Abstract
Background
Cerebrovascular disease (CVD) and amyloid-β (Aβ) often coexist, but their influence on neurodegeneration and cognition in predementia stages remains unclear. We investigated the association between CVD and Aβ on neurodegenerative markers and cognition in patients without dementia.
Methods
We included 271 memory clinic patients with subjective or objective cognitive deficits but without dementia from the BioBank Alzheimer Center Limburg cohort (n = 99) and the LeARN (n = 50) and DESCRIPA (n = 122) multicenter studies. CSF Aβ1–42 and white matter hyperintensities (WMH) on magnetic resonance imaging (MRI) scans were used as measures of Aβ and CVD, respectively. Individuals were classified into four groups based on the presence (+) or absence (−) of Aβ and WMH. We investigated differences in phosphorylated tau, total tau (t-tau), and medial temporal lobe atrophy (MTA) between groups using general linear models. We examined cognitive decline and progression to dementia using linear mixed models and Cox proportional hazards models. All analyses were adjusted for study and demographics.
Results
MTA and t-tau were elevated in the Aβ − WMH+, Aβ + WMH−, and Aβ + WMH+ groups. MTA was most severe in the Aβ + WMH+ group compared with the groups with a single pathology. Both WMH and Aβ were associated with cognitive decline, but having both pathologies simultaneously was not associated with faster decline.
Conclusions
In the present study, we found an additive association of Aβ and CVD pathology with baseline MTA but not with cognitive decline. Because our findings may have implications for diagnosis and prognosis of memory clinic patients and for future scientific research, they should be validated in a larger sample with longer follow-up.
Similar content being viewed by others
Background
Cerebrovascular disease (CVD) often coexists with Alzheimer’s disease (AD), and both conditions add to cognitive decline [1, 2]. The influence of coexisting CVD and AD pathology on neurodegeneration and cognitive decline in predementia stages of AD, however, remains uncertain. Understanding the role CVD pathology in early AD is key to understanding and preventing cognitive decline in AD.
In subjects with dementia, coexistent AD and CVD pathology at autopsy is associated with more rapid cognitive decline and often a more severe form of dementia than isolated AD pathology [3, 4]. A combination of AD and CVD has also been associated with a lower burden of amyloid-β (Aβ) pathology than in isolated AD [5, 6], suggesting that less AD pathology is needed for cognitive impairment in individuals who also have CVD [7, 8]. In cognitively normal subjects, it was shown that Aβ and CVD pathology are independent contributors to cognitive decline and that both increase the risk of dementia [7, 9]. Studies on the contribution of Aβ and CVD pathology on cognitive decline in individuals with subjective cognitive decline (SCD) and mild cognitive impairment (MCI) have shown conflicting results [10, 11]. Also, how each of these pathologies relates to different markers of neurodegeneration is less well understood, because previous studies point in different directions or were focused on only a single marker instead of investigating multiple neurodegenerative markers using various modalities (e.g., magnetic resonance imaging (MRI) and cerebrospinal fluid CSF)) [12,13,14,15]. Clarity regarding the relationship between coexisting AD and CVD pathology, neurodegenerative markers, and cognition will improve diagnostic and prognostic accuracy of early AD.
The aim of this study was to investigate whether in patients with SCD and MCI there is an additive effect of CVD and Aβ on neurodegeneration measured by total tau (t-tau) and phosphorylated tau (p-tau) in CSF and medial temporal lobe atrophy (MTA) visualized by MRI, as well as on cognitive decline during follow-up.
Methods
Subjects
Two hundred seventy-one subjects were selected from memory clinics of the single-center BioBank Alzheimer Center Limburg (BBACL; n = 99) cohort and the LeARN (n = 50) [16] and DESCRIPA (Development of screening guidelines and criteria for predementia Alzheimer’s disease; n = 122) [17] multicenter studies. Inclusion criteria were (1) no diagnosis of dementia at baseline and (2) baseline data available for MRI and CSF measures. When subjects participated in more than one study, we included the data from the study with the longest follow-up. The medical ethics committee at each site approved the study. All subjects provided informed consent.
Clinical assessment
Clinical assessment included neuropsychological assessment and an assessment of medical history. Information on medical history (e.g., hypertension, diabetes, obesity) was provided by patients and/or their caregivers, or it was extracted from medical files. Neuropsychological assessment was performed according to local routine protocol of each site, including the Mini Mental State Examination (MMSE) and at least one test in the cognitive domains of memory and executive functioning. The delayed recall of a word list test was used to examine memory. For the BBACL and LeARN studies, the Rey Auditory Verbal Learning Test (RAVLT) was used [18]. For the DESCRIPA cohort, the RAVLT and Consortium to Establish a Registry for Alzheimer’s Disease word list were the primary memory tests used. DESCRIPA tests per center are described elsewhere [17]. The Trail Making Test part B (TMT-B) [19] was used to examine executive functioning. Raw scores on each test were converted to z-scores using local normative data. Z-scores below −5 (n = 7) were rounded to −5 to avoid bias through outliers in the data.
