Abstract
Background
Chronic traumatic encephalopathy (CTE) is a neurodegenerative disease that has been neuropathologically diagnosed in brain donors exposed to repetitive head impacts, including boxers and American football, soccer, ice hockey, and rugby players. CTE cannot yet be diagnosed during life. In December 2015, the National Institute of Neurological Disorders and Stroke awarded a seven-year grant (U01NS093334) to fund the “Diagnostics, Imaging, and Genetics Network for the Objective Study and Evaluation of Chronic Traumatic Encephalopathy (DIAGNOSE CTE) Research Project.” The objectives of this multicenter project are to: develop in vivo fluid and neuroimaging biomarkers for CTE; characterize its clinical presentation; refine and validate clinical research diagnostic criteria (i.e., traumatic encephalopathy syndrome [TES]); examine repetitive head impact exposure, genetic, and other risk factors; and provide shared resources of anonymized data and biological samples to the research community. In this paper, we provide a detailed overview of the rationale, design, and methods for the DIAGNOSE CTE Research Project.
Methods
The targeted sample and sample size was 240 male participants, ages 45–74, including 120 former professional football players, 60 former collegiate football players, and 60 asymptomatic participants without a history of head trauma or participation in organized contact sports. Participants were evaluated at one of four U.S. sites and underwent the following baseline procedures: neurological and neuropsychological examinations; tau and amyloid positron emission tomography; magnetic resonance imaging and spectroscopy; lumbar puncture; blood and saliva collection; and standardized self-report measures of neuropsychiatric, cognitive, and daily functioning. Study partners completed similar informant-report measures. Follow-up evaluations were intended to be in-person and at 3 years post-baseline. Multidisciplinary diagnostic consensus conferences are held, and the reliability and validity of TES diagnostic criteria are examined.
Results
Participant enrollment and all baseline evaluations were completed in February 2020. Three-year follow-up evaluations began in October 2019. However, in-person evaluation ceased with the COVID-19 pandemic, and resumed as remote, 4-year follow-up evaluations (including telephone-, online-, and videoconference-based cognitive, neuropsychiatric, and neurologic examinations, as well as in-home blood draw) in February 2021.
Conclusions
Findings from the DIAGNOSE CTE Research Project should facilitate detection and diagnosis of CTE during life, and thereby accelerate research on risk factors, mechanisms, epidemiology, treatment, and prevention of CTE.
Trial registration
Similar content being viewed by others
Background
Chronic traumatic encephalopathy (CTE) is a neurodegenerative disease that has been neuropathologically diagnosed in former contact sport athletes, military combat veterans, and other individuals exposed to repetitive head impacts [1,2,3,4,5,6,7,8,9]. Although CTE is often portrayed as a new disease, its history dates back to the 1920s and 1930s, with descriptions of “punch drunk” boxers [10] and “dementia pugilistica” [11], with the term “chronic traumatic encephalopathy” first used in publications in the 1940s [12, 13]. CTE began to receive significant lay and scientific attention in 2005, following a report of neuropathological evidence of hyperphosphorylated tau (p-tau) in an irregular pattern in a deceased former National Football League (NFL) player who had ante-mortem cognitive and neuropsychiatric symptoms [5]. CTE has since been neuropathologically diagnosed in hundreds of deceased American football players [1,2,3], in addition to other contact and collision sport athletes (e.g., ice hockey, soccer, rugby) [2, 8, 14] and military veterans [4]. Given the millions of active and former contact sport athletes, military service members, and veterans, CTE is potentially a major public health concern. However, disease incidence and prevalence remain unknown due to the inability to detect and diagnose CTE during life.
Neuropathology of CTE
In 2013, McKee et al. examined the immunocytochemical characteristics of 68 cases (including 50 American football players) with autopsy-confirmed CTE and proposed neuropathological diagnostic criteria for CTE in addition to a 4-stage classification scheme to grade the pathological severity of p-tau [2, 15]. As part of the National Institute of Neurological Disorders and Stroke (NINDS)-funded “Understanding Neurologic Injury in Traumatic Encephalopathy (UNITE)” study [16], two consensus meetings have been convened to define the neuropathological diagnostic criteria for CTE [17, 18]. The pathognomonic lesion is now defined as p-tau aggregates as neurofibrillary tangles (NFT) in neurons, with or without p-tau in astrocytes, deposited around small blood vessels, in an irregular pattern at the depths of the cortical sulci, with the focus in superficial cortical layers. The panels concluded that the pattern of p-tau in CTE is distinct from that of any other neurodegenerative disease [17, 18]. The molecular structure of tau filaments in CTE has also since been shown to be unique [19] [20] [21]. Although CTE is a mixed three and four microtubule-binding domain repeat (3R and 4R) tauopathy, similar to AD, recent research has shown that the CTE tau isoforms shift across disease severity, from 4R to 3R, with 4R isoforms found primarily in astrocytes [22]. Unlike in AD, amyloid-beta protein (Aβ) deposits in CTE are not an early feature, they are not diagnostic, and they tend to accumulate with advancing age as a co-morbidity. When present in CTE, the Aβ plaques tend to be diffuse and not neuritic [23]. CTE is nonetheless frequently co-morbid with other neurodegenerative (e.g., Lewy body disease) and non-neurodegenerative conditions (e.g., white matter rarefaction, arteriolosclerosis) [3, 24,25,26].
Risk factors for CTE
The primary risk factor for CTE is exposure to repetitive head impacts and the resulting repeated concussions and subconcussive trauma (i.e., head impacts that result in neuronal injury but do not cause immediate symptoms) [3, 9, 24, 27,28,29,30]. Repetitive subconcussive head impacts play a prominent role in the development of this disease [31, 32].The duration of American football play has been identified as a strong predictor of the risk and severity of CTE neuropathology [30]. Small autopsy case series provide suggestive links between soccer and rugby play and CTE [8, 14]. These associations between repetitive head impacts and neuropathology have been complemented by in vivo research studies that link exposure to repetitive head impacts with later-life cognitive and neuropsychiatric symptoms [24, 27, 33, 34]. However, not all individuals who are exposed to repetitive head impacts will develop CTE or other long-term neurological disorders. Risk modifiers may include severity and nature of repetitive head impact exposure (e.g., frequency [27, 35], type of contact sport played [36,37,38], younger age of first exposure [39,40,41,42,43,44]), lower cognitive reserve [45], cerebrovascular health [24, 46], and/or genetic make-up [47,48,49].
Clinical presentation of CTE and traumatic encephalopathy syndrome
CTE is a neuropathological diagnosis and cannot currently be diagnosed during life because its clinical presentation has been—until recently—ill-defined, and because validated in vivo biomarkers for the detection of CTE neuropathology do not yet exist [50]. To date, the clinical presentation of CTE has been described primarily through the use of retrospective telephone interviews with next-of-kin and other informants of brains donors with autopsy-confirmed CTE. These studies have reported a constellation of progressively worsening and non-specific cognitive impairments (particularly in executive functions and episodic memory), poor regulation or control of emotions and/or behavior (including impulsivity, explosiveness, rage, and/or emotional lability), and, in some instances, parkinsonism and motor neuron disease [3, 47, 51]. Provisional clinical research diagnostic criteria for CTE have been proposed [52, 53], including the traumatic encephalopathy syndrome (TES) research criteria published in 2014 [54]. Since the time of the original 2014 publication, the research diagnostic criteria for TES have been used in several studies. Their validity in predicting neuropathological CTE diagnoses has recently been reported along with an item-level analysis suggesting that cognitive symptoms—more than neuropsychiatric features—are particularly valuable in predicting CTE pathology [55]. These findings informed new NINDS Consensus Diagnostic Criteria for TES that have recently been published [56].
Consistent with the clinical diagnosis of other neurodegenerative diseases [57,58,59,60], an accurate diagnosis of CTE during life will require validated biomarkers of the underlying pathophysiology of the disease. There have been several preliminary studies that have examined both specific (e.g., those that measure regional p-tau pathology) and non-specific (e.g., general neurodegeneration) biomarkers of CTE. Examples of potential supportive or non-specific fluid biomarkers of CTE include cerebrospinal fluid (CSF) and plasma markers of neurodegeneration (e.g., total tau [t-tau] [35, 61, 62], neurofilament light [NfL] chain protein [63]) and microglial activation (e.g., soluble triggering receptor expressed on myeloid cells 2 [sTREM2]) [61], as well as measures of tau in exosomes isolated from plasma and proteomic profiling of plasma and CSF extracellular vesicles [64,65,66]. Candidate neuroimaging biomarkers for the detection of non-specific neurodegenerative changes of CTE have recently been reviewed [67, 68] and include the following: cavum septum pellucidum (a common gross neuropathological finding in CTE [1, 2]) on structural T1-weighted magnetic resonance imaging (MRI) [69,70,71,72]; frontotemporal and medial temporal lobe atrophy on structural T1-weighted MRI [73,74,75,76,77,78,79]; decreased cortical thickness on T1-weighted MRI [44]; white matter alterations on diffusion tensor imaging (DTI) [42, 74, 80,81,82,83,84]; cerebral hypoperfusion and functional hypoactivity on single photon emission computerized tomography [85]; arterial spin labeling [86] and functional MRI (fMRI) [87]; and neurochemical alterations on magnetic resonance spectroscopy (MRS) [88,89,90].
Efforts are underway to identify specific biomarkers of CTE. Amyloid positron emission tomography (PET) imaging is a neuropathologically validated biomarker for the early detection, tracking, and diagnosis of neuritic Aβ deposition, one of the cardinal neuropathological features of AD [58, 91]. Although postmortem studies of CTE have found diffuse Aβ plaques, evidence of neuritic plaques has primarily been found in late-stage disease [3, 15, 23]. It would be unlikely for amyloid PET tracers to demonstrate significant binding in CTE, as they bind preferentially to neuritic plaques [91]. More recently, PET imaging of paired helical filament tau has become a neuropathologically validated biomarker for the detection, tracking, and diagnosis of AD-related tau tangle deposition. For instance, the PET radiotracer flortaucipir (AV1451; T807) demonstrates high affinity binding to the mixed 3R/4R tau isoforms in AD [92]. Flortaucipir’s binding to other tauopathies with primarily 4R isoforms has not been as promising [93, 94]. Although CTE and AD have similar (3R/4R) tau isoforms, there are differences at the molecular level [19], and, as mentioned earlier, in CTE the ratio of 3R:4R differs across disease stage and between neuronal and glial tau [22].
Stern et al. studied flortaucipir PET in 26 symptomatic former NFL players (ages 40–69) and 31 same-age asymptomatic men without a history of traumatic brain injury (TBI) [95]. At a group level, the former players had significantly higher flortaucipir uptake in superior frontal, medial temporal, and parietal regions, compared to the asymptomatic men without TBI; however, the uptake levels were not as high as seen in individuals with AD. Although the level of flortaucipir uptake in the three brain regions was significantly associated with the number of years playing football, it was not significantly associated with cognitive and neuropsychiatric test scores. Importantly, the former players did not have elevated florbetapir levels compared to the unexposed group, and only one former NFL player had slightly elevated florbetapir standardized uptake value ratio (SUVR), indicating that the former NFL players’ cognitive impairment was not due to AD. Based on these findings and other in vivo and neuropathological studies [78, 96, 97], the utility and specificity of flortaucipir for the detection of CTE paired helical filament tau is unclear.
The DIAGNOSE CTE Research Project
In December 2015, NINDS funded a 7-year, multicenter grant proposal, “Chronic Traumatic Encephalopathy: Detection, Diagnosis, Course, and Risk Factors,” submitted by our multidisciplinary team of investigators, under the leadership of four co-principal investigators (co-PIs; RAS [contact PI], JLC, EMR, MES). This is now referred to as the “Diagnostics, Imaging, and Genetics Network for the Objective Study and Evaluation of Chronic Traumatic Encephalopathy (DIAGNOSE CTE) Research Project.” The specific aims of the DIAGNOSE CTE Research Project are listed in Table 1. The primary endpoints of the study are to characterize the clinical presentation of CTE and to identify in vivo biomarkers that can support a “probable CTE” diagnosis. There were several guiding principles that were followed throughout the development of the grant proposal and study design, including (1) CTE is viewed as a neurodegenerative disease; (2) although the necessary risk factor for the development of this tauopathy appears to be a history of repetitive head impact exposure, CTE itself should not be confused with TBI or considered the aggregate effect of multiple symptomatic concussions; (3) to conduct a study of the clinical presentation, diagnostic criteria, biomarkers, and risk factors of CTE requires expertise across many disciplines, including Neurology, Neuropsychology, Psychiatry, Neuroimaging, Molecular Medicine, Neuropathology, Exposure Science, Genetics, Biostatistics, Epidemiology, Computer Science, and Sociology; and (4) a team science approach is required, breaking down typical academic and institutional “silos” to conduct the best research in the most efficient manner.
The objective of this paper is to describe the rationale, methodology, and design of the DIAGNOSE CTE Research Project. We provide updates on the current status of the project and conclude with methodological considerations, and discussion of the expected impact of the project results, as well as the infrastructure and resources created to support further studies.
Methods
Infrastructure overview
The DIAGNOSE CTE Research Project is a 7-year (now expected to be 8-year following COVID-19 pandemic-related modifications described below) study that involves more than 40 investigators from 12 research institutions across the USA (Supplementary Table 1, Additional File 1). There is a 7-member External Advisory Board (Supplementary Table 2, Additional File 1) that meets annually with the co-PIs and the NINDS Scientific Program Official. The project is overseen by an Executive Committee consisting of the co-PIs, Participant Evaluation Site PIs, NINDS Scientific Program Official, Advisory Board Chair (ex officio member), and Team Leaders for the seven multidisciplinary/multi-institutional study teams: Data; Neuroimaging; Fluid Biomarkers; Clinical Outcomes; Diagnostic Criteria; Risk Assessment; and Diversity, Equity, and Inclusion (DEI). Investigator meetings are held annually.
