Abstract
Background
Pulmonary arterial hypertension (PAH) is a rare disease (15 cases per million) that is characterized by widespread loss of the pulmonary microcirculation and elevated pulmonary vascular resistance leading to pathological right ventricular remodeling and ultimately right heart failure. Regenerative cell therapies (i.e., therapies involving cells with stem or progenitor-like properties) could potentially restore the effective lung microcirculation and provide a curative therapy for PAH. Preclinical evidence suggests that regenerative cell therapy using endothelial progenitor cells or mesenchymal stem cells may be beneficial in the treatment of PAH. These findings have led to the completion of a small number of human clinical trials, albeit with modest effect compared to animal studies. The objective of this systematic review is to compare the efficacy and safety of regenerative cell therapies in preclinical models of PAH as well as assess study quality to inform future clinical studies.
Methods
We will include preclinical studies of PAH in which a regenerative cell type was administered and outcomes compared to a disease control. The primary outcome will be pulmonary hemodynamics as assessed by measurement of right ventricular systolic pressure and/or mean pulmonary arterial pressure. Secondary outcomes will include mortality, survival, right ventricular remodeling, pulmonary vascular resistance, cardiac output, cardiac index, pulmonary acceleration time, tricuspid annular systolic excursion, and right ventricular wall thickness. Electronic searches of MEDLINE and EMBASE databases will be constructed and reviewed by the Peer Review of Electronic Search Strategies (PRESS) process. Search results will be screened independently in duplicate. Data from eligible studies will be extracted, pooled, and analyzed using random effects models. Risk of bias will be assessed using the SYstematic Review Centre for Laboratory animal Experimentation (SYRCLE) risk of bias tool, and individual study reporting will be assessed according to an itemized checklist based on the Animal Research: Reporting of In vivo Experiments (ARRIVE) guidelines.
Discussion
This systematic review will examine the efficacy and safety of regenerative cell therapy in preclinical models of PAH. As well, the literature will be assessed for study quality and risk of bias. The results will guide the design of future clinical trials and preclinical animal studies.
Systematic review registration
CAMARADES (http://www.dcn.ed.ac.uk/camarades/SyRF/Protocols.htm).
Similar content being viewed by others
Background
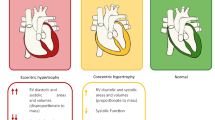
Pulmonary hypertension is a progressive disease that results from restricted blood flow through the pulmonary circulation and loss of effective pulmonary microvascular area. This leads to increased resistance in the pulmonary vasculature and eventually right heart failure [1]. Clinically, pulmonary arterial hypertension (PAH) is defined by an increase in mean pulmonary arterial pressure ≥25 mmHg at rest by right heart catheterization with a pulmonary capillary wedge pressure ≤15 mmHg. PAH, classified as World Health Organization (WHO) Group I pulmonary hypertension [1, 2], represents a group of diseases of various etiologies that are characterized by increased pulmonary vascular resistance due to pathology at the level of the precapillary arteriolar system. Although the mechanisms underlying the pathobiology of PAH are still unclear, it is thought that injury to the pulmonary endothelium leads to apoptosis which, in turn, triggers processes that reduce the effective lung vasculature, including widespread loss of functional microcirculation and obliterative remodeling of the small pulmonary arterioles due to the emergence of growth dysregulated vascular cells [3]. Ultimately, loss of lung microcirculation leads to progressive increase in pulmonary vascular resistance, right ventricular remodeling, and eventually right heart failure [4–6]. PAH is subdivided into subgroups based on etiology such as idiopathic, hereditary, drug- and toxin-induced, and PAH associated with other diseases such as connective tissue disease HIV, schistosomiasis, chronic hemolytic anemia, and congenital heart disease (Table 1).
The current standard of care PAH-specific therapies consists largely of pharmacological vasodilator agents, such as phosphodiesterase-5 inhibitors, prostacyclin analogs, and endothelin antagonists. These have only modest effects on pulmonary hemodynamics, and prognosis remains poor despite introduction of a number of new therapies in the last 5 years [7]. The most recent estimate of 5-year survival of newly diagnosed PAH is 61.2 % [7]. Thus, the development of clinically effective strategies to restore normal pulmonary structure and function in established PAH are needed.