Diagnosis of MCI at baseline was made according to the criteria of Petersen [20]. Subjects with a z-score below −1.5 on the immediate recall or delayed recall of a word list test were classified as having amnestic MCI. Subjects with a z-score below −1.5 on any of the nonmemory tests were classified as nonamnestic MCI. Diagnosis of AD-type dementia at follow-up was made according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition [21], and the National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer’s Disease and Related Disorders Association [22]. Etiological diagnoses of other types of dementia were made according to standardized clinical criteria for vascular dementia [23], frontotemporal dementia (FTD) [24], and dementia with Lewy bodies [25].
CSF analyses
CSF was collected by lumbar puncture and thereafter centrifuged and stored at −80 °C in polypropylene tubes. CSF Aβ1–42, t-tau, and p-tau were analyzed using the Innotest sandwich enzyme-linked immunosorbent assay (Innogenetics, Ghent, Belgium) in Gothenburg for the DESCRIPA cohort [17], in Amsterdam for the LeARN project [26], and in Nijmegen for the BBACL study [27]. To define abnormality of the CSF measures, the following predefined cutoffs were used: Aβ1–42 ≤ 550 pg/ml, t-tau > 375 pg/ml, and p-tau181 > 52 pg/ml [28].
Genetic analyses
The apolipoprotein E (APOE) genotype was determined in a subgroup of the sample (n = 165). Assessments were performed according to routine protocol at each site, as described elsewhere [17, 29].
MRI analyses
All subjects were scanned according to the routine MRI protocol at each site (Additional file 1). Scanning was performed at 1.0 (n = 14), 1.5 (n = 108), or 3.0 (n = 149) Tesla, and all scans included a three-dimensional T1-weighted gradient echo sequence and a fast fluid-attenuated inversion recovery sequence. To determine MTA, the Scheltens MTA visual rating scale [30] was used. The score on the MTA scale ranges from 0 to 4 for each hemisphere. The summed score of both hemispheres was used, where an abnormal MTA was defined using a cutoff ≥ 2 [31]. White matter hyperintensities (WMH) were measured with the visually rated age-related white matter changes (ARWMC) scale (range 0–3) [32] for the DESCRIPA cohort and with the visually rated Fazekas scale (range 0–3) [33] for the BBACL and LeARN cohorts. For the ARWMC scale, a cutoff score ≥ 2 in at least one of the measured brain areas was used to define WMH status [34, 35]. For the Fazekas scale, a cutoff score ≥ 2 was also used to define WMH status [36].
Subject classification
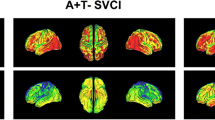
To classify individuals into subgroups, we used Aβ as a measure of AD and WMH as a measure of CVD. Subjects were classified as Aβ + when CSF Aβ1–42 levels were abnormal. Subjects were classified as WMH+ when the WMH score was high. We created four groups based on combinations of Aβ status and WMH status: Aβ − WMH−, Aβ − WMH+, Aβ + WMH−, and Aβ + WMH+.
Statistical analyses
We analyzed differences in clinical baseline and follow-up characteristics and neurodegeneration markers between groups using analysis of variance for continuous variables and chi-square tests for categorical variables. Prior to the continuous comparisons of biomarker values between groups (Tables 1 and 2), Aβ1–42, p-tau, and t-tau values were log-transformed to approximate a normalized distribution required for statistical comparisons. The raw biomarker values are shown in the tables. Comparisons between Aβ/WMH groups regarding neurodegenerative markers (Table 2) were all corrected for demographics, study, and baseline diagnosis.
The associations between Aβ/WMH groups and changes in MMSE scores, memory, and executive functioning were assessed by slope analyses with linear mixed models. The analyses included the baseline scores and all available follow-up scores (up to 4 years). All slope analyses were adjusted for study. When the interaction between Aβ/WMH group, baseline diagnosis, and time was significant, we added baseline diagnosis as a covariate in the model. The models adjusted for baseline diagnoses are reported in the tables and figures, and the results stratified by diagnoses are reported in the text. For the MMSE, we also adjusted for age, sex, and years of education because these scores are not standardized. We also tested the influence of APOE genotype in a subgroup of the sample for whom this was available. Models were fitted with random study-specific intercept and subject-specific slopes and a first-order autoregressive correlation structure. We chose this model because it provided the best −2 log-likelihood ratio and the lowest number of parameters. Cox proportional hazards models were used to investigate the risk of progression to dementia for each group after adjusting for demographics, study, and baseline diagnosis. Statistical analyses were conducted with IBM SPSS Statistics version 24.0 software (IBM, Armonk, NY, USA) with the significance level set at p < 0.05. Owing to the exploratory nature of the study, we did not control for multiple comparisons. Post hoc power calculations were conducted using IBM SPSS Statistics software and the ‘simr’ package of R statistical software (version 3.3.3; R Foundation for Statistical Computing, Vienna, Austria).