Sample selection
The targeted sample and sample size was 240 men, ages 45–74, divided into three groups based on the extent of exposure to repetitive head impacts: 120 former professional football players (PRO); 60 former college football players (COL); and a group of 60 participants with no history of participation in organized contact/collision sports, combat military service, or known concussion or other TBI, herein referred to as the unexposed comparison group (UE). Inclusion and exclusion criteria are summarized in Table 2. There were no enrollment criteria for presence or severity of cognitive or neuropsychiatric symptoms or of degree of functional independence for PRO and COL participants (other than the requirement to have adequate decisional capacity to provide consent for research at baseline). All participants were required to have a study partner who knew them well and with whom they had frequent communication. Based on telephone screening, UE participants were required to be asymptomatic.
Sample size determination and power
The sample sizes were determined to assure statistical power of 80% or greater, to detect moderate effect sizes, and assuming a significance level of 0.05 with two-tailed significance tests, for key hypotheses for Specific Aims 1–5. Power calculations were performed and based on effect sizes from our previous research. The difference in CSF p-tau/tau ratio between PRO and UE groups was used as an example of the biomarkers evaluated in Aim 1. Preliminary unpublished results from the NINDS-funded DETECT study (PI: RAS) show a difference of 0.15 (SD of 0.04) in CSF p-tau/tau ratio between former NFL players and UE participants. Our sample size has a power of > 99% to detect differences between the symptomatic PRO and COL participants (n = 120) compared to asymptomatic PRO and COL participants and UE participants (n = 120) in p-tau/tau ratio. To illustrate the power for Aim 3, the longitudinal differences between symptomatic PRO participants compared to asymptomatic PRO and UE participants for the Trail Making B test were used. Gavett et al. showed differences ranging from 35 to 60 s over a 3-year follow-up between people with normal cognition and participants with mild cognitive impairment or dementia [100]. Our sample will have 94% power to detect similar differences in a 3-year period among symptomatic PRO participants compared to asymptomatic PRO and UE participants, assuming 30% attrition.
Recruitment and retention
A Recruitment and Retention Coordinator and research assistant oversaw an extensive national recruitment campaign (Supplementary Material, Additional File 1). Recruitment efforts were aimed at enrolling across a continuum of symptom severity, from asymptomatic to mildly symptomatic to dementia, rather than to any specific level of impairment. Interested potential participants underwent a telephone screening interview by Coordinating Center staff, using a script approved by the Institutional Review Board (IRB) at BU Medical Campus (BUMC). Structured and semi-structured questions were asked about current mood, behavior, and cognitive symptoms, as well as functional status. An additional telephone screening was conducted with an informant/study partner, using similar questions and assessments. The Recruitment and Retention Coordinator determined the Participant Evaluation Site most appropriate for the participant (based on balancing the number of participants across sites, travel distance, and available schedules). To maximize sample retention over the follow-up period, participants are telephoned annually by project staff and sent birthday and holiday cards. A study-wide newsletter is published quarterly and distributed to all participants electronically. For participants with dementia, an additional annual call is made to the participant or (with permission) to a study partner/informant to assess the participant’s status and improve retention.
Study procedures
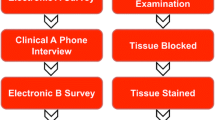
A centralized project Coordinating Center is located at Boston University (BU) School of Medicine (BUSM). There are four Participant Evaluation Sites: (1) Boston (BUSM, with MRI scans conducted at Brigham and Women’s Hospital [BWH]); (2) Las Vegas (Cleveland Clinic [CC] Lou Ruvo Center for Brain Health); (3) New York (New York University [NYU] Langone Health); and (4) Scottsdale/Phoenix (Mayo Clinic Arizona, with PET scans conducted at Banner Alzheimer’s Institute [BAI] in Phoenix). All participants received a baseline evaluation at one of the four Participant Evaluation Sites. Baseline evaluations included neurocognitive testing, assessment of functional status, neuropsychiatric questionnaires, neurological assessment (including standardized motor examination, headache severity and sleep-related symptoms measurement, and an olfaction test), MRI (including structural, diffusion, functional, and neurochemical), two PET scans (with florbetapir amyloid and flortaucipir tau tracers), lumbar puncture (LP; for CSF banking and biomarkers), blood draws (for banking, biomarkers, and DNA extraction), and saliva samples (for banking and biomarkers). In the original design, the PRO and UE groups would return for a 3-year, in-person follow-up evaluation. COL participants would not be evaluated at follow-up because their inclusion was for head impact exposure risk modeling at baseline (Aim 5) and to assure a large baseline sample size with adequate variability of clinical presentation (Aims 1 & 2).
It was required that all participants have adequate decisional capacity at the time of their baseline visit to participate. Because some participants have mild dementia, specific procedures were conducted to assure appropriate decisional capacity to consent to research participation. Some participants who reported functional difficulties (n = 16) were accompanied by their study partner or other care partner. All participants’ travel expenses (and that of a care partner if required) were paid by the study and each participant received $500 compensation for completion of the 3-day evaluation. Participants were informed during screening, at the time of consenting, and subsequent to their study visit, that they could receive a summary of non-experimental study results (including standardized neuropsychological testing and neuropsychiatric questionnaires, neurological examination, clinical reads of the structural MRI, clinical laboratory blood tests, electrocardiogram) and/or have the results sent to their primary healthcare provider. If requested, they could discuss results of the non-experimental assessments with one of the co-PIs (RAS). At all times, participants were informed orally and in written reports that the results should not be used for clinical or medico-legal decision-making. At the time of study initiation, and throughout the baseline evaluation period, flortaucipir (tau) PET imaging was in human trials and viewed as one of the experimental assessments. It received FDA approval 3 months following completion of baseline examinations for the evaluation of AD, with specific package insert wording that it is not indicated for the evaluation of CTE. Florbetapir (amyloid) PET imaging received FDA approval prior to study initiation for patients being evaluated for AD and is considered non-experimental for specific clinical purposes. For this study, the co-PIs, with input from external experts, chose not to disclose florbetapir results, though this does not necessarily represent the standard for the field moving forward.
Data collection
Clinical evaluations
Each baseline study visit was conducted over a 3-day period and each follow-up visit was planned to take place over a two- or three-day period. Tables 3 and 4 list the clinical exams and measures that were administered. Comprehensive semi-structured interviews for all participants were performed and supplemented by online questionnaires in order to collect data on demographics (e.g., age, education, racial and ethnic identity); psychosocial and lifestyle history (e.g., exercise, occupational and educational attainment, early childhood zip code or equivalent, parents’ educational attainment); medical, neurological, and psychiatric history (including substance use and performance enhancing drug use); family history of psychiatric and neurological conditions; athletic history (e.g., age of first exposure, level(s) and duration of play, position(s) played, era of play); military history; and concussion and TBI history. For the COL and PRO participants, involvement in current or pending litigation involving neurologic consequences of playing American football was also queried. Participants had vital signs (e.g., blood pressure, pulse, height and weight measurement) assessed by a registered nurse. Safety procedures (e.g., blood draw for platelet count and other clotting tests, and ECG for abnormal heart rhythms and/or clinically significant cardiovascular disease) were reviewed by a qualified clinician to ensure participants were eligible for the LP and flortaucipir PET scan, respectively. During the study visit, study partners were emailed a survey link to a web-based Research Electronic Data Capture (REDCap) system to complete standardized measures and a self-report questionnaire on the presence and onset of cognitive, behavior, and/or mood problems, as well as an assessment of functional status. If the informant accompanied the participant to the visits, she/he was asked to complete the online questionnaires prior to returning home. All informants were also interviewed by telephone to provide additional history and to clarify history provided by the participant.
Clinical measures (see Tables 3 and 4) were selected, in part, to assure harmonization with data sharing platforms, such as the Federal Interagency Traumatic Brain Injury Research (FITBIR) system and the National Alzheimer Coordinating Center (NACC). Many instruments and methodologies that overlap with the NINDS Common Data Elements (CDE) and/or the NACC Uniform Data Set (UDS) v.3.0 (the latter used by all of the National Institute on Aging-funded AD Research Centers) [110] were selected. Measures include those that assess clinical domains relevant to the features described in neuropathologically confirmed cases of CTE [2, 3, 47, 54] and were part of the 2014 TES research diagnostic criteria [54].
To assure standardization of the administration and scoring of clinical evaluations across sites and examiners, extensive training procedures were employed. Neurologists administering the Movement Disorder Society (MDS)-Unified Parkinson’s Disease Rating Scale (UPDRS) [101] completed formal online training offered through MDS. A comprehensive neuropsychological test administration and scoring manual was developed and deployed to all sites, along with an accompanying training video of a full test administration, including several demonstrations of how to respond to and score incorrect or unusual responses. All staff administering the neurocognitive tests were certified (and re-certified annually) in test administration and scoring via mock training videos that were reviewed and certified by two licensed clinical neuropsychologists at the Coordinating Center (MLA, RAS).
Neuroimaging
Neuroimaging protocols include structural T1- and T2-weighted MRI, diffusion MRI (dMRI), resting-state fMRI, MRS, and molecular imaging with two PET tracers, florbetapir and flortaucipir. During the pre-enrollment period, BWH neuroimaging investigators and Invicro (a research-dedicated organization that collaborates on large-scale diagnosis, progression, and disease monitoring trials, providing molecular imaging services, including florbetapir and flortaucipir) created study-specific image acquisition sequences and technical operations manuals and developed and implemented training and setup procedures for the MR and PET centers, respectively, at each of the Participant Evaluation Sites. Details on the neuroimaging processing and analysis are provided in the Supplementary Material (Additional File 1).
MRI
MRIs across all four sites were conducted on Wide Bore 3 T scanners (Siemens Skyra, Erlangan, Germany; software version VE11) using a 20 channel head coil in order to accommodate the wide range of participant sizes. The goal of the MRI sequence selection was to obtain the most advanced images consistent with other large multi-site studies (e.g., Alzheimer’s Disease Neuroimaging Initiative), and which could be acquired at each site within a reasonable time period to limit participant burden. The acquisition included sequences for anatomical images, as well as diffusion MRI (dMRI) and resting-state fMRI. High-resolution (1 × 1 × 1 mm3) 3D T1-weighted images using MPRAGE with an inversion time of 1100 ms were acquired, as were high-resolution (1 × 1 × 1 mm3) 3D T2-weighted images and fluid attenuated inversion recovery (FLAIR) sequences. The dMRI has a multi-shell design with 73 acquisitions spread over 5 shells (4 b = 0, 3 b = 200, 6 b = 500, 30 b = 1000, and 30 b = 2500 s/mm2). Images have a 2 × 2 × 2 mm3 resolution and 73 slices. The resting-state fMRI acquisition was an echo-planar imaging (EPI) acquisition with 3.5 × 3.5 × 3.5 mm3 resolution, with 37 slices, TR of 2.5 s, repeated 149 times.
MRS
2D-chemical shift imaging (CSI) was acquired using the localized semi-adiabatic spin-echo refocusing (semi-LASER) with Gradient-Offset independent Adiabaticity Wurst modulation (GOIA-W) pulses and spiral encoding (853-ms duration, 12-kHz bandwidth, 90° flip angle, 160 mm field of view, 1.5-s repetition time, and 40-ms echo time) [145]. Interleaved constant-density spirals simultaneously encode one frequency and two spatial dimensions (16 × 16; 3 averages) for a resolution of 1 × 1 × 1.5 cm3 and a scan time of 6 min. The 160 × 160 × 15 mm slab was placed across the corpus callosum parallel to the A/P plane. Single voxel spectroscopy (SVS) was acquired using point-resolved spectroscopy (PRESS; TE = 30 ms, TR = 2 s, 2 × 2 × 2 cm3, 128 averages; 16 average water reference) in the posterior cingulate gyrus for a scan time of 5 min [146].
PET
Participants underwent two PET imaging studies (florbetapir and flortaucipir) at baseline. Tracer doses were requested through Avid Radiopharmaceuticals (Philadelphia, PA, USA) who then ordered the doses from one of several contract manufacturing organizations (usually the most proximate to a site) and coordinated dose shipping and delivery to the four PET centers. The florbetapir protocol was as follows: immediately after a 370 MBq (10 mCi) bolus injection, the participant underwent brain scans consisting of 10 frames, each 1 min in length. Fifty minutes after injection, the participant completed a second 15-min brain scan consisting of three frames, each of which required 5 min.
The use of flortaucipir in this study was carried out through an Investigator Investigational New Drug (IND #131391) from the U.S. Food and Drug Administration. The flortaucipir protocol was as follows: 80 min after a 370 MBq (10 mCi) bolus injection, the participant completed a continuous dynamic 20-min brain scan (four frames, 5 min each). Procedures described by Stern et al. [95] will serve as a guide for initial analyses of florbetapir and flortaucipir images. However, additional analyses of PET amyloid and tau scans will be conducted, consistent with the most current methods and approaches [147,148,149].
Fluid biomarkers
The collection, tracking, banking, and distribution of all fluid biospecimens is done under the direction of the project’s Fluid Biomarker Team leader (ERP) at VA Puget Sound. CSF, blood, and saliva collection and storage complies with the National Institute on Aging Biospecimen Task Force Guidelines and with NINDS Repository Biomarkers Discovery Samples Resource. Education and training were provided at each of the Participant Evaluation Sites (through in-person training, provision of a video DVD [150], and manuals) for the safe, acceptable, and uniform methods for CSF, blood, and saliva collection. The Fluid Biomarker Team provided all sites with prefabricated CSF, blood, and saliva sample collection kits. Sample collection and sample processing procedures are detailed in the Supplementary Material (Additional File 1). An aliquot of whole blood was kept at room temperature and shipped to BUSM the day of collection for DNA extraction for genetic and genomic analyses. All other saliva, blood, and CSF samples were processed, aliquoted, and stored at − 80 °C at the four Participant Evaluation Sites, and then batch shipped on dry ice overnight to VA Puget Sound, where they are stored in two − 70 °C freezers. Banked CSF, blood products, and saliva will be made available to qualified outside investigators.
