Abstract
Background
Survival benefit from low tidal volume (VT) ventilation (LTVV) has been demonstrated for patients with acute respiratory distress syndrome (ARDS), and patients not having ARDS could also benefit from this strategy. Organizational factors may play a role on adherence to LTVV. The present study aimed to identify organizational factors with an independent association with adherence to LTVV.
Methods
Secondary analysis of the database of a multicenter two-phase study (prospective cohort followed by a cluster-randomized trial) performed in 118 Brazilian intensive care units. Patients under mechanical ventilation at day 2 were included. LTVV was defined as a VT ≤ 8 ml/kg PBW on the second day of ventilation. Data on the type and number of beds of the hospital, teaching status, nursing, respiratory therapists and physician staffing, use of structured checklist, and presence of protocols were tested. A multivariable mixed-effect model was used to assess the association between organizational factors and adherence to LTVV.
Results
The study included 5719 patients; 3340 (58%) patients received LTVV. A greater number of hospital beds (absolute difference 7.43% [95% confidence interval 0.61–14.24%]; p = 0.038), use of structured checklist during multidisciplinary rounds (5.10% [0.55–9.81%]; p = 0.030), and presence of at least one nurse per 10 patients during all shifts (17.24% [0.85–33.60%]; p = 0.045) were the only three factors that had an independent association with adherence to LTVV.
Conclusions
Number of hospital beds, use of a structured checklist during multidisciplinary rounds, and nurse staffing are organizational factors associated with adherence to LTVV. These findings shed light on organizational factors that may improve ventilation in critically ill patients.
Similar content being viewed by others
Introduction
Survival benefit from low tidal volume (VT) ventilation (LTVV) has clearly been demonstrated for patients with acute respiratory distress syndrome (ARDS) [1]. Patients not having ARDS could also benefit from this strategy [2,3,4,5], albeit that tidal volumes may not always need to be as low as in patients with ARDS [6]. As it could be difficult to discriminate patients with ARDS from those not having ARDS [7, 8], one reasonable and pragmatic approach could be to use LTVV (defined as ventilation using a VT ≤ 8 ml/kg predicted body weight [PBW]) in all invasively ventilated critically ill patients [9]. This is, at least, in part in line with international guidelines recommending a VT of 4 to 8 ml/kg PBW in patients with ARDS [10], and with the suggestion not to use a VT > 8 ml/kg PBW in patients not having ARDS [11,12,13].
Several studies have demonstrated an increased adherence to LTVV over recent decades [14,15,16,17]. Yet, many patients remain to receive ventilation with a too large VT [7, 18, 19]. For instance, the ‘Large observational study to UNderstand the Global impact of Severe Acute respiratory FailurE’ (LUNG SAFE) study showed that as many as one-third of ARDS patients receive a VT > 8 ml/kg PBW [7]. A similar proportion of patients without ARDS did not receive LTVV in the ‘PRatice of VENTilation in critically ill patients without ARDS’ (PRoVENT) study [18]. In the ‘Checklist During Multidisciplinary Visits for Reduction of Mortality in Intensive Care Units’ (CHECKLIST-ICU) study, even if the intervention led to a better adherence to LTVV as compared with the control group, only two-thirds of patients under invasive ventilation in the intervention group received a VT ≤ 8 ml/kg PBW [19].
Organizational factors associated with a better outcome in ICU patients include intensity of doctor, nurse and respiratory therapist staffing [20,21,22,23,24], continuity of care [25, 26], and use of multidisciplinary rounds and structured handovers [27, 28]. Yet, no study evaluated which organizational factors are related to adherence to LTVV. Therefore, the CHECKLIST-ICU database was used to identify organizational factors that are independently associated with adherence to LTVV.
Methods
Study design and patients
The study protocol of the CHECKLIST-ICU study was prepublished [29] and registered (clinicaltrials.gov, study identifier NCT01785966), and the results of the primary analysis were reported recently [19]. In brief, the CHECKLIST-ICU study consisted of two phases. In phase I, organizational factors and clinical outcomes were collected in 118 Brazilian adult ICUs, from August 2013 to March 2014. In phase II, the ICUs were randomized to a quality improvement intervention or to usual care, from April 2014 to November 2014. The quality improvement intervention consisted of a checklist and discussion of goals of care during daily multidisciplinary rounds, followed by clinician prompting to ensure checklist adherence and goals of care.
The checklist assessed prevention and management of lung injury, venous thromboembolism, ventilator-associated pneumonia, central line-associated bloodstream and urinary tract infections, nutritional targets, analgesia and sedation goals, detection of sepsis and ARDS, and antibiotic initiation and stewardship. In specific, for prevention of lung injury, it was advised to adhere to LTVV and to assess readiness for extubation. Other care processes, with the exception of the checklist, discussion of goals of care and clinician prompting were unchanged between the two phases of the study. The institutional review boards of all centers approved the study. The funding source had no role in the analysis or publication decisions.
The CHECKLIST-ICU restricted participation to patients 18 years or older; and with an ICU stay longer than 48 h. Patients in whom a high probability of early death was anticipated (defined as death occurring between the 48th and 72nd hours of the ICU stay), patients receiving exclusive palliative care, as well as patients who were suspected of or had a diagnosis of brain death were excluded. The current analysis uses data from both study phases, but restricted to patients who had received invasive ventilation for at least 2 days. This period was chosen for two reasons: first, to guarantee sufficient time to evaluate exposure to the intervention, and second, because the majority of patients were extubated within 3 days.
