Abstract
Background
Peripheral arterial disease (PAD) is a common cause of disability and mortality. The reconstruction of blood circulation presents to be the key to treatment, which can be achieved by surgery and interventional therapy. Since 40% patients have lost the chance for the therapy, a new method is needed to reduce the amputation and mortality rate for “no-option” patients. The objective of our systematic review and meta-analysis was to evaluate the efficacy and safety of autologous implantation of stem cells in patients with PAD critically, compared with active controls and placebo.
Methods
Randomized controlled trials (RCTs) of autologous implantation of stem cells compared with placebo and control for PAD were included. Electronic medical databases including MEDLINE, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL), the Chinese Biomedical Literature Database, China National Knowledge Infrastructure (CNKI), and ClinicalTrials.gov were searched from initial period to September 2018. Independently, two reviewers screened citations, extracted data, and assessed the risk of bias according to the criteria of the Cochrane handbook. The quality of evidence was evaluated by GRADE evidence profile. The primary outcomes consisted of amputation rate, major amputation rate, ulcer healing rate, and side effects. The second outcomes included ankle-brachial index (ABI), transcutaneous oxygen tension (TcO2), pain-free walking distance (PFWD), and rest pain score. Statistical analysis was conducted via RevMan 5.3 and Stata 12.0.
Results
According to the twenty-seven RCTs, 1186 patients and 1280 extremities were included and the majority of studies showed a high risk of bias. Meta-analysis indicated that autologous stem cell therapy was more effective than conventional therapy on the healing rate of ulcers [OR = 4.31 (2.94, 6.30)]. There was also significant improvement in ABI [MD = 0.13 (0.10, 0.17)], TcO2 [MD = 0.13 (0.10, 0.17)], and PFWD [MD = 178.25 (128.18, 228.31)] while significant reduction was showed in amputation rate [OR = 0.50 (0.36, 0.69)] and rest pain scores [MD = − 1.61 (− 2.01, − 1.21)]. But the result presented no significant improvement in major limb salvage [0.66 (0.42, 1.03)]. Besides, stem cell therapy could reduce the amputation rate [OR = 0.50 (0.06, 0.45] and improve the ulcer healing rate [OR = 4.34 (2.96, 6.38] in DM subgroup. Eight trials reported the side effects of autologous stem cell therapy, and no serious side effects related to stem cells were reported. GRADE evidence profile showed all the quality evidence of outcomes were low.
Conclusions
Based on the review, autologous stem cell therapy may have a positive effect on “no-option” patients with PAD, but presented no significant improvement in major limb salvage. However, the evidence is insufficient to prove the results due to high risk of bias and low-quality evidence of outcomes. Further researches of larger, randomized, double-blind, placebo-controlled, and multicenter trials are still in demand.
Similar content being viewed by others
Background
Peripheral arterial diseases (PAD), as a member of arteriosclerosis, mostly occur in lower extremity arteries. The morbidity of PAD generally ranged from 3 to 10%, but among the people over 60 years old, it can reach above 15% and it upregulates with aging [1]. PAD is one of the most serious complications in patients with diabetes mellitus (DM), and the overall prevalence is 21.2% in China [2]. If not properly treated in the early stage, it is very possible for the patient to suffer from critical limb ischemia (CLI) causing rest pain, ulcer, necrosis, and finally leading to amputation. The rate of amputation among PAD patients is about 1.6~4.1% with even much higher cardiovascular event incidence and mortality [3,4,5].
Patients with CLI are commonly treated conventionally at an early stage, such as risk factor control, exercise training, utilizing antiplatelet drugs, and vasodilator [6,7,8,9,10,11,12]. But the reconstruction of the blood circulation, which can be achieved by surgery and interventional therapy, presented to be the key to the treatment [13, 14]. A 5-year survival rate which was less than 50% determined a worrisome prognosis. And when both surgery and interventional therapy is not feasible, amputation may be the last choice of the patients. However, amputation has a high rate of mortality about 25~50%, of which 5~20% in perioperational period, and the re-amputation rate is up to 30% [15]. The risk is significantly raising in patients with DM, for the segmental and diffuse arterial disease as well as the higher risk of cardiovascular event. Since 40% patients have missed the chance for surgery or interventional therapy [16], a new method is in great demand to reduce the amputation and mortality rate for “no-option” patients.
