Abstract
Background
With a high mortality of 12.6% of all cancer cases, colorectal cancer (CRC) accounts for substantial burden of disease in Europe. In the past decade, more and more countries have introduced organized colorectal cancer screening programs, making systematic screening available to entire segments of a population, typically based on routine stool tests and/or colonoscopy. While the effectiveness of organized screening in reducing CRC incidence and mortality has been confirmed, studies continuously report persistent program implementation challenges. This systematic review will synthesize the literature on organized CRC screening programs. Its aim is to understand what is currently known about the barriers and facilitators that influence the implementation of these programs and about the implementation strategies used to navigate these determinants.
Methods
A systematic review of primary studies of any research design will be conducted. CENTRAL, CINAHL, EMBASE, International Clinical Trials Registry Platform, MEDLINE, PsycINFO, and Scopus will be searched. Websites of (non-)government health care organizations and websites of organizations affiliated with authors of included studies will be screened for unpublished evaluation reports. Existing organized CRC screening programs will be contacted with a request to share program-specific grey literature. Two researchers will independently screen each publication in two rounds for eligibility. Included studies will focus on adult populations involved in the implementation of organized CRC screening programs and contain information about implementation determinants/ strategies. Publications will be assessed for their risk of bias. Data extraction will include study aim, design, location, setting, sample, methods, and measures; program characteristics; implementation stage, framework, determinants, strategies, and outcomes; and service and other outcome information. Findings will be synthesized narratively using the three stages of thematic synthesis.
Discussion
With its sole focus on the implementation of organized CRC screening programs, this review will help to fill a central knowledge gap in the literature on colorectal cancer screening. Its findings can inform the decision-making in policy and practice needed to prioritize resources for establishing new and maintaining existing programs in the future.
Systematic review registration
PROSPERO (CRD42022306580).
Similar content being viewed by others
Background
With more than 500,000 yearly cases and a mortality of 12.6% of all cancer cases, colorectal cancer (CRC) accounts for a substantial burden of disease in Europe [1, 2]. A recent study estimated the costs of this burden in Europe, attributed to loss of productivity and the provision of different health care services, to have been €19.1 billion in 2015 [3]. Lifestyle related factors such as an unhealthy diet and sedentary behavior increase the risk of developing colorectal cancer, which typically begins with adenoma detectable by colonoscopy and progresses to invasive cancer over the course of 10 to 15 years [4, 5]. Based on these characteristics, it is not surprising that the pro-active, systematic, and early detection of colorectal cancer—rather than its re-active treatment—has become a priority on health policy agendas in and across European countries. In February 2021, the European Commission presented Europe's Beating Cancer Plan, including the goal to develop a new EU Cancer Screening Scheme with the aim to ensure that 90% of the eligible target population in Europe is offered a colorectal cancer screening by 2025 [6]. An additional driver of this push for enhancing preventive colorectal cancer services in Europe has been the realization that the target uptake rate of 65% among those eligible for a CRC screening—typically those aged 50 to 74—has not been reached [7]. This was the case despite remarkable progress in increasing the number of organized CRC screening programs across Europe, which are now available in 20 out of 27 countries in the European Union (EU) [6].
Organized screening programs offer systematic screening, typically based on different types of routine stool tests and/or colonoscopy, to entire segments of the population of a country or a region. Where organized screening programs do not exist, opportunistic screening is often used, i.e., screening that is not systematically monitored and which depends on primary care physician recommendations or patient requests [8]. Further characteristics of organized programs are: explicit policies that outline program offerings; a clearly defined target population; and the specification of guidelines for program administration, including instructions for implementing, monitoring, and assuring program quality, and the follow up of patients with positive screening results [5]. While the effectiveness of organized screening in reducing CRC incidence [2] and mortality [9,10,11] has been confirmed, studies continuously report persistent implementation challenges preventing organized CRC screening from reaching its full preventative potential. These include patient-related barriers to participating in screening [12,13,14]; provider-related barriers to promoting and engaging in screening [15, 16]; and system-related barriers to establishing and maintaining screening programs [15,16,17]. As a consequence of these challenges, public health authorities and health care professionals implementing cancer screening programs may not achieve the goals that they have set for the use of this otherwise research-supported intervention. This is especially critical for organized, i.e., publicly funded screening programs. The legitimacy of these programs in the public eye will depend on their demonstrated efficiency and effectiveness, and in the absence hereof funding may be discontinued, and evidence-based practice diminished [18, 19].