Data collection and definitions
The database of the CHECKLIST-ICU study contains baseline information [age, gender, reason for admission, type of admission (clinical, elective or urgent surgery), illness severity (Simplified Acute Physiology Score [SAPS] 3 and Sequential Organ Failure Assessment [SOFA])], study phase (phase I or II), ICU and hospital mortality, and ICU and hospital length of stay.
For ventilation evaluation, in the original trial VT size was recorded on day 2, 5, 8, 11, 14 and 17. The target VT in the checklist was ≤ 8 ml/kg PBW in all days, with PBW calculated as 50 + 0.91*(height [in cm] − 152.4) for males and 45.5 + 0.91*(height [in cm] − 152.4) for females. For the purpose of the current analysis, adherence to LTVV was defined as VT of ≤ 8 ml/kg PBW at the second day of ventilation only.
In the participating units, physiotherapists were responsible for the ventilator settings and the physical therapy. However, ventilatory management was adjusted according to decisions taken in multidisciplinary rounds, and after approval of the physician in charge. In some units, in particular when a physiotherapist was not a member of the team, nurses were allowed to change ventilatory settings.
The following organizational data related to the process of care of each participating ICU were collected in the CHECKLIST-ICU study and considered in the present study:
Level of hospital (tertiary vs non-tertiary);
Type of hospital (specialty vs general);
Teaching status (university affiliated vs not university affiliated);
Number of hospital beds (according to tertiles in the present study);
Number of ICU beds (according to tertiles in the present study);
Presence of multidisciplinary rounds (yes vs no);
Use of a structured checklist during rounds (yes vs no);
Presence of sedation and analgesia, and weaning, and prevention of ventilator-associated pneumonia (VAP) protocols (yes vs no);
Presence of board-certified ICU consultant (morning and afternoon vs morning or afternoon);
Presence of at least one physician for each 10 patients in all shifts; (yes vs no);
Presence of one board-certified respiratory therapist coordinator (yes vs no);
Presence of one respiratory therapist for each 10 patients in all shifts (yes vs no);
Presence of at least one nurse per 10 patients during all shifts (yes vs no).
Outcomes
The primary outcome of this analysis was the organizational factors associated with adherence to LTVV. Secondary outcomes were the adherence to LTVV on the second day of ventilation, and the impact of adherence to LTVV in ICU and hospital mortality.
Statistical analyses
Continuous variables are presented as mean ± standard deviation and compared with Student’s t test. Categorical variables are presented as absolute numbers and proportions and compared with the Chi square test or Fisher’s exact test, where appropriate. All analyses were performed using multilevel (patients nested in study centers, within the phases of the trial) mixed modeling with centers as random effect and the phase of the study as a fixed effect. Absolute difference between the groups with the respective 95%-confidence interval (95% CI) was calculated from a mixed-effect linear model and reported as mean differences for continuous variables and as risk differences for categorical variables.
The association between organizational factors and use of LTVV was assessed with a mixed-effect generalized linear model and the variables included in the multivariable models were defined according to clinical rationale and when a p value < 0.20 was found in the univariable models. The final multivariable model was adjusted for patient severity, according to SAPS 3 and SOFA. Heterogeneity between the phases of the trial was determined by fitting a fixed interaction term between the phase and organizational factors associated with use of LTVV, while overall effect is reported with phase treated as a fixed effect and centers treated as a random effect. The use of a structured checklist was not considered in the heterogeneity analysis, since it was used only in one of the phases of the study, i.e., in the cluster-randomized trial.
The impact of LTVV on ICU and hospital mortality was also assessed with a mixed-effect generalized linear model considering a binomial distribution, adjusted for SAPS 3 and SOFA at the patient level.
Continuous variables were standardized before being included in the multivariable models described above to improve convergence. All analyses were performed using the R (R, version 3.6.0, Core Team, Vienna, Austria, 2016) software, and a two-sided alpha level of 0.05 was considered.
Results
The database of the CHECKLIST-ICU study included data of a total 13,638 patients in 118 ICUs. Of them, 5719 patients had received invasive ventilation for at least 2 days, 2936 (51.3%) in phase I, and 2783 (48.7%) in phase II (Fig. 1). Baseline characteristics of patients who received LTVV (3340 patients, 58% of all patients) and patients who did not receive LTTV at the second day of ventilation (2379 patients, 42% of all patients) are shown in Table 1. Most admissions were medical, and the main reasons for admission were sepsis and acute respiratory failure. VT data were available for all patients on day 2.
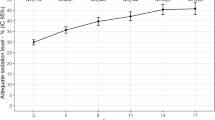
The proportion of patients receiving LTVV was 58.4% (95% CI, 57.1% to 59.7%) on day 2, and did not change thereafter (Fig. 2). Patients who received LTVV were younger, taller, were more often male, and were less severely ill according to their SAPS and SOFA scores.
Tidal volume and frequency of the use of low tidal volume ventilation over the first 17 days of follow-up. Circles are the mean and error bars the 95% confidence interval. Unadjusted mixed-effect longitudinal models with random intercept for patients and center, and with phase of the study, group, days and the interaction of group × days as fixed effects. p values for the group reflect the overall test for difference between groups across the follow-up while p values for the group × days interaction evaluate if change over time differed by group
Organizational factors with an association with adherence to LTVV in the unadjusted analysis are shown in Table 2. In the adjusted analysis, number of hospital beds (absolute difference 7.43 [0.61 to 14.24]; p = 0.038), use of a structured checklist during multidisciplinary rounds (absolute difference 5.10 [0.55 to 9.81]; p = 0.030), and presence of at least one nurse per 10 patients during all shifts (absolute difference 17.24 [0.85 to 33.60]; p = 0.045) were associated with adherence to LTVV (Table 3).