Autologous stem cell therapy is gradually known as a new therapy. Asahara isolated endothelial progenitor cells (EPCs) from blood in 1997 [17]. EPCs are a type of adult stem cells, derived from adult bone marrow and is mainly found in the embryo, adult peripheral blood, umbilical cord blood, and bone marrow. EPCs can develop into endothelial cells and then promote revascularization. Methods for isolation of EPCs include magnetic bead selection, density gradient centrifugation, and differential adhesion method and so on. Many animal trials found improved blood flows in ischemic limbs after stem cell implantation [18,19,20,21]. Afterward, the therapies of stem cells have been applied to patients with PAD. The first trial in human called therapeutic angiogenesis using cell transplantation (TACT) was performed in Japan [22]. Since then, a growing body of evidence suggested that autologous stem cell therapy was more effective than standard care/conventional treatment for PAD [23]. Former systematic review pooled analysis of both randomized controlled trials (RCTs) and non-RCTs; however, studies of different designs cannot be assessed in unification. Therefore, in the present study, we updated the systematic review to evaluate the efficacy and safety of autologous implantation of stem cells for PAD.
Methods
We followed the recommendations from the Cochrane Collaboration for systematic review and meta-analysis of RCTs and reported according to preferred reporting items for systematic reviews and meta-analyses (PRISMA) statements [24].
Inclusion criteria and searching strategies
We searched RCTs involving patients with PAD who were treated with autologous implantation of all kinds of stem cells from electronic medical databases including MEDLINE, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL), the Chinese Biomedical Literature Database, China National Knowledge Infrastructure (CNKI), and ClinicalTrials.gov from initial period to September 2018. The MeSH terms were outlined in Additional file 1: Table S1.
Data extraction and bias assessment
Two investigators selected the studies and extracted data from studies independently. Controversy was resolved by discussion with a third investigator. Extracted data included basic information (author name, study year, country, sample size, design of study, follow-up time), characteristics of patients (sex, age, stage of PAD), methods, intervention details (type and number of stem cells, transplantation routine, intervention in control group), outcomes, and side effect. The bias of the trials included in our study was assessed according to the Cochrane Handbook for Interventions [25]. The components included allocation sequence generation, allocation concealment, blinding of participants, caregivers, outcome assessors and outcome adjudicators, incomplete outcome data, selective outcome reporting, and other sources of bias. For each item, studies were categorized as high, low, or unclear risk of bias.
Observation index
The primary outcomes consisted of amputation rate, major amputation rate, ulcer healing rate, and side effect. The second outcomes were ankle-brachial index (ABI), transcutaneous oxygen tension (TcO2), rest pain score, and pain-free walking distance (PFWD).
Statistical analysis
We performed a meta-analysis of all RCTs using the data from the cell therapy group and control group. Statistical analysis was conducted via RevMan 5.3 and Stata 12.0. Continuous and dichotomous outcome variables were respectively described as mean difference (MD) and odds ratios (OR) with 95% confidence intervals (CI), which were derived from Inverse Variance and Mantel-Haenszel estimate and summarized by Forest plots. Heterogeneity among studies was evaluated by the I2 parameter and chi-squared tests. Fixed effect model was used for meta-analysis when I2 values < 50% and random effect model when I2 values ≥ 50% as heterogeneity indicated. Incomplete outcome data were analyzed by intention to treat analysis. Sensitivity analyses were conducted to examine the difference between random and fixed effects model as to their effect measures such as OR, relative risk (RR), and risk difference (RD). We explored the publication bias by funnel plots (when the number of included studies more than 9) and Egger’s test for continuous endpoints and Harbord’s test for dichotomous endpoints.
The GRADE approach was used to evaluate the quality of evidence of each outcome, which was classified as high, moderate, low, and very low after the all-round assessment of study limitations, inconsistency, imprecision, indirectness, and publication bias [26].
Results
Study selection and characteristics
Among the 16,977 studies, 27 RCTs [22, 27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54] involving 1186 patients and 1280 limbs were included in our systematic review. The inclusion and exclusion flow was listed in flow Fig. 1. Among the 27 RCTs, 16 studies were from Asians [22, 27, 29,30,31,32,33,34,35, 37, 43,44,45, 48, 50, 54], 7 [28, 36, 38, 46, 49, 52, 53] from Europeans, and 4 [39,40,41,42, 47, 51] from Americans. Patients in the trials were identified as PAD or diabetic foot (DF) with different classifications. Stem cells, including BMMSCs, BMMNCs, BMAC, PBMNC, CD34+ cells, VesCell, PBMCs, and CD133+ cells, were transplanted by intramuscular injection [22, 27,28,29,30,31,32,33,34,35,36,37, 39,40,41,42,43,44,45,46,47,48,49,50,51, 53, 54] or intra-arterial injection [28, 38, 52]. The average follow-up time was 4.7 months (1–36 m). Details of studies were listed in Table 1.