Results
Cohort characteristics
We included 271 individuals with a mean age of 65.6 (SD 9.0) years. One hundred sixty-five (61%) were female, and 153 (57%) had a diagnosis of MCI at baseline, of whom 99 (65%) were classified as having amnestic MCI. Follow-up data were available for 233 individuals (86%). The availability of follow-up data was not different among the Aβ/WMH groups (p = 0.396) or studies (p = 0.730). After a mean follow-up of 2.5 (SD 1.2) years, 46 (17%) subjects had progressed to dementia. The majority (80%) of the individuals who progressed to dementia had a clinical diagnosis of AD-type dementia.
Table 1 shows baseline and follow-up characteristics of the four Aβ/WMH groups. The group without pathology was younger (p < 0.001) and progressed less frequently to dementia than the other three groups (p < 0.001). We found no difference in the prevalence of several vascular risk factors between the four groups (hypertension, p = 0.563; obesity, p = 0.486; diabetes, p = 0.106). We found no difference in Aβ load between the group with only Aβ and the group with both Aβ and WMH pathologies (p = 0.502). Likewise, the proportion of WMH was not different between the two WMH+ groups (Aβ − WMH+ and Aβ + WMH+; p = 0.175).
Neurodegeneration markers
Table 2 shows the values and frequency of abnormal neurodegenerative markers for the Aβ/WMH groups. We found that, compared with the group without pathology, MTA was more severe in the groups with only Aβ (p < 0.001) and with only WMH (p < 0.001), as well as in the mixed pathology group (p < 0.001). The Aβ + WMH+ group had higher MTA scores than the group with only WMH (p = 0.025) and the group with only Aβ (p = 0.002). t-tau was increased in all three groups with a form of pathology compared with the group without pathology (Aβ − WMH+, p < 0.001; Aβ + WMH−, p < 0.001; Aβ + WMH+, p = 0.047), but this effect was influenced by baseline diagnosis (Aβ/WMH group × baseline diagnosis, F = 3.20, p = 0.024). When stratified by diagnosis, the effect was found only in subjects with MCI. There was no difference in t-tau levels between the Aβ − WMH+, Aβ + WMH−, and Aβ + WMH+ groups, regardless of baseline diagnosis. p-tau was increased only in the group with only Aβ compared with the Aβ − WMH− group (p < 0.001), regardless of baseline diagnosis. The association between p-tau and Aβ/WMH group was influenced by APOE genotype because we found that the elevated p-tau levels in the Aβ + WMH− group were limited to APOE ε4 allele carriers (Aβ/WMH group × APOE status, F = 3.72, p = 0.013).
Baseline cognitive performance and cognitive decline
In the total sample, MMSE scores did not differ between the Aβ/WMH groups at baseline (Table 3, Fig. 1). Baseline MMSE scores of the individuals with MCI were lower than those of individuals with SCD, regardless of pathology (p < 0.001). In subjects with MCI, there was a difference in baseline MMSE score only between the Aβ − WMH− and the Aβ + WMH− groups (p = 0.020). In subjects with SCD, there was no difference in baseline MMSE scores. In the total sample, the groups with one or both pathologies declined in MMSE score over time (Aβ − WMH+, p = 0.014; Aβ + WMH−, p = 0.035; Aβ + WMH+, p = 0.045), whereas scores remained stable in the Aβ − WMH− group (p = 0.793). The rate of decline was higher in the Aβ − WMH+ group than in the Aβ − WMH− group (p = 0.035). There were no differences in the rate of decline between the three groups with pathology. In subjects with SCD, the Aβ/WMH groups showed no decline over time. In subjects with MCI, the results were similar to those found in the total sample. Baseline delayed recall memory scores were lower in the three groups with pathology than in the group without pathology (Aβ − WMH+, p = 0.004; Aβ + WMH−, p < 0.001; Aβ + WMH+, p = 0.009), which was not influenced by baseline diagnosis. None of the groups showed significant decline over time. TMT-B scores did not differ at baseline between the groups and did not change during follow-up (Table 3, Fig. 1). APOE genotype did not influence any of the baseline or longitudinal associations.