There was no heterogeneity between study phases and the effect of number of hospital beds on adherence to LTVV (p = 0.254). There was an interaction between study phases and the effect of the presence of at least one nurse per 10 patients during all shifts on adherence to LTVV (estimate, − 16.13 [− 31.0 to − 1.41]; p = 0.032). In the second phase of the study, presence of at least one nurse per 10 patients during all shifts and adherence to LTVV were no longer associated (Additional file 1: Figure S1).
There was no difference in ICU (absolute difference, 0.27 [− 2.29 to 2.84]; p = 0.833) or hospital mortality (absolute difference, 0.03 [− 2.51 to 2.57]; p = 0.980) according to the use LTVV (Additional file 1: Table S1).
Discussion
This study suggests that the larger centers with a higher number of hospital beds, use of structured checklists during multidisciplinary rounds, and the presence of at least one nurse for every 10 patients in all shifts are the three organizational factors associated with adherence to LTVV. Interestingly, VT stays remarkable unchanged over the total duration of ventilation, i.e., VT does not change beyond the second day of ventilation. Mortality was not different between patients who received and those who did not receive LTVV.
The finding that the number of hospital beds is associated with a higher adherence to LTVV might be explained as follows. First, ICUs in larger hospitals usually have higher number of caregivers, more experienced teams, and also higher volumes of invasively ventilated patients. Second, ICU bed supply and quality of care in ICUs are usually related to the size of a hospital [30, 31], and smaller hospitals frequently suffer with lack of beds and consequently inappropriate allocation, which is also associated with a lower quality of care [32]. Nevertheless, in Brazil usually the larger hospitals are the public university-affiliated hospitals, and in the present analyses this intersection could not be completely assessed. However, the association among larger hospitals and adherence to LTVV could reflect, indirectly, a higher adherence in teaching hospitals also. All those characteristics, however, were not directly collected and measured in the CHECKLIST-ICU study.
The finding that the use of a structured checklist during multidisciplinary rounds is associated with adherence to LTVV is in line with findings of previous studies. One study in invasively ventilated ICU patients with ARDS showed that use of a written ventilation protocol was associated with higher use of LTVV [33]. Another study in critically ill ICU patients demonstrated that charts installed on ventilators showing the adequate VT target (4–6 ml/kg PBW) for each patient led to a significant decrease in VT [24]. Such findings suggest that adoption of written documents such as protocols, checklists and charts may improve adherence to LTVV and ensure translation of evidence for benefit, in this case of LTVV, into clinical practice. Of note, protocols for mechanical ventilation often do not incorporate LTVV strategies [34], and use of a protocol does not guarantee that all patients will receive the best practice [35]. However, one large Brazilian study demonstrated that the implementation of protocols was associated with better patient outcomes and more efficient use of resources [27].
The finding that adherence to LTVV increased with presence of more nurses is also in line with previous findings [20,21,22]. A nurse-to-patient ratio > 1:1.5 was independently associated with a lower risk of in-hospital death in a large multicenter cohort of ICU patients in a worldwide study [22]. Vice versa, a lower ICU nurse staffing was associated with adverse outcomes in a study in hospitals across the USA [21]. In Brazil, ICU nurse staffing varies considerably depending on local regulations. However, a study in 93 Brazilian ICUs showed that ICUs where nurses have higher autonomy, including start of weaning from ventilation and the titrating FiO2, have better outcomes compared to ICUs where there is less nurse autonomy [36]. After implementation of the structured checklist in the second phase of the CHECKLIST-ICU study, the positive effect of one nurse for every 10 patients in all shifts on the use of LTVV was no longer associated with compliance with LTVV. This finding is important, and suggests that a structured checklist can increase the adoption of LTVV, even in institutions where the nurse-to-patient ratio is low. At the end, the impact of a higher nurse-to-patient ratio on adherence to LTVV can be explained by several different factors, including (1) adoption of the checklist, per se; (2) better use of the checklist by healthcare providers like respiratory therapists, typically more present in ICUs with a higher nurse-to-patient ratio; and (3) presence of more nurses, who can adjust ventilator settings.
Use of LTVV was not associated with lower mortality as described in previous studies [3, 5, 37]. This may be explained by the small difference in VT between the two groups, i.e., 6.7 (5.9–7.4) vs 9.2 (8.5–10.2) ml/kg PBW. This is different from previous studies that used VT of as high as 12 ml/kg PBW for comparison. Of note, one recent randomized clinical trial in patients not having ARDS did found beneficial effects of a low VT strategy [resulting in VT of 6.6 (5.5–8.7) ml/kg PBW] when compared to an intermediate VT strategy [resulting in VT of 9.3 (8.1–10.1) ml/kg PBW] [6]. Despite this, identifying factors that have an effect of use of LTVV could help improving ICU organization as well as safety of invasively ventilated patients in general.
Interestingly, the current study suggests that early use of LTVV is associated with continued use of ventilation with a low VT on successive days. This finding shows that patients who had VT correctly titrated to PBW early on ICU admission were more likely to continue with LTVV. This finding could suggest that adherence to LTVV is not necessarily related to severity of diseases. Vice versa, a patient who starts ventilation with a too high VT is at risk of not receiving LTVV a later time point.