Therefore, there is an urgent need to better understand current best knowledge on the implementation of organized CRC screening programs. Few scholars have aimed to synthesize this knowledge base for organized screening programs only [14, 16, 20,21,22], and of these, none have solely focused on the entire range of implementation conditions for colorectal cancer screening programs—despite important differences in these conditions existing for organized screening programs in general and for organized colorectal cancer screening programs in particular. Organized screening programs in general require the use of population registers and monitoring systems, they depend on substantial negotiation with and joint engagement of multiple groups of health care professionals, and on the systematic development of capacity to maintain program activities over time. The multiple screening modalities available as part of many organized CRC screening programs add an additional layer of implementation complexity that differentiates this type of cancer screening from others. While programs may aim at reducing this complexity by only offering one screening modality, opportunistic screening based on alternative modalities continues to occur outside of programs [15, 23]. Furthermore, CRC screening modalities are often viewed as unattractive by eligible program participants making it particularly challenging to build and maintain program reach [14, 24].
In the field of implementation science, models and methods have been developed to systematically examine implementation in health care. Among these, implementation determinants and strategies are central concepts. Implementation determinants are the barriers and facilitators that, at different levels of an implementing system, can influence the outcomes of an implementation [25, 26]. To address and/or navigate these, health care professionals and their organizations depend on purposely crafted implementation strategies, i.e., methods and activities used to enhance the uptake, implementation and sustainment of evidenced interventions and services [27]. They are the means with which program robustness can be established, and obstacles and challenges to CRC screening program implementation be overcome [21, 28]. Ideally, implementation strategies are selected and designed prospectively, based on both a detailed analysis of anticipated implementation determinants and on knowledge about which strategies are best suited to target these determinants. This knowledge is still lacking and has led to calls for enhancing implementation strategy research in health and human services [29, 30]. In the field of CRC screening, this research has grown in recent years, with an increasing number of studies examining the use of implementation strategies [31,32,33], their feasibility [34, 35] or ability to improve program outcomes [36, 37]. However, due to a lack of synthesis, it is unclear to what degree this slowly accumulating knowledge base is related to organized CRC screening programs, and how it can contribute to improving their implementation.
Therefore, the aim of this review is to synthesize the literature on implementing organized colorectal cancer screening programs developed for adult populations at average risk for colorectal cancer and to examine, what is currently known about
-
The barriers and facilitators, i.e., determinants, that influence the implementation of these programs in Europe, and about
-
The implementation strategies used to navigate these determinants.
Methods/design
This systematic review has been registered with the International Prospective Register of Systematic Reviews (PROSPERO, https://www.crd.york.ac.uk/prospero/, registration number: CRD42022306580). The review protocol is being reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocol (PRISMA-P) checklist [38], which is available as Additional file 1.
The review is an element of the research project Improving Organized Colorectal Cancer Screening: An Implementation science study (OCCSI). Funded by Swiss Cancer Research, and based on a mixed-methods design, OCCSI aims to build an understanding of current practices in implementing organized CRC screening programs in Switzerland. Enforced by a decentralized political structure, Swiss organized CRC screening programs are established at a cantonal level. Since the development of the first Swiss organized CRC screening program in 2013, about half of all 26 Swiss cantons have followedFootnote 1. The majority of these programs were established in the years since 2019 and are in early stages of their implementation. This review will contribute to building the knowledge base on how to optimize this implementation and that of further programs to be established in Switzerland in the future.
The review is designed as a systematic integrative review (SIR), building on the SIR framework by Whittemore and Knafl [39], allowing for the inclusion of quantitative as well as qualitative study designs.
Criteria for considering studies for this review
Criteria for selecting studies for this review were developed based on the SPIDER tool [40] and include: sample, phenomenon of interest, design, evaluation, and research type.
Sample
Studies focused on adult populations who are involved in the implementation of European organized colorectal cancer screening programs developed for individuals at average risk for colorectal cancer will be included in this systematic review. Among relevant study populations are, for example, program participants/recipients, health care professionals such as general practitioners or gastroenterologists, program administrators/coordinators, leaders, policy developers, politicians, funders, or individuals in other roles. “Implementation” refers to any activities undertaken to establish, improve, or sustain an organized CRC screening program. European countries are those that are considered part of the European Region of the World Health Organization (WHO)Footnote 2.
Phenomenon of interest
The characteristics of organized CRC screening programs developed by the International Agency for Research on Cancer [41] will be applied. These include for screening to be organized at a national or regional level, and to be based on an explicit policy. They also imply for a central team to be responsible for organizing the program, the systematic participant invitation based on prespecified target populations, and the health care services provided within the program. The existence of a structure for program quality assurance is a further characteristic.
