Abstract
Background
Burkitt lymphoma is a high-grade B cell lymphoma which accounts for less than 1% of all adult cases of non-Hodgkin lymphoma. Rare instances of Burkitt lymphoma developing secondary to prior irradiation have been described in the literature.
Case presentation
We report a case of a 90-year-old white woman with a recent history of irradiation for Hodgkin lymphoma, who presented with primary Burkitt lymphoma of the supraglottic larynx. She underwent emergency awake tracheostomy with biopsy. A histopathological examination confirmed non-Hodgkin, B cell lymphoma of Burkitt type. Given her age and poor functional status, she underwent treatment with palliative radiotherapy.
Conclusions
A literature review was performed to clarify the clinical characteristics of radiation-induced Burkitt lymphoma in the head and neck, as well as its diagnosis and management. The present case represents the second case of radiation-induced Burkitt lymphoma in the head and neck in the reported literature, and the first in the supraglottic larynx. It highlights the need to maintain a broad differential in the assessment of malignancies of the larynx, particularly in patients with a prior history of radiation treatment.
Similar content being viewed by others
Background
Burkitt lymphoma is a high-grade B cell lymphoma that was first described by Denis Burkitt in the mid-twentieth century as an aggressive malignancy of the mandible in African children [1]. The World Health Organization (WHO) classifies Burkitt lymphoma as endemic, sporadic, or immunodeficiency-associated, based on underlying mechanisms of cancer formation. Endemic Burkitt lymphoma is that which occurs in African children, and is almost always associated with Epstein–Barr virus (EBV) infection. Sporadic Burkitt lymphoma refers to cases occurring worldwide with no specific geographic distribution, and accounts for 1 to 2% of adult lymphoma cases in the USA and Western Europe [2–4]. Tumor cells are EBV-positive in only 15 to 30% of cases of sporadic Burkitt lymphoma occurring in the USA [5]. Sporadic Burkitt lymphoma primarily involves lymph nodes in the abdomen, although occasionally occurs extranodally in the ovaries and kidneys and less frequently presents in the head and neck as cervical adenopathy. Extranodal head and neck presentations account for less than 10% of all cases of sporadic Burkitt lymphoma [6]. Rarely, Burkitt lymphoma develops secondary to prior irradiation, with only a few previous cases having been reported in the literature [7].
We present the case of a 90-year-old woman who was diagnosed with Burkitt lymphoma of the supraglottic larynx following radiation for a previous Hodgkin lymphoma. This is a rare extranodal head and neck presentation of Burkitt lymphoma, particularly in light of the patient’s advanced age and her previous radiation treatment for Hodgkin lymphoma.
Case presentation
A 90-year-old white woman presented with a large neck mass and a 6-week history of increasing dysphonia, stridor, and left-sided otalgia. On examination, there was a firm 2×3 cm left-sided level III neck mass with no overlying skin changes. Flexible fiberoptic nasolaryngoscopy revealed a large exophytic mass with complete airway obstruction. A computed tomography (CT) scan revealed the mass to measure approximately 3.3×3.7×3.1 cm. It was shown to involve her left supraglottic larynx and extend down to at least the level of her glottis (Fig. 1).
Eight years earlier, she was diagnosed as having primary Hodgkin lymphoma in a left cervical node. Pathology of the node revealed large atypical cells, Reed–Sternberg cells, and a fine reticular sclerosis pattern. Immunophenotyping performed on a paraffin block demonstrated positive staining of the large atypical cells with cluster of differentiation (CD) 15 and CD30. The stains were negative for leukocyte common antigen (LCA), CD20, EBV-encoded small ribonucleic acid (RNA) (EBER). She was classified as Stage 1A classical Hodgkin lymphoma, mixed cellularity type, which was a rare diagnosis at age 82. Due to her localized disease, she was treated with definitive radiotherapy at a dose of 3500 cGy in 20 fractions delivered over 4 weeks.
Her past medical history was otherwise significant for a left hip fracture and surgical repair 1 year earlier, as well as mild cognitive decline, with difficulties in sequencing, planning, memory, attention, and insight. Due to her cognitive status, she was reliant on family members for many of her daily activities.
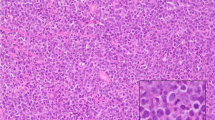
Following presentation, she underwent an emergency awake tracheostomy with laryngoscopy and biopsy of the supraglottic tumor. Microscopic examination revealed infiltrating sheets of poorly differentiated lymphoid cells with round nuclei containing several small nucleoli and dispersed chromatin and a small amount of amphophilic cytoplasm (Fig. 2). A high mitotic rate and a “starry sky” appearance, due to numerous tingible body macrophages, were noted. An extensive immunohistochemical panel was performed and the tumor cells were immunoreactive for CD20, BCL6, PAX 5, c-myc, and EBER (Fig. 2). Ki-67, a proliferation index marker, highlighted almost 100% of cells (Fig. 2). BCL2 was negative. Fluorescence in situ hybridization was performed and demonstrated the confirmatory myc rearrangement. The final histopathological diagnosis was a non-Hodgkin, B cell lymphoma of Burkitt type. This was distinct from her previous diagnosis of Hodgkin lymphoma 8 years prior.