Risk of bias
According to Cochrane Handbook, each risk of bias item for each included RCTs and each risk of bias item of all included RCTs were presented in Figs. 2 and 3. The figures showed high risk of bias mainly resulted from the lack of allocation concealment, absent blinding, and incomplete outcome data. Among the 27 RCTs, only 6 (22.2%) studies [22, 33, 43, 45, 46, 52] adequately generated the randomization sequence, 4 (14.8%) [22, 40, 45, 49] concealed allocation, 8 [22, 38, 40, 42, 43, 47, 51, 52] (29.6%) blinding of participants and personnel, and 10 (37.0%) [22, 29, 38, 40, 42, 43, 47, 48, 51, 52] blinding of outcome assessment. Twelve (44.4%) [22, 35, 37, 38, 40, 43, 47,48,49, 51, 53, 54] trials had no incomplete outcome data, and 22 (81.5%) [22, 27,28,29, 31, 32, 35,36,37,38, 40, 42, 43, 45,46,47,48,49,50,51,52,53] were free of selective outcome reporting.
Amputation rate
Among the 27 RCTs, 16 trials [27, 28, 31, 36, 38, 40, 42, 43, 46,47,48,49,50,51,52,53] reported the detailed amputation rate. The meta-analysis showed a lower amputation rate in cell therapy group compared with control (88/425 vs 142/444; OR 0.50, 95% CI 0.36 to 0.69, I2 = 11%)(Fig. 4).
Major amputation rate
Eight studies [39, 42, 47,48,49,50,51,52] reported the detailed major amputation rate. The meta-analysis showed a lower major amputation rate in the stem cell therapy group than control but with no statistical significance (49/232 vs. 60/197; OR 0.66, 95% CI 0.42 to 1.03, I2 = 0%) (Fig. 5).
Ulcer healing rate
Fourteen studies [27,28,29,30,31, 37, 42, 43, 45, 46, 48,49,50, 52] reported the detailed ulcer healing rate. The meta-analysis showed a higher ulcer healing rate in the cell therapy group compared with control (170/313 vs 90/310; OR 4.31, 95% CI 2.94 to 6.30, I2 = 17%) (Fig. 6).
ABI
Sixteen studies [22, 27, 29, 31, 33,34,35, 37, 43, 44, 46, 47, 49, 50, 53, 54] reported the detailed ABI. The meta-analysis showed higher ABI in the cell therapy group compared with control (MD 0.13, 95% CI 0.10 to 0.17, I2 = 69%) (Fig. 7).
TcO2
Eight studies [22, 29, 38, 43, 44, 46, 49, 54] reported the detailed TcO2. The meta-analysis showed higher TcO2 in the cell therapy group compared with control (MD 12.62, 95% CI 5.73to 19.51, I2 = 97%) (Fig. 8).
Rest pain score
Nine studies [27, 28, 31, 33, 34, 38, 43, 44, 46] reported the detailed rest pain score. The meta-analysis showed lower rest pain score in the cell therapy group compared with control (MD − 1.61, 95% CI − 2.01 to − 1.21, I2 = 92%) (Fig. 9).
Pain-free walking distance
Only three studies [27, 31, 32] reported detailed PFWD. The meta-analysis showed that PFWD in stem cell therapy group was higher than the control group (MD 178.25, 95% CI 128.18 to 228.31, I2 = 0%) (Fig. 10).
Subgroup analysis
Thirteen studies [27, 30,31,32,33,34,35, 43,44,45,46, 50, 54] included DM patients. The meta-analysis showed that stem cell therapy could reduce the amputation rate (3/109 vs 32/155; OR 0.17, 95% CI 0.06 to 0.45, I2 = 0%) (Additional file 2: Figure S1) and improve the ulcer healing rate (167/305 vs 89/304; OR 4.34, 95% CI 2.96 to 6.38, I2 = 23%) (Additional file 3: Figure S2) in DM patients.
Side effect association with cell therapy
Eight studies [22, 33, 37, 40, 42, 43, 47, 52] reported the side effect of stem cell therapy. Side effect included slight edema of limbs, transient increase of serum creatine phosphokinase, bleeding, pain, infection, and cellulitis after puncture or injection, hematocrit, proliferative retinopathy, moderate hypotension, and chest distress during mobilization and severe worsening of CLI in the target leg after injection. The most serious side effect was wound sepsis on the injected leg and with the ending of amputation. The detailed side events were showed in Additional file 4: Table S2.