The present study has limitations. First, it is a secondary analysis of a study designed to evaluate the effectiveness of a multifaceted quality improvement strategy including a checklist in ICU. Thus, some important data regarding mechanical ventilation and patient severity are missing, like other ventilatory parameters, and the development of complications. Second, all included ICUs are from Brazil, and it is widely known that organizational factors and process of care differ worldwide. For example, in the present study only half of the patients were admitted to ICUs with board-certified intensivists on the morning and afternoon shifts [27, 28]. Indeed, the lower number of board-certified intensivists is a well-known problem in low-income countries [38]. Third, no information about the presence of ARDS is available and this could have influenced the adoption of LTVV and the impact of LTVV on hospital mortality. Indeed, in the here studied cohort the majority of the patients were extubated within 3 days, thus the percentage of patients with ARDS was probably low, which can partly explain the lack of power to detect any association between LTVV and mortality. Fourth, it is important to emphasize that current findings may only be generalizable to settings with a comparable infrastructure, especially the nurse-to-patient ratio, since Brazil has a much lower nurse-to-patient ratio then ICUs in, e.g., Europe and the US [22]. Finally, no information about the ventilatory mode was available, and this could have influenced the results.
Conclusions
In Brazil, the number of hospital beds, use of a structured checklist during multidisciplinary rounds, and presence of at least one nurse for every 10 patients in all shifts were the only organizational factors associated with adherence to LTVV. These findings shed light on organizational factors that may increase adherence to LTVV.
References
The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–8.
Determann RM, Royakkers A, Wolthuis EK, et al. Ventilation with lower tidal volumes as compared with conventional tidal volumes for patients without acute lung injury: a preventive randomized controlled trial. Crit Care. 2010;14:R1–14.
Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA. 2012;308:1651–9.
Serpa Neto A, Simonis FD, Barbas CS, et al. Lung-protective ventilation with low tidal volumes and the occurrence of pulmonary complications in patients without acute respiratory distress syndrome: a systematic review and individual patient data analysis. Crit Care Med. 2015;43:2155–63.
Serpa Neto A, Simonis FD, Barbas CS, et al. Association between tidal volume size, duration of ventilation, and sedation needs in patients without acute respiratory distress syndrome: an individual patient data meta-analysis. Intensive Care Med. 2014;40:950–7.
Writing Group for the PReVENT Investigators, Simonis FD, Serpa Neto A, et al. Effect of a low vs intermediate tidal volume strategy on ventilator-free days in intensive care unit patients without ARDS: a randomized clinical trial. JAMA. 2018;320:1872–80.
Bellani G, Laffey JG, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800.
Madotto F, Pham T, Bellani G, et al. Resolved versus confirmed ARDS after 24 h: insights from the LUNG SAFE study. Intensive Care Med. 2018;44:564–77.
Rackley CR, MacIntyre NR. Low tidal volumes for everyone? Chest. 2019;156:783–91.
Fan E, Del Sorbo L, Goligher EC, et al. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195:1253–63.
Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43:304–77.
Shrestha GS, Kwizera A, Lundeg G, et al. International Surviving Sepsis Campaign guidelines 2016: the perspective from low-income and middle-income countries. Lancet Infect Dis. 2017;17:893–5.
Fichtner F, Moerer O, Weber-Carstens S, et al. Clinical guideline for treating acute respiratory insufficiency with invasive ventilation and extracorporeal membrane oxygenation: evidence-based recommendations for choosing modes and setting parameters of mechanical ventilation. Respiration. 2019;98:357–72.
Esteban A, Anzueto A, Frutos F, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287:345–55.
Esteban A, Ferguson ND, Meade MO, et al. Evolution of mechanical ventilation in response to clinical research. Am J Respir Crit Care Med. 2008;177:170–7.
Esteban A, Frutos-Vivar F, Muriel A, et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med. 2013;188:220–30.
Schaefer MS, Serpa Neto A, Pelosi P, et al. Temporal changes in ventilator settings in patients with uninjured lungs: a systematic review. Anesth Analg. 2019;129:129–40.
Neto AS, Barbas CS, Simonis FD, et al. Epidemiological characteristics, practice of ventilation, and clinical outcome in patients at risk of acute respiratory distress syndrome in intensive care units from 16 countries (PRoVENT): an international, multicentre, prospective study. Lancet Respir Med. 2016;4:882–93.
Cavalcanti AB, Bozza FA, Machado FR, et al. Effect of a quality improvement intervention with daily round checklists, goal setting, and clinician prompting on mortality of critically ill patients: a randomized clinical trial. JAMA. 2016;315:1480–90.
Sasichay-Akkadechanunt T, Scalzi CC, Jawad AF. The relationship between nurse staffing and patient outcomes. J Nurs Adm. 2003;33:478–85.
Needleman J, Buerhaus P, Mattke S, et al. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346:1715–22.
Sakr Y, Moreira CL, Rhodes A, et al. The impact of hospital and ICU organizational factors on outcome in critically ill patients. Crit Care Med. 2015;43:519–26.
Radosevich MA, Wanta BT, Meyer TJ, et al. Implementation of a goal-directed mechanical ventilation order set driven by respiratory therapists improves compliance with best practices for mechanical ventilation. J Intensive Care Med. 2019;34:550–6.
Taniguchi C, Carnieli-Cazati D, Timenetsky KT, et al. Implementation of an educational program to decrease the tidal volume size in a general intensive care unit: a pilot study. Intensive Care Med. 2016;42:1185–6.