Supraglottic larynx biopsy demonstrating infiltrating sheets of poorly differentiated lymphoid cells, numerous mitoses, and tingible body macrophages imparting a “starry-sky” pattern. a Hematoxylin and eosin (H&E) stain 40× magnification. b H&E stain, 100× magnification. c Tumor cell CD20 reactivity, 100× magnification. d Tumor cell c-myc reactivity, 100× magnification. e Tumor cell Ki-67 reactivity
This case was reviewed at a multidisciplinary tumor board to determine the appropriate course of management. She was not deemed a candidate for systemic therapy in light of her age and functional status. She underwent a 7-day course of high-dose prednisone (100 mg daily) before starting palliative radiation at a dose of 3600 cGy in 18 fractions. She subsequently developed mucositis, and was treated palliatively for symptom control. She had recurrent aspiration and developed bacteremia secondary to aspiration pneumonia for which she opted to forgo antibiotics. She died approximately 3 months following her initial presentation, before a repeat laryngeal examination could be conducted.
Discussion
Squamous cell carcinoma is the most frequently encountered cancer of the larynx; less commonly encountered laryngeal cancers include adenocarcinoma, adenoid cystic carcinoma, and neuroendocrine tumors. Malignant lymphomas account for less than 1% of all laryngeal tumors [8]. While the head and neck is the second most common extranodal site of involvement in non-Hodgkin lymphoma (NHL), the larynx is rarely involved, with structures typically affected being Waldeyer’s ring, ocular adnexal structures, the nasal cavity, nasopharynx, paranasal sinuses, thyroid gland, as well as salivary glands [9, 10]. Among cases of NHL affecting the larynx, the most common classifications described in the literature include mucosa-associated lymphoid tissue (MALT) lymphoma, plasmacytoma, and diffuse large B cell lymphoma. The supraglottic larynx is most commonly involved [9]. Among extranodal head and neck presentations of sporadic Burkitt lymphoma, the nasopharynx and tonsils were the most common sites of occurrence in one large case series of American sporadic Burkitt lymphoma [3]. Other extranodal sites of involvement within the head and neck, which occur in less than 5% of patients with sporadic Burkitt lymphoma, include the nasopharynx, tonsils, palate, sinuses, nasal septum, and other facial bones [3, 6, 11, 12]. This is the first reported case of primary Burkitt lymphoma of the larynx.
The aggressiveness of primary treatment for Hodgkin lymphoma, especially radiation therapy, is a primary risk factor in the development of subsequent lymphoma [13]. Our patient’s development of non-Hodgkin, Burkitt-type lymphoma following recent irradiation for cervical Hodgkin lymphoma is also an exceedingly uncommon occurrence. NHL is reported to occur following treatment for Hodgkin lymphoma at a rate of only 0.9% at 6.7 years, and 1.6% at 15 years [14].
To ascertain the frequency of radiation-induced Burkitt lymphoma, we performed a detailed electronic search of PubMed, MEDLINE, and Embase for studies reporting on radiation-induced Burkitt lymphoma. The following MeSH terms were used in varying combinations: Burkitt lymphoma, radiation-induced, radiotherapy, radiation-injury, and neoplasm. The search identified 22 potential studies, of which one was relevant for the qualitative synthesis [15]. We subsequently performed a hand-search of the literature which yielded one additional study for inclusion in our analysis [7]. These two studies together identified a total of 18 cases of Burkitt lymphoma which developed following prior radiation treatment for primary malignant neoplasm (Table 1). One case occurred in the mandible of a patient previously treated for oropharyngeal cancer [15]. This is, to the best of our knowledge, the only previously described case of Burkitt lymphoma developing in the head and neck secondary to prior radiation treatment.