Publication bias
The funnel plot and statistical test showed publication bias in amputation rate, major amputation rate, ABI, and no publication bias in ulcer healing rate, TcO2, rest pain score, and PFWD (Additional files 5, 6, 7, and 8: Figures S3-S6; Additional file 9: Table S3).
Sensitivity analyses
Results of sensitivity analyses were showed in Additional file 10: Table S4 and Additional file 11: Table S5. All the effect measures obtained by random effects do not significantly differ from those by the fixed effect model except for major amputation rate. RD derived from the random model differed from that in the fixed model.
Quality of evidence
GRADE evidence profile is showed in Table 2. All the quality evidence of outcomes were low. The low quality may due to inconsistency, imprecision, and publication bias.
Discussion
This meta-analysis indicated that autologous implantation of stem cells improved ulcer healing rate, ABI, TcO2, PFWD, and reduced amputation rate and rest pain score compared with standard care/conventional treatment. Stem cell therapy could reduce major amputation rate but with no statistical significance and seemingly no significant improvement in limb salvage (P = 0.64). Sensitivity analysis showed instability in the result of major amputation rate which may be related to small sample size and publication bias. Stem cell therapy could reduce amputation rate and improve ulcer healing rate in DM subgroup. The results suggested that stem cell therapy may alter the outcome of intractable CLI to a certain degree.
To our knowledge, this is the systematic review including the most RCTs of autologous implantation of stem cells for PAD up to now. We excluded one study [55] included in the previous systematic review [23]. The study used allogeneic bone marrow-derived mesenchymal stem cell for implantation, which did not meet the inclusion criteria. But we included nine studies that were not analyzed in the previous systematic review. The study of Tateishi-Yuyama reported two parts of the experiment and one is RCT [22]. The other eight studies [30, 33,34,35, 37, 44, 45, 53] also met the inclusion criteria in every way but were not included in the previous systematic review. In addition, the previous systematic reviews did secondary analysis including non-RCTs and RCTs, but studies of different designs should not be analyzed in a combined manner. In this case, we believe that our results are more reliable than the previous ones. Besides, we are the first to perform the subgroup analysis for patients with DM who bear the increased risk of PAD, segmental and diffuse arterial disease, and cardiovascular event. Most DM patients are not suitable for surgery or interventional therapy, and they may benefit from stem cell therapy.
Our study showed only one serious side effect related to the implantation of stem cells which shall remind us of the importance of aseptic technique during the injection. Due to the short follow-up, a full understanding of the side effect of stem cell implantation calls for further study. There were some observational studies reporting a serious side effect of stem cell therapy. Horie has reported heart failure, myocardial infarction, severe infection, and stroke post-cell therapy [56]. Moreover, the relationship between the tumor and stem cell therapy remains disputable. Among the 162 patients receiving stem cell implantation in Horie’s study [56], 9 patients had malignant tumor during 24.6 months follow-up. Two patients were diagnosed with a malignant tumor before the study, and the other 7 patients developed a small intestinal tumor, pancreatic cancer, lung cancer, gallbladder carcinoma, gastric cancer, and groin tumor. But this was an observational study and there is no direct cause-and-effect relationship between those events and stem cells therapy. Thus, RCTs of large sample size and longer follow-up time are needed to verify the safety of cell therapy.
There are several limitations in our study. Firstly, most trials have a high or unclear risk of bias so the trials may be underpowered. Low quality of methodology mainly results from inadequate sequence generation, lack of allocation concealment, absent blinding, and incomplete outcome data. Some RCTs mentioned “random” but did not report the specific randomization method. Some RCTs did not use allocation concealment and blinding method. Secondly, several studies had a small sample size and limited information for outcomes, such as adverse events. Thirdly, the included patients, types of stem cells, methods of transplantation, control group, and follow-up time were different among RCTs, which may lead to heterogeneity. The patients in the included studies were identified as having PAD or DF according to a different classification. There were eight types of stem cells including BMMSCs, BMMNCs, BMAC, PBMNC, CD34+ cells, VesCell, PBMCs, and CD133+ cells in our studies. Stem cells were transplanted by intramuscular injection or intra-arterial injection. Besides, the number of stem cells used varied among RCTs and part of studies did not report the number of transplanted stem cells. Stem cells used in the included studies may be the major cause of heterogeneity. Thus, standardization in the transplantation method, stem cell type, and quantity should be valued in transplantation. Treatments in control groups contain non-mobilized peripheral blood mononuclear cells, conventional treatment, and placebo. Follow-up time ranged from 1 to 36 months. These differences lead to great heterogeneity in meta-analysis of ABI, TcO2 and rest pain score. Twenty-seven RCTs included in this study all reported positive results, and we only included studies in English and Chinese, which may lead to publication bias.