Treggiari MM, Martin DP, Yanez ND, et al. Effect of intensive care unit organizational model and structure on outcomes in patients with acute lung injury. Am J Respir Crit Care Med. 2007;176:685–90.
Cooke CR, Watkins TR, Kahn JM, et al. The effect of an intensive care unit staffing model on tidal volume in patients with acute lung injury. Crit Care Med. 2008;12:R134.
Soares M, Bozza FA, Angus DC, et al. Organizational characteristics, outcomes, and resource use in 78 Brazilian intensive care units: the ORCHESTRA study. Intensive Care Med. 2015;41:2149–60.
Nassar AP, Zampieri FG, Salluh JI, et al. Organizational factors associated with target sedation on the first 48 h of mechanical ventilation: an analysis of checklist-ICU database. Crit Care. 2019;23:34.
Machado F, Bozza F, Ibrain J, et al. A cluster randomized trial of a multifaceted quality improvement intervention in Brazilian intensive care units: study protocol. Implement Sci. 2015;10:8.
Wallace DJ, Seymour CW, Kahn JM. Hospital-level changes in adult ICU bed supply in the United States. Crit Care Med. 2017;45:e67–76.
Loux SL, Payne SMC, Knott A. Comparing Patient Safety in Rural Hospitals by Bed Count. In: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in patient safety: from research to implementation (Volume 1: Research Findings). Rockville (MD): Agency for Healthcare Research and Quality (US); 2005.
Stowell A, Claret PG, Sebbane M, et al. Hospital out-lying through lack of beds and its impact on care and patient outcome. Scand J Trauma Resusc Emerg Med. 2013;21:17.
Umoh NJ, Fan E, Mendez-Tellez PA, et al. Patient and intensive care unit organizational factors associated with low tidal volume ventilation in acute lung injury. Crit Care Med. 2008;36:1463–8.
Ellis SM, Dainty KN, Munro G, et al. Use of mechanical ventilation protocols in intensive care units: a survey of current practice. J Crit Care. 2012;27:556–63.
Lomas J, Anderson GM, Domnick-Pierre K, et al. Do practice guidelines guide practice? The effect of a consensus statement on the practice of physicians. N Engl J Med. 1989;321:1306–11.
Zampieri FG, Salluh JI, Azevedo LC, et al. ICU staffing feature phenotypes and their relationship with patients’ outcomes: an unsupervised machine learning analysis. Intensive Care Med. 2019;45:1599–607.
Lanspa MJ, Peltan ID, Jacobs JR, et al. Driving pressure is not associated with mortality in mechanically ventilated patients without ARDS. Crit Care. 2019;23:424.
Arabi YM, Phua J, Koh Y, et al. Structure, organization, and delivery of critical care in Asian ICUs. Crit Care Med. 2016;44:e940–8.
Acknowledgements
CHECKLIST ICU–investigators Cardioeste: Pedro Aniceto Nunes Neto, Carlos Alberto Fernandes, Cristiano Ávila Luchesi; Casa de Saúde Santa Marta: Natalia Rodrigues de Sa, Roberta Antunes Faria Rodrigues, Larissa Stefany Radespiel; Casa de Saúde São Bento: Vinicius Leonardo dos Santos Iorio, Danielle Bhering, Viviane Ribeiro Linhares; Centro Hospitalar Unimed: Glauco Adrieno Westphal, Geonice Sperotto; Complexo Hospitalar São Mateus: Soraya Byana Rezende da Silva Rossi, Thaismari Escarmanhani Ferreira; Fundação Hospital de Clinicas Gaspar Vianna: Edgar de Brito Sobrinho, Helder Jose Lima Reis, Mauricio Soares Carneiro, Adriana de Oliveira Lameira Veríssimo; Fundação Hospital Getúlio Vargas: Juliana Fernandez Fernandes, Rodrigo Lopes Ferreira; Hospital Aristides Maltez: Sylvania Campos Pinho, Leonardo Dultra, Lise Oliveira Hizumi; Hospital Aviccena: Neiva Fernandes de Lima, Alexsandra Raimunda da Silva, Liliane dos Santos; Hospital Casa de Caridade de Carangola: Sidiner Mesquita Vaz, José Marcio Oliveira, Miria Bonjour Laviola; Hospital Casa de Portugal: Wania Vasconcelos de Freitas, Leonardo Passos; Hospital Copa D’Or: Ligia Sarmet Cunha Farah Rabello, Carollina Resende de Siqueira; Hospital da Sagrada Familia: Luiz Carlos de Oliveira Silva, Francisco Felix Barreto Junior, Eduarda Maria Alves Cruz; Hospital das Clinicas–FMUSP: Luiz Marcelo Sa Malbouisson, Fabiola Prior Caltabeloti, Estevão Bassi, Patrícia Regiane da Silva, Filipe Cadamuro, Renata Graciliano dos Santos Cagnon, Yeh-Li Ho, Lucas Chaves Neto, Bruno Azevedo Randi; Hospital das Clinicas da UFPE: Michele Maria Goncalves de Godoy, Pollyanna Dutra Sobral, Evônio de Barros Campelo Júnior; Hospital das Clínicas da Faculdade de Medicina de Botucatu/UNESP: Laercio Martins de Stefano, Ana Lucia Gut, Greicy Mara Mengue Feniman de