Head impact exposure assessment and modeling
A challenge of evaluating the long-term consequences of repetitive head impacts is that the outcomes are chronic, but the exposures are acute and, in this setting, remote. Each impact is of short duration, can be ambiguous, and rarely quantified. Task-based exposure assessment methods, such as job-exposure matrices, are often utilized to develop retrospective exposure metrics for investigating exposure-disease relationships [151]. The same will be applied to retrospectively estimate repetitive head impact exposure in the COL and PRO groups. A position-exposure matrix (PEM) will be developed. Different football positions (e.g., running back, offensive lineman) experience different impacts in terms of frequency, intensity, location, and type (linear or rotational) [152,153,154]. These measurements have been collected for over 1.8 million head impacts during games and practices using the Head Impact Telemetry (HIT) System™ [155,156,157,158,159]. Information from this extensive database will be utilized to construct the PEM. The PEM will use the most current HIT data to summarize the variation of impacts by position and level of play. One limitation of this approach is that the NFL has not publicly released, nor have there been published reports of HIT System or other head impact sensor data from NFL players, thus resulting in the need to rely on college player HIT System data in these PEMs. We will combine the PEM with each participant’s football history (i.e., age of first exposure, level[s] and duration of play, position[s] played) to develop participant-specific estimates of cumulative exposure to head impacts [27, 61, 160, 161]. Additional methods of estimating repetitive head impact exposure will be included as they become available. Practical proxies of exposure to repetitive head impacts will be examined, such as years of American football play and age of first exposure to American football, among others. Data on the participant’s self-reported number of concussions [162, 163] and number of episodes of loss of consciousness using the Ohio State University TBI Identification Method-Interview Form [164] were collected as metrics of additional history. The participant-specific exposure estimates will be used to evaluate clinical and biomarker outcomes.
Genetics
Whole blood collected at the time of the blood draw was shipped directly to the Molecular Genetics Core at BUSM where DNA was isolated, frozen, and used for apolipoprotein E (APOE) genotyping. We will conduct genome-wide genotyping using the Illumina Global Screening Array (Illumina, Inc., San Diego, CA, USA).
Multidisciplinary Diagnostic Consensus Conferences (MDCC)
Each month there are two MDCCs held through videoconference and attended by a panel of 16 clinician-investigators, including 8 neurologists, 5 neuropsychologists, 2 psychiatrists, and 1 neurosurgeon, from 7 institutions. Each MDCC is required to have a quorum of one panelist from at least three of the four Participant Evaluation Sites, a minimum of two neurologists and two neuropsychologists, representation from at least two sites outside of BU, and a minimum of five panelists in attendance. At each MDCC, the history and findings from approximately 5–9 participants are presented. Following presentation of the history, course, and test score summaries (including measures of subjective cognitive complaints, functional independence, and sleep, as well as neurocognitive, neuropsychiatric, neurologic, and motor functioning), each MDCC member provides their independent diagnosis of TES, in addition to other clinical disorders due to neurodegenerative diseases using established diagnostic criteria (e.g., mild cognitive impairment [MCI] and AD dementia using the National Institute on Aging – Alzheimer’s Association criteria [165]) and psychiatric disorders based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [166]. The MDCC members share and discuss their ratings and adjudicate a final consensus diagnosis (based on majority).
Modified remote follow-up evaluations
As a result of the COVID-19 pandemic, the project co-PIs, in collaboration with NINDS Program Officials, and with input from the Executive Committee and External Advisory Board, decided that all follow-up evaluations would be changed to entirely remote assessments to maintain the safety of our participants and study staff, while also preserving the scientific integrity of the overall study. Remote assessments were required given that participants are flown from their homes to one of the 4 Participant Evaluation Sites, and the pandemic placed severe restrictions on travel. All follow-up procedures were approved by the BUMC IRB. Each participant is assessed for decisional capacity to provide consent for research participation, using a modification of the University of California, San Diego Brief Assessment of Capacity to Consent (UBACC) [167]. Informed consent forms are signed digitally and, in the case of participants who are determined to lack decisional capacity, their research proxy or legally authorized representative digitally signs the consent form. Each participant receives $325 compensation for completion of all follow-up procedures. The modified remote follow-up evaluation is conducted using three separate platforms: (1) telephone, (2) online, and (3) video. Based on prior Baseline Evaluation experience, all participants have access to a telephone and most have access to an internet-connected desktop or laptop computer. Results from a survey conducted of study participants in the spring of 2020 indicated that a large majority have access to a desktop or laptop computer with a webcam for videoconferencing. Most of the tests included in the remote follow-up evaluation have been found to result in comparable performance when administered in-person or remotely via telephone, online, or videoconference platforms [107, 115, 168,169,170,171].
All follow-up participants are interviewed over the telephone to update any history and lifestyle information and to conduct standardized interview-based assessments. In addition, all participants are administered a telephone-based neurocognitive evaluation which includes the telephone modification of the NACC UDS 3.0 cognitive assessment battery (T-Cog, including the Neuropsychological Assessment Battery (NAB) List Learning Test) [99, 110] and the telephone version of the Montreal Cognitive Assessment (MoCA) (T-MoCA) [107]. Participants with access to an internet-connected desktop or laptop computer also complete a battery of web-based computerized cognitive tests from the Cambridge Neuropsychological Test Automated Battery (CANTAB) [114]. Those participants who have a webcam (with proficiency in using these devices determined during a screening prior to follow-up) are administered additional video-based (using the Zoom videoconference platform) neurocognitive tests and also undergo a neurological evaluation, including a modified MDS-UPDRS examination [172, 173], by a board-certified and MDS-UPDRS-trained neurologist who specializes in movement disorders (CHA). Selection of the final battery of neurocognitive measures was made by the full team of project neuropsychologist-investigators to assure that all domains of interest were assessed. All participants and study partners are asked to complete an online REDCap survey to assess cognitive, mood, and behavior difficulties, as well as functional independence, using identical methods employed during baseline evaluations. Follow-up tests and questionnaires, including the modality of assessment, are listed in Tables 3 and 4. The Adverse Childhood Experiences (ACEs) questionnaire [174] was added to the follow-up evaluation to assess childhood factors that may contribute to adult physical and psychological health outcomes.
All consenting participants have a fasting blood draw at their home at the time of their follow-up evaluations. Blood collection and sample preparation is conducted by phlebotomists from ExamOne (a Quest Diagnostics Company, Lenexa, KS) who undergo study-specific training and who are provided with prefabricated blood collection and sample preparation supplies, along with a manual and infographic detailing all procedures, from the BU Coordinating Center. Whole blood, serum, and plasma samples are prepared and aliquoted, put on dry ice within 90 min of centrifugation, and shipped to VA Puget Sound, where they are banked for biomarker assays and distribution to qualified investigators (see Supplementary Material, Additional File 1, for details).
All participants will receive a follow-up diagnosis 4 years after their initial assessment using the NINDS Consensus Diagnostic Criteria for TES [56] through the same MDCC process as baseline diagnoses.
Management and sharing of data and biospecimens
The Biostatistics and Epidemiology Data Analytics Center (BEDAC) at the BU School of Public Health provides data management, database and web development, and data analytics for the project (the latter in collaboration with the project’s lead biostatistician and Data Team Leader (YT)). Data are collected using web-based data capture for assessments using REDCap, as well as customized forms for complex data. Common data elements and study-specific data elements are uploaded to FITBIR on a regular basis to allow for data sharing in the latter part of the project. Once baseline data collection was completed, the Data Team developed a web-based data sharing platform, initially for use by project investigators, with the plan for subsequent availability to all qualified researchers (i.e., in the latter part of the project). Based on the specific needs of an investigator, a customized dataset is created using an automated system. Raw imaging data and fluid biosamples will be made available to qualified investigators (see Supplementary Material, Additional File 1).
Results
Participants
All Participant Evaluation Site institutions (i.e., BU, CC, Mayo, NYU) and associated sites (BWH, BAI) received approval by their governing IRB by January 2017. All participants provided written informed consent during their baseline visit. Enrollment began in September 2016 and the last baseline evaluation was completed in February 2020. The final analytic sample includes 240 men, ages 45–74, including 120 PRO, 60 COL, and 60 UE participants. Table 5 summarizes sample demographics. An additional 24 participants who underwent some or all baseline evaluations are excluded from all data analyses and subsequent evaluation for a variety of reasons, including UE participants who reported a history of concussion (n = 6) or who were found to have extensive psychiatric history (n = 3) during in-person interview, participants with incomplete biomarker data (n = 10), participants who self-withdrew (n = 2), or were withdrawn by a PI for other reasons (n = 3). Three-year follow-up in-person evaluations (for PRO and UE participants) began in October 2019, with 11 completed by March 6, 2020. Due to the COVID-19 pandemic, all in-person study activities were ceased on March 16, 2020. Follow-up evaluations have shifted to fully remote and are being conducted on all participants, including the COL participants (see below for details).
Neuroimaging
Neuroimaging protocols completed include structural T1- and T2-weighted MRI, diffusion MRI (dMRI), resting-state fMRI, MRS, as well as molecular imaging with two PET tracers, florbetapir and flortaucipir. Imaging calibration and quality control (QC) procedures were completed for all sites prior to participant enrollment and throughout data acquisition. PET phantoms from Invicro were checked and each site was certified by the Invicro team using their standard protocols. Additional MRI and MRS harmonization and QC procedures were employed by the BWH Psychiatry Neuroimaging Laboratory (PNL) and Center for Clinical Spectroscopy (CCS) (see Supplementary Material, Additional File 1). The four MRI sequences were acquired in approximately 40 min. Total MRS scan time was 15 min, including shimming. Participants also completed florbetapir and flortaucipir PET scans and 214 participants completed both PET scans. Florbetapir scans were typically conducted first (n = 157 [73%] of the 214 participants who had both PET scans), with at least 12 h between the two scans. PET protocol length is described above.
Fluid biomarkers
At the completion of all baseline evaluations, plasma, and CSF samples were shipped on dry ice overnight from VA Puget Sound to the University of Gothenburg, Sweden, where primary biomarker assays were conducted in batch. Primary fluid biomarkers include plasma and CSF measures of p-tau181, p-tau217, p-tau231, total tau, abeta40, abeta42, abeta38, glial fibrillary acidic protein (GFAP), NfL, soluble triggering receptor expressed on myeloid cells 2 (sTREM2), and soluble platelet-derived growth factor receptor beta (sPDGFRbeta). Supplemental assays will be conducted at VA Puget Sound and University of Washington and will include the following: CSF and plasma CNS-derived extracellular vesicle (EV) total tau and p-tau epitopes 181, 231, and 396; vascular endothelial growth factor-A (VEGF-A); basic fibroblast growth factor (bFGF); interleukins (ILs) 1alpha and beta, 7, and 17a; tumor necrosis factor (TNF)-a; monocyte chemotactic protein (MCP)-1; C-reactive protein (CRP); alpha-synuclein; CSF serum albumin ratio; and CSF catecholamines and indolamines and their precursors and metabolites. Additional CSF, plasma, and saliva biomarkers will be examined as new discoveries direct.
Multidisciplinary Diagnostic Consensus Conferences (MDCC)
MDCCs were completed for all participants following their baseline evaluations using the provisional 2014 TES criteria [54]. MDCCs are being repeated for all baseline evaluations to derive new TES diagnoses using the recently published 2021 NINDS Consensus Diagnostic Criteria for TES [56], but without re-diagnosing other conditions. Only these new TES diagnoses will be used in baseline data analyses. MDCCs will be held following remote follow-up evaluations to determine any change in TES diagnosis (using the 2021 criteria) or in other neurodegenerative and/or psychiatric diagnoses.
First NINDS Consensus Workshop to define the diagnostic criteria for TES
Refinement and validation of the 2014 research diagnostic criteria for TES [54] is an aim of the DIAGNOSE CTE Research Project. Since the time of the original 2014 publication, the TES criteria have been used in several ongoing research studies, including the UNITE study [55] and for the initial baseline evaluation MDCCs in this DIAGNOSE CTE Research Project. In April 2019, the First NINDS Consensus Workshop to Define the Diagnostic Criteria for TES was held in Phoenix, Arizona. The goal of the workshop was to evaluate and update TES criteria based on the following: (1) inter-rater reliability data from research studies (including baseline MDCC data from this project); (2) predictive validity data, both published [55] and unpublished, examining the relationship between the specific criteria and neuropathologically diagnosed CTE; (3) systematic review of CTE literature to date; and (4) expert opinion. A Modified Delphi approach was followed and included a first round of anonymous voting that took place during the Workshop, followed by three additional online voting rounds on revised criteria. Voting panelists included 20 clinician-researchers across a variety of disciplines (e.g., Neurology, Neuropsychology, Psychiatry, Physical Medicine and Rehabilitation, Neurosurgery), areas of expertise (e.g., neurodegenerative disease, TBI), and academic institutions (i.e., ten). The Delphi process was completed in January 2020 and a report on the new NINDS Consensus Diagnostic Criteria for TES was published in 2021 [56]. These new TES diagnostic criteria are intended for research purposes and not for clinical diagnosis. It is expected that the criteria will be further updated and revised through future NINDS Consensus Workshops as research in this field and on the criteria evolve and biomarker data become available.
Discussion
This report provides a description of the methodology for the DIAGNOSE CTE Research Project, a multicenter, observational, cohort study designed to develop, refine, and validate in vivo biomarkers for CTE; characterize the clinical course and presentation of this tauopathy; identify potential risk factors; and refine and validate research diagnostic criteria for the clinical presentation associated with CTE (i.e., TES). This report also provides a description of the demographics of the sample, comprised of 120 former NFL players, 60 former college football players, and 60 unexposed same-age asymptomatic men.