Recent understanding of the role of adult stem and progenitor cells in the maintenance of vascular homeostasis and repair of injury has stimulated interest in the potential for regenerative cell therapies for PAH. Most of the preclinical studies of cell therapy for PAH have used two cell types in particular, early-outgrowth endothelial progenitor cells (EPCs, also known as circulating angiogenic cells, myeloid angiogenic cells) and mesenchymal stromal cells (MSCs, also known as mesenchymal stem cells, adult stem cells) [8, 9]. EPCs and MSCs have been described as dynamic and responsive cells that can migrate to sites of vascular injury in several in vivo animal disease models [10], facilitating neovascularization and reducing inflammation [8]. As a treatment for PAH, preclinical studies involving these cell types have demonstrated efficacy in improving key pathological features of PAH such as cardiopulmonary hemodynamics, restoring the degenerated microvascular area, and reducing both right ventricular and pulmonary vascular remodeling [8]. A small number of clinical studies involving stem/progenitor cell therapy on PAH patients have been completed or are underway and show some promise in controlling the extent of the disease [3, 11]. However, to date, there has been no systematic synthesis of preclinical studies investigating stem cells therapy for the treatment of PAH.
In order to address this knowledge gap, we will conduct a preclinical systematic review of regenerative cell therapy for PAH. In contrast to narrative preclinical reviews of stem cells for PAH treatment, this systematic review will provide additional key evaluations. The meta-analysis will provide an estimation of the cumulative overall effect of stem cell treatment on pulmonary hemodynamics based on currently available data in preclinical studies. This systematic review will also attempt to evaluate the quality of currently available evidence based on risk of bias assessment and completeness of reporting, and the potential for publication bias. This data may impact the design of current preclinical testing of stem cell therapies and potentially influence the design of future clinical trials.
Study questions
In preclinical studies of pulmonary arterial hypertension, do PAH animals receiving regenerative cell therapy exhibit improved pulmonary hemodynamics compared to PAH animals not receiving regenerative cell therapy and is regenerative cell therapy safe?
Methods/design
Protocol and registration
The protocol was developed by a research team of clinical (DS, AZ) and preclinical research scientists (CS, ML), experts in knowledge synthesis and translation (DF, LM). The protocol will follow the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) checklist (Additional file 1: PRISMA checklist). The protocol is registered through the Collaborative Approach to Meta Analyses and Review of Animal Data from Experimental Studies (CAMARADES) website (http://www.camarades.info).
Types of studies
This review will include controlled studies (randomized, pseudo-randomized and non-randomized) that evaluate the efficacy or safety of regenerative cell therapy for PAH.
Types of preclinical animal models
We will include preclinical in vivo models of PAH that reproduce features of the pathophysiology associated and/or etiology of human PAH [1]. Specifically, the eligible animal models are the rodent monocrotaline (MCT), chronic hypoxia (CH), and SU5416 + chronic hypoxia (SU+CH) models. These are recognized as the most representative and most widely utilized methods of induction for modeling human PAH [12]. These models do not require invasive surgery or extensive manipulation that could be subject to technical variability and therefore provide a predictable disease phenotype. These models share in common the characteristic pathological features of human PAH: endothelial dysfunction, SMC proliferation, inflammation, and vascular narrowing and rarefaction resulting in pulmonary hypertension and right ventricular remodeling; however, only the SU+CH model reproduces the complex obliterative vascular lesions that are typical of human PAH [13]. Mouse models will not be considered for this systematic review as currently available models (chronic hypoxia) lack significantly elevated pulmonary pressures, right ventricular hypertrophy, and pulmonary arteriolar remodeling [12].
Animal models of PH secondary to other causes such as left heart disease, lung disease, or thromboembolism (WHO Groups 3-5) [4] will not be included. Genetically modified animals and will also be excluded. Since the purpose of this study to inform future decisions for designing clinical trials for adult populations, this study will exclude neonatal animal models of pulmonary hypertension.
Types of interventions
The intervention group will include animals receiving any regenerative cell therapy (xenogeneic, syngeneic, or allogeneic cells from any tissue source). Experiments involving pretreatment of cells, co-treatment, and/or genetic manipulation (e.g., engineered to over- or under-express certain genes) will be classified as “cell modifications” for subgroup analysis. Studies using non-stem/progenitor cells (i.e., terminally differentiated cells such as mature endothelial cells, smooth muscle cells, or fibroblasts) as the therapeutic intervention will be excluded. Studies that do not include the administration of viable cells, for example, studies with only cell-free products derived from stem/progenitor cells such as conditioned media, will also be excluded.