Stefano; Hospital das Clinicas de Goiás: Denise Milioli Ferreira, Fernanda Alves Ferreira Gonçalves; Hospital das Clinicas Luzia de Pinho Melo–SPDM: Fernanda Rubia Negrao Alves, Wilson Nogueira Filho, Renata Ortiz Marchetti; Hospital de Base do Distrito Federal: Sheila Sa, Nadia Tomiko Anabuki; Hospital de Clinicas de Porto Alegre: Silvia Regina Rios Vieira, Edino Parolo, Karen Prado, Natalia Gomes Lisboa; Hospital de Messejana Dr Carlos Alberto Studart Gomes: Simone Castelo Branco Fortaleza, Maria Liduina Nantua Beserra Porfirio, Marcela Maria Sousa Colares; Hospital de Urgência e Emergência de Rio Branco: Rosicley Souza da Silva, Marcia Vasconcelos, Fabio de Souza; Hospital Distrital Dr Evandro Ayres de Moura: Lanese Medeiros de Figueiredo, Niedila Pinheiro Bastos Seabra, Paula Celia Pires de Oliveira; Hospital do Coração Balneário Camboriú: Marcio Andrade Martins, Ricardo Beduschi Muller, Manoela Cristina Recalcatti; Hospital e Pronto Socorro Dr Aristóteles Platao Bezerra de Araújo: Riani Helenditi Fernandes Camurça Martins, Leatrice Emilia Ferreira de França; Hospital Eduardo de Menezes: Frederico Bruzzi de Carvalho, Gustavo Cesar Augusto Moreira; Hospital Estadual Américo Brasiliense: Evelin Drociunas Pacheco Cechinatti, Aline Cristina Passos, Mariana da Costa Ferreira; Hospital Estadual Getúlio Vargas–Secretaria de Estado de Saúde: Antonio Carlos Babo Rodrigues, Vladimir dos Santos Begni; Hospital Estadual Monsenhor Walfredo Gurgel: Alfredo Maximo Grilo Jardim, Amanda Carvalho Maciel; Hospital Evangélico de Cachoeira de Itapemirim: Marlus Muri Thompson, Erica Palacio Berçacola Pinheiro, Claudio Henrique Pinto Gonçalves; Hospital Federal da Lagoa: Ricardo Schilling Rosenfeld, Valéria Abrahao Rosenfeld, Leticia Japiassú; Hospital Federal Servidores do Estado: Maria Inês Pinto de Oliveira Bissoli, Rosemary da Costa Tavares, Marta Rocha Gonçalves; Hospital Fernandes Tavora: Laercia Ferreira Martins, Maria Helena Oliveira, Adriana Kelly Almeida Ferreira; Hospital Geral de Camaçari: Emídio Jorge Santos Lima, Tárcio de Almeida Oliveira, Milena Teixeira Campos; Hospital Geral de Fortaleza: Nilce Almino de Freitas, Stephanie Wilkes da Silva, Vera Lucia Bento Ferreira; Hospital Geral de Nova Iguaçu: Alexander de Oliveira Sodré, Cid Leite Villela, Eduardo Duque Estrada Medeiros; Hospital Geral de Palmas: Nairo Jose de Souza Junior, Jhocrenilcy de Souza Maya Nunes, Rones de Souza Monteiro; Hospital Guilherme Álvaro: André Scazufka Ribeiro, Carlos Cesar Nogueira Giovanini, Elisete Tavares Carvalho; Hospital Instituto Dr Jose Frota: Lenise Castelo Branco Camurça Fernandes, Domitilha Maria Coelho Rocha, Cristiane Maria Gadelha de Freitas; Hospital Joari: Marcia Adélia de Magalhaes Menezes, Rosa Imaculada Stancato, Guilherme Brenande Alves Faria, Giovanna Asturi; Hospital Maternidade e Pronto Socorro Santa Lucia: Ricardo Reinaldo Bergo, Frederico Toledo Campo Dall’Orto, Gislayne Rogante Ribeiro; Hospital Maternidade Municipal Dr Odelmo Leão Carneiro: Cidamaiá Aparecida Arantes, Michelle Aparecida dos Santos Toneto; Hospital Moinhos de Vento: Cassiano Teixeira, Juçara Gasparetto Maccari; Hospital Municipal Dr Carmino Caricchio: Sergio Tadeu Górios, Julliana Pires de Morais, Daniela Marangoni Zambelli; Hospital Municipal de Paracatu: Roberta Machado de Souza, Eduardo Cenísio Teixeira de Paiva, Alessandra Gonçalves Ribeiro; Hospital Municipal Dr Mario Gatti: Marcus Vinicius Pereira, Leoni Nascimento, Rosangela da Silva; Hospital Municipal Padre Germano Lauck de Foz do Iguaçu: Roberto de Almeida, Karin Aline Zilli Couto, Izabella Moroni Toffolo; Hospital Municipal Pedro II: Jorge Eduardo da Rocha Paranhos, Antonio Ricardo Paixão Fraga; Hospital Municipal Souza Aguiar: Alberto Augusto de Oliveira Junior, Roberto Lannes, Andrea da Silva Gomes Ludovico; Hospital Naval Marcilio Dias: Luiz Fernando Costa Carvalho, Leticia de Araújo Campos, Patricia Soboslai; Hospital Nereu Ramos: Israel Silva Maia, Tatiana Rassele, Christiany Zanzi; Hospital Nossa Senhora Auxiliadora: Valeria Nunes Martins Michel, Sinésio Pontes Gonçalves; Hospital Nossa Senhora dos Prazeres: Ricardo Rath de Oliveira Gargioni, Rosangela Zen Duarte; Hospital 9 de Julho: Mariza D’Agostino Dias, Andrea Delfini Diziola, Daniela Veruska da Silva, Melissa Sayuri Hagihara; Hospital Primavera: André Luís Veiga de Oliveira, Diego Leonnardo Reis, Janaina Feijó; Hospital Procordis: Marco Antonio da Costa Oliveira, Luiza