Conclusions
The “no-option” patients with PAD may benefit from stem cells therapy, but there was seemingly no significant improvement in major limb salvage. Due to the low-quality evidence, further researches including larger, randomized, double-blinded, placebo-controlled, multicenter trials with long-term follow-up of high quality are still in demand to prove the efficacy and safety of stem cells therapy for PAD.
Abbreviations
- ABI:
-
Ankle-brachial index
- CENTRAL:
-
Cochrane Central Register of Controlled Trials
- CI:
-
Confidence intervals
- CLI:
-
Critical limb ischemia
- CNKI:
-
China National Knowledge Infrastructure
- DF:
-
Diabetic foot
- DM:
-
Diabetes mellitus
- EPC:
-
Endothelial progenitor cell
- MD:
-
Mean difference
- OR:
-
Odds ratios
- PAD:
-
Peripheral arterial disease
- PFWD:
-
Pain-free walking distance
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- RCT:
-
Randomized controlled trial
- RD:
-
Risk difference
- RR:
-
Relative risk
- SMD:
-
Standard mean difference
- TACT:
-
Therapeutic angiogenesis using cell transplantation
- TcO2 :
-
Transcutaneous oxygen tension
References
Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004;110(6):738–43.
Zhang X, Ran X, Xu Z, Cheng Z, Shen F, Yu Y, et al. Epidemiological characteristics of lower extremity arterial disease in Chinese diabetes patients at high risk: a prospective, multicenter, cross-sectional study. J Diabetes Complicat. 2018;32(2):150–6.
Leng GC, Lee AJ, Fowkes FG, Whiteman M, Dunbar J, Housley E, et al. Incidence, natural history and cardiovascular events in symptomatic and asymptomatic peripheral arterial disease in the general population. Int J Epidemiol. 1996;25(6):1172–81.
Steg PG, Bhatt DL, Wilson PW, D'Agostino R Sr, Ohman EM, Röther J, et al. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297(11):1197–206.
Heald CL, Fowkes FG, Murray GD, Price JF. Ankle Brachial Index CollaborationRisk of mortality and cardiovascular disease associated with the ankle-brachial index: systematic review. Atherosclerosis. 2006;189(1):61–9.
Steffen LM, Duprez DA, Boucher JL, Ershow AG, Hirsch AT. Management of peripheral arterial disease. Diabetes Spectr. 2008;21(3):171–7.
Feringa HH, van Waning VH, Bax JJ, Elhendy A, Boersma E, Schouten O, et al. Cardioprotective medication is associated with improved survival in patients with peripheral arterial disease. J Am Coll Cardiol. 2006;47(6):1182–7.
Sobel M, Verhaeghe R. Antithrombotic therapy for peripheral artery occlusive disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest. 2008;133(6 Suppl):815S–43S.
Fokkenrood HJ, Bendermacher BL, Lauret GJ, Willigendael EM, Prins MH, Teijink JA. Supervised exercise therapy versus non-supervised exercise therapy for intermittent claudication. Cochrane Database Syst Rev. 2013;23(8):CD005263.
Robertson L, Andras A. Prostanoids for intermittent claudication. Cochrane Database Syst Rev. 2013;30(4):CD000986.
Lièvre M, Morand S, Besse B, Fiessinger JN, Boissel JP. Oral Beraprost sodium, a prostaglandin I (2) analogue, for intermittent claudication: a double-blind, randomized, multicenter controlled trial. Circulation. 2000;102(4):426–31.
Thompson PD, Zimet R, Forbes WP, Zhang P. Meta-analysis of results from eight randomized, placebo-controlled trials on the effect of cilostazol on patients with intermittent claudication. Am J Cardiol. 2002;90(12):1314–9.
Bradbury AW, Adam DJ, Bell J, Forbes JF, Fowkes FG, Gillespie I, et al. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Health Technol Assess. 2010;14(14):1–210 iii-iv.
Frangogiannis NG. Cell therapy for peripheral artery disease. Curr Opin Pharmacol. 2018;39:27–34.