Design
Published primary studies, i.e., studies reporting original, new data, of any research design will be eligible for this review.
Evaluation
Information about (a) determinants, i.e., factors perceived or empirically reported to influence the implementation of organized CRC screening programs and (b) the strategies used to navigate these determinants are the central findings of interest for this review. Implementation strategies will be defined as the methods or techniques used to enhance the adoption, implementation, or sustainment of organized CRC screening programs [27].
Determinants may influence program implementation in positive or negative direction and affect, e.g., program reach, engagement of health care professionals, program implementation speed, funding availability or security, and other implementation characteristics and outcomes. In identifying strategies, any activities aimed at navigating, removing, or utilizing these determinants will be included. Information about determinants and strategies may be reported as perceptions, characteristics, views, experiences, or in other either qualitative or quantitative formats.
Research type
This review will include qualitative, quantitative, and mixed methods peer-reviewed primary studies. Grey literature will be limited to evaluation reports issued by government and non-government organizations.
Information sources and search strategy
The databases below will be searched for studies published from January 2000 onward. This cut-off year was chosen based on a review of the commencement years for organized CRC screening programs in Europe listed in the International Agency for Research on Cancer’s (IARC) Handbook on Colorectal Cancer Screening [41]. This review showed that all but one program had been established after 2000. The exception was Italy, where organized CRC screening began in Florence in 1982. All other regions commenced screening in 2000 or later, confirming that the central evidence base in focus of this review would be included in studies published in or after this year.
-
Cochrane Central Register of Controlled Trials (CENTRAL)
-
Cumulative Index to Nursing and Allied Health Literature (CINAHL)
-
EMBASE
-
International Clinical Trials Registry Platform (ICTRP)
-
MEDLINE
-
PsycINFO
-
Scopus
Search strategies to be used are outlined in Additional file 2.
Supplementary searches
Given the central position of (non-)government health care organizations in initiating and implementing organized colorectal cancer screening programs in Europe, websites of organizations known to be engaged in promoting and scaling cancer screening efforts will be screened for unpublished evaluation reports. The final list of websites will include but not be limited to:
-
Association of European Cancer Leagues
-
Cancer Research UK
-
Digestive Cancers Europe (DICE)
-
European Cancer Organization
-
European Cancer Patient Coalition
-
International Agency for Research on Cancer (IARC)
-
Innovative Partnership for Action Against Cancer (iPAAC)
-
National Institute for Health and Care Excellence (NICE)
-
Medical Research Council (MRC)
-
UK National Screening Committee (UK NCS)
-
World Endoscopy Organization (WEO)
Websites of organizations affiliated with authors of included studies will also be searched for eligible publications. Furthermore, reference lists of previous systematic reviews identified through the search process together with reference lists of included studies will be screened for relevant literature. Finally, existing organized CRC screening programs [41] will be contacted with a request to share program-specific grey literature.
Language of publication
Studies written in Danish, English, French, German, Italian, Norwegian, Spanish, or Swedish will be included.
Data collection and management
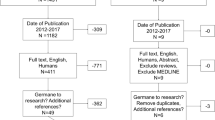
Following the upload of all references to the online systematic review application CovidenceFootnote 3, all screening work will occur on this platform. A PRISMA flowchart will be developed to summarize the inputs and results of each stage of the screening process.
Study selection
Two researchers will independently screen each publication in two rounds, one focused on titles and abstracts and one on full texts. Both rounds will involve the testing of a screening protocol, guiding the decision-making of individual researchers. Researchers will test each protocol independently on a sample of ten studies, compare results and discuss (a) the degree to which the protocol requires refinement, and (b) final decision-making on the respective study. Protocols will then be refined and prepared for use with the remaining studies. Individual researchers will apply eligibility criteria independently and be blind to each other’s decisions about the in- or exclusion of publications. Disagreements between their individual judgements will be resolved by consensus or a third researcher.
Quality appraisal
All included publications will be assessed for their risk of bias using checklists developed by JBIFootnote 4 for different study designs, including randomized controlled trials, qualitative, and economic evaluations.
Data extraction
Pairs of researchers will independently extract data from 10% of the studies. Data extraction results will be compared, and disagreements discussed in our research team to achieve full consensus on how to approach data extraction among all research team members.
