Abstract
Background
Preoperative anxiety is a health concern among patients scheduled for surgical interventions. Little is known about the prevalence of preoperative anxiety among patients in different healthcare systems of developing countries. This study was conducted to determine the prevalence of preoperative anxiety among patients undergoing surgery in Palestine. Another objective was to identify the factors associated with preoperative anxiety.
Methods
This study was conducted in a cross-sectional descriptive design. Patients scheduled for surgical interventions were interviewed using an interviewer-administered questionnaire. The questionnaire collected the demographic, clinical, and surgical variables of the patients. The questionnaire also contained the Amsterdam preoperative anxiety and information scale (APAIS), and a short version of the Spielberger state-trait anxiety inventory (STAIS-5/STAIT-5).
Result
A total of 280 patients were included. The mean APAIS total score was 13.6 ± 5.9, the mean APAIS anxiety domain score was 8.3 ± 4.3, and the mean APAIS need for information domain was 1.6 ± 0.50. Of the patients, 76 (27.1%) had high anxiety and 160 (57.1%) expressed a high need for information. The higher APAIS anxiety scores were predicted by being female, having chronic diseases, being scheduled to be operated on within 24 h, and having experienced surgical complications. The mean STAIS-5 score was 10.0 ± 4.2 and the mean STAIT-5 was 10.3 ± 3.8. Of the patients, 140 (50.0%) had high state anxiety and 56 (20.0%) had high trait anxiety. Higher STAIS-5 scores were predicted by being female, younger than 42 years, and scheduled to be operated on within 24 h. Higher STAIT-5 scores were predicted by being female. A positive correlation was identified between APAIS total, APAIS anxiety, APAIS need for information, STAIS-5, and STAIT-5 scores.
Conclusion
Preoperative anxiety was prevalent among patients scheduled for surgical operations in Palestinian hospitals. Anesthesiologists and other providers of perioperative care should screen preoperative patients who are female, have chronic diseases, are scheduled to be operated on within 24 h, and having had experienced surgical complications for preoperative anxiety. More studies are still needed to investigate the effects of the implemented measures on the prevalence of preoperative anxiety.
Similar content being viewed by others
Background
Surgical and medical interventions carried out under general, regional, and local anesthesia are common. It has been estimated that annually more than 230 million major surgical interventions are carried out under anesthesia globally (Weiser et al. 2008). Previous studies have reported that the majority of patients undergoing surgery would experience some level of anxiety; therefore, preoperative anxiety has been recognized as a health concern in perioperative care (Eberhart et al. 2020; Abate et al. 2020; Zemła et al. 2019). Anxiety is an unpleasant feeling of dread over something unlikely to happen, such as the feeling of imminent death (Fernández-Donaire et al. 2019). Anxiety is often accompanied by restlessness, fatigue, problems in concentration, and muscular tension. Preoperative anxiety is described as a vague, uneasy feeling the source of which is often nonspecific to the individual (Ayele et al. 2021).
Previous studies have shown that the prevalence and severity of preoperative anxiety were associated with different patient- and healthcare-related factors (Eberhart et al. 2020; Abate et al. 2020; Zemła et al. 2019). Age, gender, marital status, educational level, type of surgery, type of anesthesia, and presence of chronic diseases were reportedly associated with preoperative anxiety (Eberhart et al. 2020; Abate et al. 2020; Zemła et al. 2019; Liu et al. 2022; Moura et al. 2016; Fentie et al. 2022; Bedaso et al. 2022). Of the different factors, worrying about the success of surgery, postoperative course, and complications were the most important factors (Khalili et al. 2019; Mariyam et al. 2020). In a systematic review with meta-analysis that included 14,652 surgical patients, Abate et al. reported that the pooled prevalence rate of preoperative anxiety among the patients was 48% (95% confidence interval (CI) 39 to 47%) (Abate et al. 2020). In another systematic review with meta-analysis that included 5575 surgical patients from 12 low- and middle-income countries, Bedaso et al. reported that the pooled prevalence rate of preoperative anxiety among the patients was 55.7% (95% CI 48.60 to 62.93) (Bedaso et al. 2022).