Cognitive decline by amyloid-β/white matter hyperintensities (Aβ/WMH) group for global cognition, memory, and executive functioning. The graphs show mean scores and 95% CIs of cognitive decline over time for four different groups based on Aβ/WMH status. The left graph shows cognitive decline for global cognition (Mini Mental State Examination [MMSE]) after adjusting for demographics, study, and baseline diagnosis. The middle graph shows cognitive decline for memory (delayed recall of Rey Auditory Verbal Learning Test) after adjusting for study. The right graph shows cognitive decline for executive functioning (Trail Making Test part B) after adjusting for study
Progression to dementia
Table 4 and Fig. 2 show the risk of progression to dementia for the Aβ/WMH groups. Compared with the group without pathology, the groups with a form of pathology have an increased risk of progressing to dementia (Aβ- WMH+ HR: 3.25, p = 0.021, Aβ + WMH- HR: 4.89, p < 0.001, Aβ + WMH+ HR:3.00, p = 0.036), but this was influenced by baseline diagnosis (Aβ/WMH group*baseline diagnosis: HR = 2.89; p = 0.007) as the effect was mainly attributable to MCI subjects (Fig. 2). There was no difference in progression rates between the groups with isolated or coexisting Aβ/WMH pathology, when analyzing the total sample or only MCI subjects. Results were similar when using progression to AD-type dementia as outcome.
Risk of progression to dementia over time for amyloid-β/white matter hyperintensities (Aβ/WMH) groups, by baseline diagnosis. The graph shows the probability of surviving without dementia during a 4-year follow-up period for the four Aβ/WMH groups after adjusting for demographics and study, stratified by baseline diagnosis. MCI Mild cognitive impairment, SCD Subjective cognitive decline
Post hoc analyses
Because both Aβ and WMH were associated with MTA, we tested the interaction between the two pathologies on MTA. General linear model analyses showed no interaction between Aβ and WMH on MTA, using dichotomous variables created with cutoff points (p = 0.770) or continuous variables (p = 0.631).
We repeated the main analyses after exclusion of subjects with CSF Aβ1–42 values 10% around the cutoff. The results remained similar after this exclusion. The results were also comparable after exclusion of the four subjects in the Aβ − WMH− group who progressed to FTD at follow-up, as well as when repeating the analyses using Aβ and tau for classification of AD profiles instead of only Aβ.
We conducted age sensitivity analyses in which we age-matched the Aβ/WMH groups by selecting only individuals between 64 and 79 years of age. Most results were similar to the original results. Results that were different are shown in Additional file 2. Associations that showed a similar direction but no longer reached significance because of a reduction in sample size (p values between 0.05 and 0.09) were considered unchanged.
Observed power calculations were done for the main analyses. For the comparisons of neurodegenerative markers (Table 2), the observed power ranged from 0.71 to 0.99. For the comparisons of cognitive performance and decline (Table 3), the observed baseline power ranged from 0.37 to 0.67, and for the slopes it ranged from 0.34 to 0.61. Regarding the comparisons in progression to dementia (Table 4), the observed power was 0.66.
Discussion
We investigated the relation of Aβ and CVD pathology with markers of neurodegeneration and cognitive decline. We found that the neurodegeneration markers t-tau in CSF and MTA on MRI scans were associated with both Aβ and CVD, as well as that there was an additive association of the two pathologies on MTA. Decline of global cognition scores during follow-up was seen in both Aβ and CVD, but there was no additive or synergistic effect.
Medial temporal lobe atrophy
The association between AD pathology and MTA has been well characterized in the literature. The first neuropathological changes underlying AD are thought to occur in the medial temporal lobe [37]. The relationship between MTA and CVD, however, is still somewhat controversial. Some studies have found that CVD was associated with MTA [12, 15, 38], whereas others did not find this relationship [7, 13]. Our results support an association between CVD and MTA, although we measured only one aspect of CVD (i.e., WMH). Interestingly, we found that MTA was most severe in the group with mixed Aβ/WMH pathology compared with the groups with a single form of pathology. In post hoc analyses, we found no interaction between Aβ and WMH on MTA, and therefore we conclude that WMH and Aβ are independent determinants of MTA severity and that when both are present, their effects are additive.
Tau
Increased CSF t-tau was associated with both WMH and Aβ pathology, which is consistent with previous studies where t-tau was considered a measure of neuronal damage [14, 39]. Our finding that t-tau levels were also elevated in patients with WMH and no Aβ pathology contradicts a previous study in which researchers concluded that elevated t-tau levels in patients with vascular damage could be the result of coexisting Aβ pathology [40]. That elevated t-tau levels in the groups with one or both pathologies were found only in subjects with MCI is in line with previous work that strongly related tau to cognitive dysfunction [41]. p-tau was significantly increased only in the Aβ + WMH− group and only slightly increased in the Aβ + WMH+ group, supporting the hypothesis that this could be a specific biomarker for AD [39].