Methodological decisions were made in designing the DIAGNOSE CTE Research Project based on the overarching goal of establishing clinical diagnostic criteria for CTE with highly accurate in vivo biomarkers. As such, we decided to focus on a sample of former college and professional American football players to ensure a sample at high risk for CTE [3] and to maximize power for hypothesis testing. Although the inclusion of a more heterogeneous sample of contact and collision sport athletes (e.g., boxers, soccer players, ice hockey players, including women), as well as participants with other sources of repetitive head impact exposure, such as military combat veterans with blast-injuries, survivors of intimate partner violence, and younger participants, may increase generalizability, it would be difficult to estimate “exposure” levels or achieve adequate statistical power or assure that the sample was at high risk for CTE. Thus, at the time of initial development of in vivo CTE diagnostics, homogeneity of the source of repetitive head impacts was prioritized. An area of active investigation by our team includes other, non-football contact sport athletes (e.g., soccer, ice hockey, rugby), particularly female former contact sport athletes. Some investigators of DIAGNOSE CTE are leading a new NIH-funded initiative (PI: Stern), known as the Head Impact and Trauma Surveillance Study (HITSS), that will leverage the online Brain Health Registry platform and recruit, enroll, and longitudinally follow female and male former soccer players and male former American football players (across all levels of play). This initiative will increase our understanding of the long-term effects of repetitive head impacts across sports and in females, and lead to future investigations that are similar to DIAGNOSE CTE, allowing for rich clinical characterizations of female former contact sport athletes.
The UE group was carefully selected. If the primary goal was to study disease risk, then certain variables should have been well-controlled, e.g., cardiovascular/cerebrovascular risks, performance enhancing drug use, substance use, history of team sport involvement. However, our primary goals were to examine possible biomarkers to detect CTE and the refinement of diagnostic criteria for the clinical manifestations of CTE. Therefore, our comparison group included individuals who were similar to the former American football players in terms of age, sex, and BMI, but did not have repetitive head impact exposure and were asymptomatic. This type of design is appropriate for biomarker development and validation. Importantly, while the UE group will allow us to answer questions regarding biomarker development and validation, their inclusion in other types of analyses requires careful consideration. For instance, it would be inappropriate to characterize the effect of repetitive head impact exposure on clinical measures in both the former player groups and UE group, given that the UE group was required to be asymptomatic (for neurological and psychiatric conditions) at the time of recruitment and the former players were not. Even among questions pertaining to biomarkers, it will be important to conduct sensitivity analyses to determine if any potential group differences are related to exposure to repetitive head impacts or to other factors. Lastly, other types of “control” groups were considered, but not incorporated into the design of the study. There have been efforts to recruit former professional baseball players or body builders as controls for similar studies, because they have similar lifestyles and body habitus as former American football players. Yet, there have been very few who had never participated in organized contact sports or who, in the case of baseball players, had not reported multiple concussions. Planned ancillary studies will also recruit participants with AD dementia and AD-related dementias as disease comparison groups to the former profession American football players.
All participants were required to have a study partner who knows them well to provide assessments of their perspective of the participant’s cognitive, behavioral, and functional status. In some cases, these reports may be inaccurate due to a variety of factors, including misattributions of symptoms to age-related changes or stress; exaggeration of deficits for potential secondary gain (including financial compensation from disability or legal cases); and denial/unawareness of deficits (including anosognosia) due to neurodegenerative disease and other neurologic conditions. This requirement may introduce some degree of selection bias due to the potential for some participants with underlying CTE to have neuropsychiatric features (e.g., rage, aggression, impulsivity) that result in the loss of close relationships and overall social isolation. Therefore, it is possible that potential participants with more severe neuropsychiatric features were excluded due to those features limiting the availability of a study partner.
The primary method of validating biomarkers for the detection of CTE pathology or to truly examine risk factors for the development of CTE pathology is to compare data collected during life with postmortem neuropathology and diagnosis. The large majority of former college and professional football players in the DIAGNOSE CTE cohort have agreed to brain donation. At the time of the current paper, five former players had already died, and their brain tissue will be examined for these clinicopathological correlation and validation studies.
Our goal was to enroll a similar proportion of Black participants across the three exposure groups (i.e., PRO, COL, UE), with the target of approximately 40% overall. Although the PRO and UE groups have a similar proportion of Black participants, with 42.5% and 40.0%, respectively, the COL group has a significantly smaller proportion of black participants (16.7%). Interactive effects between levels of exposure to repetitive head impacts and Black racial identity on potential neuroimaging and fluid biomarkers of CTE have been reported [161]. Moreover, there are potential differences between Black and White participants in the expression of psychiatric symptoms and performance on cognitive tests [175, 176], as well as important racial disparities in life-course social determinants of health, cognitive aging, and neurodegenerative disease [177,178,179]. For these reasons, interpretation of data analyses including the COL group will be done with these racial identity differences in mind [180].
Conclusions
The DIAGNOSE CTE Research Project will lead to a rich dataset that will be used to further our understanding of CTE in terms of its clinical presentation, in vivo biomarkers, clinical research diagnostic criteria, and risk and resiliency factors for the development of CTE. In addition to repetitive head impact exposure and genetic factors, project data will inform on the role of demographic, lifestyle, medical, and psychiatric risk and resilience variables, as well as on social determinants of health and racial disparities. Importantly, the data will provide the infrastructure and resources for opportunities to conduct ancillary or add-on studies that target questions not being directly examined by the DIAGNOSE CTE Research Project. Ultimately, it is anticipated that findings from the DIAGNOSE CTE Research Project and associated ancillary studies will facilitate the ability to detect and diagnose CTE during life and thereby accelerate research on risk factors, mechanisms, epidemiology, and, most importantly, treatment and prevention of CTE.
Availability of data and materials
The datasets generated and analyzed during the current study will be available in the Federal Interagency Traumatic Brain Injury Research (FITBIR) repository, https://fitbir.nih.gov. Datasets will also be available through a data sharing portal for the DIAGNOSE CTE Research Project, http://diagnosecte.com. It is also anticipated that study datasets will be available in the Global Alzheimer’s Association Interactive Network (GAAIN) repository, http://www.gaain.org.
Abbreviations
- 3R:
-
Three microtubule-binding domain repeat tau isoform
- 4R:
-
Four microtubule-binding domain repeat tau isoform
- Aβ:
-
Beta-amyloid
- AD:
-
Alzheimer’s disease
- AxD:
-
Axial diffusivity
- BAI:
-
Banner Alzheimer’s Institute
- BMI:
-
Body mass index
- BU:
-
Boston University
- BUMC:
-
Boston University Medical Campus
- BUSM:
-
Boston University School of Medicine
- BWH:
-
Brigham and Women’s Hospital
- CC:
-
Cleveland Clinic
- CDE:
-
Common Data Elements
- CSF:
-
Cerebrospinal fluid
- COL:
-
Former college player group
- CTE:
-
Chronic traumatic encephalopathy
- DEI:
-
Diversity, equity, and inclusion
- DIAGNOSE CTE:
-
Diagnostics, Imaging, and Genetics Network for the Objective Study and Evaluation of Chronic Traumatic Encephalopathy
- dMRI:
-
Diffusion MRI
- DTI:
-
Diffusion tensor imaging
- FA:
-
Fractional anisotropy
- FITBIR:
-
Federal Interagency Traumatic Brain Injury Research
- FLAIR:
-
Fluid attenuated inversion recovery
- fMRI:
-
Functional magnetic resonance imaging
- GWAS:
-
Genome-wide sequencing studies
- IRB:
-
Institutional Review Board
- LP:
-
Lumbar puncture
- MD:
-
Mean diffusivity
- MDCC:
-
Multidisciplinary diagnostic consensus conference
- MDS:
-
Movement Disorder Society
- MRI:
-
Magnetic resonance imaging
- MRS:
-
Magnetic resonance spectroscopy
- NFL:
-
National Football League
- NFT:
-
Neurofibrillary tangle
- NINDS:
-
National Institute for Neurological Disorders and Stroke
- NYU:
-
New York University
- PET:
-
Positron emission tomography
- PI:
-
Principal investigator
- PNL:
-
Psychiatry Neuroimaging Laboratory
- PRO:
-
Former profession (NFL) player group
- p-tau:
-
Hyperphosphorylated tau
- QC:
-
Quality control
- RD:
-
Radial diffusivity
- SNP:
-
Single-nucleotide polymorphism
- TBI:
-
Traumatic brain injury
- TES:
-
Traumatic encephalopathy syndrome
- t-tau:
-
Total tau
- UDS:
-
Uniform Data Set
- UE:
-
Unexposed group
- UNITE:
-
Understanding Neurologic Injury in Traumatic Encephalopathy
References
McKee AC, Cantu RC, Nowinski CJ, Hedley-Whyte ET, Gavett BE, Budson AE, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropath Exp Neurol. 2009;68(7):709–35. https://doi.org/10.1097/NEN.0b013e3181a9d503.
McKee AC, Stern RA, Nowinski CJ, Stein TD, Alvarez VE, Daneshvar DH, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain. 2013;136(1):43–64. https://doi.org/10.1093/brain/aws307.
Mez J, Daneshvar DH, Kiernan PT, Abdolmohammadi B, Alvarez VE, Huber BR, et al. Clinicopathological evaluation of chronic traumatic encephalopathy in players of American Football. JAMA. 2017;318(4):360–70. https://doi.org/10.1001/jama.2017.8334.
Goldstein LE, Fisher AM, Tagge CA, Zhang XL, Velisek L, Sullivan JA, et al. Chronic traumatic encephalopathy in blast-exposed military veterans and a blast neurotrauma mouse model. Sci Transl Med. 2012;16(134):1–16.
Omalu BI, DeKosky ST, Minster RL, Kamboh MI, Hamilton RL, Wecht CH. Chronic traumatic encephalopathy in a National Football League player. Neurosurgery. 2005;57(1):128–34. https://doi.org/10.1227/01.NEU.0000163407.92769.ED.
Omalu BI, DeKosky ST, Hamilton RL, Minster RL, Kamboh MI, Shakir AM, et al. Chronic traumatic encephalopathy in a National Football League player: part II. Neurosurgery. 2006;59(5):1086–92. https://doi.org/10.1227/01.NEU.0000245601.69451.27.
Omalu BI, Fitzsimmons RP, Hammers J, Bailes J. Chronic traumatic encephalopathy in a professional American wrestler. J Forensic Nursing. 2010;6(3):130–6. https://doi.org/10.1111/j.1939-3938.2010.01078.x.
Ling H, Morris HR, Neal JW, Lees AJ, Hardy J, Holton JL, et al. Mixed pathologies including chronic traumatic encephalopathy account for dementia in retired association football (soccer) players. Acta Neuropathol. 2017;133(3):337–52. https://doi.org/10.1007/s00401-017-1680-3.
Bieniek KF, Ross OA, Cormier KA, Walton RL, Soto-Ortolaza A, Johnston AE, et al. Chronic traumatic encephalopathy pathology in a neurodegenerative disorders brain bank. Acta Neuropathol. 2015;130(6):877–89. https://doi.org/10.1007/s00401-015-1502-4.
Martland HS. Punch drunk. JAMA. 1928;91(15):1103–7. https://doi.org/10.1001/jama.1928.02700150029009.
Millspaugh JA. Dementia pugilistica. US Naval Med Bull. 1937;35:297–303.
Bowman KM, Blau A. Psychotic states following head and brain injury in adults and children. Injuries of the skull, brain and spinal cord: Neuro-psychiatric, surgical, and medico-legal aspects. Baltimore: Williams & Wilkins Co; 1940.
Critchley M. Punch-drunk syndromes: the chronic traumatic encephalopathy of boxers. In: Vincent C, editor. Neurochirurgie Hommage à Clovis Vincent. Paris: Maloine; 1949.
Buckland ME, Sy J, Szentmariay I, Kullen A, Lee M, Harding A, et al. Chronic traumatic encephalopathy in two former Australian National Rugby League players. Acta Neuropathol Comm. 2019;7(1):97. https://doi.org/10.1186/s40478-019-0751-1.
Alosco ML, Cherry JD, Huber BR, Tripodis Y, Baucom ZH, Kowall NW, et al. Characterizing tau deposition in chronic traumatic encephalopathy (CTE): Utility of the McKee CTE Staging Scheme. Acta Neuropathol. 2020;140(4):495–512. https://doi.org/10.1007/s00401-020-02197-9.
Mez J, Solomon TM, Daneshvar DH, Murphy L, Kiernan PT, Montenigro PH, et al. Assessing clinicopathological correlation in chronic traumatic encephalopathy: rationale and methods for the UNITE study. Alzheimers Res Ther. 2015;7(1):62. https://doi.org/10.1186/s13195-015-0148-8.
McKee AC, Cairns NJ, Dickson DW, Folkerth RD, Keene CD, Litvan I, et al. The first NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. Acta Neuropathol. 2016;131(1):75–86. https://doi.org/10.1007/s00401-015-1515-z.
Bieniek KF, Cairns NJ, Crary JF, Dickson DW, Folkerth RD, Keene CD, et al. The second NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. J Neuropath Exp Neurol. 2021;80(3):210–9. https://doi.org/10.1093/jnen/nlab001.
Falcon B, Zivanov J, Zhang W, Murzin AG, Garringer HJ, Vidal R, et al. Novel tau filament fold in chronic traumatic encephalopathy encloses hydrophobic molecules. Nature. 2019;568(7752):420–3. https://doi.org/10.1038/s41586-019-1026-5.
Falcon B, Zhang W, Murzin AG, Murshudov G, Garringer HJ, Vidal R, et al. Structures of filaments from Pick's disease reveal a novel tau protein fold. Nature. 2018;561(7721):137–40. https://doi.org/10.1038/s41586-018-0454-y.