Anxiety is an unpleasant and disturbing experience that would involve tension, apprehension, uneasiness, and high autonomic activity. Therefore, preoperative anxiety was shown to be associated with significant negative effects on the health and quality of life of the patients. These effects include changes in blood pressure, fluid and electrolyte imbalances, diminished immune responses, and longer wound healing (Bedaso and Ayalew 2019). These negative effects can increase the risk of perioperative complications and delay postoperative recovery. Additionally, preoperative anxiety can increase the intensity of pain, which in turn, would increase the need for higher doses of anesthetics, consumption of analgesics, morbidity, and mortality. Different approaches to reducing or managing preoperative anxiety were described (Kuzminskaitė et al. 2019). These approaches include using anxiolytics, prayers, massage, music therapy, and counseling/conversation with physicians, counselors, or relatives.
Although preoperative anxiety is a common and important health issue in perioperative healthcare, it is often an overlooked health problem in many healthcare systems of developing countries. Currently, little is known about the prevalence of preoperative anxiety among patients undergoing surgery in Palestine and other developing countries. Additionally, little research was done to identify the factors that could be associated with higher or lower levels of preoperative anxiety among patients undergoing surgeries in developing countries. Therefore, this study was conducted to determine the prevalence of preoperative anxiety among patients undergoing surgery in a developing country. Another objective was to identify the factors associated with preoperative anxiety. The findings of this study might have significant implications for the perioperative care of patients being managed in developing countries.
Methods
Study design
This study was conducted in a cross-sectional descriptive design to assess the prevalence of preoperative anxiety among hospitalized patients and to identify the factors associated with preoperative anxiety in Palestine as a developing country. The study was conducted and reported in adherence to the strengthening of the reporting of observational studies in epidemiology (STROBE) statement (Vandenbroucke et al. 2007).
Study population, sample size, and recruitment
The study population was patients scheduled for elective surgeries in different hospitals. The sample size was calculated using an online sample size calculator (www.raosoft.com). The sample size was calculated at a 90% confidence interval (95% CI) tolerating a margin of error of 5%.
In this study, patients scheduled for minor or major elective surgeries were approached and recruited from 14 different hospitals by three final-year medical students (MT, NA, ZS) who were trained to interview patients. The patients were recruited when they met the following inclusion criteria: (1) being older than 18 years and younger than 75 years, (2) being admitted to a surgical ward in a hospital for minor or major elective surgery, (3) willingness to respond to items in a questionnaire, and (4) providing written informed consent. Patients with psychiatric illnesses, cognitive impairments, and those who were admitted for emergency surgeries were not included in this study.
Study tool
This study was conducted with the help of a data collection form that was developed specifically for this study. The data collection form was based on previous related studies (Eberhart et al. 2020; Abate et al. 2020; Ayele et al. 2021; Moura et al. 2016; Fentie et al. 2022; Bedaso et al. 2022; Khalili et al. 2019; Mariyam et al. 2020; Bedaso and Ayalew 2019; Aust et al. 2018; Gürler et al. 2022; Li et al. 2021; Moerman et al. 1996; Navarro-Gastón and Munuera-Martínez 2020; Yu et al. 2022). The data collection form was organized into sections. The first section collected the demographic, clinical, and surgical variables of the patients including gender, age, marital status, educational level, employment status, place of residence, and household monthly income. Additionally, the patients were asked to self-rate their satisfaction with their social life and religious commitment. The medical and surgical records of the patients were used to collect information on whether the patient had chronic diseases, type of surgery, the timing of surgery, type of anesthesia, type of hospital, whether the patient had previous surgeries, and whether the patient had suffered surgical or anesthesia complications. The second section contained the Amsterdam Preoperative Anxiety and Information Scale (APAIS) (Moerman et al. 1996). This scale contained 6 items on which the patients responded by describing how they felt using a Likert scale of 5-points (1 = not at all, 5 = extremely). The third section contained the short form of the Spielberger State-Trait Anxiety Inventory (STAIS-5/STAIT-5) (Zsido et al. 2020). The scale was of 2 domains (state = 5 items and trait = 5 items, total = 10 items) on which the patients responded using a Likert scale of 1–4 (1 = not at all, 4 = very much). State anxiety described how the patient felt at the moment and trait anxiety described how the patient generally felt.