Data from the remaining 90% of the studies will be extracted independently by one researcher, and the extraction checked, and quality assured by the lead author. The following information will be extracted: study aim; study design; location; methods; study settings; study sample; CRC screening program characteristics; implementation stage; implementation framework use; study measures; implementation determinant information; implementation strategy information; implementation, service and other outcomes that are related to determinants and/or strategies; information needed to conduct risk of bias assessment (design dependent). Implementation strategy information extraction will be based on the “Prerequisites to Measuring Implementation Strategies” (PMIS) framework [27], recommending for implementation strategies to be specified by name, included components, actors, actions, action targets, temporality, dose, implementation outcome targets, and justification. To enable the coding process described below, both implementation determinant and strategy information will be extracted in the form of entire sentences and/or text sections included in original articles.
Should missing data be detected during data extraction, lead authors of papers will be contacted for unreported data and/or any other additional details of interest to the research team.
Data analysis
Findings will be synthesized narratively using the three stages of thematic synthesis [42]: (1) Line by line coding; (2) the development of descriptive themes; and [3] the generation of analytical themes.
As part of the line-by-line coding of extracted information, information on the determinants to and strategies for implementing organized CRC screening programs will be coded using both deductive and inductive coding. The deductive coding of determinants will be guided by the Consolidated Framework for Implementation Research, CFIR [25, 43] and that of implementation strategies by the Expert Recommendations for Implementing Change (ERIC) compilation of implementation strategies [44]. The CFIR is a framework developed to build the knowledge base on quality implementation of complex interventions and contains five domains of factors potentially influencing implementation processes. These include the intervention, the individuals involved in an implementation, the inner and outer setting of the implementation, and the implementation process. The CFIR has been widely used by scholars to categorize and analyze determinants to colorectal cancer screening efforts, both as part of systematic reviews [32, 45, 46] and of primary studies [47,48,49]. For this review, a recently updated version of the CFIR will be used [43].
The ERIC compilation of implementation strategies [44] includes the description of 73 implementation strategies commonly acknowledged as relevant activities that, when used separately or in combination, can facilitate the integration of evidenced interventions into routine health care and prevention. While scholars have pointed to limitations in using the ERIC compilation as a coding tool [50, 51] due to a lack of granularity characterizing some of its strategies, it represents the most comprehensive and varied list of implementation strategies available for coding purposes. It has been applied in multiple health care focused systematic reviews [52,53,54]. The parallel use of the PMIS framework [27] will further ensure that implementation strategies are thoroughly categorized and analyzed. Furthermore, the coding of strategies and determinants will also be inductive, allowing researchers to register any information not aligned with framework-based coding categories under the category “other”. Finally, researchers will be asked to develop brief memos of coding challenges related to framework use as they emerge, such that these can be addressed during regular team meetings.
Based on these considerations, a coding protocol will be developed. The coding protocol will be piloted by all members of the research team on a sample of five different studies. Researchers will identify potential limitations and needs for improvement individually and discuss these in a review team meeting to develop concrete steps for adjusting the coding protocol. The revised protocol will then be used for the coding of all included studies, with researchers having access to ad hoc support from other review team members and weekly research team meetings serving as an additional forum for problem solving around coding. These meetings will also be used to discuss inductive codes to enable decisions on whether to add new codes, and how to handle previously coded manuscripts.
To develop descriptive themes, two researchers will independently review the textual information retrieved for each code and develop descriptive themes by, e.g., identifying commonalities and differences in the ways in which implementation determinants and the use of implementation strategies are described; and by identifying how, e.g., different determinants, different strategies, and determinants and strategies are interlinked with each other. Descriptive themes will be based on the semantic level of texts, i.e., closely related to the language used in text excerpts. A summary of descriptive themes will be discussed among all members of the research team in two rounds—once at a preliminary stage to retrieve early input, and a second time to refine a more consolidated list of descriptive themes prior to their finalization.
In developing analytical themes, the research team will move to the latent level of meaning included in and across studies and build shared understandings of, e.g.,
-
Commonalities in determinants to the implementation of organized CRC screening programs and how they impact this implementation
-
Characteristics of implementation strategies used in the implementation of organized CRC screening programs
-
Commonalities and differences in strategies selected to address specific determinants
-
Linkages between determinants only, strategies only and determinants and strategies
-
Gaps in the current knowledge base for the implementation of organized CRC screening programs
Preliminary ideas for analytical themes will be mirrored in descriptive themes and discussed in the research team also considering review findings and the wider literature on organized CRC screening program implementation. Based on this discussion, two researchers will draft a first list of potential analytical themes for further input from and discussion among all review team members. This will lead to further refinement and the finalization of all analytical themes.