Zhang W, Tarutani A, Newell KL, Murzin AG, Matsubara T, Falcon B, et al. Novel tau filament fold in corticobasal degeneration. Nature. 2020;580(7802):283–7. https://doi.org/10.1038/s41586-020-2043-0.
Cherry JD, Kim SH, Stein TD, Pothast MJ, Nicks R, Meng G, et al. Evolution of neuronal and glial tau isoforms in chronic traumatic encephalopathy. Brain Pathol. 2020;30(5):913–25. https://doi.org/10.1111/bpa.12867.
Stein TD, Montenigro PH, Alvarez VE, Xia W, Crary JF, Tripodis Y, et al. Beta-amyloid deposition in chronic traumatic encephalopathy. Acta Neuropathol. 2015;130(1):21–34. https://doi.org/10.1007/s00401-015-1435-y.
Alosco ML, Stein TD, Tripodis Y, Chua AS, Kowall NW, Huber BR, et al. Association of white matter rarefaction, arteriolosclerosis, and tau with dementia in chronic traumatic encephalopathy. JAMA Neurol. 2019;76(11):1298–308. https://doi.org/10.1001/jamaneurol.2019.2244.
Adams JW, Alvarez VE, Mez J, Huber BR, Tripodis Y, Xia W, et al. Lewy body pathology and chronic traumatic encephalopathy associated with contact sports. J Neuropathol Exp Neurol. 2018;77(9):757–68. https://doi.org/10.1093/jnen/nly065.
Standring OJ, Friedberg J, Tripodis Y, Chua AS, Cherry JD, Alvarez VE, et al. Contact sport participation and chronic traumatic encephalopathy are associated with altered severity and distribution of cerebral amyloid angiopathy. Acta Neuropathol. 2019;138(3):401–13. https://doi.org/10.1007/s00401-019-02031-x.
Montenigro PH, Alosco ML, Martin BM, Daneshvar DH, Mez J, Chaisson CE, et al. Cumulative head impact exposure predicts later-life depression, apathy, executive dysfunction, and cognitive impairment in former high school and college football players. J Neurotrauma. 2017;34(2):328–40. https://doi.org/10.1089/neu.2016.4413.
Bieniek KF, Blessing MM, Heckman MG, Diehl NN, Serie AM, Paolini MA 2nd, et al. Association between contact sports participation and chronic traumatic encephalopathy: a retrospective cohort study. Brain Pathol. 2020;30(1):63–74. https://doi.org/10.1111/bpa.12757.
Cherry JD, Tripodis Y, Alvarez VE, Huber B, Kiernan PT, Daneshvar DH, et al. Microglial neuroinflammation contributes to tau accumulation in chronic traumatic encephalopathy. Acta neuropathol Commun. 2016;4(1):112. https://doi.org/10.1186/s40478-016-0382-8.
Mez J, Daneshvar DH, Abdolmohammadi B, Chua AS, Alosco ML, Kiernan PT, et al. Duration of American football play and chronic traumatic encephalopathy. Ann Neurol. 2020;87(1):116–31. https://doi.org/10.1002/ana.25611.
Morley WA. Environmental subconcussive injury, axonal injury, and chronic traumatic encephalopathy. Front Neurol. 2018;9:166. https://doi.org/10.3389/fneur.2018.00166.
Stein TD, Alvarez VE, McKee AC. Concussion in chronic traumatic encephalopathy. Curr Pain Headache Rep. 2015;19(10):47. https://doi.org/10.1007/s11916-015-0522-z.
Roberts AL, Pascual-Leone A, Speizer FE, Zafonte RD, Baggish AL, Taylor H Jr, et al. Exposure to American football and neuropsychiatric health in former National Football League players: findings from the football players health study. Am J Sports Med. 2019;47(12):2871–80. https://doi.org/10.1177/0363546519868989.
Wright MJ, Woo E, Birath JB, Siders CA, Kelly DF, Wang C, et al. An index predictive of cognitive outcome in retired professional American Football players with a history of sports concussion. J Clin Exp Neuropsychol. 2016;38(5):561–71. https://doi.org/10.1080/13803395.2016.1139057.
Kochsiek J, O'Donnell LJ, Zhang F, Bonke EM, Sollmann N, Tripodis Y, et al. Exposure to repetitive head impacts is associated with corpus callosum microstructure and plasma total tau in former professional American football players. J Magnetic Resonance Imaging 202;1 Jun 16. doi: 10.1002/jmri.27774. Online ahead of print.
Esopenko C, Chow TW, Tartaglia MC, Bacopulos A, Kumar P, Binns MA, et al. Cognitive and psychosocial function in retired professional hockey players. J Neurol Neurosurg Psychiatry. 2017;88(6):512–9. https://doi.org/10.1136/jnnp-2016-315260.
McMillan TM, McSkimming P, Wainman-Lefley J, Maclean LM, Hay J, McConnachie A, et al. Long-term health outcomes after exposure to repeated concussion in elite level: rugby union players. J Neurol Neurosurg Psychiatry. 2017;88(6):505–11. https://doi.org/10.1136/jnnp-2016-314279.
Montenigro PH, Bernick C, Cantu RC. Clinical features of repetitive traumatic brain injury and chronic traumatic encephalopathy. Brain Pathol. 2015;25(3):304–17. https://doi.org/10.1111/bpa.12250.
Alosco ML, Kasimis AB, Stamm JM, Chua AS, Baugh CM, Daneshvar DH, et al. Age of first exposure to American football and long-term neuropsychiatric and cognitive outcomes. Translational Psychiatry. 2017;7(9):e1236. https://doi.org/10.1038/tp.2017.197.
Stamm JM, Bourlas AP, Baugh CM, Fritts NG, Daneshvar DH, Martin BM, et al. Age of first exposure to football and later-life cognitive impairment in former NFL players. Neurology. 2015;84(11):1114–20. https://doi.org/10.1212/WNL.0000000000001358.
Schultz V, Stern RA, Tripodis Y, Stamm J, Wrobel P, Lepage C, et al. Age at first exposure to repetitive head impacts is associated with smaller thalamic volumes in former professional American football players. J Neurotrauma. 2018;35(2):278–85. https://doi.org/10.1089/neu.2017.5145.
Stamm JM, Koerte IK, Muehlmann M, Pasternak O, Bourlas AP, Baugh CM, et al. Age at first exposure to football is associated with altered corpus callosum white matter microstructure in former professional football players. J Neurotrauma. 2015;32(22):1768–76. https://doi.org/10.1089/neu.2014.3822.
Alosco ML, Mez J, Tripodis Y, Kiernan PT, Abdolmohammadi B, Murphy L, et al. Age of first exposure to tackle football and chronic traumatic encephalopathy. Ann Neurology. 2018;83(5):886–901. https://doi.org/10.1002/ana.25245.
Kaufmann D, Sollmann N, Kaufmann E, Veggeberg R, Tripodis Y, Wrobel PP, et al. Age at first exposure to tackle football is associated with cortical thickness in former professional American football players. Cerebral Cortex. 2021;31(7):3426–34. https://doi.org/10.1093/cercor/bhab021.
Alosco ML, Mez J, Kowall NW, Stein TD, Goldstein LE, Cantu RC, et al. Cognitive reserve as a modifier of clinical expression in chronic traumatic encephalopathy: a preliminary examination. J Neuropsychiat Clin Neurosci. 2017;29(1):6–12. https://doi.org/10.1176/appi.neuropsych.16030043.
Alosco ML, Koerte IK, Tripodis Y, Mariani M, Chua AS, Jarnagin J, et al. White matter signal abnormalities in former National Football League players. Alzheimer's Dementia. 2018;10(1):56–65. https://doi.org/10.1016/j.dadm.2017.10.003.
Stern RA, Daneshvar DH, Baugh CM, Seichepine DR, Montenigro PH, Riley D, et al. Clinical presentation of chronic traumatic encephalopathy. Neurology. 2013;81(13):1122–9. https://doi.org/10.1212/WNL.0b013e3182a55f7f.
Cherry JD, Mez J, Crary JF, Tripodis Y, Alvarez VE, Mahar I, et al. Variation in TMEM106B in chronic traumatic encephalopathy. Acta Neuropathol Comm. 2018;6(1):115. https://doi.org/10.1186/s40478-018-0619-9.
Phelps A, Mez J, Stern RA, Alosco ML. Risk factors for chronic traumatic encephalopathy: a proposed framework. Sem Neurol. 2020;40(4):439–49.
Mariani M, Alosco ML, Mez J, Stern RA. Clinical presentation of chronic traumatic encephalopathy. Sem Neurol. 2020;40(4):370–83.
McKee AC, Gavett BE, Stern RA, Nowinski CJ, Cantu RC, Kowall NW, et al. TDP-43 proteinopathy and motor neuron disease in chronic traumatic encephalopathy. J Neuropath Exp Neurology. 2010;69(9):918–29. https://doi.org/10.1097/NEN.0b013e3181ee7d85.
Jordan BD. The clinical spectrum of sport-related traumatic brain injury. Nat Rev Neurol. 2013;9(4):222–30. https://doi.org/10.1038/nrneurol.2013.33.
Victoroff J. Traumatic encephalopathy: review and provisional research diagnostic criteria. NeuroRehabilitation. 2013;32(2):211–24. https://doi.org/10.3233/NRE-130839.
Montenigro PH, Baugh CM, Daneshvar DH, Mez J, Budson AE, Au R, et al. Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimers Res Ther. 2014;6(5):68. https://doi.org/10.1186/s13195-014-0068-z.
Mez J, Alosco ML, Daneshvar DH, Saltiel N, Baucom Z, Abdolmohammadi B, et al. Validity of the 2014 traumatic encephalopathy syndrome criteria for CTE pathology. Alzheimer's Dementia. 2021. https://doi.org/10.1002/alz.12338 Online ahead of print.
Katz DI, Bernick C, Dodick DW, Mez J, Mariani ML, Adler CH, et al. National Institute of Neurological Disorders and Stroke Consensus Diagnostic Criteria for Traumatic Encephalopathy Syndrome. Neurology. 2021;96(18):848–63. https://doi.org/10.1212/WNL.0000000000011850.
Jack CR Jr, Bennett DA, Blennow K, Carrillo MC, Feldman HH, Frisoni GB, et al. A/T/N: An unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology. 2016;87(5):539–47. https://doi.org/10.1212/WNL.0000000000002923.
Jack CR Jr, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer's disease. Alzheimer's Dementia. 2018;14(4):535–62. https://doi.org/10.1016/j.jalz.2018.02.018.
McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor JP, Weintraub D, et al. Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology. 2017;89(1):88–100. https://doi.org/10.1212/WNL.0000000000004058.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimer's Dementia. 2011;7(3):263–9. https://doi.org/10.1016/j.jalz.2011.03.005.
Alosco ML, Tripodis Y, Fritts NG, Heslegrave A, Baugh CM, Conneely S, et al. Cerebrospinal fluid tau, Abeta, and sTREM2 in former National Football League players: modeling the relationship between repetitive head impacts, microglial activation, and neurodegeneration. Alzheimer's Dementia. 2018;4(9):1159–70.
Alosco ML, Tripodis Y, Jarnagin J, Baugh CM, Martin B, Chaisson CE, et al. Repetitive head impact exposure and later-life plasma total tau in former National Football League players. Alzheimer's Dementia. 2017;7(1):33–40. https://doi.org/10.1016/j.dadm.2016.11.003.
Dickstein DL, De Gasperi R, Gama Sosa MA, Perez-Garcia G, Short JA, Sosa H, et al. Brain and blood biomarkers of tauopathy and neuronal injury in humans and rats with neurobehavioral syndromes following blast exposure. Mol Psychiatry. 2020. https://doi.org/10.1038/s41380-020-0674-z Online ahead of print.
Muraoka S, Jedrychowski MP, Tatebe H, DeLeo AM, Ikezu S, Tokuda T, et al. Proteomic profiling of extracellular vesicles isolated from cerebrospinal fluid of former National Football League players at risk for chronic traumatic encephalopathy. Front Neurosci. 2019;13:1059. https://doi.org/10.3389/fnins.2019.01059.
Goetzl EJ, Ledreux A, Granholm AC, Elahi FM, Goetzl L, Hiramoto J, et al. Neuron-derived exosome proteins may contribute to progression from repetitive mild traumatic brain injuries to chronic traumatic encephalopathy. Front Neurosci. 2019;13:452. https://doi.org/10.3389/fnins.2019.00452.
Stern RA, Tripodis Y, Baugh CM, Fritts NG, Martin BM, Chaisson C, et al. Preliminary study of plasma exosomal tau as a potential biomarker for chronic traumatic encephalopathy. J Alzheimer's Dis. 2016;51(4):1099–109. https://doi.org/10.3233/JAD-151028.
Alosco ML, Culhane J, Mez J. Neuroimaging biomarkers of chronic traumatic encephalopathy: targets for the academic memory disorders clinic. Neurotherapeutics. 2021. https://doi.org/10.1007/s13311-021-01028-3 Online ahead of print.
Lin A, Charney M, Shenton ME, Koerte IK. Chronic traumatic encephalopathy: neuroimaging biomarkers. Handbook Clinical Neurol. 2018;158:309–22. https://doi.org/10.1016/B978-0-444-63954-7.00029-X.
Gardner RC, Hess CP, Brus-Ramer M, Possin KL, Cohn-Sheehy BI, Kramer JH, et al. Cavum septum pellucidum in retired American pro-football players. J Neurotrauma. 2016;33(1):157–61. https://doi.org/10.1089/neu.2014.3805.
Gardner RC, Possin KL, Hess CP, Huang EJ, Grinberg LT, Nolan AL, et al. Evaluating and treating neurobehavioral symptoms in professional American football players: Lessons from a case series. Neurol Clin Pract. 2015;5(4):285–95. https://doi.org/10.1212/CPJ.0000000000000157.