Validity and reliability
A pilot study was conducted among 25 patients who did not participate in the larger study. The patients were asked to respond to the questionnaire twice. The test–retest method was used to ensure the reliability and stability of the scores over a short period. The internal consistency (item-relatedness) was investigated using Cronbach’s alpha. In this study, Pearson’s correlation coefficient (Pearson’s r) was 0.93 which indicated excellent stability of responses. The Cronbach’s alpha of the 6-item APAIS was 0.77 and the Cronbach’s alpha of the 10 STAIS-5/STAIT-5 items was 0.84 (the Cronbach’s alpha of the 5-item STAIS-5 was 0.86 and the Cronbach’s alpha of the 5 item STAIT-5 was 0.75). These high values indicated that the questionnaire was reliable and internally consistent.
Data analysis
The data collected in this study were tabulated in Microsoft Excel Spreadsheets. For each patient, the total APAIS, STAIS-5, and STAIT-5 scores were calculated by summing the responses of the patient on each item in the respective scale (Moerman et al. 1996; Zsido et al. 2020). The APAIS anxiety scores were calculated by summing the responses of the patients on items 1, 2, 4, and 5 and the APAIS need for information scores were calculated by summing the responses of the patients on items 3 and 6. A total APAIS anxiety score of < 11 indicated no or minimal anxiety and a total APAIS anxiety score of ≥ 11 indicated high anxiety. A total APAIS need for information score between 2 and 5 indicated no or little need for information and a total APAIS need for information score of > 5 indicated a high need for information. A total STAIS-5 score of > 9.5 indicated high state anxiety and a total STAIT-5 score of > 13.5 indicated high trait anxiety.
The data were entered into IBM SPSS v.21.0. The data were tested for normal distribution using absolute skewness and kurtosis values. The data were considered normally distributed when the absolute skewness values were between − 2 to + 2 and the absolute kurtosis values were between − 7 to + 7. Because the data were normally distributed, means with their respective standard deviation (SD) were used. Scores were compared using t-tests or analysis of variance (ANOVA) as appropriate. To control potentially confounding factors, the variables that were significantly associated in the t tests and ANOVA were included in multiple linear regression models. Goodness-of-fit was assessed using statistically significant R2. Tolerance and variance inflation factor (VIF) values were used to detect multicollinearity issues. Categorical data were compared using Chi-square or Fisher’s exact test (FET) as appropriate. To control potentially confounding factors, the variables that were significantly associated in the chi-square or FET were included in multivariate logistic regression models. Odds ratios (OR) with their 95% confidence intervals (95% CI) were calculated. In this study, statistical significance was indicated by a p value of < 0.05. Scores were correlated using Pearson’s correlations. Pearson’s correlation coefficient (Pearson’s r) of ≥ 0.70 was arbitrarily considered strong, 0.70 < Pearson’s r ≥ 0.30 was considered moderate, and < 0.30 was considered weak.
Ethical considerations
This study was conducted in compliance with the international ethical standards in the Declaration of Helsinki. The study received approval from the Institutional Review Board (IRB) of An-Najah National University (IRB protocol approval # Nov.3.2021). Approval was also obtained from the Office of Health Education of the Palestinian Ministry of Health. Written informed consent was obtained from each patient. The data collected were treated as confidential and were coded before analysis.
Results
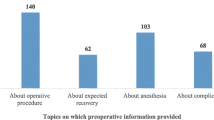
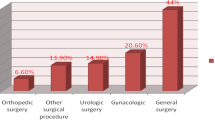
The data were collected from 280 patients. The mean age was 42.3 ± 14.7 years. The majority of the patients (61.8%) were scheduled for surgeries in governmental hospitals. Of the patients, 152 (54.3%) were female, 142 (50.7%) were less than 42 years old, 73 (26.1%) were single, 83 (29.6%) had a university education, 138 (49.3%) were currently employed, and 166 (59.3%) lived in urban areas. The majority of the patients reported moderate satisfaction with their household income, social life, and religious commitment. Of the patients, 175 (62.5%) had chronic diseases, 206 (73.6%) were scheduled to be operated on within 24 h, 239 (85.4%) were scheduled to receive general or regional anesthesia, 194 (69.3%) have had previous surgeries, 27 (9.6%) have had surgical complications, and 84 (30.0%) were scheduled to receive general surgery. The detailed demographic, clinical, and surgical variables of the patients are shown in Table 1.