Types of control comparisons
The preclinical comparison group will include animals from studies that have had experimentally induced PAH but have not been administered a regenerative cell (vehicle control, control cell type, or no treatment).
Timing of outcome measurements
Outcomes will be assessed at least 1 week after intervention to exclude the possibility of acute effects of cell administration.
Preclinical primary endpoints
The current gold standard for the diagnosis and evaluation of clinical pulmonary hypertension is direct pulmonary hemodynamic measures by right heart catheterization. The primary endpoint will be direct measures of pulmonary hemodynamics (mean pulmonary arterial pressure, right ventricular systolic pressure) measured after administration of cells (Table 2). The primary outcome will be assessed at the end of the follow-up period.
Preclinical secondary endpoints
We will collect data on all deaths and animal mortality. Right ventricular (RV) remodeling is a forerunner of right heart failure, which is characterized by decreased function and dilatation of the RV and strongly correlates with prognosis and survival in PH patients [14]. We will collect morphometric data on right ventricular remodeling expressed as the weight ratio of right ventricle/left ventricle + septum. Other measures of cardiac function and hemodynamics will also be collected to assess functional performance of the heart such as cardiac output and cardiac index (cardiac output/body weight) and pulmonary vascular resistance.
We will collect data from other noninvasive measures obtained by echocardiography to evaluate cardiac structure and pulmonary hemodynamics (Table 2). Mortality and survival will also be collected to evaluate the safety of the intervention.
Electronic search methods for study identification
In consultation with the review team, electronic search strategies will be developed for each database by an experienced medical information specialist. Ovid MEDLINE®, Ovid MEDLINE® In-Process & Other Non-Indexed Citations, and EMBASE Classic + EMBASE will be searched. The strategy appended was used to search in MEDLINE (Additional file 2). The search strategy will be validated using the Peer Review of Electronic Search Strategies (PRESS) template by another information specialist [15].
Search strategies will use a combination of controlled vocabulary (for example stem cells, pulmonary hypertension) and keywords (for example, EPC, MSC, iPSC, HSC, PAH), and parsing will be formatted accordingly to each database. We will use modified animal filters from previously published methods [16, 17] validated for PubMed/MEDLINE and EMBASE. There will be no date restrictions on any of the searches. In addition, a manual review of the bibliographies of selected articles and relevant reviews will be performed. Only articles in the English language will be included in the review.
Study selection
Titles and abstracts of search results will be screened independently by two individuals. Full text of all potentially eligible studies will be reviewed based on our eligibility criteria. Disagreements between reviewers will be resolved by consensus or by a third member of the systematic review team (DJS). Reasons for exclusion of potentially eligible studies will be recorded in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines developed for proper reporting of clinical systematic reviews [18].
Data collection and process and data items
Data will be extracted independently by two individuals into standardized, electronic pilot-tested forms using DistillerSR software (https://distillercer.com). Specific data elements collected for this review are listed in Table 2.
Assessment of risk of bias
Risk of bias will be assessed independently in duplicate for each included study using the Systematic Review Centre for Laboratory animal Experimentation (SYRCLE) risk of bias tool. The SYRCLE tool was adapted from the Cochrane Risk of Bias Tool to assess the methodological quality using criteria specific to animal studies (Table 3). Items in this tool include assessments for selection bias (sequence generation, baseline characteristics, allocation concealment), performance bias (random housing, blinding), detection bias (random outcome assessment, blinded outcome assessment), attrition bias (completeness of outcome data), and reporting bias. For each included study, each parameter for type of bias will be scored as low, high, or unclear risk of bias.
Assessment of external validity
This review will record features that will facilitate judgments of external validity. External validity in preclinical research concerns the extent to which results can be generalized to different experimental measures, settings, and times [19]. These assessments aid in the ability to replicate experimental findings. External validity will be assessed by subgroup analysis of the primary outcome based on: age, gender, species and strain of animal, model of PAH, severity of PAH, use of cell preservation, tissue source of regenerative cell product, timing of cell administration, dose of cells, type of control, presence of cell modification, and number of participating study centers (Table 4). These data will help evaluate the effect of factors such as animal characteristics and regenerative cell preparation. As well, this will help identify optimal conditions for regenerative cell therapy to inform future clinical trials.