Veiga Coelho de Souza; Hospital Pronto Socorro 28 de Agosto: Liane de Oliveira Cavalcante, Jacilda Rodrigues, Moises Cruz de Pinho; Hospital Regional da Unimed Fortaleza: Marcos Antonio Gadelha Maia, Vladia Fabiola Jorge Lima, Emilianny Maria Nogueira, Antonielle Carneiro Gomes; Hospital Regional de Juazeiro: Katia Regina de Oliveira, Jose Antonio Bandeira, Carla Cordeiro Botelho Mesquita; Hospital Universitário Regional dos Campos Gerais: Guilherme Arcaro, Camila Wolff, Délcio Caran Bertucci Filho; Hospital Regional de Presidente Prudente: Gustavo Navarro Betonico, Rafaela Pereira Maroto, Leonardo Fantinato Menegon; Hospital Regional Deputado Manoel Gonçalves Abrantes: Patrício Junior Henrique da Silveira, Germana Estrela Gadelha de Queiroga Oliveira, Wallber Moreno da Silva Lima; Hospital Regional Público do Araguaia: Lilian Batista Nunes, Sotero Gonçalves Martins Neto, Liwcy Keller de Oliveira Lopes Lima; Hospital Regional João Penido: Maria Augusta de Mendonça Lima, Lidiane Miranda Milagres, Vivian Gribel D’Ávila; Hospital Santa Casa de Campo Mourão: Paulo Marcelo Schiavetto, Paulo Alves dos Santos, Francislaine de Matos Raimundo; Hospital Municipal Santa Isabel–Joao Pessoa: Carmen Leonilia Tavares de Melo, Aline Albuquerque de Carvalho, Cynthia Franca de Santana; Hospital Santa Lucia de Divinópolis: Adriana Lessa Ventura Fonseca, Martha Aparecida da Silva; Hospital Santa Rosa: Mara Lilian Soares Nasrala, Eloisa Kohl Pinheiro, Mara Regina Pereira Santos; Hospital Municipal São Francisco de Assis: Guilherme Abdalla da Silva, Rener Moreira, Marcia Loureiro Sebold; Hospital São Joao de Deus: Marcone Lisboa Simões da Rocha, Marco Antonio Ribeiro Leão, Jaqueline de Assis; Hospital São Jose–Criciúma: Felipe Dal Pizzol, Cristiane Damiani Tomasi; Hospital São Jose de Doenças Infecciosas: Jose Nivon da Silva, Luciana Vladia Carvalhedo Fragoso, Denise Araújo Silva Nepomuceno Barros; Hospital São Jose de Teresópolis: Mauricio Mattos Coutinho, Robson Sobreira Pereira, Veronica Oliveira dos Santos; Hospital São Jose do Avaí: Sergio Kiffer Macedo, Diego de Souza Bouzaga Furlani, Eduardo Silva Aglio Junior; Hospital São Paulo: Aécio Flavio Teixeira de Góis, Kathia Teixeira, Paula Zhao Xiao Ping; Hospital São Vicente de Paula–Cruz Alta: Paulo Ricardo Nazario Viecili, Simone Daniela Melo de Almeida; Hospital São Vicente de Paulo–Vitória da Conquista: Geovani Moreno Santos Junior, Djalma Novaes Araújo Segundo, Marielle Xavier Santana; Hospital São Vicente de Paulo–Passo Fundo: Jose Oliveira Calvete, Luciana Renner; Hospital Unimed Bebedouro: Vinicius Vandré Trindade Francisco, Danytieli Silva de Carvalho, Adriana Neri da Silva Batista Campos; Hospital Unimed Costa do Sol: Sergio Leôncio Fernandes Curvelo Jr, Nayara Ribas de Oliveira, Suelem de Paula Freitas Deborssan; Hospital Unimed Maceió: Maria Raquel dos Anjos Silva Guimaraes, Luiz Claudio Gomes Bastos, Luciene Moraes Gomes; Hospital Unimed Natal: Erico de Lima Vale, Dionísia Arianne Vieira da Silva; Hospital Unimed Rio: Renato Vieira Gomes, Marco Antonio Mattos, Pedro Miguel Matos Nogueira, Viviane Cristina Caetano Nascimento; Hospital Universitário–Universidade Estadual de Londrina: Cintia Magalhaes Carvalho Grion, Alexsandro Oliveira Dias, Glaucia de Souza Omori Maier; Hospital Universitário Cassiano Antonio Moraes–Universidade Federal do Espirito Santo: Paula Frizera Vassallo, Maria Helena Buarque Souza de Lima, Wyllyam Loss dos Reis, Walace Lirio Loureiro, Andressa Tomazini Borghardt; Hospital Universitário Lauro Wanderley: Ciro Leite Mendes, Paulo Cesar Gottardo, Jose Melquiades Ramalho Neto; Hospital Universitário Onofre Lopes: Eliane Pereira da Silva, Maria Gorette Lourenço da Silva Aragao, Elisângela Maria de Lima; Hospital Universitário Polydoro Ernani de São Thiago–Universidade Federal de Santa Catarina: Rafael Lisboa de Souza, Ken Sekine Takashiba; Hospital Universitário Prof. Edgar Santos–Universidade Federal da Bahia: Dimitri Gusmão-Flores, Taciana Lago Araújo, Rosana Santos Mota; Hospital Universitário Regional de Maringá: Almir Germano, Flavia Antunes, Sandra Regina Bin Silva; Hospital Universitário São Francisco de Paula–Pelotas: Marcio Osório Guerreiro, Marina Peres Bainy, Patrícia de Azevedo Duarte Hardt; Hospital Vila da Serra–Instituto Materno Infantil de Minas Gerais: Hugo Correa de Andrade Urbano, Camila Amurim de Souza; Hospital Vivalle: Claudia Mangini, Fernando Jose da Silva