Abstract
Purpose
To study whether ICU staffing features are associated with improved hospital mortality, ICU length of stay (LOS) and duration of mechanical ventilation (MV) using cluster analysis directed by machine learning.
Methods
The following variables were included in the analysis: average bed to nurse, physiotherapist and physician ratios, presence of 24/7 board-certified intensivists and dedicated pharmacists in the ICU, and nurse and physiotherapist autonomy scores. Clusters were defined using the partition around medoids method. We assessed the association between clusters and hospital mortality using logistic regression and with ICU LOS and MV duration using competing risk regression.
Results
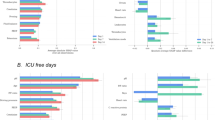
Analysis included data from 129,680 patients admitted to 93 ICUs (2014–2015). Three clusters were identified. The features distinguishing between the clusters were: the presence of board-certified intensivists in the ICU 24/7 (present in Cluster 3), dedicated pharmacists (present in Clusters 2 and 3) and the extent of nurse autonomy (which increased from Clusters 1 to 3). The patients in Cluster 3 exhibited the best outcomes, with lower adjusted hospital mortality [odds ratio 0.92 (95% confidence interval (CI), 0.87–0.98)], shorter ICU LOS [subhazard ratio (SHR) for patients surviving to ICU discharge 1.24 (95% CI 1.22–1.26)] and shorter durations of MV [SHR for undergoing extubation 1.61(95% CI 1.54–1.69)]. Cluster 1 had the worst outcomes.
Conclusion
Patients treated in ICUs combining 24/7 expert intensivist coverage, a dedicated pharmacist and nurses with greater autonomy had the best outcomes. All of these features represent achievable targets that should be considered by policy makers with an interest in promoting equal and optimal ICU care.



Similar content being viewed by others
References
Soares M, Bozza FA, Angus DC, Japiassú AM, Viana WN, Costa R, Brauer L, Mazza BF, Corrêa TD, Nunes AL, Lisboa T, Colombari F, Maciel AT, Azevedo LC, Damasceno M, Fernandes HS, Cavalcanti AB, do Brasil PE, Kahn JM, Salluh JI (2015) Organizational characteristics, outcomes, and resource use in 78 Brazilian intensive care units: the ORCHESTRA study. Intensive Care Med 41(12):2149–2160
Soares M, Bozza FA, Azevedo LC, Silva UV, Corrêa TD, Colombari F, Torelly AP, Varaschin P, Viana WN, Knibel MF, Damasceno M, Espinoza R, Ferez M, Silveira JG, Lobo SA, Moraes AP, Lima RA, de Carvalho AG, do Brasil PE, Kahn JM, Angus DC, Salluh JI (2016) Effects of organizational characteristics on outcomes and resource use in patients with cancer admitted to intensive care units. J Clin Oncol 34(27):3315–3324
Sakr Y, Moreira CL, Rhodes A, Ferguson ND, Kleinpell R, Pickkers P, Kuiper MA, Lipman J, Vincent JL, Extended Prevalence of Infection in Intensive Care Study Investigators (2015) The impact of hospital and ICU organizational factors on outcome in critically ill patients: results from the extended prevalence of infection in intensive care study. Crit Care Med 43(3):519–526
Neuraz A, Guérin C, Payet C, Polazzi S, Aubrun F, Dailler F, Lehot JJ, Piriou V, Neidecker J, Rimmelé T, Schott AM, Duclos A (2015) Patient mortality is associated with staff resources and workload in the ICU: a multicenter observational study. Crit Care Med 43(8):1587–1594
Gershengorn HB, Harrison DA, Garland A, Wilcox ME, Rowan KM, Wunsch H (2017) Association of intensive care unit patient-to-intensivist ratios with hospital mortality. JAMA Intern Med 177(3):388–396
Wilcox ME, Chong CA, Niven DJ, Rubenfeld GD, Rowan KM, Wunsch H, Fan E (2013) Do intensivist staffing patterns influence hospital mortality following ICU admission? A systematic review and meta-analyses. Crit Care Med 41(10):2253–2274
Krapohl G, Manojlovich M, Redman R, Zhang L (2010) Nursing specialty certification and nursing-sensitive patient outcomes in the intensive care unit. Am J Crit Care 19(6):490–498
Sevransky JE, Checkley W, Herrera P, Pickering BW, Barr J, Brown SM, Chang SY, Chong D, Kaufman D, Fremont RD, Girard TD, Hoag J, Johnson SB, Kerlin MP, Liebler J, O’Brien J, O’Keefe T, Park PK, Pastores SM, Patil N, Pietropaoli AP, Putman M, Rice TW, Rotello L, Siner J, Sajid S, Murphy DJ, Martin GS, United States Critical Illness and Injury Trials Group-Critical Illness Outcomes Study Investigators (2015) Protocols and hospital mortality in critically ill patients: the United States critical illness and injury trials group critical illness outcomes study. Crit Care Med 43(10):2076–2084
Writing Group for the CHECKLIST-ICU Investigators and the Brazilian Research in Intensive Care Network (BRICNet), Cavalcanti AB, Bozza FA, Machado FR, Salluh JI, Campagnucci VP, Vendramim P, Guimaraes HP, Normilio-Silva K, Damiani LP, Romano E, Carrara F, de Lubarino Diniz Souza J, Silva AR, Ramos GV, Teixeira C, da Brandão Silva N, Chang CC, Angus DC, Berwanger O (2016) Effect of a quality improvement intervention with daily round checklists, goal setting, and clinician prompting on mortality of critically ill patients: a randomized clinical Trial. JAMA 315(14):1480–1490