Sprengers RW, Moll FL, Verhaar MC. Stem cell therapy in PAD. Eur J Vasc Endovasc Surg. 2010;39(Suppl 1):S38–43.
Das AK. Stem cell therapy for critical limb ischaemia - a review. Indian J Surg. 2009;71(4):177–81.
Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997;275(5302):964–7.
Takahashi T, Kalka C, Masuda H, Chen D, Silver M, Kearney M, et al. Ischemia- and cytokine-induced mobilization of bone marrow-derived endothelial progenitor cells for neovascularization. Nat Med. 1999;5(4):434–8.
Kamihata H, Matsubara H, Nishiue T, Fujiyama S, Tsutsumi Y, Ozono R, et al. Implantation of bone marrow mononuclear cells into ischemic myocardium enhances collateral perfusion and regional function via side supply of angioblasts, angiogenic ligands, and cytokines. Circulation. 2001;104(9):1046–52.
Kalka C, Masuda H, Takahashi T, Kalka-Moll WM, Silver M, Kearney M, et al. Transplantation of ex vivo expanded endothelial progenitor cells for therapeutic neovascularization. Proc Natl Acad Sci U S A. 2000;97(7):3422–7.
Meng J, Yao X, Kang S, Kang S, Yang Y, Zhou C. Treatment of ischemic limbs by transplantation of G-CSF stimulated bone marrow cells in diabetic rabbits. Clin Invest Med. 2010;33(3):E174–80.
Tateishi-Yuyama E, Matsubara H, Murohara T, Ikeda U, Shintani S, Masaki H, et al. Therapeutic angiogenesis for patients with limb ischaemia by autologous transplantation of bone-marrow cells: a pilot study and a randomised controlled trial. Lancet. 2002;360(9331):427–35.
Rigato M, Monami M, Fadini GP. Autologous cell therapy for peripheral arterial disease: systematic review and meta-analysis of randomized, nonrandomized, and noncontrolled studies. Circ Res. 2017;120(8):1326–40.
ClinicalTrials.gov. Why should I register and submit results? http://www.clinicaltrials.gov/ct2/manage-recs/background. Accessed 10 Aug 2018.
Online The Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions [EB/OL]. [2009-09-01]. http://www.cochrane.org/.htm. Accessed 6 Oct 2018.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Huang P, Li S, Han M, Xiao Z, Yang R, Han ZC. Autologous transplantation of granulocyte colony-stimulating factor-mobilized peripheral blood mononuclear cells improves critical limb ischemia in diabetes. Diabetes Care. 2005;28(9):2155–60.
Barć P, Skóra J, Pupka A, Turkiewicz D, Dorobisz AT, Garcarek J, et al. Bone-marrow cells in therapy of critical limb ischaemia of lower extremities-own experience. Acta Angiol. 2006;12(4):155–66.
Arai M, Misao Y, Nagai H, Kawasaki M, Nagashima K, Suzuki K, et al. Granulocyte colony-stimulating factor: a noninvasive regeneration therapy for treating atherosclerotic peripheral artery disease. Circ J. 2006;70(9):1093–8.
Zhang Z, Liu W, Zhao X. Transplantation of autologous bone marrow stem cell for diabetic foot ulcer. Pract Clin Med. 2007;8(8):58–60.
Lu D, Jiang Y, Liang Z, Li X, Zhang Z, Chen B. Autologous transplantation of bone marrow mesenchymal stem cells on diabetic patients with lower limb ischemia. J Med Coll PLA. 2008;23(2):106–15.
Dash NR, Dash SN, Routray P, Mohapatra S, Mohapatra PC. Targeting nonhealing ulcers of lower extremity in human through autologous bone marrow-derived mesenchymal stem cells. Rejuvenation Res. 2009;12(5):359–66.
Chen B, Lu D, Liang Z, Jiang Y, Wang F, Wu Q, et al. Autologous bone marrow mesenchymal stem cell transplantation for treatment of diabetic foot following amplification in vitro. Chin J Tissue Eng Res. 2009;13(32):6227–30.
Gan Y, Li T, Yu L, Zheng C, Dong L, Jin R, et al. Curative effect of the combination of autologous bone marrow stem cell transplantation and Tongmai Huayu soup on diabetic foot. Chin J Dermatovenereol Integrated Tradit Western Med. 2009;8(1):5–7.
Shi J, Yan Z, Hu X, Cao L, Zhang X, Ma X. Clinical study of autologous bone marrow hematopoietic stem cell transplantation for treatment of diabetic lower limb vascular lesions. Chin J Postgraduates Med. 2009;32(34):50–2.