Ramos, Luany Pereira de Araújo; Instituto Nacional de Infectologia Evandro Chagas/Fiocruz: André Miguel Japiassú, Denise Machado Medeiros, Michele Fernanda Borges da Silva; Irmandade da Santa Casa de Misericórdia de São Paulo: Fabiano Hirata, Roberto Marco, Elzo Peixoto; Irmandade do Hospital Nossa Senhora das Dores: Marcio Luiz Fortuna Esmeraldo, Leide Aparecida Damásio Pereira, Raquel Carvalho Leal; Irmandade Santa Casa de Misericórdia de Maringá: Paulo Roberto Aranha Torres, Maricy Morbin Torres; Santa Casa de Belo Horizonte: Mara Rubia de Moura, Claudio Dornas de Oliveira, Andressa Siuves Gonçalves Moreira, Brisa Emanuelle Silva Ferreira, Carolina Leticia dos Santos Cruz, Patrícia Moreira Soares, Paulo Cesar Correia, Lorena Lina Silva Almeida; Santa Casa de Caridade de Diamantina: Marcelo Ferreira Sousa, Andrey Antonio Santiago Vial, Marcia Maria Ferreira Souza; Santa Casa de Misericórdia de Anapolis: Diogo Quintana, Ana Cecilia Barbosa Guimaraes, Maria Dolores Menezes Diniz; Santa Casa de Misericórdia de Feira de Santana: Paulo Henrique Panelli Ferreira, Rosa Maria Rios Santana Cordeiro, Murilo Oliveira da Cunha Mendes; Santa Casa de Misericórdia de Guaxupé: Sergio Oliveira de Lima, Silvia Aparecida Bezerra, Aurélia Baquiao dos Reis da Silva; Santa Casa de Misericórdia de Pelotas: Cristiano Correa Batista, Thaís Neumann, Rafael Olivé Leite; Santa Casa de Misericórdia de Porto Alegre: Thiago Costa Lisboa, Martha Hädrich, Edison Moraes Rodrigues Filho; Santa Casa de Misericórdia de São Joao Del Rei: Jorge Luiz da Rocha Paranhos, Carlos Henrique Nascimento dos Santos, Hélia Cristina de Souza; Sociedade Beneficente Hospitalar Maravilha: Robson Viera de Souza, Jose Luís Toribio Cuadra, Jonas Spanholi; Unidade de Emergência, Hospital das Clinicas de Ribeirão Preto–FMRP-USP: Marcos de Carvalho Borges, Wilson Jose Lovato, Tania Mara Gomes, Luís Artur Mauro Witzel Machado; Hospital de Clinicas–Universidade Estadual de Campinas: Thiago Martins Santos, Marco Antonio de Carvalho Filho, Karina Aparecida Garcia Bernardes; Vila Velha Hospital: Jose Roberto Pereira Santos, Aline Esteves Mautoni Queiroga Liparizi, Patrícia Venturim Lana; Vitoria Apart Hospital: Claudio Piras, Luiz Virgílio Nespoli, Aparecida Silva Taliule.
CHECKLIST ICU—Checklist During Multidisciplinary Visits for Reduction of Mortality in Intensive Care Units.
Funding
This study was conducted as part of the Program to Support Institutional Development of Universal Health System (PROADI) from the Brazilian Ministry of Health. It was funded mainly by the Brazilian Health Surveillance Agency (ANVISA), PROADI, and Brazilian Development Bank (BNDES). D’Or Institute for Research and Education also contributed with additional funding.
Author information
Authors and Affiliations
Consortia
Contributions
TDM participated in the study design and concept, organized the dataset, conducted the statistical analyses and drafted the manuscript. FAB participated in the study design and concept, conduction of the original study, and drafted the manuscript. FRM participated in the study design and concept, conduction of the original study, and drafted the manuscript. HPG participated in the study design and concept, conduction of the original study, and drafted the manuscript. JIS participated in the study design and concept, conduction of the original study, and drafted the manuscript. APN participated in the study design and concept, conduction of the original study, and drafted the manuscript. KN-S participated in the study design and concept, conduction of the original study, and drafted the manuscript. MJS participated in the study design and concept, drafted the manuscript and supervised the study. ABC participated in the study design and concept, conduction of the original study, drafted the manuscript and supervised the study. ASN participated in the study design and concept, organized the dataset, conducted the statistical analyses, drafted the manuscript and supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Online Supplement.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Midega, T.D., Bozza, F.A., Machado, F.R. et al. Organizational factors associated with adherence to low tidal volume ventilation: a secondary analysis of the CHECKLIST-ICU database. Ann. Intensive Care 10, 68 (2020). https://doi.org/10.1186/s13613-020-00687-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-020-00687-3