Kim MM, Barnato AE, Angus DC, Fleisher LA, Kahn JM (2010) The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med 170(4):369–376
Rose L, Nelson S, Johnston L, Presneill JJ (2007) Decisions made by critical care nurses during mechanical ventilation and weaning in an Australian intensive care unit. Am J Crit Care 16(5):434–443
Hirzallah FM, Alkaissi A, do Céu Barbieri-Figueiredo M (2019) A systematic review of nurse-led weaning protocol for mechanically ventilated adult patients. Nurs Crit Care 24(2):89–96
Larson GE, McKeever S (2018) Nurse titrated analgesia and sedation in intensive care increases the frequency of comfort assessment and reduces midazolam use in paediatric patients following cardiac surgery. Aust Crit Care 31(1):31–36
Radosevich MA, Wanta BT, Meyer TJ, Weber VW, Brown DR, Smischney NJ, Diedrich DA (2017) Implementation of a goal-directed mechanical ventilation order set driven by respiratory therapists improves compliance with best practices for mechanical ventilation. J Intensive Care Med 1:885066617746089
Fagoni N, Piva S, Peli E, Turla F, Pecci E, Gualdoni L, Fiorese B, Rasulo F, Latronico N (2018) Comparison between a nurse-led weaning protocol and weaning based on physician’s clinical judgment in tracheostomized critically ill patients: a pilot randomized controlled clinical trial. Ann Intensive Care 8(1):11
Zampieri FG, Soares M, Borges LP, Salluh JIF, Ranzani OT (2017) The Epimed Monitor ICU Database®: a cloud-based national registry for adult intensive care unit patients in Brazil. Rev Bras Ter Intensiva 29(4):418–426
Zampieri FG, Bozza FA, Moralez GM et al (2017) The effects of performance status 1 week before hospital admission on the outcomes of critically ill patients. Intensive Care Med 43:39–47
Moreno RP, Metnitz PG, Almeida E, Jordan B, Bauer P, Campos RA, Iapichino G, Edbrooke D, Capuzzo M, Le Gall JR, SAPS 3 Investigators (2005) SAPS 3–From evaluation of the patient to evaluation of the intensive care unit. Part 2: Development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med 31(10):1345–1355
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on sepsis-related problems of the European Society of intensive care medicine. Intensive Care Med 22(7):707–710
van der Maaten LJP, Hinton GE (2008) Visualizing high-dimensional data using t-SNE. J Mach Learn Res 9:2579–2605
Gray B. cmprsk: Subdistribution Analysis of Competing Risks. 2014. R package version 2.2-7. https://CRAN.R-project.org/package=cmprsk
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ 85(11):867–872
Orinovsky I, Raizman E (2018) Improvement of nutritional intake in intensive care unit patients via a nurse-led enteral nutrition feeding protocol. Crit Care Nurse 38(3):38–44
Al Ashry HS, Abuzaid AS, Walters RW, Modrykamien AM (2016) Effect of compliance with a nurse-led intensive care unit checklist on clinical outcomes in mechanically and nonmechanically ventilated patients. J Intensive Care Med 31(4):252–257
Armellino D, Quinn Griffin MT, Fitzpatrick JJ (2010) Structural empowerment and patient safety culture among registered nurses working in adult critical care units. J Nurs Manag 18(7):796–803
Fitzpatrick JJ, Campo TM, Graham G, Lavandero R (2010) Certification, empowerment, and intent to leave current position and the profession among critical care nurses. Am J Crit Care 19(3):218–226
Hauck A, Quinn Griffin MT, Fitzpatrick JJ (2011) Structural empowerment and anticipated turnover among critical care nurses. J Nurs Manag 19(2):269–276
Ganz FD, Raanan O, Khalaila R, Bennaroch K, Scherman S, Bruttin M, Sastiel Z, Fink NF, Benbenishty J (2013) Moral distress and structural empowerment among a national sample of Israeli intensive care nurses. J Adv Nurs 69(2):415–424
Papathanassoglou ED, Karanikola MN, Kalafati M, Giannakopoulou M, Lemonidou C, Albarran JW (2012) Professional autonomy, collaboration with physicians, and moral distress among European intensive care nurses. Am J Crit Care 21(2):e41–e52
Acknowledgements
This study was supported by the National Council for Scientific and Technological Development (CNPq), Carlos Chagas Filho Foundation for Research Support of the State of Rio de Janeiro (FAPERJ) and by departmental funds from the D’Or Institute for Research and Education. We dedicate this work to the memory of Dr. Dieter Eduardo Sielfeld Araya, ORCHESTRA Study investigator, who recently passed away.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
JIFS and MS are founders and proprietors of Epimed Solutions®. LPB is an employee of Epimed Solutions®. FGZ has received grant for an investigator-initiated clinical trial from Bactiguard®, Sweden, which is unrelated to the aspects of this work. The other authors report no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dieter E. S. Araya: In Memoriam.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zampieri, F.G., Salluh, J.I.F., Azevedo, L.C.P. et al. ICU staffing feature phenotypes and their relationship with patients’ outcomes: an unsupervised machine learning analysis. Intensive Care Med 45, 1599–1607 (2019). https://doi.org/10.1007/s00134-019-05790-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05790-z