Assessment of construct validity
Construct validity in preclinical research refers to the ability of a study to generalizable to a clinical scenario [20]. Threats to construct validity arise when experimental conditions (model, intervention, outcomes) are not representative of the clinical scenario.
We will assess construct validity based on a pre-defined checklist of factors aimed evaluate how closely the study resembles clinical PAH. The domains assessed will be animal subjects, outcome measures, modeling of disease, administration of intervention, and environment (Table 5). These will be recorded as yes/no answers.
Description of reporting
We will apply the Animal Research: Reporting of In vivo Experiments (ARRIVE) guidelines to evaluate the quality of reporting in preclinical studies. The ARRIVE guidelines were developed by the National Centre for the Replacement, Refinement, and Reduction of Animals in Research (NC3Rs) to improve the transparent and comprehensive reporting of research methods and results for in vivo animal experiments [21].
Data analysis
Continuous endpoints will be pooled using the ratio of weighted means using the inverse variance random effects method [22, 23]. Death will be analyzed as the mortality ratio of ndeaths/ntotal at defined endpoints and by mean survival in days. Statistical heterogeneity of included studies will be measured using the I2 test with 95 % confidence intervals [24]. An evaluation for the presence of publication bias will be conducted with funnel plots and Egger’s regression test [25].
Planned subgroup analyses will be examined on the primary endpoint of right heart catheterization hemodynamics (RVSP/mPAP). Heterogeneity will be analyzed for the following: PAH induction method, age, sex, strain, regenerative cell type, tissue origin of cells, timing of administration (<2 weeks post-induction, ≥2 weeks post-induction), follow-up period (0, 1, 2, 3, 4+ weeks post-intervention), route of delivery, cell dose, dose frequency, use of cell pretreatments and other enhancement strategies (e.g., gene transfection), and sample sizes of study.
Discussion
The timing of this review is highly relevant, as clinical trials have been completed (NCT00257413, NCT00641836, NCT00469027) [11, 3 ,26]. So far, based on limited short-term data, the results of completed clinical trials have shown relatively modest benefits [11] compared to the effect sizes reported in some preclinical literature [27, 28]. Most of the evidence supporting regenerative cell therapy for PAH has been based on findings observed in prevention studies rather than treatment studies in established pulmonary hypertension [8], which may have contributed to the overestimation of the degree of their efficacy. Therefore, a thorough examination of the study design with attention to the timing of interventions and suitability of follow-up duration must be conducted to determine the validity of the available evidence and potential for clinical translation.
Systematic reviews should be valuable in stem cell research because of the high degree of heterogeneity of cell products used for therapy. As such, a secondary aim of this study will be to evaluate the relative efficacy between regenerative cell types. Although EPCs and MSCs have both been studied extensively in preclinical models, we anticipate that other cell products such as cells derived from embryonic stem cells or induced pluripotent stem cell may also have in vivo efficacy. Still, guidelines and/or criteria for what constitutes a particular regenerative cell type are ill-defined and when available, they are loosely defined based on an evolving understanding of stem cell biology [29]. In the absence of such standards, this review will address the level of transparency in reporting of pertinent information regarding stem cell isolation and culture techniques and quality control for each cell type, as well as the delivery and dosing methods.
We anticipate that this comprehensive synthesis will provide valuable information in translating stem cell therapy to the clinic. In addition, this review will have an immediate impact on preclinical research by highlighting knowledge gaps and areas to improve study design for future preclinical investigations of PAH.
Abbreviations
ALK-1, activin receptor-like kinase 1; ARRIVE, Animal Research, Reporting of In vivo Experiments; BMPR2, bone morphogenetic receptor, type 2; CAMARADES, Collaborative Approach to Meta Analysis and Review of Animal Data from Experimental Studies; CAV1, caveolin 1; ENG, endoglin; EPC, endothelial progenitor cell; KCNK3, potassium channel subfamily K member 3; mPAP, mean pulmonary arterial pressure; MSC, mesenchymal stem cell, marrow stromal cell, or mesenchymal stromal cell; PAH, pulmonary arterial hypertension; PVR, pulmonary vascular resistance; RV, right ventricle; RVSP, right ventricular systolic pressure; SMAD9, mothers against decapentaplegic homolog 9; SYRCLE, Systematic Review Centre for Laboratory animal Experimentation.