Involvement of program implementers
Organized Swiss colorectal cancer screening programs are at the center of the overarching OCCSI study, in which this review is embedded. Through two open, one-hour online meetings, individuals actively involved in implementing these programs will therefore be invited to participate in discussions about descriptive and analytic themes. Meeting invites will be issued twice—once when a first list of descriptive themes exists, and once at the outset of developing analytic themes—and e-mailed directly to the research team’s network of CRC screening program stakeholders. These meetings will be aimed at helping the research team understand program implementers’ perspective on preliminary review findings, thereby ensuring that these can be interpreted with these review users in mind. At a later stage of the review process, stakeholders will also be asked for feedback and input on the development of strategies for the wider dissemination of review findings.
Discussion
In a new guide document, WHO Europe characterizes CRC screening as one of the “best buys” that exist in cancer screening [55]. The organization also recommends countries to build their screening efforts on organized programs with a capacity to reach at least 70% of an eligible population. This emphasizes the relevance of filling a gap in the literature on colorectal cancer screening by synthesizing the knowledge about how this type of program has been implemented thus far. Such synthesis can help to inform the decision-making in policy and practice needed to prioritize resources for establishing new and maintaining existing programs in the future.
One strength of this review will be to solely focus on studies conducted in the context of organized European CRC screening programs, thereby filtering out knowledge that has been created in contexts of opportunistic screening and/or of research trials that may involve systematic screening efforts but at a much smaller scale than that of entire populations in a region, state, or nation. A further strength is that all review stages will be informed by an implementation science-based perspective, reflected in the use of clearly delineated concepts—implementation determinants and strategies—and frameworks supporting their analysis in the context of CRC screening. In combination with the inclusion of a broad range of knowledge types—qualitative as well as quantitative—this will allow for generating a much-needed knowledge base that currently is missing for the implementation of organized colorectal cancer screening programs.
It is also expected that the review team will encounter some limitations when conducting this review. First, a substantial number of existing organized CRC screening programs in Europe listed in the most recent version of the IARC Handbook on Colorectal Cancer Screening [41] have been established in the past 10–12 years, a period during which the field of implementation science also underwent considerable growth and development. This may limit the number of genuine implementation studies conducted of organized CRC screening programs—a limitation that we will address by consulting complementary grey literature existing in the public domain but not indexed in electronic databases. Second, with organized CRC screening programs being at the core of this review, significant heterogeneity could make synthesis difficult. Included studies will have been conducted in a broad range of countries, representing different policy contexts, welfare state regimes and health care systems, making it difficult to compare and synthesize findings. Furthermore, CRC screening programs presented may be at different stages of their implementation (with some being in, e.g., a pilot phase, and others reporting on multiple years of implementation experience) or include different program components (with some providing, e.g., different types of stool tests only, and others also including colonoscopies). In our data extraction, analysis, and synthesis, we will work to take these contextual differences into account and report on them as deemed relevant. Finally, the inclusion of a broad range of study designs in this review implies that—when presenting findings—small scale case studies are assigned the same weight as large-scale population research, potentially skewing results. To address this concern, we will provide detailed information about the evidence quality of studies, thereby allowing review users to put findings into perspective. Moreover, it is worth keeping in mind that this review pursues the explorative aim of understanding what is currently known about the implementation determinants and strategies related to organized CRC screening programs, making it relevant to consider the broadest possible range of evidence.
This breadth will allow for review findings to inform policy processes through the greatest possible variety in determinants and strategies that are relevant to consider when planning for program resources, design, and implementation. Simultaneously, review results will be usable in existing organized CRC program practice by identifying promising approaches to implementing and maintaining programs over time, providing decision-makers with information on which aspects of program practice may need particular effort, or ongoing adjustment and improvement. The findings from this review will therefore be disseminated in multiple forms, including scientific publication, conference presentations and targeted formats to be developed in collaboration with the stakeholders participating in the overarching study to which this review is linked.
Should protocol amendments be needed in the future, these will be registered in the PROSPERO repository and reported in the final review report.
Availability of data and materials
Not applicable.
Notes
An overview is available at https://www.swisscancerscreening.ch/de/angebote-in-ihrem-kanton
As listed on the WHO website at https://www.who.int/countries
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org
JBI’s repository of quality appraisal tools can be accessed here: https://jbi.global/critical-appraisal-tools
Abbreviations
- CFIR:
-
Consolidated Framework for Implementation Research
- CRC:
-
Colorectal Cancer
- ERIC:
-
Expert Recommendations for Implementing Change
- EU:
-
European Union
- IARC:
-
International Agency for Research on Cancer
- JBI:
-
Joanna Briggs Institute
- PMIS:
-
Prerequisites to Measuring Implementation Strategies
- WHO:
-
World Health Organization
References
Ferlay J, Colombet M, Soerjomataram I, Dyba T, Randi G, Bettio M, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer. 2018;103:356–87.