The diagnosis of Burkitt lymphoma is made on the basis of histology and immunohistochemistry. On histologic examination, it is characterized by neoplastic lymphoid cells with round nuclei, dispersed chromatin, several small nucleoli, and a small amount of amphophilic cytoplasm. Mitoses are numerous and the tumor cells are admixed with tingible body macrophages, which are macrophages phagocytosing apoptotic debris, imparting a “starry sky” pattern. Most Burkitt lymphomas are immunoreactive for surface immunoglobulin M (IgM), as well as pan-B cell antigens including CD19, CD20, and CD22, and co-express CD10, CD43, and BCL6, but not CD5, CD23, BCL2, or TdT [16, 17] Nuclear staining with c-myc antibody is positive: in all cases of Burkitt lymphoma, a translocation exists between the c-Myc gene and either the IgH gene, as is found in 80% of cases, or either the kappa or lambda light chain gene, found in the other 20% [18]. Another important feature of Burkitt lymphoma is that nearly 100% of the tumor cells are positive for Ki-67, a proliferation index marker, in keeping with the tumor’s extremely rapid rate of growth: the doubling time of Burkitt lymphoma is among the fastest of any human malignancy [19]. Of note, EBV antibody titers are found to be positive in almost 100% of patients with endemic Burkitt lymphoma, but are only positive in 15 to 30% of patients with sporadic Burkitt lymphoma [16].
Given its fast-growing nature, prompt diagnosis of Burkitt lymphoma is essential to prevent local growth with compression of vital structures in the head and neck, or early widespread dissemination. The former occurred in the case we described, resulting in airway obstruction. Typical staging consists of abdominal and chest CT, a bone marrow biopsy, and cerebrospinal fluid (CSF) testing. Due to our patient’s advanced age, poor functional status, and palliative treatment approach, a staging workup was not performed. Although localized early stage Burkitt lymphoma is highly responsive to chemotherapy, advanced age and high tumor burden at presentation are poor prognostic factors [16, 20].
The treatment of Burkitt lymphoma typically consists of intermittent high-dose chemotherapy, most commonly using cyclophosphamide, vincristine, doxorubicin, and methotrexate. Rituximab, a monoclonal CD20 antibody, has also shown some promise when used in conjunction with a typical chemotherapeutic regimen [21]. Tumor debulking may be beneficial as an adjunct therapy when the anatomical location is permissive, although its role in the treatment of head and neck presentations of Burkitt has not been well studied [22, 23]. When prognosis is poor, as in the case described, locoregional radiation plays a palliative role in providing local symptom control [24].
Conclusions
Burkitt lymphoma is a B cell NHL with an extremely fast rate of growth, necessitating prompt diagnosis. Sporadic Burkitt lymphoma occasionally presents extranodally in the head and neck, although the most common head and neck presentation is cervical adenopathy. Rarely, radiation therapy has been linked to the subsequent development of Burkitt lymphoma. This case report describes a rare presentation of Burkitt lymphoma of the larynx in a 90-year-old patient previously irradiated for Hodgkin lymphoma. It represents the first reported case of Burkitt lymphoma in the larynx, and only the second described case of irradiation-induced Burkitt lymphoma occurring in the head and neck. It highlights the need to maintain a broad differential in the assessment of malignancies of the larynx, particularly in the context of a prior history of radiation treatment. Biopsy is a necessary step in the diagnosis of Burkitt lymphoma and in subsequent treatment planning, including selection of an appropriate chemotherapeutic regimen. When detected early, Burkitt lymphoma has a favorable prognosis and high remission rates. However, high tumor burden, advanced age, and poor functional status are associated with disease progression. In advanced stage or chemoresistant disease, there is good evidence that radiotherapy provides local symptom control.
Abbreviations
- CD:
-
Cluster of differentiation
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computed tomography
- EBER:
-
Epstein–Barr virus-encoded small RNA
- EBV:
-
Epstein–Barr virus
- LCA:
-
Leukocyte common antigen
- MALT:
-
Mucosa-associated lymphoid tissue
- NHL:
-
Non-Hodgkin lymphoma
- WHO:
-
World Health Organization
References
Burkitt D. A sarcoma involving the jaws in African children. Br J Surg. 1958;46:218–23.
van den Bosch CA. Is endemic Burkitt’s lymphoma an alliance between three infections and a tumour promoter? Lancet Oncol. 2004;5:738–46.
Levine PH, Lakshimi S, Kamaraju MD, Connelly RR, Costan W, et al. The American Burkitt’s Lymphoma Registry: Eight years’ experience. Cancer. 1982;49:1016–22.
Diebold J, Jaffe E, Raphael M, Warnke R. Burkitt lymphoma. In: Jaffe E, Harris N, Stein H, Vardiman J, editors. Pathology and Genetics of Tumors of Hematopoietic and Lymphoid Tissues. Lyon: IARC Press; 2001. p. 181–4.
Burmeister T, Schwartz S, Horst HA, et al. Molecular heterogeneity of sporadic adult Burkitt-type leukemia/lymphoma as revealed by PCR and cytogenetics: correlation with morphology, immunology and clinical features. Leukemia. 2005;19:1391–8.
Wang MB, Strasnick B, Zimmerman MC. Extranodal American Burkitt’s lymphoma of the head and neck. Arch Otolaryngol Head Neck Surg. 1992;118:193–9.