References
Simonneau G, Gatzoulis MA, Adatia I, Celermajer D, Denton C, Ghofrani A, Gomez Sanchez MA, Krishna Kumar R, Landzberg M, Machado RF, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62:D34–41.
Simonneau G, Robbins IM, Beghetti M, Channick RN, Delcroix M, Denton CP, Elliott CG, Gaine SP, Gladwin MT, Jing ZC, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2009;54:S43–54.
Jurasz P, Courtman D, Babaie S, Stewart DJ. Role of apoptosis in pulmonary hypertension: from experimental models to clinical trials. Pharmacol Ther. 2010;126:1–8.
McLaughlin VV, Archer SL, Badesch DB, Barst RJ, Farber HW, Lindner JR, Mathier MA, McGoon MD, Park MH, Rosenson RS, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association: developed in collaboration with the American College of Chest Physicians, American Thoracic Society, Inc., and the Pulmonary Hypertension Association. Circulation. 2009;119:2250–94.
Humbert M, Morrell NW, Archer SL, Stenmark KR, MacLean MR, Lang IM, Christman BW, Weir EK, Eickelberg O, Voelkel NF, Rabinovitch M. Cellular and molecular pathobiology of pulmonary arterial hypertension. J Am Coll Cardiol. 2004;43:13S–24S.
Schermuly RT, Ghofrani HA, Wilkins MR, Grimminger F. Mechanisms of disease: pulmonary arterial hypertension. Nat Rev Cardiol. 2011;8:443-55.
Farber HW, Miller DP, Poms AD, Badesch DB, Frost AE, Muros-Le Rouzic E, Romero AJ, Benton WW, Elliott CG, McGoon MD, Benza RL. Five-Year outcomes of patients enrolled in the REVEAL Registry. Chest. 2015;148:1043–54.
Suen CM, Mei SH, Kugathasan L, Stewart DJ. Targeted delivery of genes to endothelial cells and cell- and gene-based therapy in pulmonary vascular diseases. Compr Physiol. 2013;3:1749–79.
Foster WS, Suen CM, Stewart DJ. Cell and tissue-based regenerative therapies for pulmonary arterial hypertension. Can J Cardiol. 2014;30:1350-60
Takahashi T, Kalka C, Masuda H, Chen D, Silver M, Kearney M, Magner M, Isner JM, Asahara T. Ischemia- and cytokine-induced mobilization of bone marrow-derived endothelial progenitor cells for neovascularization. Nat Med. 1999;5:434–8.
Wang X-X, Zhang F-R, Shang Y-P, Zhu J-H, Xie X-D, Tao Q-M, Zhu J-H, Chen J-Z. Transplantation of autologous endothelial progenitor cells may be beneficial in patients with idiopathic pulmonary arterial hypertension: a pilot randomized controlled trial. J Am Coll Cardiol. 2007;49:1566–71.
Ryan JJ, Marsboom G, Archer SL. Rodent models of group 1 pulmonary hypertension. Handb Exp Pharmacol. 2013;218:105–49.
Stenmark KR, Meyrick B, Galie N, Mooi WJ, McMurtry IF. Animal models of pulmonary arterial hypertension: the hope for etiological discovery and pharmacological cure. Am J Physiol Lung Cell Mol Physiol. 2009;297:L1013–1032.
Vonk-Noordegraaf A, Haddad F, Chin KM, Forfia PR, Kawut SM, Lumens J, Naeije R, Newman J, Oudiz RJ, Provencher S, et al. Right heart adaptation to pulmonary arterial hypertension: physiology and pathobiology. J Am Coll Cardiol. 2013;62:D22–33.
McGowan J, Sampson M, Lefebvre C. An evidence based checklist for the peer review of electronic search strategies (PRESS EBC). Evid Based Libr Inf Pract. 2010;5:149–54.
de Vries RB, Hooijmans CR, Tillema A, Leenaars M, Ritskes-Hoitinga M. A search filter for increasing the retrieval of animal studies in Embase. Lab Anim. 2011;45:268–70.