Cardoso R, Guo F, Heisser T, Hackl M, Ihle P, Schutter HD, et al. Colorectal cancer incidence, mortality, and stage distribution in European countries in the colorectal cancer screening era: an international population-based study. Lancet Oncol. 2021;22(7):1002–13.
Henderson RH, French D, Maughan T, Adams R, Allemani C, Minicozzi P, et al. The economic burden of colorectal cancer across Europe: a population-based cost-of-illness study. Lancet Gastroenterol Hepatol. 2021;6(9):709–22.
Keum N, Giovannucci E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroentero. 2019;16(12):713–32.
Schreuders EH, Ruco A, Rabeneck L, Schoen RE, Sung JJY, Young GP, et al. Colorectal cancer screening: a global overview of existing programmes. Gut. 2015;64(10):1637.
European Commission. Communication from the Commission to the European Parliament and the Council: Europe’s Beating Cancer Plan. European Commission; 2021. https://ec.europa.eu/health/sites/default/files/non_communicable_diseases/docs/eu_cancer-plan_en.pdf. Accessed 23 Feb 2023.
Senore C, Basu P, Anttila A, Ponti A, Tomatis M, Vale DB, et al. Performance of colorectal cancer screening in the European Union member states: data from the second European screening report. Gut. 2019;68(7):1232.
Dominitz JA, Levin TR. What is organized screening and what is its value? Gastrointest Endosc Clin North Am. 2020;30(3):393–411.
Levin TR, Corley DA, Jensen CD, Schottinger JE, Quinn VP, Zauber AG, et al. Effects of organized colorectal cancer screening on cancer incidence and mortality in a large community-based population. Gastroenterology. 2018;155(5):1383–1391.e5.
Gini A, Jansen EEL, Zielonke N, Meester RGS, Senore C, Anttila A, et al. Impact of colorectal cancer screening on cancer-specific mortality in Europe: a systematic review. Eur J Cancer. 2020;127:224–35.
Lin JS, Piper MA, Perdue LA, Rutter CM, Webber EM, O’Connor E, et al. Screening for colorectal cancer: Updated evidence report and systematic review for the US preventive services task force. JAMA. 2016;315(23):2576.
Clarke N, Sharp L, Osborne A, Kearney PM. Comparison of uptake of colorectal cancer screening based on Fecal Immunochemical Testing (FIT) in males and females: a systematic review and meta-analysis. Cancer Epidemiol Prev Biomarkers. 2015;24(1):39–47.
Honein-AbouHaidar GN, Kastner M, Vuong V, Perrier L, Daly C, Rabeneck L, et al. Systematic review and meta-study synthesis of qualitative studies evaluating facilitators and barriers to participation in colorectal cancer screening. Cancer Epidemiol Prev Biomarkers. 2016;25(6):907–17.
Dressler J, Johnsen AT, Madsen LJ, Rasmussen M, Jorgensen LN. Factors affecting patient adherence to publicly funded colorectal cancer screening programmes: a systematic review. Public Health. 2021;190:67–74.
Turnbull E, Priaulx J, van Ravesteyn NT, Heinävaara S, Siljander I, Senore C, et al. A health systems approach to identifying barriers to breast cancer screening programmes. Methodology and application in six European countries. Health Policy. 2018;122(11):1198–205.
Priaulx J, Turnbull E, Heijnsdijk E, Csanádi M, Senore C, de Koning HJ, et al. The influence of health systems on breast, cervical and colorectal cancer screening: an overview of systematic reviews using health systems and implementation research frameworks. J Health Serv Res Po. 2020;25(1):49–58.
Hernández-Leal MJ, Pérez-Lacasta MJ, Feijoo-Cid M, Ramos-García V, Carles-Lavila M, Group on behalf of the P, et al. Healthcare professionals’ behaviour regarding the implementation of shared decision-making in screening programmes: a systematic review. Patient Educ Couns. 2021;104(8):1933–44.
Flitcroft KL, Salkeld GP, Gillespie JA, Trevena LJ, Irwig LM. Fifteen years of bowel cancer screening policy in Australia: putting evidence into practice? Med J Aust. 2010;193(1):37–42.
Pienaar K, Petersen A, Bowman DM. Matters of fact and politics: generating expectations of cancer screening. Soc Sci Med. 2019;232:408–16.
Bongaerts TH, Büchner FL, Middelkoop BJ, Guicherit OR, Numans ME. Determinants of (non-)attendance at the Dutch cancer screening programmes: a systematic review. J Med Screen. 2020;27(3):121–9.