APAIS scores
The mean APAIS total score was 13.6 ± 5.9, the mean APAIS anxiety domain score was 8.3 ± 4.3, and the mean APAIS need for information domain was 1.6 ± 0.50. Of the patients, 76 (27.1%) had high anxiety and 160 (57.1%) expressed a high need for information. The detailed responses of the patients are shown in Table 2.
Association between APAIS scores with demographic, clinical, and surgical variables of the patients
The t tests, ANOVA, chi-square, and Fisher’s exact tests showed that APAIS total and APAIS anxiety scores were significantly higher for the patients who were female, younger than 42 years, married, employed, had chronic diseases, scheduled to be operated on within 24 h, scheduled to receive general or regional anesthesia, had experienced surgical complications, and were scheduled to receive either obstetrical/gynecological, ophthalmological, general, or ear, nose, and throat operation. On the other hand, the APAIS need for information scores were significantly higher for patients who were female, scheduled to be operated on within 24 h, scheduled to receive general or regional anesthesia, whose surgery would be performed in a governmental hospital, and who were scheduled to receive ophthalmological operation. Differences in APAIS scores are shown in Supplementary Table S1 and associations between demographic, clinical, and surgical variables of the patients with anxiety and need for information categories are shown in Supplementary Table S2.
To control potentially confounding factors, the variables that were significantly associated in the t tests and ANOVA were included in multiple linear regression models. The models showed that higher APAIS total scores were predicted by being female, scheduled to be operated on within 24 h, and having experienced surgical complications. The higher APAIS anxiety scores were predicted by being female, having chronic diseases, being scheduled to be operated on within 24 h, and having experienced surgical complications. On the other hand, higher APAIS need for information scores were predicted by being scheduled to be operated on within 24 h and operated in a governmental hospital. Details of the multiple linear regression are shown in Table 3.
To control potentially confounding factors, the variables that were significantly associated in the Chi-square or Fisher’s exact tests were included in multivariate logistic regression models. Female patients were 2.89 times (95% CI 1.44–5.81) more likely to express high anxiety compared to male patients. On the other hand, patients to be operated within 24 h, scheduled to receive general or regional anesthesia, and those to be operated in governmental hospitals were 2.04-times (95% CI 1.15–3.60), 2.36-times (95% CI 1.14–4.88), and 2.08-times (1.24–3.50) compared to those who would be operated after 24 h, scheduled to receive local anesthesia, and those to be operated in private hospitals. Details of the multivariate logistic regression models are shown in Table 4.
STAIS-5/STAIT-5 scores
The mean STAIS-5 score was 10.0 ± 4.2 and the mean STAIT-5 was 10.3 ± 3.8. Of the patients, 140 (50.0%) had high state anxiety and 56 (20.0%) had high trait anxiety. The detailed responses of the patients are shown in Table 5.
Association between STAIS-5 and STAIT-5 scores with demographic, clinical, and surgical variables of the patients
The t tests, ANOVA, chi-square, and Fisher’s exact tests showed that STAIS-5 scores were significantly higher for patients who were female, younger than 42 years, married, employed, scheduled to be operated on within 24 h, and scheduled to receive either obstetrical/gynecological, ophthalmological, general, or ear, nose, and throat operations. On the other hand, the STAIT-5 scores were significantly higher for patients who were female, scheduled to receive general or regional anesthesia, and scheduled to receive either obstetrical/gynecological, cardiac surgery/interventions, ophthalmological, general, or ear, nose, and throat operations. Differences in STAIS-5 and STAIT-5 scores are shown in Supplementary Table S3 and associations between demographic, clinical, and surgical variables of the patients with anxiety and need for information categories are shown in Supplementary Table S4.
