59.0 N (range 35.3–111.8 N) in group B (p = 0.403) (see Figs. 3, 4).
Similar to the 6-week follow-up, at 3 months postoperatively no significant differences were detected for the group comparison of ΔF (for F max p = 0.641; for F mean p = 0.403).
ROM
The results of ROM are summarized in Table 1. Neither at 6 weeks nor at 12 weeks after surgery any differences were observed between groups. Furthermore, for each group no statistically significant differences in ROM were seen when confronted the injured with the uninjured side (not shown).
Outcome scoring
At 6 weeks postoperatively, the QuickDASH-Score showed a median of 34 (range 0–75) points in group A and 30 (range 5–57) points in group B (p = 0.789). After 12 weeks, the values strongly decreased with a QuickDASH of 3.5 (range 0–55) points in group A and 5 (range 0–23) points in group B indicating an improved functional outcome (p = 0.887) (Fig. 5).
For the Mayo-Wrist-Score, satisfying results were shown after 6 weeks in both groups with a median of 70 (range 30–100) points in group A (including 8 excellent, 6 good, 7 satisfying, and 10 bad outcomes), and 70 (range 50–110) in group B (including 1 excellent, 8 good, 13 satisfying, and 7 bad outcomes). At 12 weeks the values improved in both groups representing excellent results with median 100 (range 40–100) points in group A (25 excellent, 4 good, 2 bad outcomes) and 95 (range 50–100) points in group B (23× excellent outcomes, 5× good outcomes, 1× bad outcome). No significant differences could be verified between groups (p = 0.994 at 6 weeks; p = 0.657 at 12 weeks).
VAS
At 6 weeks postoperatively a significant reduction of pain was found following repair of the PQ muscle with a pain level between 0 and 2 in 84 % of the patients in group A versus only 62 % in group B (p = 0.017). At the 12-week follow-up no significant difference could be seen (pain level between 0 and 2 in group A—91 % and group B—93 %; p = 1.000) (Fig. 6).
For both groups, complete bony healing was seen in all fractures after 12 weeks without any implant-related complications. There were no wound healing disturbances and tendon irritations or ruptures, respectively.
Discussion
The pronator quadratus muscle repair after volar plating of distal radius fractures is still a topic of debate in the current literature. According to a recent survey, the majority of surgeons attempt to repair the PQ muscle after plate fixation [17]. Even though there are several studies evaluating the functional outcome with special respect to the PQ repair, to the best of our knowledge, no prospective comparative study measuring the objective pronation strength has been published to date [4, 12, 13, 18, 19]. The aim of the present study was to prove the theory that a PQ muscle repair leads to higher isometric pronation strengths in the initial postoperative period. Moreover, various functional outcome parameters were assessed to be compared between patients with PQ repair versus no repair.
The most important finding of this study was that an increased pronation strength in patients with PQ repair was evident 6 and 12 weeks after surgery. Nevertheless, the higher values of maximum (+30 %) at 6 weeks; (+7.9 %) at 12 weeks and mean (+19.5 %) at 6 weeks; (+7.8 %) at 12 weeks pronation strengths in the PQ repair group were not statistically significant compared to the no repair group, so that the aforementioned hypothesis could not be confirmed. These strength deficits, however, match favorably to those of the study of McConkey et al. [20]. The authors reported on a 16–23 % significant loss of isometric pronation torque (depending on forearm rotation) upon complete denervation of the PQ muscle in healthy volunteers when compared to the normal arm side, and these results likely correlate with those of patients without PQ repair in this study. The decreasing difference in pronation strength between groups during the follow-up visits is probably caused by muscle and soft tissue scarring, regardless of a PQ repair or not. The question, however, remains whether a difference of approximate 7.9 % in pronation strength is clinically relevant in the rehabilitation period 12 weeks after surgery or later. For answering this question, further evaluations with a longer follow-up are needed.
Furthermore, in the present study, groups were confronted with respect to the strength ratio (ΔF) between the operated and non-operated armside. The rationale, therefore, was that it seems natural that a straight comparison of the affected and non-affected extremity in the early postoperative period would show decreased strength values. Nevertheless, no differences were found between groups either. Huh et al. demonstrate less isokinetic pronation strengths at 6 months in the operated forearm than in the normal side, but at 12 months postoperatively, the differences in pronation strength were not significant anymore [19]. As consequence the authors suggested that dissection of the PQ may have minimal clinical impact on the forearm pronation function. Nonetheless, the authors also pointed out that dissected PQ muscles were not completely repaired in their cohort of patients and assumed a better pronation power during the early recovery period with a preserved or well-repaired PQ muscle [18]. This fact could not be verified in the present study.