Procházka V, Gumulec J, Jalůvka F, Salounová D, Jonszta T, Czerný D, et al. Cell therapy, a new standard in management of chronic critical limb ischemia and foot ulcer. Cell Transplant. 2010;19(11):1413–24.
Wen J, Huang P. Autologous peripheral blood mononuclear cells transplantation in treatment of 30 cases of critical limb ischemia: 3-year safety follow-up. J Clin Rehabil Tissue Eng Res. 2010;14(45):8526–30.
Walter DH, Krankenberg H, Balzer JO, Kalka C, Baumgartner I, Schlüter M, et al. Intraarterial administration of bone marrow mononuclear cells in patients with critical limb ischemia: a randomized-start, placebo-controlled pilot trial (PROVASA). Circ Cardiovasc Interv. 2011;4(1):26–37.
Iafrati MD, Hallett JW, Geils G, Pearl G, Lumsden A, Peden E, et al. Early results and lessons learned from a multicenter, randomized, double-blind trial of bone marrow aspirate concentrate in critical limb ischemia. J Vasc Surg. 2011;54(6):1650–8.
Benoit E, O'Donnell TF Jr, Iafrati MD, Asher E, Bandyk DF, Hallett JW, et al. The role of amputation as an outcome measure in cellular therapy for critical limb ischemia: implications for clinical trial design. J Transl Med. 2011;9:165.
Powell RJ, Comerota AJ, Berceli SA, Guzman R, Henry TD, Tzeng E, et al. Interim analysis results from the RESTORE-CLI, a randomized, double-blind multicenter phase II trial comparing expanded autologous bone marrow-derived tissue repair cells and placebo in patients with critical limb ischemia. J Vasc Surg. 2011;52(4):1032–41.
Powell RJ, Marston WA, Berceli SA, Guzman R, Henry TD, Longcore AT, et al. Cellular therapy with Ixmyelocel-T to treat critical limb ischemia: the 25 randomized, double-blind, placebo-controlled RESTORE-CLI trial. Mol Ther. 2012;20(6):1280–6.
Lu D, Chen B, Liang Z, Deng W, Jiang Y, Li S, et al. Comparison of bone marrow mesenchymal stem cells with bone marrow-derived mononuclear cells for treatment of diabetic critical limb ischemia and foot ulcer: a double-blind, randomized, controlled trial. Diabetes Res Clin Pract. 2011;92(1):26–36.
Guan W, Gan Y, Li T, Yu L, Zheng C, Jia P, et al. Curative effect of autologous bone marrow stem cell transplantation on diabetic foot and its relation with serum level of basic fibroblast growth factor. Chin J Dermatovenereol Integrated Tradit Western Med. 2011;10(2):90–2.
Jain P, Perakath B, Jesudason MR, Nayak S. The effect of autologous bone marrow-derived cells on healing chronic lower extremity wounds: results of a randomized controlled study. Ostomy Wound Management. 2011;57(7):38–44.
Ozturk A, Kucukardali Y, Tangi F, Erikci A, Uzun G, Bashekim C, et al. Therapeutical potential of autologous peripheral blood mononuclear cell transplantation in patients with type 2 diabetic critical limb ischemia. J Diabetes Complicat. 2012;26(1):29–33.
Losordo DW, Kibbe MR, Mendelsohn F, Marston W, Driver VR, Sharafuddin M, et al. A randomized, controlled pilot study of autologous CD34+ cell therapy for critical limb ischemia. Circ Cardiovasc Interv. 2012;5(6):821–30.
Li M, Zhou H, Jin X, Wang M, Zhang S, Xu L. Autologous bone marrow mononuclear cells transplant in patients with critical leg ischemia: preliminary clinical results. Exp Clin Transplant. 2013;11(5):435–9.
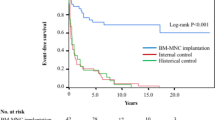
Szabo GV, Kovesd Z, Cserepes J, Daroczy J, Belkin M, Acsady G. Peripheral blood-derived autologous stem cell therapy for the treatment of patients with late-stage peripheral artery disease-results of the short- and long-term follow-up. Cytotherapy. 2013;15(10):1245–52.
Mohammadzadeh L, Samedanifard SH, Keshavarzi A, Alimoghaddam K, Larijani B, Ghavamzadeh A, et al. Therapeutic outcomes of transplanting autologous granulocyte colony-stimulating factor-mobilised peripheral mononuclear cells in diabetic patients with critical limb ischaemia. Exp Clin Endocrinol Diabetes. 2013;121(1):48–53.