Koerte IK, Hufschmidt J, Muehlmann M, Tripodis Y, Stamm JM, Pasternak O, et al. Cavum septi pellucidi in symptomatic former professional football players. J Neurotrauma. 2016;33(4):346–53. https://doi.org/10.1089/neu.2015.3880.
Kuhn AW, Zuckerman SL, Solomon G, Casson I. Interrelationships among neuroimaging biomarkers, neuropsychological test data, and symptom reporting in a cohort of retired National Football League players. Neurosurgery. 2016;63(Suppl 1):173.
Coughlin JM, Wang Y, Munro CA, Ma S, Yue C, Chen S, et al. Neuroinflammation and brain atrophy in former NFL players: An in vivo multimodal imaging pilot study. Neurobiol Dis. 2015;74:58–65. https://doi.org/10.1016/j.nbd.2014.10.019.
Goswami R, Dufort P, Tartaglia MC, Green RE, Crawley A, Tator CH, et al. Frontotemporal correlates of impulsivity and machine learning in retired professional athletes with a history of multiple concussions. Brain Struct Funct. 2016;221(4):1911–25. https://doi.org/10.1007/s00429-015-1012-0.
Adler CM, DelBello MP, Weber W, Williams M, Duran LR, Fleck D, et al. MRI evidence of neuropathic changes in former college football players. Clin J Sport Med. 2018;28(2):100–5. https://doi.org/10.1097/JSM.0000000000000391.
Singh R, Meier TB, Kuplicki R, Savitz J, Mukai I, Cavanagh L, et al. Relationship of collegiate football experience and concussion with hippocampal volume and cognitive outcomes. JAMA. 2014;311(18):1883–8. https://doi.org/10.1001/jama.2014.3313.
Lesman-Segev OH, Edwards L, Rabinovici GD. Chronic traumatic encephalopathy: a comparison with Alzheimer's disease and frontotemporal dementia. Sem Neurology. 2020;40(4):394–410.
Mantyh WG, Spina S, Lee A, Iaccarino L, Soleimani-Meigooni D, Tsoy E, et al. Tau positron emission tomographic findings in a former US football player with pathologically confirmed chronic traumatic encephalopathy. JAMA Neurol. 2020.
Lepage C, Muehlmann M, Tripodis Y, Hufschmidt J, Stamm J, Green K, et al. Limbic system structure volumes and associated neurocognitive functioning in former NFL players. Brain Imaging Behav. 2019;13(3):725–34. https://doi.org/10.1007/s11682-018-9895-z.
Strain J, Didehbani N, Cullum CM, Mansinghani S, Conover H, Kraut MA, et al. Depressive symptoms and white matter dysfunction in retired NFL players with concussion history. Neurology. 2013;81(1):25–32. https://doi.org/10.1212/WNL.0b013e318299ccf8.
Strain JF, Didehbani N, Spence J, Conover H, Bartz EK, Mansinghani S, et al. White matter changes and confrontation naming in retired aging National Football League athletes. J Neurotrauma. 2016;34(2):372–9. https://doi.org/10.1089/neu.2016.4446.
Mishra VR, Zhuang X, Sreenivasan KR, Banks SJ, Yang Z, Bernick C, et al. Multimodal MR imaging signatures of cognitive impairment in active professional fighters. Radiology. 2017;285(2):555–67. https://doi.org/10.1148/radiol.2017162403.
Bazarian JJ, Zhu T, Zhong J, Janigro D, Rozen E, Roberts A, et al. Persistent, long-term cerebral white matter changes after sports-related repetitive head impacts. Plos One. 2014;9(4):e94734. https://doi.org/10.1371/journal.pone.0094734.
Koerte IK, Ertl-Wagner B, Reiser M, Zafonte R, Shenton ME. White matter integrity in the brains of professional soccer players without a symptomatic concussion. JAMA. 2012;308(18):1859–61. https://doi.org/10.1001/jama.2012.13735.
Amen DG, Willeumier K, Omalu B, Newberg A, Raghavendra C, Raji CA. Perfusion neuroimaging abnormalities alone distinguish National Football League players from a healthy population. J Alzheimer's D. 2016;53(1):237–41. https://doi.org/10.3233/JAD-160207.
Hart J Jr, Kraut MA, Womack KB, Strain J, Didehbani N, Bartz E, et al. Neuroimaging of cognitive dysfunction and depression in aging retired National Football League players: a cross-sectional study. JAMA Neurology. 2013;70(3):326–35. https://doi.org/10.1001/2013.jamaneurol.340.
Hampshire A, MacDonald A, Owen AM. Hypoconnectivity and hyperfrontality in retired American football players. Sci Rep. 2013;3(1):2972. https://doi.org/10.1038/srep02972.
Alosco ML, Tripodis Y, Rowland B, Chua AS, Liao H, Martin B, et al. A magnetic resonance spectroscopy investigation in symptomatic former NFL players. Brain Imaging Behav. 2020;14(5):1419–29. https://doi.org/10.1007/s11682-019-00060-4.
Lin AP, Ramadan S, Stern RA, Box HC, Nowinski CJ, Ross BD, et al. Changes in the neurochemistry of athletes with repetitive brain trauma: preliminary results using localized correlated spectroscopy. Alzheimers Res Ther. 2015;7(1):13. https://doi.org/10.1186/s13195-015-0094-5.
Tremblay S, De Beaumont L, Henry LC, Boulanger Y, Evans AC, Bourgouin P, et al. Sports concussions and aging: a neuroimaging investigation. Cerebral Cortex. 2013;23(5):1159–66. https://doi.org/10.1093/cercor/bhs102.
Clark CM, Pontecorvo MJ, Beach TG, Bedell BJ, Coleman RE, Doraiswamy PM, et al. Cerebral PET with florbetapir compared with neuropathology at autopsy for detection of neuritic amyloid-β plaques: a prospective cohort study. Lancet Neurol. 2012;11(8):669–78. https://doi.org/10.1016/S1474-4422(12)70142-4.
Fleisher AS, Pontecorvo MJ, Devous MD Sr, Lu M, Arora AK, Truocchio SP, et al. Positron Emission Tomography Imaging With [18F]flortaucipir and Postmortem Assessment of Alzheimer Disease Neuropathologic Changes. JAMA Neurology. 2020;77(7):829–39. https://doi.org/10.1001/jamaneurol.2020.0528.
Tsai RM, Bejanin A, Lesman-Segev O, LaJoie R, Visani A, Bourakova V, et al. (18)F-flortaucipir (AV-1451) tau PET in frontotemporal dementia syndromes. Alzheimers Res Ther. 2019;11(1):13.
Soleimani-Meigooni DN, Iaccarino L, La Joie R, Baker S, Bourakova V, Boxer AL, et al. 18F-flortaucipir PET to autopsy comparisons in Alzheimer's disease and other neurodegenerative diseases. Brain. 2020;143(11):3477–94. https://doi.org/10.1093/brain/awaa276.
Stern RA, Adler CH, Chen K, Navitsky M, Luo J, Dodick DW, et al. Tau positron-emission tomography in former National Football League players. N Engl J Med. 2019;380(18):1716–25. https://doi.org/10.1056/NEJMoa1900757.
Marquie M, Aguero C, Amaral AC, Villarejo-Galende A, Ramanan P, Chong MST, et al. [(18)F]-AV-1451 binding profile in chronic traumatic encephalopathy: a postmortem case series. Acta Neuropath Comm. 2019;7(1):164.
Lesman-Segev OH, La Joie R, Stephens ML, Sonni I, Tsai R, Bourakova V, et al. Tau PET and multimodal brain imaging in patients at risk for chronic traumatic encephalopathy. Neuroimage Clin. 2019;24:102025. https://doi.org/10.1016/j.nicl.2019.102025.
Golden CJ, Freshwater SM. Stroop Color and Word Test. Torrance: Western Psychological Services (WPS); 2002.
Stern RA, White T. Neuropsychological Assessment Battery. Lutz, FL: Psychological Assessment Resources, Inc.; 2003.
Gavett BE, Ozonoff A, Doktor V, Palmisano J, Nair AK, Green RC, et al. Predicting cognitive decline and conversion to Alzheimer's disease in older adults using the NAB List Learning test. J Int Neuropsychol Soc. 2010;16(4):651–60. https://doi.org/10.1017/S1355617710000421.
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, et al. Movement Disorder Society-sponsored revision of the Unified Parkinson's Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008;23(15):2129–70. https://doi.org/10.1002/mds.22340.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Amer Geriatrics Soc. 1991;39(2):142–8. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x.
Tombaugh T. Test of Memory Malingering (TOMM). North Tonawanda: Multi-Health Systems; 1996.
Benedict RHB. Brief Visuospatial Memorty Test-Revised. Lutz: Psychological Assessment Resources, Inc.; 1997.
Wilkinson GS, Robertson GJ. Wide Range Achievement Test. Lutz: Psychological Assessment Resources, Inc.; 2006.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Amer Geriatrics Soc. 2005;53(4):695–9. https://doi.org/10.1111/j.1532-5415.2005.53221.x.
Katz MJ, Wang C, Nester CO, Derby CA, Zimmerman ME, Lipton RB, et al. T-MoCA: A valid phone screen for cognitive impairment in diverse community samples. Alzheimers Dementia. 2021;13(1):e12144.
Smith A. Symbol digit modalities test. Los Angeles: Western Psychological Services; 1973.
Reitan RM. Trail making test: manual for administration and scoring. Tucson: Reitan Neuropsychological Laboratory; 1992.
Weintraub S, Besser L, Dodge HH, Teylan M, Ferris S, Goldstein FC, et al. Version 3 of the Alzheimer Disease Centers’ neuropsychological test battery in the Uniform Data Set (UDS). Alzheimer Dis Assoc Dis. 2018;32(1):10–7. https://doi.org/10.1097/WAD.0000000000000223.
Roth RM, Isquith PK, Gioia GA. Behavior rating inventory of executive function-adult version (BRIEF-A). Lutz: Psychological Assessment Resources, Inc.; 2005.
Lezak MD. Neuropsychological Assessment. 5th ed. New York: Oxford University Press; 2012.
Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, et al. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry. 2008;165(2):203–13. https://doi.org/10.1176/appi.ajp.2007.07010042.
Cambridge-Cognition. CANTAB Web-Based Testing. Available from: https://www.cambridgecognition.com/products/cognitive-research/web-based-testing. Accessed 10 July 2021.
Backx R, Skirrow C, Dente P, Barnett JH, Cormack FK. Comparing web-based and lab-based cognitive assessment using the Cambridge Neuropsychological Test Automated Battery: a within-subjects counterbalanced study. J Med Internet Res. 2020;22(8):e16792. https://doi.org/10.2196/16792.
Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, Fillenbaum G, et al. The Consortium to Establish a Registry for Alzheimer's Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer's disease. Neurology. 1989;39(9):1159–65. https://doi.org/10.1212/wnl.39.9.1159.
Benton AL, Abigail B, Sivan AB, Kd H, Varney NR, Spreen O. Contributions to neuropsychological assessment: a clinical manual. USA: Oxford University Press; 1994.
Pfeffer RI, Kurosaki TT, Harrah CH Jr, Chance JM, Filos S. Measurement of functional activities in older adults in the community. J Gerontol. 1982;37(3):323–9. https://doi.org/10.1093/geronj/37.3.323.
Galvin JE. The Quick Dementia Rating System (QDRS): a rapid dementia staging tool. Alzheimer's Dementia. 2015;1(2):249–59. https://doi.org/10.1016/j.dadm.2015.03.003.
Boeve BF, Molano JR, Ferman TJ, Smith GE, Lin SC, Bieniek K, et al. Validation of the Mayo Sleep Questionnaire to screen for REM sleep behavior disorder in an aging and dementia cohort. Sleep Med. 2011;12(5):445–53. https://doi.org/10.1016/j.sleep.2010.12.009.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–5. https://doi.org/10.1093/sleep/14.6.540.
Doty RL. Brief Smell Identification Test (B-SIT): Administration Manual. Haddon Heights: Sensonics, Inc.; 2001.
Kosinski M, Bayliss MS, Bjorner JB, Ware JE, Garber WH, Batenhorst A, et al. A six-item short-form survey for measuring headache impact: The HIT-6™. Quality Life Res. 2003;12(8):963–74. https://doi.org/10.1023/A:1026119331193.
Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med. 1994;23(2):129–38.
Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. The Clin J Pain. 2004;20(5):309–18. https://doi.org/10.1097/00002508-200409000-00005.
Babor TF, De La Fuente J, Saunders J, Grant M. The Alcohol Use Disorders Test: guidelines of use in primary health care. Geneva: World Health Organization; 1989.
Group WAW. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–94. https://doi.org/10.1046/j.1360-0443.2002.00185.x.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Quality Life Res. 2011;20(10):1727–36. https://doi.org/10.1007/s11136-011-9903-x.
NHANES Physical Activity and Physical Fitness Questionnaire (PAQ): Centers for Disease Control and Prevention (CDC); 2013 Available from: https://www.cdc.gov/nchs/data/nhanes/nhanes_15_16/PAQ_I.pdf.
Prevention CfDCa. NHANES Weight History Questionnaire: Centers for Disease Control and Prevention; 2013. Available from: https://www-cdc-gov.ezproxy.bu.edu/nchs/nhanes.
Moore SR, Gresham LS, Bromberg MB, Kasarkis EJ, Smith RA. A self report measure of affective lability. J Neurol Neurosurg Psychiatry. 1997;63(1):89–93. https://doi.org/10.1136/jnnp.63.1.89.
Barratt ES. Factor analysis of some psychometric measures of impulsiveness and anxiety. Psychol Rep. 1965;16(2):547–54. https://doi.org/10.2466/pr0.1965.16.2.547.
Brown GL, Goodwin FK, Ballenger JC, Goyer PF, Major LF. Aggression in humans correlates with cerebrospinal fluid amine metabolites. Psychiatry Res. 1979;1(2):131–9. https://doi.org/10.1016/0165-1781(79)90053-2.