Brouwers MC, Vito CD, Bahirathan L, Carol A, Carroll JC, Cotterchio M, et al. Effective interventions to facilitate the uptake of breast, cervical and colorectal cancer screening: an implementation guideline. Implement Sci. 2011;6(1):112.
Lynge E, Törnberg S, von Karsa L, Segnan N, van Delden JJM. Determinants of successful implementation of population-based cancer screening programs. Eur J Cancer. 2012;48:743–8.
Rossi PG, Carrozzi G, Federici A, Mancuso P, Sampaolo L, Zappa M. Invitation coverage and participation in Italian cervical, breast and colorectal cancer screening programmes. J Med Screen. 2017;25(1):17–23.
Wools A, Dapper EA, de Leeuw JRJ. Colorectal cancer screening participation: a systematic review. Eur J Pub Health. 2016;26(1):158–68.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. https://doi.org/10.1186/1748-5908-4-50.
Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. Conceptualizing outcomes for use with the Consolidated Framework for Implementation Research (CFIR): the CFIR Outcomes Addendum. Implement Sci. 2022;17(1):7.
Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8:139. https://doi.org/10.1186/1748-5908-8-139.
Issaka RB, Avila P, Whitaker E, Bent S, Somsouk M. Population health interventions to improve colorectal cancer screening by fecal immunochemical tests: a systematic review. Prev Med. 2018;118:113–21.
Leeman J, Birken SA, Powell BJ, Rohweder C, Shea CM. Beyond "implementation strategies": classifying the full range of strategies used in implementation science and practice. Implement Sci. 2017;12(1):125. https://doi.org/10.1186/s13012-017-0657-x.
Powell BJ, Fernandez ME, Williams NJ, et al. Enhancing the Impact of Implementation Strategies in Healthcare: A Research Agenda. Front Public Health. 2019;7:3. https://doi.org/10.3389/fpubh.2019.00003.
Petrik AF, Green B, Schneider J, Miech EJ, Coury J, Retecki S, et al. Factors influencing implementation of a colorectal cancer screening improvement program in community health centers: an applied use of configurational comparative methods. J Gen Intern Med. 2020;35(Suppl 2):815–22.
Lam H, Quinn M, Cipriano-Steffens T, Jayaprakash M, Koebnick E, Randal F, et al. Identifying actionable strategies: using Consolidated Framework for Implementation Research (CFIR)-informed interviews to evaluate the implementation of a multilevel intervention to improve colorectal cancer screening. Implement Sci Commun. 2021;2(1):57.
Adams SA, Rohweder CL, Leeman J, Friedman DB, Gizlice Z, Vanderpool RC, et al. Use of evidence-based interventions and implementation strategies to increase colorectal cancer screening in federally qualified health centers. J Community Health. 2018;43(6):1044–52.
Weiner BJ, Rohweder CL, Scott JE, Teal R, Slade A, Deal AM, et al. Using practice facilitation to increase rates of colorectal cancer screening in community health centers, North Carolina, 2012–2013: Feasibility, facilitators, and barriers. Prev Chronic Dis. 2017;14:E66.
Tate CE, Matlock DD, Dalton AF, Schilling LM, Marcus A, Schommer T, et al. Implementation and evaluation of a novel colorectal cancer decision aid using a centralized delivery strategy. Jt Comm J Qual Patient Saf. 2018;44(6):353–60.
Coury J, Miech EJ, Styer P, Petrik AF, Coates KE, Green BB, et al. What’s the “secret sauce”? How implementation variation affects the success of colorectal cancer screening outreach. Implement Sci Commun. 2021;2(1):5.
Hirst Y, Skrobanski H, Kerrison RS, Kobayashi LC, Counsell N, Djedovic N, et al. Text-message reminders in colorectal cancer screening (TRICCS): a randomised controlled trial. Brit J Cancer. 2017;116(11):1408–14.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1–9.
Whittemore R, Knafl K. The integrative review: updated methodology. Methodol Issues Nurs Res. 2005;52(2):546–53.
Cooke A, Smith D, Booth A. Beyond PICO: The SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22(10):1435–43.
International Agency for Research on Cancer (IARC). Colorectal cancer screening. IARC Handb Cancer Prev. 2019;17:1–300. http://publications.iarc.fr/573. Accessed 23 Feb 2023.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45–10.
Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci. 2022;17(1):75.
Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21. https://doi.org/10.1186/s13012-015-0209-1.