Amyloid-β
We found similar levels of Aβ for the group with only amyloid pathology and the group with mixed Aβ/WMH pathology. This was in contrast to our expectations based on the literature, because we expected the group with mixed pathology to have a lower amyloid load (i.e., higher Aβ1–42 levels) [5, 6]. Possibly, the cognitive status of the investigated population (i.e., individuals with SCD or MCI vs. cognitively normal individuals) might play a role, in particular in combination with the method of measuring amyloid load (by CSF or amyloid positron emission tomography), because a study comparing these two methods showed that discordance was dependent on disease stage [42]. Further studies should be done to determine the associations of both factors with amyloid load in mixed AD/CVD patients. The suggestion of expanding the recently proposed “A/T/N” classification system with a vascular component would be valuable in addressing these and other research questions [43].
Cognitive performance and decline
The decrease in performance in global cognition over time was similar for the three groups with pathology, indicating that WMH and Aβ pathology are drivers of cognitive decline. This is in line with findings derived from a previous study of cognitively normal individuals in which investigators also found that both pathologies contribute to cognitive decline [9]. However, in contrast to this previous study, we did not find any differences in cognitive trajectories between individuals with only Aβ pathology and those with mixed Aβ/WMH pathology. This may relate to the fact that we included subjects with SCD and MCI instead of cognitively normal subjects or to the type of cognitive measures used. Also, risk of progression to dementia during follow-up did not differ between WMH and Aβ, and having both pathologies simultaneously did not increase the risk any further.
Strengths and limitations
This study has several limitations. First, using WMH as a marker of CVD can be seen as a limitation because we did not take other forms of CVD such as lacunar infarcts or cortical microbleeds into account. Although using only WMH reflects a method of defining vascular damage frequently used in clinical practice [44], this makes our findings less generalizable to CVD in general. Also, WMH are heterogeneous in their etiology and pathophysiology, and the underlying mechanisms causing WMH are not yet completely understood [45]. However, in an aging population such as we used in the present study, WMH are mostly considered a consequence of cerebral vascular damage [46, 47]. Second, our follow-up length ranged from 1 to 4 years, which might have been too short to detect differences in cognitive decline in nondemented individuals. Third, our sample was derived from different studies, which might have led to variability in the data, despite adjustment for study in all of the analyses. However, our multistudy design makes our findings more generalizable to other memory clinic settings. Fourth, a methodological consideration of this study was that our results were based on both subjects with SCD and subjects with MCI. Although we did examine the influence of the baseline diagnosis in all analyses and when needed adjusted for this and reported the differences, the smaller sample sizes when analyzing per diagnosis could have influenced the results. The smaller sample sizes in general could reflect a lack of statistical power, and therefore our results should be interpreted with caution and validated in future studies. Although observed power calculations should be interpreted with caution [48], we recommend that researchers in future studies make group sizes more balanced and include a larger number of complete follow-up visits, in particular for outcome measures with smaller effect sizes (e.g., executive functioning measures). The major strengths of this study were the longitudinal setup, the reflection of clinical practice, and the availability of different neurodegeneration markers to provide novel insights into the role of neurodegeneration in relation to AD and CVD.
Conclusions
The findings of the present study may have implications for the diagnosis and prognosis of memory clinic patients but also for future scientific research. For clinicians, it is important to realize that MTA on MRI and elevated t-tau values in CSF may reflect underlying AD as well as CVD pathology, and that the effects of Aβ and WMH on MTA could be additive. On the basis of data derived from the present study, we conclude that the short-term cognitive prognosis of patients with SCD or patients with MCI with mixed amyloid/WMH pathology may be similar to that of patients with solely Aβ or WMH pathology. Future research with longer follow-up and a larger sample size is needed to confirm these findings and determine whether this is also the case when focusing on long-term prognosis.
Change history
20 June 2018
Upon publication of this article [1], it was noticed that there were some inconsistencies in Tables 1, 2 and 3. Some of the superscript letters were incorrectly assigned. Please see below the correct tables:
Abbreviations
- AD:
-
Alzheimer’s disease
- APOE:
-
Apolipoprotein E
- ARMWS:
-
Age-related white matter changes scale
- Aβ:
-
Amyloid-β
- BBACL:
-
BioBank Alzheimer Center Limburg
- CSF:
-
Cerebrospinal fluid
- CVD:
-
Cerebrovascular disease
- DESCRIPA:
-
Development of screening guidelines and criteria for predementia Alzheimer’s disease
- FTD:
-
Frontotemporal dementia
- MCI:
-
Mild cognitive impairment
- MMSE:
-
Mini Mental State Examination
- MRI:
-
Magnetic resonance imaging
- MTA:
-
Medial temporal lobe atrophy
- p-tau:
-
Phosphorylated tau
- RAVLT:
-
Rey Auditory Verbal Learning Test
- SCD:
-
Subjective cognitive decline
- TMT-B:
-
Trail Making Test part B
- t-tau:
-
Total tau
- WMH:
-
White matter hyperintensities
References
Schneider JA, Aggarwal NT, Barnes L, Boyle P, Bennett DA. The neuropathology of older persons with and without dementia from community versus clinic cohorts. J Alzheimers Dis. 2009;18(3):691–701.