Hooijmans CR, Tillema A, Leenaars M, Ritskes-Hoitinga M. Enhancing search efficiency by means of a search filter for finding all studies on animal experimentation in PubMed. Lab Anim. 2010;44:170–5.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. w264.
Sena ES, Currie GL, McCann SK, Macleod MR, Howells DW. Systematic reviews and meta-analysis of preclinical studies: why perform them and how to appraise them critically. J Cereb Blood Flow Metab. 2014;34:737–42.
Henderson VC, Kimmelman J, Fergusson D, Grimshaw JM, Hackam DG. Threats to validity in the design and conduct of preclinical efficacy studies: a systematic review of guidelines for in vivo animal experiments. PLoS Med. 2013;10:e1001489.
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG. Improving Bioscience Research Reporting: The ARRIVE Guidelines for Reporting Animal Research. PLoS Biol. 2010;8:e1000412.
Friedrich JO, Adhikari NK, Beyene J. The ratio of means method as an alternative to mean differences for analyzing continuous outcome variables in meta-analysis: a simulation study. BMC Med Res Methodol. 2008;8:32.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Hayashino Y, Noguchi Y, Fukui T. Systematic evaluation and comparison of statistical tests for publication bias. J Epidemiol. 2005;15:235–43.
Zhu JH, Wang XX, Zhang FR, Shang YP, Tao QM, Zhu JH, Chen JZ. Safety and efficacy of autologous endothelial progenitor cells transplantation in children with idiopathic pulmonary arterial hypertension: open-label pilot study. Pediatr Transplant. 2008;12:650–5.
Nagaya N, Kangawa K, Kanda M, Uematsu M, Horio T, Fukuyama N, Hino J, Harada-Shiba M, Okumura H, Tabata Y, et al. Hybrid cell-gene therapy for pulmonary hypertension based on phagocytosing action of endothelial progenitor cells. Circulation. 2003;108:889–95.
Zhao YD, Courtman DW, Deng Y, Kugathasan L, Zhang Q, Stewart DJ. Rescue of monocrotaline-induced pulmonary arterial hypertension using bone marrow-derived endothelial-like progenitor cells: efficacy of combined cell and eNOS gene therapy in established disease. Circ Res. 2005;96:442–50.
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop D, Horwitz E. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8:315–7.
Urboniene D, Haber I, Fang YH, Thenappan T, Archer SL. Validation of high-resolution echocardiography and magnetic resonance imaging vs. high-fidelity catheterization in experimental pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol. 2010;299:L401–412.
Badesch DB, Raskob GE, Elliott CG, Krichman AM, Farber HW, Frost AE, Barst RJ, Benza RL, Liou TG, Turner M, et al. Pulmonary arterial hypertension: baseline characteristics from the REVEAL Registry. Chest. 2010;137:376–87.
Gaine SP, Rubin LJ. Primary pulmonary hypertension. Lancet. 1998;352:719–25.
McQuillan BM, Picard MH, Leavitt M, Weyman AE. Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation. 2001;104:2797–802.
Acknowledgements
CS holds a Vanier Canada Graduate Scholarship and a Canadian Institutes of Health Research Training Program in Regenerative Medicine fellowship. We would like to thank Becky Skidmore (Information Specialist) and Risa Shorr (Librarian, The Ottawa Hospital) for providing assistance with the generation of a systematic search strategy and article retrieval.
Authors’ contributions
CS, AZ, and DS conceived the study design. CS and ML were responsible for the initial drafting of the manuscript. CW and BL were responsible for the data collection. DS, ML, LM, and DF provided critical revisions for important intellectual content. All authors have reviewed and approved the final version of the manuscript.
Competing interests
DS is President and CEO of Northern Therapeutics (Montréal, QC, Canada).
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1:
Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) 2015 checklist: recommended items to address in a systematic review protocol*. (DOC 81 kb)
Additional file 2:
Appendix A1. MEDLINE Search Strategy. (DOCX 126 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Suen, C.M., Zhai, A., Lalu, M.M. et al. Efficacy and safety of regenerative cell therapy for pulmonary arterial hypertension in animal models: a preclinical systematic review protocol. Syst Rev 5, 89 (2016). https://doi.org/10.1186/s13643-016-0265-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-016-0265-x