Buss AH, Durkee A. An inventory for assessing different kinds of hostility. J Consult Psychol. 1957;21(4):343–9. https://doi.org/10.1037/h0046900.
Ismail Z, Agüera-Ortiz L, Brodaty H, Cieslak A, Cummings J, Fischer CE, et al. The Mild Behavioral Impairment Checklist (MBI-C): a rating scale for neuropsychiatric symptoms in pre-dementia populations. J Alzheimer's Dis. 2017;56(3):929–38. https://doi.org/10.3233/JAD-160979.
Kaufer DI, Cummings JL, Ketchel P, Smith V, MacMillan A, Shelley T, et al. Validation of the NPI-Q, a brief clinical form of the Neuropsychiatric Inventory. J Neuropsychiatry Clin Neurosci. 2000;12(2):233–9. https://doi.org/10.1176/jnp.12.2.233.
Spielberger CD. State-Trait Anger Expression Inventory–2 (STAXI-2). Lutz: Psychological Assessment Resources, Inc.; 1999.
Marin R, Biedrzycki R, Firinciogullari S. Reliability and validity of the Apathy Evaluation Scale. Psychiatry Res. 1991;38(2):143–62. https://doi.org/10.1016/0165-1781(91)90040-V.
Beck A. Beck Anxiety Inventory. San Antonio: Psychological Corporation, Inc.; 1993.
Beck A, Steer R, Brown G. Manual for the BDI-II. San Antonio: Psychological Corporation; 1977.
Beck A, Steer R. Manual for the Beck Hopelessness Scale. San Antonio: Psychological Corporation; 1988.
Weathers FW, Huska JA, Keane TM. PCL-C for DSM-IV. Boston: National Center for PTSD – Behavioral Science Division; 1991.
Coric V, Stock EG, Pultz J, Marcus R, Sheehan DV. Sheehan Suicidality Tracking Scale (Sheehan-STS): Preliminary Results from a Multicenter Clinical Trial in Generalized Anxiety Disorder. Psychiatry (Edgmont). 2009;6(1):26–31.
Russell D, Peplau LA, Ferguson ML. Developing a measure of loneliness. J Personality Assess. 1978;42(3):290–4. https://doi.org/10.1207/s15327752jpa4203_11.
Andronesi OC, Gagoski BA, Sorensen AG. Neurologic 3D MR spectroscopic imaging with low-power adiabatic pulses and fast spiral acquisition. Radiology. 2012;262(2):647–61. https://doi.org/10.1148/radiol.11110277.
Rowland B, L S, S J, Lin A. OpenMRSLab: an open-source software repository for magnetic resonance spectroscopy data analysis tools. Proc Int Soc Magn Reson Med. 2017;25:687-688.
Ghisays V, Goradia DD, Protas H, Bauer RJ 3rd, Devadas V, Tariot PN, et al. Brain imaging measurements of fibrillar amyloid-β burden, paired helical filament tau burden, and atrophy in cognitively unimpaired persons with two, one, and no copies of the APOE ε4 allele. Alzheimer's Dementia. 2020;16(4):598–609. https://doi.org/10.1016/j.jalz.2019.08.195.
Whittington A, Gunn R. TauIQ - a canonical image based algorithm to quantify tau PET scans. J Nucl Med. 2021 ;jnumed.120.258962. doi: 10.2967/jnumed.120.258962. Online ahead of print.
Schoemaker D, Charidimou A, Zanon Zotin MC, Raposo N, Johnson KA, Sanchez JS, et al. Association of memory impairment with concomitant tau pathology in patients with cerebral amyloid angiopathy. Neurology. 2021;96(15):e1975–86. https://doi.org/10.1212/WNL.0000000000011745.
Peskind ER. The lumbar puncture procedure (the Alzheimer's Disease Neuroimaging Initiative and the Alzheimer's Disease Cooperative Study, in collaboration with White Noise Productions); 2005.
Nieuwenhuijsen MJ. Exposure assessment in occupational & environmental epidemiology: Oxford University Press; 2003, doi: https://doi.org/10.1093/acprof:oso/9780198528616.001.0001.
Crisco JJ, Fiore R, Beckwith JG, Chu JJ, Brolinson PG, Duma S, et al. Frequency and location of head impact exposures in individual collegiate football players. J Athl Train. 2010;45(6):549–59. https://doi.org/10.4085/1062-6050-45.6.549.
Crisco JJ, Wilcox BJ, Beckwith JG, Chu JJ, Duhaime AC, Rowson S, et al. Head impact exposure in collegiate football players. J Biomech. 2011;44(15):2673–8. https://doi.org/10.1016/j.jbiomech.2011.08.003.
McAllister TW, Ford JC, Flashman LA, Maerlender A, Greenwald RM, Beckwith JG, et al. Effect of head impacts on diffusivity measures in a cohort of collegiate contact sport athletes. Neurology. 2014;82(1):63–9. https://doi.org/10.1212/01.wnl.0000438220.16190.42.
Beckwith JG, Greenwald RM, Chu JJ. Measuring head kinematics in football: correlation between the head impact telemetry system and Hybrid III headform. Ann Biomed Eng. 2012;40(1):237–48. https://doi.org/10.1007/s10439-011-0422-2.
Crisco JJ, Chu JJ, Greenwald RM. An algorithm for estimating acceleration magnitude and impact location using multiple nonorthogonal single-axis accelerometers. J Biomech Eng. 2004;126(6):849–54. https://doi.org/10.1115/1.1824135.
Duma SM, Manoogian SJ, Bussone WR, Brolinson PG, Goforth MW, Donnenwerth JJ, et al. Analysis of real-time head accelerations in collegiate football players. Clin J Sport Med. 2005;15(1):3–8. https://doi.org/10.1097/00042752-200501000-00002.
Kelley ME, Kane JM, Espeland MA, Miller LE, Powers AK, Stitzel JD, et al. Head impact exposure measured in a single youth football team during practice drills. J Neurosurg Pediatr. 2017;20(5):489–97. https://doi.org/10.3171/2017.5.PEDS16627.
Stemper BD, Shah AS, Harezlak J, Rowson S, Duma S, Mihalik JP, et al. Repetitive head impact exposure in college football following an NCAA rule change to eliminate two-a-day preseason practices: a study from the NCAA-DoD CARE Consortium. Ann Biomed Eng. 2019;47(10):2073–85. https://doi.org/10.1007/s10439-019-02335-9.
Kmush BL, Mackowski M, Ehrlich J, Walia B, Owora A, Sanders S. Association of professional football cumulative head impact index scores with all-cause mortality among National Football League players. JAMA Network Open. 2020;3(5):e204442. https://doi.org/10.1001/jamanetworkopen.2020.4442.
Alosco ML, Tripodis Y, Koerte IK, Jackson JD, Chua AS, Mariani M, et al. Interactive effects of racial identity and repetitive head impacts on cognitive function, structural MRI-derived volumetric measures, and cerebrospinal fluid tau and Aβ. Front Hum Neurosci. 2019;13:440. https://doi.org/10.3389/fnhum.2019.00440.
Alosco ML, Jarnagin J, Tripodis Y, Martin B, Chaisson C, Baugh CM, et al. Utility of providing a concussion definition in the assessment of concussion history in former NFL players. Brain Inj. 2017;31(8):1116–23. https://doi.org/10.1080/02699052.2017.1294709.
Robbins CA, Daneshvar DH, Picano JD, Gavett BE, Baugh CM, Riley DO, et al. Self-reported concussion history: impact of providing a definition of concussion. Open Access J Sports Med. 2014;5:99–104.
Corrigan J, Bogner J. Initial reliability and validity of the Ohio State University TBI identification method. J Head Trauma Rehabil. 2007;22(6):318–29. https://doi.org/10.1097/01.HTR.0000300227.67748.77.
Jack CR Jr, Albert MS, Knopman DS, McKhann GM, Sperling RA, Carrillo MC, et al. Introduction to the recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimer's Dementia. 2011;7(3):257–62. https://doi.org/10.1016/j.jalz.2011.03.004.
Diagnostic and statistical manual of mental disorders: DSM-5™, 5th ed. American Psychiatric Association D-TF, editor. Arlington: American Psychiatric Publishing, Inc.; 2013.
Jeste DV, Palmer BW, Appelbaum PS, Golshan S, Glorioso D, Dunn LB, et al. A new brief instrument for assessing decisional capacity for clinical research. Arch Gen Psychiat. 2007;64(8):966–74. https://doi.org/10.1001/archpsyc.64.8.966.
Tailby C, Collins AJ, Vaughan DN, Abbott DF, O'Shea M, Helmstaedter C, et al. Teleneuropsychology in the time of COVID-19: the experience of The Australian Epilepsy Project. Seizure. 2020;83:89–97. https://doi.org/10.1016/j.seizure.2020.10.005.
Carlew AR, Fatima H, Livingstone JR, Reese C, Lacritz L, Pendergrass C, et al. Cognitive assessment via telephone: a scoping review of instruments. Arch Clin Neuropsychol. 2020;35(8):1215–33. https://doi.org/10.1093/arclin/acaa096.
Marra DE, Hamlet KM, Bauer RM, Bowers D. Validity of teleneuropsychology for older adults in response to COVID-19: A systematic and critical review. Clin Neuropsychol. 2020;34(7-8):1411–52. https://doi.org/10.1080/13854046.2020.1769192.
Parks AC, Davis J, Spresser CD, Stroescu I, Ecklund-Johnson E. Validity of in-home teleneuropsychological testing in the wake of COVID-19. Arch Clin Neuropsychol. 2021:acab002. https://doi.org/10.1093/arclin/acab002 Online ahead of print.
Stillerova T, Liddle J, Gustafsson L, Lamont R, Silburn P. Remotely assessing symptoms of Parkinson's disease using videoconferencing: a feasibility study. Neurol Res Int. 2016;2016:4802570. https://doi.org/10.1155/2016/4802570.
Schneider RB, Myers TL, Tarolli CG, Amodeo K, Adams JL, Jensen-Roberts S, et al. Remote administration of the MDS-UPDRS in the time of COVID-19 and beyond. J Parkinson's Dis. 2020;10(4):1379–82. https://doi.org/10.3233/JPD-202121.
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–58. https://doi.org/10.1016/S0749-3797(98)00017-8.
Amariglio RE, Buckley RF, Rabin JS, Papp KV, Quiroz YT, Mormino EC, et al. Examining cognitive decline across Black and White participants in the Harvard Aging Brain Study. J Alzheimer's Dis. 2020;75(4):1437–46. https://doi.org/10.3233/JAD-191291.
Kurasz AM, Smith GE, McFarland MG, Armstrong MJ. Ethnoracial differences in Lewy body diseases with cognitive impairment. J Alzheimer's Dis. 2020;77(1):165–74. https://doi.org/10.3233/JAD-200395.
Meeker KL, Wisch JK, Hudson D, Coble D, Xiong C, Babulal GM, et al. Socioeconomic status mediates racial differences seen using the AT(N) framework. Ann Neurol. 2021;89(2):254–65. https://doi.org/10.1002/ana.25948.
Caunca MR, Odden MC, Glymour MM, Elfassy T, Kershaw KN, Sidney S, et al. Association of racial residential segregation throughout young adulthood and cognitive performance in middle-aged participants in the CARDIA Study. JAMA Neurol. 2020;77(8):1000–7. https://doi.org/10.1001/jamaneurol.2020.0860.
Avila JF, Rentería MA, Jones RN, Vonk JMJ, Turney I, Sol K, et al. Education differentially contributes to cognitive reserve across racial/ethnic groups. Alzheimer's Dementia. 2021;17(1):70–80. https://doi.org/10.1002/alz.12176.
Ioannidis JPA, Powe NR, Yancy C. Recalibrating the use of race in medical research. JAMA. 2021;325(7):623–4. https://doi.org/10.1001/jama.2021.0003.
Acknowledgements
We thank Debra Babcock, M.D., Ph.D., Scientific Program Official of this U01 grant at NINDS, for her support, guidance, and advice. We also thank our External Advisory Board (David Knopman, M.D., [Chair], Col. [Ret.] Dallas Hack, M.D., Mike Haynes, Brian Hainline, M.D., Thomas McAllister, M.D., Arthur Toga, Ph.D., and Michael Weiner, M.D.) for sharing their time, effort, and expertise. Finally, we thank all of our participants and their study partners for making this study possible and for their tremendous contribution to our understanding of chronic traumatic encephalopathy and other long-term consequences of repetitive head impacts.
The DIAGNOSE CTE Research Project Current and Former Investigators and Key Personnel
Banner Alzheimer’s Institute
Investigators
Eric Reiman, M.D. (Co-PI)
Yi Su, Ph.D.
Kewei Chen, Ph.D.
Hillary Protas, Ph.D.
Non-Investigators
Connie Boker, M.B.A. (Director, Imaging Center Operations)
Boston University School of Medicine
Investigators
Michael L. Alosco, Ph.D.
Rhoda Au, Ph.D.
Robert C. Cantu, Ph.D.
Lindsay Farrer, Ph.D.
Robert Helm, M.D. *
Douglas I. Katz, M.D.
Neil Kowall, M.D. *
Ann C. McKee, M.D.
Jesse Mez, M.D.
Gustavo Mercier, M.D., Ph.D. *
James Otis, M.D. *
Robert A. Stern, Ph.D. (Co-PI)
Jason Weller, M.D.