To control potentially confounding factors, the variables that were significantly associated in the t-tests and ANOVA were included in multiple linear regression models. The models showed that higher STAIS-5 scores were predicted by being female, younger than 42 years, and scheduled to be operated on within 24 h. On the other hand, higher STAIT-5 scores were predicted by being female. Details of the multiple linear regression are shown in Table 6.
To control potentially confounding factors, the variables that were significantly associated in the Chi-square or Fisher’s exact tests were included in multivariate logistic regression models. Patients who were female, younger than 42 years, and married were 2.61-times (95% CI 1.53–4.46), 1.90-times (95% CI 1.14–3.15), and 2.02-times (95% CI 1.11–3.66) more likely to express high state anxiety compared male, 42 years and older, and single patients, respectively. On the other hand, the patients who were female and those who were younger than 42 years were 1.99-times (95% CI 1.06–3.71) and 1.95-times (95% CI 1.06–3.60) more likely to express high trait anxiety compared to male and 42 years and older patients, respectively. Details of the multivariate logistic regression models are shown in Table 7.
Correlation between APAIS total, APAIS anxiety, APAIS need for information, STAIS-5, and STAIT-5 scores
There was a strong and positive correlation between APAIS total scores with APAIS anxiety scores (Pearson’s r = 0.90, p value < 0.001), and APAIS need for information scores (Pearson’s r = 0.74, p value < 0.001). On the other hand, there was a moderate and positive correlation between APAIS total scores and STAIS-5 scores (Pearson’s r = 0.60, p value < 0.001) and STAIT-5 scores (Pearson’s r = 0.41, p value < 0.001). There was a moderate correlation between APAIS anxiety scores and APAIS need for information scores (Pearson’s r = 0.39, p value < 0.001), STAIS-5 scores (Pearson’s r = 0.65, p value < 0.001) and STAIT-5 scores (Pearson’s r = 0.40, p value < 0.001). Similarly, there was a weak and positive correlation between APAIS need for information scores and STAIS-5 scores (Pearson’s r = 0.28, p value < 0.001) and STAIT-5 scores (Pearson’s r = 0.27, p value < 0.001). Moreover, there was a moderate and positive correlation between STAIS-5 scores and STAIT-5 scores (Pearson’s r = 0.46, p value < 0.001).
Discussion
Improving the care of patients in perioperative care has been prioritized in different healthcare systems around the world (Tola et al. 2021). For the first time, this study assessed the prevalence of perioperative anxiety among patients scheduled for surgical operations/interventions under anesthesia in Palestine. Additionally, the study identified the factors associated with higher anxiety. The findings of this study could be informative to decision and policymakers in healthcare authorities, anesthesiologists, and other providers of perioperative care who might need to design and implement measures to reduce preoperative anxiety and improve perioperative care in developing countries.
Using the APAIS scale, the prevalence of high preoperative anxiety was 27.1%. On the other hand, the prevalence of a high need for information was 57.1%. Moreover, the prevalence of high state anxiety was 50% and the prevalence of high trait anxiety was 20%. Recent systematic reviews reported that the prevalence rates of preoperative anxiety ranged from 17 to 89% (Bedaso et al. 2022; Oteri et al. 2021; Friedrich et al. 2022). The prevalence rate reported in this study was comparable to that reported in a recent large-scale multicenter study in China despite using a different scale to measure preoperative anxiety (Li et al. 2021). These findings were not surprising as the different scales measured the same constructs. In this study, scores obtained in the APAIS, STAIS-5, and STAIT-5 correlated positively. On the other hand, the prevalence of preoperative anxiety reported in this study was less than that reported in a recent study in Germany (Aust et al. 2018). Similarly, the prevalence rate reported in this study was lower than the reported global pooled rate of 48% (Friedrich et al. 2022). Another systematic review with meta-analysis reported a prevalence rate of preoperative anxiety of 55.7% in low- and middle-income countries (Bedaso et al. 2022). Taken together, these findings indicate that the prevalence rate of preoperative anxiety can vary significantly by the tools used to measure preoperative anxiety as well as patient- and healthcare-system-related factors (Bedaso et al. 2022; Aust et al. 2018; Gürler et al. 2022; Yu et al. 2022; Friedrich et al. 2022). Therefore, decision and policymakers need to consider the tools used to assess preoperative anxiety as well as the patient- and healthcare-system-related factors when interpreting and considering prevalence rates of preoperative anxiety.