Attems J, Jellinger KA. The overlap between vascular disease and Alzheimer’s disease - lessons from pathology. BMC Med. 2014;12:206.
Heyman A, Fillenbaum GG, Welsh-Bohmer KA, Gearing M, Mirra SS, Mohs RC, Peterson BL, Pieper CF. Cerebral infarcts in patients with autopsy-proven Alzheimer’s disease: CERAD, part XVIII. Consortium to Establish a Registry for Alzheimer’s Disease. Neurology. 1998;51(1):159–62.
Zea-Sevilla MA, Fernandez-Blazquez MA, Calero M, Bermejo-Velasco P, Rabano A. Combined Alzheimer’s disease and cerebrovascular staging explains advanced dementia cognition. Alzheimers Dement. 2015;11(11):1358–66.
Jack Jr CR, Wiste HJ, Vemuri P, Weigand SD, Senjem ML, Zeng G, Bernstein MA, Gunter JL, Pankratz VS, Aisen PS, et al. Brain β-amyloid measures and magnetic resonance imaging atrophy both predict time-to-progression from mild cognitive impairment to Alzheimer’s disease. Brain. 2010;133(11):3336–48.
Jellinger KA. Understanding the pathology of vascular cognitive impairment. J Neurol Sci. 2005;229–230:57–63.
Vemuri P, Knopman DS. The role of cerebrovascular disease when there is concomitant Alzheimer disease. Biochim Biophys Acta. 2016;1862(5):952–6.
Zekry D, Duyckaerts C, Moulias R, Belmin J, Geoffre C, Herrmann F, Hauw JJ. Degenerative and vascular lesions of the brain have synergistic effects in dementia of the elderly. Acta Neuropathol. 2002;103(5):481–7.
Vemuri P, Lesnick TG, Przybelski SA, Knopman DS, Preboske GM, Kantarci K, Raman MR, Machulda MM, Mielke MM, Lowe VJ, et al. Vascular and amyloid pathologies are independent predictors of cognitive decline in normal elderly. Brain. 2015;138(Pt 3):761–71.
Nebes RD, Snitz BE, Cohen AD, Aizenstein HJ, Saxton JA, Halligan EM, Mathis CA, Price JC, Kamboh MI, Weissfeld LA, et al. Cognitive aging in persons with minimal amyloid-β and white matter hyperintensities. Neuropsychologia. 2013;51(11):2202–9.
Ye BS, Seo SW, Kim GH, Noh Y, Cho H, Yoon CW, Kim HJ, Chin J, Jeon S, Lee JM, et al. Amyloid burden, cerebrovascular disease, brain atrophy, and cognition in cognitively impaired patients. Alzheimers Dement. 2015;11(5):494–503.e3.
Bastos-Leite AJ, van der Flier WM, van Straaten EC, Staekenborg SS, Scheltens P, Barkhof F. The contribution of medial temporal lobe atrophy and vascular pathology to cognitive impairment in vascular dementia. Stroke. 2007;38(12):3182–5.
Lo RY, Jagust WJ. Alzheimer’s Disease Neuroimaging Initiative. Vascular burden and Alzheimer disease pathologic progression. Neurology. 2012;79(13):1349–55.
Hesse C, Rosengren L, Andreasen N, Davidsson P, Vanderstichele H, Vanmechelen E, Blennow K. Transient increase in total tau but not phospho-tau in human cerebrospinal fluid after acute stroke. Neurosci Lett. 2001;297(3):187–90.
Freeze WM, Jacobs HI, Gronenschild EH, Jansen JF, Burgmans S, Aalten P, Clerx L, Vos SJ, van Buchem MA, Barkhof F, et al. White matter hyperintensities potentiate hippocampal volume reduction in non-demented older individuals with abnormal amyloid-β. J Alzheimers Dis. 2017;55(1):333–42.
Handels RL, Aalten P, Wolfs CA, OldeRikkert M, Scheltens P, Visser PJ, Joore MA, Severens JL, Verhey FR. Diagnostic and economic evaluation of new biomarkers for Alzheimer’s disease: the research protocol of a prospective cohort study. BMC Neurol. 2012;12:72.
Visser PJ, Verhey FR, Boada M, Bullock R, De Deyn PP, Frisoni GB, Frolich L, Hampel H, Jolles J, Jones R, et al. Development of screening guidelines and clinical criteria for predementia Alzheimer’s disease: the DESCRIPA Study. Neuroepidemiology. 2008;30(4):254–65.
Lezak MD, Howieson DB, Loring DW. Neuropsychological assessment. 4th ed. Oxford: Oxford University Press; 2004.
Reitan R. Trail-Making Test. Tucson: Reitan Neuropsychology Laboratory; 1979.
Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256(3):183–94.