Non-Investigators
Irene Simkin, M.S. (Lab Manager, Molecular Genetics Core Facility)
Boston University Project Coordinating Center Staff
Alondra Andino, B.A. (Project Administrative Manager) *
Shannon Conneely, B.A. (Site Coordinator) *
Courtney Diamond, M.B.A. (Project Manager) *
Tessa Fagle, B.A. (Research Assistant)
Olivia Haller, B.A. (Recruitment Coordinator) *
Tennyson Hunt, M.B.A. (Project Administrative Manager) *
Nicole Gullotti, M.B.A. (Research Administrator) *
Megan Mariani, B.S., B.A. (Project Manager)
Brian Mayville, B.S. (Site Coordinator)
Kathleen McLaughlin, B.A. (Research Assistant)
Mary Nanna, B.A. (Retention Coordinator)
Taylor Platt, M.P.H. (Recruitment Coordinator) *
Surya Pulukuri, B.A. (Research Assistant)
Fiona Rice, M.P.H. (Project Manager) *
Madison Sestak, B.S. (Assistant Recruitment Coordinator) *
Boston University School of Public Health
Investigators
Michael McClean, Sc.D.
Yorghos Tripodis, Ph.D.
Data Team Staff
Douglas Annis, M.S. (Systems Analyst) *
Christine Chaisson, M.P.H. (Leader of Data Management Sub-team) *
Diane B. Dixon (Project Manager)
Carolyn Finney, B.A. (Data Manager)
Kerrin Gallagher, M.P.H. (Statistical Analyst) *
Kaitlin Hartlage, M.P.H. (Statistical Analyst)
Jun Lu, M.S. (Data Security and Technology Analyst)
Brett Martin, M.S. (Statistical Manager)
Emmanuel Ojo, M.P.H. (Statistical Analyst) *
Joseph N. Palmisano, M.A., M.P.H. (Leader of Data Management Sub-team)
Brittany Pine, B.A., B.S. (Statistical Analyst)
Janani Ramachandran, M.S. (Data Manager)
Brigham and Women’s Hospital
Investigators
Sylvain Bouix, Ph.D.
Jennifer Fitzsimmons, M.D. *
Alexander P. Lin, Ph.D.
Inga K. Koerte, M.D., Ph.D.
Ofer Pasternak, Ph.D.
Martha E. Shenton, Ph.D. (Co-PI)
Non-Investigators
Hector Arciniega, Ph.D. (Postdoctoral Research Fellow)
Tashrif Billah, M.S. (Software Engineer)
Elena M. Bonke, M.S. (Ph.D. Student)
Katherine Breedlove, Ph.D. (Postdoctoral Research Fellow)
Eduardo Coello, Ph.D. (Postdoctoral Research Fellow)
Michael J. Coleman, M.A. (Senior Scientist)
Leonard B. Jung, (Ph.D. Student)
Huijun Liao, B.S. (Study Coordinator)
Maria Loy, M.B.A., M.P.H. (Senior Program Coordinator)
Elizabeth Rizzoni, B.A. (Research Assistant)
Vivian Schultz, M.D. (Postdoctoral Research Fellow)
Annelise Silva, B.S. (Research Assistant) *
Brynn Vessey, B.S. (Research Assistant)
Tim L.T. Wiegand, (Ph.D. Student)
Cleveland Clinic Lou Ruvo Center for Brain Health
Investigators
Sarah Banks, Ph.D. (Now at University of California, San Diego)
Charles Bernick, M.D. (Now at University of Washington)
Jason Miller, Ph.D.
Aaron Ritter, M.D.
Marwan Sabbagh, M.D. *
Non-Investigators
Raelynn de la Cruz, (Psychometrician)*
Jan Durant, (Psychometrician)*
Morgan Golceker (Site Coordinator)
Nicolette Harmon, (Site Coordinator) *
Kaeson Kaylegian, (Psychometrician)*
Rachelle Long, (Site Coordinator) *
Christin Nance, (Psychometrician)*
Priscilla Sandoval (Site Coordinator) *
George Washington University School of Medicine and Health Sciences
Investigator
Robert W. Turner, Ph.D.
Invicro (formerly Molecular NeuroImaging)
Investigator
Kenneth L. Marek, M.D.
Non-Investigator
Andrew Serrano, M.B.A.
Mayo Clinic Arizona
Investigators
Charles H. Adler, M.D., Ph.D.,
David W. Dodick, M.D.
Yonas Geda, M.D., MSc (Now at Barrow Neurological Institute)
Jennifer V. Wethe, Ph.D.
Non-Investigators
Bryce Falk, R.N.
Amy Duffy, (Site Coordinator) *
Marci Howard, (Psychometrician)*
Michelle Montague, (Psychometrician)*
Thomas Osgood, (Site Coordinator)
National Institute of Neurological Disorders and Stroke (NINDS)
Debra Babcock, M.D., Ph.D. (Scientific Program Official)
Patrick Bellgowan, Ph.D. (Administrative Program Official)*
New York University:
Investigators
Laura Balcer, M.D., M.S.C.E.
William Barr, PhD.
Judith Goldberg, Sc.D.
Thomas Wisniewski, M.D. *
Ivan Kirov, Ph.D.
Yvonne Lui, M.D.
Charles Marmar, M.D.
Non-Investigators
Lisena Hasanaj (Site Coordinator)
Liliana Serrano
Alhassan Al-Kharafi (Psychometrician)*
Allan George (Psychometrician)*
Sammie Martin (Psychometrician)*
Edward Riley (Psychometrician)*
William Runge (Psychometrician)*
University of Nevada, Las Vegas
Jeffrey L. Cummings, M.D., ScD (Co-PI)
University of Washington and VA Puget Sound
Investigator
Elaine R. Peskind, M.D.
Non-Investigator
Elizabeth Colasurdo (Lab Manager)
Washington University (CNDA)
Investigators
Daniel S. Marcus, Ph.D.
Non-Investigator
Jenny Gurney, M.S.
Consultants
Richard Greenwald, Ph.D. (Simbex)*
Keith A. Johnson, M.D. (Massachusetts General Hospital)
*No longer involved in project.
Funding
This work was supported by grants from the National Institutes of Health (U01NS093334; P30AG13846; R01NS078337; K23NS102399; P30AG019610; K01AG054762; R01NS100952; K00NS113419). This publication was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through BU-CTSI Grant Number 1UL1TR001430. The primary funding source is the National Institute of Neurological Disorders and Stroke (NINDS), through a U01 Research Project Cooperative Agreement (U01NS093334).
Author information
Authors and Affiliations
Consortia
Contributions
MLA and RAS drafted the manuscript. RAS, JLC, EMR, and MES designed and oversaw the study. MLM provided additional drafting of the manuscript and served as project manager of the study. CHA, LJB, CB, and RAS were PIs of the baseline performance evaluation sites and oversaw data and sample collection. RA and MDM oversaw risk assessment aspects of the study, with JM and LAF contributing to the genetics sections and RWT providing additional contributions to sociodemographic data issues. MES, SB, MJC, IK, APL, and DSM designed and implemented the MRI and MRS data collection and analytics. EMR and KLM designed and oversaw the PET data collection and analytics. MLA, SJB, WBB, JVW, and RAS designed and implemented the neuropsychological battery and data collection. DIK, CB, DWD, JM, and RAS designed and implemented the consensus diagnostic conferences. CHA and RCC designed the neurological and motor assessments. JLC, YEG, and RAS designed the neuropsychiatric assessments. EP designed and oversaw fluid biomarker collection and planned analyses. ACM provided input regarding the neuropathology of CTE and NWK provided additional input regarding underlying mechanisms. JNP oversaw data management systems. YT oversaw biostatistical and data analytic plans. All authors critically reviewed and revised the manuscript and approved its content before submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All Participant Evaluation Sites have received approval by their respective Institutional Review Boards. All participants provide written informed consent during their baseline and follow-up study visits.
○ Boston University Medical Campus Institutional Review Board, #H-34799
○ Cleveland Clinic Institutional Review Board, #16-1694
○ Mayo Clinic Institutional Review Boards, #16-002662
○ NYU School of Medicine Institutional Review Board, #i16-01032 CR3
○ Partners Human Research Institutional Review Board, #2016P001359 and #2016P001328
○ Western Copernicus Group (WCG) Institutional Review Board (Banner Alzheimer’s Institute), #1168489
Consent for publication
Not applicable.
Competing interests
MLA: None to report.
MLM: None to report.
CHA: None to report.
LJB is Editor-in-Chief of the Journal of Neuro-Ophthalmology, and is a paid consultant to Biogen (Cambridge, MA, USA).
CB receives research support from the Ultimate Fighting Championship, Top Rank promotions, Haymon Boxing, Las Vegas Raiders, and Professional Bull Riders. He is a paid consultant for Aurora Concussion Therapy Systems, Inc. (St. Paul, MN).
RA is a paid consultant to Biogen (Cambridge, MA, USA) and serves on the Scientific Advisory Board of Signant Health (Blue Bell, PA).
SJB: None to report.
WBB provides expert witness testimony in legal cases involving concussion and CTE.
SB: None to report.
RCC is a Senior Advisor to the NFL Head Neck & Spine Committee; Vice President, National Operating Committee on Standards for Athletic Equipment; and Chair, Scientific Advisory Committee, Co-Founder, and Medical Director, Concussion Legacy Foundation. He is a member of the Medical Science Committee for the National Collegiate Athletic Association Student-Athlete Concussion Injury Litigation, and he receives royalties for published books from Houghton Mifflin Harcourt.
MJC: None to report.
DWD reports the following competing interests: Consulting: AEON, Amgen, Clexio, Cerecin, Cooltech, Ctrl M, Allergan, Alder, Biohaven, GSK, Linpharma, Lundbeck, Promius, Eli Lilly, eNeura, Novartis, Impel, Satsuma, Theranica, WL Gore, Nocira, XoC, Zosano, Upjohn (Division of Pfizer), Pieris, Praxis, Revance, Equinox. Honoraria: Clinical Care Solutions, CME Outfitters, Curry Rockefeller Group, DeepBench, Global Access Meetings, KLJ Associates, Academy for Continued Healthcare Learning, Majallin LLC, Medlogix Communications, MJH Lifesciences, Miller Medical Communications, Southern Headache Society (MAHEC), WebMD Health/Medscape, Wolters Kluwer, Oxford University Press, Cambridge University Press. Research Support: Department of Defense, National Institutes of Health, Henry Jackson Foundation, Sperling Foundation, American Migraine Foundation, Patient Centered Outcomes Research Institute (PCORI). Stock Options/Shareholder/Patents/Board of Directors: Ctrl M (options), Aural analytics (options), ExSano (options), Palion (options), Healint (Options), Theranica (Options), Second Opinion/Mobile Health (Options), Epien (Options/Board), Nocira (options), Matterhorn (Shares/Board), Ontologics (Shares/Board), King-Devick Technologies (Options/Board), Precon Health (Options/Board). Patent 17189376.1-1466:vTitle: Botulinum Toxin Dosage Regimen for Chronic Migraine Prophylaxis.
LAF: None to report.
YEG has received research funding from Roche Inc and has been a paid consultant for Lundbeck.
DIK receives royalties from Springer/Demos Publishing for a text book on brain injury, serves as expert witness in legal cases involving brain injury and concussion, receives a stipend from Encompass Health as program medical director for brain injury and chair of the annual Neurorehabilitation conference; and has received honoraria for a keynote address for the HealthSouth annual Medical Directors meeting and some grand rounds lectures involving TBI.
IKK: None to report.
NWK: None to report.
APL is a paid consultant to Agios Pharmaceuticals (Cambridge, MA, USA), Biomarin Pharmaceuticals (Novato, CA, USA), and Moncton MRI (Moncton, Canada). He is the co-founder of BrainSpec, Inc.
DSM has an equity interest in Radiologics, Inc., White Rabbit, Inc., and Sora Neuroscience, LLC.
KLM is a consultant for the Michael J Fox Foundation, GE Healthcare, Roche, UCB, Lysosomal Therapeutic, Inc, Denali, Takeda, Samumed, Cerapsir, HANDL, Biohaven, Neuron23, Aprinoia, Hemacure, Genentech, and Invicro,
MDM: None to report.
ACM: None to report.
JM: None to report.
JNP: None to report.
EP: None to report.
YT: None to report.
RWT: None to report.
JVW: None to report.
JLC has provided consultation to Acadia, Alkahest, AriBio, Avanir, Axsome, Behren Therapeutics, Biogen, Cassava, Cerecin, Cerevel, Cortexyme, EIP Pharma, Eisai, GemVax, Genentech, Green Valley, Grifols, Janssen, Jazz, Karuna, Merck, Novo Nordisk, Otsuka, ReMYND, Resverlogix, Roche, Samumed, Samus, Signant Health, Sunovion, Suven, United Neuroscience, and Unlearn AI pharmaceutical and assessment companies. He owns the copyright of the Neuropsychiatric Inventory.
EMR is a compensated scientific advisor for Alkahest, Alzheon, Aural Analytics, Denali, Green Valley, Retromer Therapeutics, and Vaxxinity, and a co-founder of ALZPath.
MES: None to report.
RAS is a paid consultant to Biogen (Cambridge, MA, USA). He is a member of the Board of Directors of King-Devick Technologies, Inc. (Chicago, IL, USA), and he receives royalties for published neuropsychological tests from Psychological Assessment Resources, Inc. (Lutz, FL, USA). He is a member of the Medical Science Committee for the National Collegiate Athletic Association Student-Athlete Concussion Injury Litigation.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alosco, M.L., Mariani, M.L., Adler, C.H. et al. Developing methods to detect and diagnose chronic traumatic encephalopathy during life: rationale, design, and methodology for the DIAGNOSE CTE Research Project. Alz Res Therapy 13, 136 (2021). https://doi.org/10.1186/s13195-021-00872-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-021-00872-x
Keywords
- Neurodegenerative disease
- Biomarkers
- Chronic traumatic encephalopathy
- Cognitive function
- Concussion
- Football
- Head trauma
- MRI
- MRS
- National Football League
- College football
- Neuroimaging
- Repetitive head impacts
- Traumatic brain injury
- Subconcussion
- Traumatic encephalopathy syndrome
- Positron emission tomography
- Tau
- Remote assessment