Raval AN, Schmuck EG, Tefera G, Leitzke C, Ark CV, Hei D, et al. Bilateral administration of autologous CD133+ cells in ambulatory patients with refractory critical limb ischemia: lessons learned from a pilot randomized, double-blind, placebo-controlled trial. Cytotherapy. 2014;16(12):1720–32.
Teraa M, Sprengers RW, Schutgens RE, Slaper-Cortenbach IC, van der Graaf Y, Algra A, et al. Effect of repetitive intraarterial infusion of bone marrow mononuclear cells in patients with no-option limb ischemia: the randomized, double-blind, placebo-controlled Rejuvenating Endothelial Progenitor Cells via Transcutaneous Intra-arterial Supplementation (JUVENTAS) trial. Circulation. 2015;131(10):851–60.
Skóra J, Pupka A, Janczak D, Barć P, Dawiskiba T, Korta K, et al. Combined autologous bone marrow mononuclear cell and gene therapy as the last resort for patients with critical limb ischemia. Arch Med Sci. 2015;11(2):325–31.
Lu A, Zhao J, Zhang S, Li D, Zhang L, Nan J. The clinical observation of 20 cases of diabetic vascular lesion of lower limbs treated with autologous peripheral blood stem cell transplant after bone marrow mobilization. Inner Mongolia Med J. 2016;48(4):402–4.
Gupta PK, Chullikana A, Parakh R, Desai S, Das A, Gottipamula S, et al. A double blind randomized placebo controlled phase I/II study assessing the safety and efficacy of allogeneic bone marrow derived mesenchymal stem cell in critical limb ischemia. J Transl Med. 2013;10:143.
Horie T, Onodera R, Akamastu M, Ichikawa Y, Hoshino J, Kaneko E, et al. Long-term clinical outcomes for patients with lower limb ischemia implanted with G-CSF-mobilized autologous peripheral blood mononuclear cells. Atherosclerosis. 2010;208(2):461–6.
Acknowledgements
Not applicable.
Funding
This study is supported by National Natural Science Foundation of China (grant no. 81471043), Science and Technology Bureau of Sichuan Province (grant nos. 2015SZ0228-4, 2018SZ0239, 2019YFS0306), Science and Technology Bureau of Chengdu city (grant no 2017-CY02-00028-GX), the National Science and Technology Major Project (grant no. 2017 ZX09304023), and National Key R&D Program of China (grant no. 2017YFC1309605).
Availability of data and materials
All supporting data are included in the article and its additional files.
Author information
Authors and Affiliations
Contributions
WG and XR were responsible for the study concept and design and supervised the study. WG, DC, and GL were responsible for the acquisition of data, analysis, and interpretation of data. WG drafted the manuscript, and DC, GL, and XR undertook for critical revision of the manuscript. WG and GL did the statistical analysis. WG and XR acquired the funding. XR is the study guarantor. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Table S1. Details of search terms. (DOCX 13 kb)
Additional file 2:
Figure S1. Forest plot showing the effect of stem cell therapy on amputation rate in DM subgroup. (DOCX 24 kb)
Additional file 3:
Figure S2. Forest plot showing the effect of stem cell therapy on ulcer healing rate in DM subgroup. (DOCX 27 kb)
Additional file 4:
Table S2. Side effect association with stem cell therapy. (DOCX 16 kb)
Additional file 5:
Figure S3. Funnel plot of amputation rate. (DOCX 22 kb)
Additional file 6:
Figure S4. Funnel plot of ulcer healing rate. (DOCX 22 kb)
Additional file 7:
Figure S5. Funnel plot of ABI. (DOCX 21 kb)
Additional file 8:
Figure S6. Funnel plot of rest pain score. (DOCX 21 kb)
Additional file 9:
Table S3. Statistical test showed publication bias. (DOCX 15 kb)
Additional file 10:
Table S4. Sensitivity analysis: random model VS fixed model and OR VS RR VS RD on outcomes (*P > 0.05). (DOCX 15 kb)
Additional file 11:
Table S5. Sensitivity analysis: random model VS fixed model and MD VS SMD on outcome. (DOCX 15 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gao, W., Chen, D., Liu, G. et al. Autologous stem cell therapy for peripheral arterial disease: a systematic review and meta-analysis of randomized controlled trials. Stem Cell Res Ther 10, 140 (2019). https://doi.org/10.1186/s13287-019-1254-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-019-1254-5