American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: APA; 1994.
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34(7):939–44.
Roman GC, Tatemichi TK, Erkinjuntti T, Cummings JL, Masdeu JC, Garcia JH, Amaducci L, Orgogozo JM, Brun A, Hofman A, et al. Vascular dementia: diagnostic criteria for research studies: report of the NINDS-AIREN International Workshop. Neurology. 1993;43(2):250–60.
Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, Freedman M, Kertesz A, Robert PH, Albert M, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51(6):1546–54.
McKeith IG, Galasko D, Kosaka K, Perry EK, Dickson DW, Hansen LA, Salmon DP, Lowe J, Mirra SS, Byrne EJ, et al. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology. 1996;47(5):1113–24.
Vos SJ, Visser PJ, Verhey F, Aalten P, Knol D, Ramakers I, Scheltens P, Rikkert MG, Verbeek MM, Teunissen CE. Variability of CSF Alzheimer’s disease biomarkers: implications for clinical practice. PLoS One. 2014;9(6):e100784.
de Jong D, Kremer BP, Olde Rikkert MG, Verbeek MM. Current state and future directions of neurochemical biomarkers for Alzheimer’s disease. Clin Chem Lab Med. 2007;45(11):1421–34.
Mulder C, Verwey NA, van der Flier WM, Bouwman FH, Kok A, van Elk EJ, Scheltens P, Blankenstein MA. Amyloid-β(1–42), total tau, and phosphorylated tau as cerebrospinal fluid biomarkers for the diagnosis of Alzheimer disease. Clin Chem. 2010;56(2):248–53.
Aalten P, Ramakers IH, Biessels GJ, de Deyn PP, Koek HL, OldeRikkert MG, Oleksik AM, Richard E, Smits LL, van Swieten JC, et al. The Dutch Parelsnoer Institute - Neurodegenerative diseases; methods, design and baseline results. BMC Neurol. 2014;14:254.
Scheltens P, Leys D, Barkhof F, Huglo D, Weinstein HC, Vermersch P, Kuiper M, Steinling M, Wolters EC, Valk J. Atrophy of medial temporal lobes on MRI in “probable” Alzheimer’s disease and normal ageing: diagnostic value and neuropsychological correlates. J Neurol Neurosurg Psychiatry. 1992;55(10):967–72.
Korf ES, Wahlund LO, Visser PJ, Scheltens P. Medial temporal lobe atrophy on MRI predicts dementia in patients with mild cognitive impairment. Neurology. 2004;63(1):94–100.
Wahlund LO, Barkhof F, Fazekas F, Bronge L, Augustin M, Sjogren M, Wallin A, Ader H, Leys D, Pantoni L, et al. A new rating scale for age-related white matter changes applicable to MRI and CT. Stroke. 2001;32(6):1318–22.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149(2):351–6.
Wahlund LO, Westman E, van Westen D, Wallin A, Shams S, Cavallin L. Larsson EM; Imaging Cognitive Impairment Network (ICINET). Imaging biomarkers of dementia: recommended visual rating scales with teaching cases. Insights Imaging. 2017;8(1):79–90.
Carotenuto A, Rea R, Colucci L, Ziello AR, Molino I, Carpi S, Traini E, Amenta F, Fasanaro AM. Late and early onset dementia: what is the role of vascular factors? A retrospective study. J Neurol Sci. 2012;322(1-2):170–5.
Fazekas F, Barkhof F, Wahlund LO, Pantoni L, Erkinjuntti T, Scheltens P, Schmidt R. CT and MRI rating of white matter lesions. Cerebrovasc Dis. 2002;13 Suppl 2:31–6.
Braak H, Braak E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 1991;82(4):239–59.
Akinyemi RO, Firbank M, Ogbole GI, Allan LM, Owolabi MO, Akinyemi JO, Yusuf BP, Ogunseyinde O, Ogunniyi A, Kalaria RN. Medial temporal lobe atrophy, white matter hyperintensities and cognitive impairment among Nigerian African stroke survivors. BMC Res Notes. 2015;8:625.
Blennow K, Hampel H. CSF markers for incipient Alzheimer’s disease. Lancet Neurol. 2003;2(10):605–13.
Kurz A, Riemenschneider M, Wallin A. Potential biological markers for cerebrovascular disease. Int Psychogeriatr. 2003;15 Suppl 1:89–97.
Nelson PT, Alafuzoff I, Bigio EH, Bouras C, Braak H, Cairns NJ, Castellani RJ, Crain BJ, Davies P, Del Tredici K, et al. Correlation of Alzheimer disease neuropathologic changes with cognitive status: a review of the literature. J Neuropathol Exp Neurol. 2012;71(5):362–81.