High functional outcomes (near preinjury ROM, minor values of the QuickDASH indicating a very low level of upper extremity disability, excellent results of the Mayo-Wrist-Score in >93 % of the patients) were seen at the latest follow-up in both groups, even though without differences among each other. Trosti and Ilyas [13] also performed a prospective evaluation of pronator quadratus repair versus no repair following volar plate fixation with a minimum follow-up of 12 months. They even found no significantly different results between groups according to ROM at the wrist, DASH scores, grip strength, and VAS scores. These findings as well as the results of the present study compare favorably to those of other recently published studies [21, 22]. In a retrospective study with a 3-month follow-up, Ahsan et al. [4] found no differences in ROM and grip strength in 108 patients with complete and incomplete PQ repair. Hershman et al. [12] examined the outcome effects in 112 patients treated with or without PQ repair after a follow-up of 1 year. They found no differences in pronation, pain and DASH scores and, therefore, concluded that there is no advantage in repairing the PQ muscle during volar plating of distal radius fractures.
The lack of significant differences between groups in the present study may be caused by PQ repair failure as well. Nevertheless, Swigart et al. [17] in their prospective clinical cohort study have shown that only 4 % of the PQ repairs failed within the first 3 months after surgery. The repair of the pronator quadratus muscle, however, can be frequently challenging due to various reasons such as traumatic disruption, fracture comminution or poor soft tissue quality, particularly in aged patients. For that reason patients presenting with open fractures and complex intra-articular fracture types were excluded from the present study. In the repair group the reconstruction of the PQ muscle could be performed in all patients. There are some few authors who state that a complete or, if not possible, at least an incomplete PQ repair is the critical factor to reduce flexor tendon irritations or ruptures [4, 23]. In recent years, diverse authors have, therefore, reported on pronator sparing or splitting techniques to address this difficulty [10, 24]. The reported incidence of tendon complications after volar plating varies between 2 and 12 % [11, 22, 25, 26]. As opposed to this, in both groups of the present study no tendon irritations or ruptures were clinically apparent during the follow-up period and similar results were also shown in the current literature [4]. Correspondingly, a significant difference in pain (measured on VAS scale 0–10) was observed between the PQ repair and no repair group (p = 0.017) within the initial rehabilitation period of 6 weeks postoperatively. This fact might be explained by the better hardware coverage and, therefore, less irritation of the overlying flexor tendons.
This study has some limitations. First of all, it has to be clearly stated that the results seen in this very short duration of follow-up might change with a longer follow-up term. However, concerning about the functional outcomes of cited studies above that have shown no differences up to 1 year of follow-up, it is doubtful whether the pronation strength or other functional parameters will be changed during the further postoperative time period [4, 12, 18, 19]. This study did not examine pronation strengths in relation to the dominant arm side, which can potentially be influenced by a PQ repair or not, and moreover, the quality of fracture reduction or plate positioning was ignored. A power analysis has not been performed a priori, as, during the planning of the study, no comparable studies have been published.
Nevertheless, this study has several strengths presented by multi-functional outcome scorings including objective pronation strength testing of all included patients at both follow-up visits and the comparability of evaluated groups. The demographic characteristics (age, gender) as well as the fracture pattern and the used implants were matchable between both groups. Furthermore to our research of the literature, this study is the first prospective randomized trial evaluating the objective forearm pronation strengths after volar plating of distal radius fractures and pronator quadratus muscle repair.
Conclusions
In the present study, with the PQ muscle repair after volar locked plating of distal radius fractures only a positive trend could be shown on forearm pronation strength in the early postoperative period of 3 months. The statement, however, that a PQ repair will lead to a higher pronation strength versus no repair could not be proven. The authors, therefore, conclude that there is no advantage in repairing the PQ muscle during volar plating of distal radius fractures in terms of pronation strength improvement. Even though not supported by the present data, the authors subscribe to previous authors’ recommendation for a careful reconstruction of the PQ muscle to reduce postoperative pain, achieve safe coverage of the implant and thus potentially avoid postoperative complications.
Abbreviations
- PQ:
-
pronator quadratus muscle
- VAS:
-
visual analog scale
- ROM:
-
range of motion
- F max :
-
maximum pronation strength
- F mean :
-
mean pronation strength
References
Gehrmann SV, Windolf J, Kaufmann RA. Distal radius fracture management in elderly patients: a literature review. J Hand Surg Am. 2008;33(3):421–9.
Nellans KW, Kowalski E, Chung KC. The epidemiology of distal radius fractures. Hand Clin. 2012;28(2):113–25.
Rozental TD, Blazar PE, Franko OI, Chacko AT, Earp BE, Day CS. Functional outcome and complications after volar plating for dorsally displaced, unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. A prospective randomized trial. J Bone Surg Am. 2009;91(8):1837–46.
Ahsan ZS, Yao J. The importance of pronator quadratus repair in the treatment of distal radius fractures with volar plating. HAND. 2012;7(3):276–80.
Orbay J, Badia A, Khoury RK, Gonzalez E, Indriago I. Volar fixed-angle fixation of distal radius fractures: the DVR plate. Tech Hand Up Extrem Surg. 2004;8(3):142–8.