In this study, preoperative anxiety scores were higher for female patients. These findings were consistent with those reported in previous studies that were conducted in different healthcare systems (Bedaso et al. 2022; Navarro-Gastón and Munuera-Martínez 2020; Yu et al. 2022; Oteri et al. 2021; Friedrich et al. 2022). Probably, anesthesiologists and other providers of perioperative care need to consider the sex of the patient when planning preoperative counseling. Additionally, the findings of this study showed that patients who had chronic diseases reported higher anxiety compared to those who did not have chronic diseases. These findings were not surprising because it is well-established that chronic diseases can deteriorate the outcomes of surgical interventions. A recent study that analyzed data from the English National Health System showed that the presence of chronic disease was associated with a 10 times higher risk of postoperative mortality among surgical patients (Fowler et al. 2022). Probably, patients with chronic diseases feared death or the occurrence of postoperative complications as a result of their pre-existing health conditions. Therefore, decision-makers, anesthesiologists, and other providers of perioperative care should consider providing tailored counseling to patients with chronic diseases. Moreover, having experienced surgical complications was a predictor of higher anxiety among preoperative patients. These findings were consistent with those reported in previous studies (Li et al. 2021; Friedrich et al. 2022). These studies showed that higher anxiety was associated with the degree of surgical invasiveness. Taken together, providers of perioperative care should provide more information to patients who have had surgical complications and the measures that would be taken to avoid the occurrence of these complications. Again, this study showed that anxiety increased as the scheduled operation approached. These findings indicate that providers of perioperative care should intensify measures to reduce preoperative anxiety in the hours that precede the surgical intervention. Previous studies have shown that some audiovisual interventions were effective in reducing preoperative anxiety (Chow et al. 2016). Anesthesiologists and other providers of perioperative care might use effective interventions to reduce preoperative anxiety.
Strengths and limitations
The findings of this study might be interpreted after considering the following strengths and limitations. First, this is the first study to assess the prevalence of preoperative anxiety among patients in the Palestinian healthcare system. Additionally, the study identified the predictors of high anxiety. The findings of this study might be used by decision and policymakers, anesthesiologists, and other providers of perioperative care to design and implement measures to reduce preoperative anxiety, especially among those with risk factors. Second, the patients included in this study were diversified in terms of demographic, clinical, and surgical variables. The study patients were recruited from different hospitals. This diversity should have improved the representativeness of the entire population of preoperative patients and should have improved the external validity of the study. Third, anxiety was measured using different validated and reliable scales. These scales assessed the different domains of anxiety. This should have added depth and width to the findings reported in this study. Fourth, the questionnaire was tested in a pilot study before it was used in the larger study. Additionally, the test–retest reliability and internal consistency were used as diagnostics for the suitability of the questionnaire. These steps should have ensured the generation of valid and reliable findings.
On the other hand, this study had some limitations. First, this study was conducted using an observational design. The use of an intervention to reduce preoperative anxiety should have produced more interesting findings. Second, the sample size was calculated using a 90% CI. A larger sample size could have produced more reliable findings. Third, the results of this study were self-reported as in this study no somatic signs and symptoms were used to assess anxious patients. Fourth, desirability bias could not be excluded as some patients might have tended to provide more positive answers or hide their anxiety. In this case, the prevalence of preoperative anxiety might have been underestimated. Finally, this study was conducted in Palestine. Studies conducted in more than one country should report more interesting findings.
Conclusion
Preoperative anxiety was prevalent among patients scheduled for surgical operations in Palestinian hospitals. Anesthesiologists and other providers of perioperative care should screen preoperative patients who are female, have chronic diseases, are scheduled to be operated on within 24 h, and having had experienced surgical complications for preoperative anxiety. The findings reported in this study could be used by decision and policymakers in developing countries to plan, design, and implement effective interventions to reduce preoperative anxiety among surgical patients. More studies are still needed to investigate the effects of the implemented measures on the prevalence of preoperative anxiety.