Mattsson N, Insel PS, Donohue M, Landau S, Jagust WJ, Shaw LM, Trojanowski JQ, Zetterberg H, Blennow K, Weiner MW, et al. Independent information from cerebrospinal fluid amyloid-β and florbetapir imaging in Alzheimer’s disease. Brain. 2015;138(Pt 3):772–83.
Jack Jr CR, Bennett DA, Blennow K, Carrillo MC, Feldman HH, Frisoni GB, Hampel H, Jagust WJ, Johnson KA, Knopman DS, et al. A/T/N: an unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology. 2016;87(5):539–47.
Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 2010;341:c3666.
Gouw AA, Seewann A, van der Flier WM, Barkhof F, Rozemuller AM, Scheltens P, Geurts JJ. Heterogeneity of small vessel disease: a systematic review of MRI and histopathology correlations. J Neurol Neurosurg Psychiatry. 2011;82(2):126–35.
Prins ND, Scheltens P. White matter hyperintensities, cognitive impairment and dementia: an update. Nat Rev Neurol. 2015;11(3):157–65.
Wardlaw JM, Valdés Hernández MC, Muñoz-Maniega S. What are white matter hyperintensities made of? Relevance to vascular cognitive impairment. J Am Heart Assoc. 2015;4(6):001140.
Hoenig JM, Heisey DM. The abuse of power: the pervasive fallacy of power calculations for data analysis. Am Stat. 2001;55(1):19–24.
Acknowledgements
Not applicable.
Funding
The present study was conducted as part of the Project VPH-DARE@IT funded by the European Union Seventh Framework Programme (EU-FP7; FP7-ICT-2011-9-601055) under grant agreement number 601055, as well as by the European Medical Information Framework Alzheimer’s disease (EMIF-AD) project, which has received support from the Innovative Medicines Initiative joint undertaking under EMIF grant agreement number 115372, resources of which are composed of financial contributions from the European Union’s Seventh Framework Programme (FP7/2007-2013) and European Federation of Pharmaceutical Industries and Associations (EFPIA) companies’ in-kind contribution. The DESCRIPA study was funded by the European Commission within the 5th framework program (QLRT-2001-2455). The LeARN project was supported by the Center for Translational Molecular Medicine (www.ctmm.nl), grant agreement number 02 N-101.
Availability of data and materials
The datasets analyzed during the present study are not publicly available, but they are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
IB and SJBV conceived of and designed the study. All authors acquired and/or interpreted data. IB, SJBV, and PJV performed statistical analysis and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from all participants before inclusion in the study. The medical ethics committee at each site approved the study (Additional file 3).
Consent for publication
Not applicable.
Competing interests
IB receives research support from the Innovative Medicines Initiative Joint Undertaking under EMIF grant agreement number 115372 resources that are composed of financial contributions from EU FP7 (FP7/2007-2013) and in-kind contributions from EFPIA. HH serves as a senior associate editor for the journal Alzheimer’s & Dementia®. HH has been a scientific consultant and/or speaker and/or attended scientific advisory boards of Axovant Sciences, Anavex Life Sciences, Eli Lilly and Company, GE Healthcare Life Sciences, Cytox, Jung Diagnostics, Roche, Biogen Idec, Takeda-Zinfandel, and Oryzon Genomics; receives research support from the Association for Alzheimer Research (Paris), Pierre and Marie Curie University (Paris), Pfizer and Avid (paid to institution); and has patents as a coinventor but has received no related royalties. PS has acquired grant support (for the institution) from GE Healthcare Life Sciences, Danone Research, Piramal, and Merck. In the past 2 years, PS has received consultancy/speaker’s fees (paid to the institution) from Eli Lilly and Company, GE Healthcare Life Sciences, Janssen Pharmaceuticals, Probiodrug, Biogen, Roche, and EIP Pharma. PJV receives research support from the Innovative Medicines Initiative Joint Undertaking under EMIF grant agreement number 115372 and European Prevention of Alzheimer's Dementia grant agreement 115736, resources that are composed of financial contributions from EU FP7 (FP7/2007-2013) and in-kind contributions from EFPIA. SJBV receives research support from ZonMw and from the Innovative Medicines Initiative Joint Undertaking under EMIF grant agreement number 115372, resources that are composed of financial contributions from EU FP7 (FP7/2007-2013) and in-kind contributions from EFPIA. All other authors declare no conflict of interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Scan parameters and MRI protocols used at each center. (DOCX 87 kb)
Additional file 2:
Additional results in age-matched groups. Results that deviate in age sensitivity analyses from original findings. (DOCX 56 kb)
Additional file 3:
Approval committee of each center. The ethics committee in each center that approved the data acquisition. (DOCX 84 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bos, I., Verhey, F., Ramakers, I. et al. Cerebrovascular and amyloid pathology in predementia stages: the relationship with neurodegeneration and cognitive decline. Alz Res Therapy 9, 101 (2017). https://doi.org/10.1186/s13195-017-0328-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-017-0328-9