Davis MM, Freeman M, Shannon J, Coronado GD, Stange KC, Guise JM, et al. A systematic review of clinic and community intervention to increase fecal testing for colorectal cancer in rural and low-income populations in the United States – How, what and when? BMC Cancer. 2018;18(1):40.
Witwer E, Baldwin LM, Cole A. Qualitative assessment of Washington State Medicaid health plan readiness to implement systems-based approaches to colorectal cancer screening. Inq J Heal Care Organization Provis Financing. 2019;56:0046958019880743.
Baldwin LM, Schneider JL, Schwartz M, Rivelli JS, Green BB, Petrik AF, et al. First-year implementation of mailed FIT colorectal cancer screening programs in two Medicaid/Medicare health insurance plans: qualitative learnings from health plan quality improvement staff and leaders. BMC Health Serv Res. 2020;20(1):132.
Kegler MC, Liang S, Weiner BJ, Tu SP, Friedman DB, Glenn BA, et al. Measuring constructs of the Consolidated Framework for Implementation Research in the context of increasing colorectal cancer screening in federally qualified health centers. Health Serv Res. 2018;53(6):4178–203.
Zoellner JM, Porter KJ, Thatcher E, Allanson D, Brauns M. Improving Fecal Immunochemical Test Return Rates: A Colorectal Cancer Screening Quality Improvement Project in a Multisite Federally Qualified Health Center. Health Promotion Practice. Published online April 6, 2022. https://doi.org/10.1177/15248399221083294.
Albers B, Metz A, Burke K, Bührmann L, Bartley L, Driessen P, et al. Implementation support skills: findings from a systematic integrative review. Res Soc Work Pract. 2021;31(2):147–70.
Varsi C, Nes LS, Kristjansdottir OB, Kelders SM, Stenberg U, Zangi HA, et al. Implementation strategies to enhance the implementation of eHealth programs for patients with chronic illnesses: realist systematic review. J Med Internet Res. 2019;21(9):e14255.
Ballengee LA, Rushton S, Lewinski AA, et al. Effectiveness of Quality Improvement Coaching on Process Outcomes in Health Care Settings: A Systematic Review. J Gen Intern Med. 2022;37(4):885–99. https://doi.org/10.1007/s11606-021-07217-2.
Goorts K, Dizon J, Milanese S. The effectiveness of implementation strategies for promoting evidence informed interventions in allied healthcare: a systematic review. BMC Health Serv Res. 2021;21(1):241.
Morrow A, Chan P, Tucker KM, Taylor N. The design, implementation, and effectiveness of intervention strategies aimed at improving genetic referral practices: a systematic review of the literature. Genet Med. 2021;23(12):2239–49.
World Health Organization - Regional Office for Europe. A short guide to cancer screening - Increase effectiveness, maximize benefits and minimize harm. 2022. Accessed 23 Feb 2023. https://apps.who.int/iris/bitstream/handle/10665/351396/9789289057561-eng.pdf.
Acknowledgements
We wish to thank Dr. Martina Gosteli, Main Library, University of Zurich, for supporting the preparation of this review protocol.
Funding
Funding for this systematic review has been provided by Swiss Cancer Research (grant number HSR-5224-11-2020, PI Clack). The funder was in no way involved in developing the protocol for this systematic review.
Author information
Authors and Affiliations
Contributions
LC, BA, RA, and KS developed the review question. BA drafted the manuscript, and all co-authors provided comments during multiple rounds of revisions. BA and LC developed the search strategy with support from a librarian. LCa, EN, EP, CP, FR, and JW contributed to identifying target literature, and conducting preliminary literature searches. RA and KS provided both methodological advice and subject matter expertise. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors affiliated with the Institute for Implementation Science in Health Care and Dr. Clara Podmore and Ms. Ekaterina Plys declare that they have no known conflicts of interests.
Dr. Kevin Selby is a member of the steering committee for the Vaud Colorectal Cancer Screening Program (CH) and a member of the Swiss Cancer Screening committee. His work has been funded by Swiss Cancer Research .
Dr. Reto Auer is a member of the expert committee for the Bern Colorectal Cancer Screening Program (CH). His work on colorectal cancer screening has been funded by the Swiss National Science Foundation (grant number: NFP74. 407440_167519) and Swiss Cancer Research (grant number: HSR-4366-11-2017).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA-P 2015 Checklist.
Additional file 2.
Search Strategy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Albers, B., Auer, R., Caci, L. et al. Implementing organized colorectal cancer screening programs in Europe—protocol for a systematic review of determinants and strategies. Syst Rev 12, 26 (2023). https://doi.org/10.1186/s13643-023-02193-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-023-02193-6