Availability of data and materials
All data relevant to this study were included in the results or provided as supplementary materials with this manuscript.
References
Abate SM, Chekol YA, Basu B. Global prevalence and determinants of preoperative anxiety among surgical patients: a systematic review and meta-analysis. Int J Surg Open. 2020;25:6–16.
Aust H, Eberhart L, Sturm T, Schuster M, Nestoriuc Y, Brehm F, Rüsch D. A cross-sectional study on preoperative anxiety in adults. J Psychosom Res. 2018;111:133–9.
Ayele B, Tadesse M, Tilahun R, Nega B. Translation of the Amsterdam Preoperative Anxiety and Information Score (APAIS) into the Amharic Version and Its Validation for Evaluation of Preoperative Anxiety. Ethiop J Health Sci. 2021;31(2):349–58.
Bedaso A, Ayalew M. Preoperative anxiety among adult patients undergoing elective surgery: a prospective survey at a general hospital in Ethiopia. Patient Saf Surg. 2019;13(1):1–8.
Bedaso A, Mekonnen N, Duko B. Prevalence and factors associated with preoperative anxiety among patients undergoing surgery in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open. 2022;12(3):e058187.
Chow CH, Van Lieshout RJ, Schmidt LA, Dobson KG, Buckley N. Systematic review: audiovisual interventions for reducing preoperative anxiety in children undergoing elective surgery. J Pediatr Psychol. 2016;41(2):182–203.
Eberhart L, Aust H, Schuster M, Sturm T, Gehling M, Euteneuer F, Rüsch D. Preoperative anxiety in adults - a cross-sectional study on specific fears and risk factors. BMC Psychiatry. 2020;20(1):140.
Fentie Y, Yetneberk T, Gelaw M. Preoperative anxiety and its associated factors among women undergoing elective caesarean delivery: a cross-sectional study. BMC Pregnancy Childbirth. 2022;22(1):648.
Fernández-Donaire L, Romero-Sánchez JM, Paloma-Castro O, Boixader-Estévez F, Porcel-Gálvez AM. The nursing diagnosis of “death anxiety”: content validation by experts. Int J Nurs Knowl. 2019;30(4):211–8.
Fowler AJ, Wahedally MAH, Abbott TEF, Smuk M, Prowle JR, Pearse RM, Cromwell DA. Death after surgery among patients with chronic disease: prospective study of routinely collected data in the English NHS. Br J Anaesth. 2022;128(2):333–42.
Friedrich S, Reis S, Meybohm P, Kranke P. Preoperative anxiety. Curr Opin Anaesthesiol. 2022;35(6):674–8.
Gürler H, Yılmaz M, Türk KE. Preoperative anxiety levels in surgical patients: a comparison of three different scale scores. J Perianesth Nurs. 2022;37(1):69–74.
Khalili N, Karvandian K, Ardebili HE, Eftekhar N, Nabavian O. Predictive factors of preoperative anxiety in the anesthesia clinic: a survey of 231 surgical candidates. Arch Anesthesiol Crit Care. 2019;5(4):122–7.
Kuzminskaitė V, Kaklauskaitė J, Petkevičiūtė J. Incidence and features of preoperative anxiety in patients undergoing elective non-cardiac surgery. Acta Medica Lituanica. 2019;26(1):93.
Li XR, Zhang WH, Williams JP, Li T, Yuan JH, Du Y, Liu JD, Wu Z, Xiao ZY, Zhang R, et al. A multicenter survey of perioperative anxiety in China: Pre- and postoperative associations. J Psychosom Res. 2021;147:110528.
Liu W, Xu R, Jia J, Shen Y, Li W, Bo L. Research progress on risk factors of preoperative anxiety in children: a scoping review. Int J Environ Res Public Health. 2022;19(16):9828.