Protopsaltis TS, Ruch DS. Volar approach to distal radius fractures. J Hand Surg Am. 2008;33(6):958–65.
Johnsons RK, Shrewsbury MM. The pronator quadratus in motions and stabilization of the radius and ulna at the distal radioulnar joint. J Hand Surg Am. 1976;1(3):205–9.
Klug RA, Press CM, Gonzales MH. Rupture of the flexor pollicis longus tendon after volare fixed-angle plating of a distal radius fracture: a case report. J Hand Surg. 2007;32(7):984–8.
Kihara H, Short WH, Werner FW, Fortino MD, Palmer AK. The stabilizing mechanism of the distal radioulnar joint during pronation and supination. J Hand Surg Am. 1995;20(6):930–6.
Sen MK, Strauss N, Harvey EJ. Minimally invasive plate osteosynthesis of distal radius fractures using a pronator sparing approach. Tech Hand Up Extrem Surg. 2008;12(1):2–6.
Berglund LM, Messer TM. Complications of volar plate fixation for managing distal radius fractures. J Am Acad Orthop Surg. 2009;17(6):369–77.
Hershman SH, Immermann I, Bechtel C, Lekic N, Paksima N, Egol KA. The effects of pronator quadratus repair on outcomes after volar plating of the distal radius fractures. J Orthop Trauma. 2013;27(3):130–3.
Tosti R, Ilyas AM. Prospective evaluation of pronator quadratus repair following volar plate fixation of distal radius fractures. J Hand Surg. 2013;38(9):1678–84.
Germann G, Harth A, Wind G, Demir E. Standardisation and validation of the German version 2.0 of the disability of arm, shoulder, hand (DASH) questionnaire. Unfallchirurg. 2003;106:13–9.
Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006;7:44.
Lamey D, Fernandez D. Results of the modified Sauvé-Kapandji procedure in the treatment of chronic posttraumatic derangement of the distal radioulnar joint. J Bone Joint Surg. 1998;80-A:1758–69.
Swigart CR, Badon MA, Bruegel VL, Dodds SD. Assessment of pronator quadratus repair integrity following volar plate fixation. J Hand Surg Am. 2012;37(9):1868–73.
Fan J, Chen K, Zhu H, Jiang B, Yuan F, Zhu X, Mei J, Yu G. Effect of fixing distal radius fracture with volar locking palmar plates while preserving pronator quadratus. Chin Med J (Engl). 2014;127(16):2929–33.
Huh JK, Lim JY, Song CH, Baek GH, Lee YH, Gong HS. Isokinetic evaluation of the pronation after volar plating of a distal radius fracture. Injury Int J Care Injured. 2012;43(2):200–4.
McConkey MO, Schwab TD, Travlos A, Oxland TR, Goetz T. Quantification of pronator quadratus contribution to isometric pronation torque of the forearm. J Hand Surg Am. 2009;34(9):1612–7.
Hakimi M, Jungbluth P, Windolf J, Wild M. Functional results and complications following locking palmar plating on the distal radius: a retrospective study. J Hand Surg Eur. 2010;35(4):283–8.
Jupiter JB, Marent-Huber M, LCP Study Group. Operative management of distal radial fractures with 2.4-millimeter locking plates: a multicenter prospective case series. J Bone Joint Surg Am. 2009;91(1):55–65.
Ateschrang A, Stuby F, Werdin F, Schaller HE, Weise K, Albrecht D. Flexor tendon irritations after locked plate fixation of the distal radius with the 3.5 mm T-plate identification of risk factors. Z Orthop Unfall. 2010;148:319–25.
Dos Remedios C, Nebout J, Benlarbi H, Caremier J, Sam-Wing JF, Beya R. Pronator quadratus preservation for distal radius fractures with locking palmar plate osteosynthesis. Surgical technique. Chir Main. 2009;28:224–9.
Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007;21:316–22.
Soong M, Earp BE, Bishop G, Leung A, Blazar P. Volar locking plate implant prominence and flexor tendon rupture. J Bone Joint Surg Am. 2011;93:328–35.
Authors’ contributions
SH, GS, TK, US and SS were substantially involved in conception and design of the study, coordination and supervision of data collection, statistics, drafting the initial version of the manuscript and final approval of the version to be published. They are responsible for the overall content as guarantors. SD, FF, TT and PB were involved in conception and design of the study, data collection, technical support and reviewing of the manuscript for important intellectual content. SH and IR carried out the statistical analysis. US and PB reviewed and revised the manuscript and approved the final manuscript as submitted. All authors read and approved the final manuscript.
Acknowledgements
We thank Fritz Seidl, MA interpreting and translating for his excellent language copyediting.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sandra Häberle and Gunther Hubertus Sandmann contributed equally
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Häberle, S., Sandmann, G.H., Deiler, S. et al. Pronator quadratus repair after volar plating of distal radius fractures or not? Results of a prospective randomized trial. Eur J Med Res 20, 93 (2015). https://doi.org/10.1186/s40001-015-0187-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-015-0187-4