Salloum E, Tallini G, Levy A, Cooper DL. Burkitt’s lymphoma-leukemia in patients treated for Hodgkin’s disease. Cancer Invest. 1996;14:527–33.
Horny HP, Kaiserling E. Involvement of the larynx by hematopoietic neoplasms. An investigation of autopsy cases and review of the literature. Pathol Res Pract. 1995;191:130–8.
Vega F, Lin P, Medeiros J. Extranodal lymphomas of the head and neck. Ann Diagn Pathol. 2005;9:340–50.
Hanna E, Wanamaker J, Adelstein D, Tubbs R, Lavertu P. Extranodal lymphomas of the head and neck. A 20-year experience. Arch Otolaryngol Head Neck Surg. 1997;123:1318–23.
Patton LL, McMillan CW, Webster WP. American Burkitt’s lymphoma: a 10-year review and case study. Oral Surg Oral Med Oral Pathol. 1990;69:307–16.
Aslan G. Unusual presentation of sporadic Burkitt’s lymphoma originating from the nasal septum: a case report. J Med Case Rep. 2013;7:60.
Henry-Amar M. Second cancer after the treatment for Hodgkin’s disease: a report from the International Database on Hodgkin’s Disease. Ann Oncol. 1992;3 suppl 4:117–28.
Tucker MA, Coleman CN, Cox RS, Varghese A, Rosenberg SA. Risk of second cancers after treatment for Hodgkin’s disease. N Engl J Med. 1988;318:76–81.
Nagasaki A, Yamanoha A, Okudaira T, Miyagi T, Takasu N. Treatment-related Burkitt’s lymphoma: literature review and case report of successful treatment with rituximab monotherapy. Acta Haematol. 2009;122(4):211–5.
Ferry JA. Burkitt’s lymphoma: Clinicopathologic features and differential diagnosis. Oncologist. 2006;11:375–83.
Chuang S-S, Ye H, Du M-Q, Lu C-L, Dogan A, et al. Histopathology and immunohistochemistry in distinguishing Burkitt’s lymphoma from diffuse large B-cell lymphoma with very high proliferation index and with or without a starry-sky pattern. A comparative study with EBER and FISH. Am J Clin Pathol. 2007;128:558–64.
Ruzinova MB, Caron T, Rodig SJ. Altered subcellular localization of c-myc protein identifies aggressive B-cell lymphomas harboring a c-MYC translocation. Am J Surg Pathol. 2010;34(6):882–91.
Schnitzer B, Weaver DK. Lymphoreticular disorders. In: Bataskis JG et al., editors. Tumors of the Head and Neck: Clinical and Pathological Considerations. 2nd ed. Baltimore: Williams & Wilkins; 1979. p. 448–91.
Kearns DB, Smith RJH, Pitcock JK. Burkitt’s lymphoma. Int J Pediatr Otorhinolaryngol. 1986;12:73–84.
Barnes JA, LaCasce AS, Feng Y, Toomey CE, Neuberg D, et al. Evaluation of the addition of rituximab to CODOX-M/IVAC for Burkitt’s lymphoma: a retrospective analysis. Ann Oncol. 2011;22:1859–64.
Kemeny MM, Magrath IT, Brennan MF. The role of surgery in the management of Burkitt’s lymphoma and its treatment. Ann Surg. 1982;196(1):82–6.
Brigger MT, Cunningham MJ. Malignant cervical masses in children. Otolaryngol Clin North Am. 2015;48:59–77.
Lowry L, Smith P, Qian W, Falk S, Benstead K, et al. Reduced dose radiotherapy for local control in non-Hodgkin lymphoma: A randomized phase III trial. Radiother Oncol. 2011;100:86–92.
Acknowledgements
Not applicable.
Funding
The authors have no funding to declare.
Availability of data and materials
The data that support the findings of this study are available from The Ottawa Hospital but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of The Ottawa Hospital.
Authors’ contributions
AQ participated in the design of the study, acquired data, performed a literature review, and drafted the manuscript. LC conceived the study, participated in its design and coordination, acquired data, and helped to draft and edit the manuscript. DR participated in the design of the study and edited the manuscript. SJ participated in the design of the study and edited the manuscript. BP acquired data, participated in the design of the study, and edited the manuscript. LS acquired data, participated in the design of the study, and edited the manuscript. LE acquired data, participated in the design of the study, and edited the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethics approval and consent to participate
The need for ethics approval was waived.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Quimby, A.E., Caulley, L., Rodin, D. et al. Primary Burkitt lymphoma of the supraglottic larynx: a case report and review of the literature. J Med Case Reports 11, 65 (2017). https://doi.org/10.1186/s13256-017-1209-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-017-1209-3