Mariyam Z, Safdar L, Fatima S, Zaheer J. Preoperative anxiety and fear of anesthesia in patients admitted in tertiary care hospitals of Rawalpindi. J Rawalpindi Med College. 2020;24(1):52–8.
Moerman N, van Dam FSAM, Muller MJ, Oosting H. The Amsterdam Preoperative Anxiety and Information Scale (APAIS). Anesth Analg. 1996;82(3):445–51.
Moura LA, Dias IM, Pereira LV. Prevalence and factors associated with preoperative anxiety in children aged 5–12 years. Rev Lat Am Enfermagem. 2016;24:e2708.
Navarro-Gastón D, Munuera-Martínez PV. Prevalence of Preoperative Anxiety and Its Relationship with Postoperative Pain in Foot Nail Surgery: A Cross-Sectional Study. Int J Environ Res Public Health. 2020;17(12):4481.
Oteri V, Martinelli A, Crivellaro E, Gigli F. The impact of preoperative anxiety on patients undergoing brain surgery: a systematic review. Neurosurg Rev. 2021;44(6):3047–57.
Tola YO, Chow KM, Liang W. Effects of non-pharmacological interventions on preoperative anxiety and postoperative pain in patients undergoing breast cancer surgery: A systematic review. J Clin Nurs. 2021;30(23–24):3369–84.
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4(10):e297.
Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR, Gawande AA. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372(9633):139–44.
Yu J, Zhang Y, Yu T, Mi W, Yao S, Wang Z, Xu L, Huang Y. Preoperative anxiety in Chinese adult patients undergoing elective surgeries: a multicenter cross-sectional study. World J Surg. 2022;46(12):2927–38.
Zemła AJ, Nowicka-Sauer K, Jarmoszewicz K, Wera K, Batkiewicz S, Pietrzykowska M. Measures of preoperative anxiety. Anaesthesiol Intensive Ther. 2019;51(1):64–9.
Zsido AN, Teleki SA, Csokasi K, Rozsa S, Bandi SA. Development of the short version of the spielberger state—trait anxiety inventory. Psychiatry Res. 2020;291:113223.
Acknowledgements
The authors would like to thank the patients who participated in the study. An-Najah National University is acknowledged for making this study possible.
Funding
This study did not receive any specific funding.
Author information
Authors and Affiliations
Contributions
RS, MJ, HH, IM, and HH were involved in the conception and design of the work, analysis, and interpretation of data, drafting, and final approval of the manuscript. MT, NA, and ZS were involved in the data acquisition, analysis, drafting of the work and final approval of the version to be published. The authors read and approved the final manuscript.
Authors’ information
Ramzi Shawahna, Associate Professor, Department of Physiology, Pharmacology and Toxicology, Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine, Clinical Research Center, An-Najah National University Hospital, Nablus, Palestine. Mohammad Jaber, Hatim Hijaz, and Iyad Maqboul were Assistant Professors, Department of Medicine, Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine, An-Najah National University Hospital, Nablus, Palestine. Marah Tebi, Nada Al-Sayed Ahmed, and Ziyad Shabello, Doctor of Medicine candidates, Department of Medicine, Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted in compliance with the international ethical standards in the Declaration of Helsinki. The study received approval from the Institutional Review Board (IRB) of An-Najah National University (IRB protocol approval # Nov.3.2021). Approval was also obtained from the Office of Health Education of the Palestinian Ministry of Health. Written informed consent was obtained from each patient. The data collected were treated as confidential and were coded before analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table S1.
Differences in APAIS scores.
Additional file 2: Supplementary Table S2.
Associations between demographic, clinical, and surgical variables of the patients with APAIS anxiety and need for information categories.
Additional file 3: Supplementary Table S3.
Differences in STAIS-5 and STAIT-5 scores.
Additional file 4: Supplementary Table S4.
Associations between demographic, clinical, and surgical variables of the patients with STAIS-5 and STAIT-5 categories.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shawahna, R., Jaber, M., Maqboul, I. et al. Prevalence of preoperative anxiety among hospitalized patients in a developing country: a study of associated factors. Perioper Med 12, 47 (2023). https://doi.org/10.1186/s13741-023-00336-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13741-023-00336-w