Abstract
Orthopedic foreign body-associated infection can be difficult to treat due to the formation of biofilms protecting microorganisms from both antimicrobials and the immune system. Exebacase is an antistaphylococcal lysin (cell wall hydrolase) under consideration for local treatment for biofilm-based infections caused by methicillin-resistant Staphylococcus aureus (MRSA). To determine the activity of exebacase, we formed MRSA biofilms on orthopedic Kirschner wires and exposed them to varying concentrations (0.098, 0.98, 9.8 mg/ml) of exebacase and/or daptomycin over 24 h. The biofilm consisted of 5.49 log10 colony forming units (cfu)/K-wire prior to treatment and remained steady throughout the experiment. Exebacase showed significant biofilm reduction at all timepoints (up to 5.78 log10 cfu/K-wire; P < 0.0495) compared to the controls at all concentrations and all time points with bactericidal activity (> 3 log10 cfu/K-wire reduction) observed for up to 12 h for the 0.098 and 0.98 mg/ml concentrations and at 24 h for 9.8 mg/ml. Daptomycin showed significant biofilm reduction, although non-bactericidal, at all time points for 0.98 and 9.8 mg/ml and at 4 and 8 h with 0.098 mg/ml (P < 0.0495). This study supports further evaluation of local administration of exebacase as a potential treatment for orthopedic implant infections.
Similar content being viewed by others
Introduction
Orthopedic implant related infections represent a challenging issue in patients with implanted instrumentation or medical devices. The location of the orthopedic implant offers bacteria an environment to evade both systemic antibiotics and the immune system. When implants become infected, bacteria often form protective biofilms, and colonize the local bone tissue by invading the osteocyte lacuno-canalicular network and entering cells such as osteoblasts and fibroblasts, shielding themselves from neighboring immune cells [1, 2]. These areas also have low blood supply, limiting access of antibiotics delivered systemically. Surgery is often needed to debride infected sites, sometimes with implant removal [3]. Local treatment options are limited but would be beneficial in treating these hard-to-reach infections.
Exebacase is a recombinantly produced peptidoglycan hydrolytic enzyme that elicits rapid cell wall destabilization and concomitant osmotic lysis of staphylococci. Exebacase exhibits (i) rapid, targeted bactericidal activity; (ii) synergy with antistaphylococcal antibiotics, including daptomycin (DAP) and vancomycin; (iii) a low propensity for the development of resistance; (iv) no cross-resistance with antibiotics; (v) the capacity to both suppress antibiotic resistance and “re-sensitize” antibiotic-resistant bacteria; and (vi) in vitro and in vivo postantibiotic effects [4,5,6,7,8,9,10,11,12,13]. In vivo activity has been demonstrated in experimental animal models of S. aureus infection, including murine bacteremia [8], pneumonia [10] and thigh infection [14]; rat osteomyelitis [15]; and rabbit endocarditis [16] and implant related infection [17]. Here, exebacase (ContraFect, Yonkers, NY) and/or daptomycin (Teva Pharmaceuticals USA Inc., North Wales, PA) at varying concentrations were tested against methicillin-resistant Staphylococcus aureus (MRSA) biofilms on orthopedic Kirschner wires (K-wires).
Methods
Biofilms were established on 5 × 1.1 mm threaded stainless steel K-wires (Zimmer Biomet, Warsaw, IN) in 1 ml containing 106 cfu/ml of MRSA IDRL-6169 (clinical MRSA isolate from a periprosthetic hip infection at Mayo Clinic) in Bacto™ Tryptic Soy Broth (BD, Sparks, MD) (TSB) at 37 °C on an orbital shaker. After 10 h, K-wires were randomly transferred to one of nine treatment groups in triplicate. The two control groups were the exebacase carrier (20 mM L-histidine and 5% D-sorbitol) and the daptomycin carrier (saline). Exebacase and daptomycin each were tested at 0.098, 0.98 and 9.8 mg/ml. The combination of exebacase and daptomycin at 0.098 mg/ml each was also tested. K-wires were placed into 40 μl of solution and treated for 2, 4, 8, 12 or 24 h, after which they were removed from the treatment solution and rinsed in sterile saline to remove remnant solution that could impede organism recovery. To recover any remaining viable biofilm, K-wires were placed into 0.5 ml of sterile saline, vortexed for 30 s, sonicated for 5 min (40 kHz, 0.22 W/cm2) and vortexed an additional 30 s. Sonicate fluid was serially diluted and plated onto Trypticase™ Soy Agar with 5% Sheep Blood (BD, Sparks, MD) and 3 ml TSB was added to the remaining sonicate fluid. Cultures were incubated for 48 h at 37 °C. Results were reported as mean log10 colony forming units (cfu)/K-wire. Positive broth cultures were reported as 0.65 log10 cfu/K-wire and the limit of detection was 0.13 log10 cfu/K-wire. Statistical analyses were performed using SAS software version 9.4 (SAS Inc, Cary, NC) with the Wilcoxon rank sum test for making pairwise comparisons between the groups. P-values less than 0.05 were considered significant.
Results
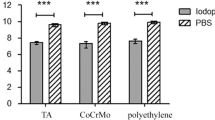
Biofilm time kill curves are shown in Fig. 1. The mean biofilm density was 5.49 log10 cfu/K-wire prior to treatment. Biofilm density of the controls remained steady throughout the time course of experiments, with biofilms in controls (exebacase and daptomycin carriers) being 5.69 and 5.79 log10 cfu/K-wire, respectively, at 24 h. In Fig. 1A, exebacase was more active than the control carrier solution at all concentrations and showed significant biofilm reduction at all timepoints (up to 5.78 log10 cfu/K-wire; P < 0.0495). Bactericidal activity (> 3 reduction of log10 cfu/K-wire compared to carrier control) was observed for up to 12 h for the 0.098 and 0.98 mg/ml concentrations and at 24 h for the highest concentration, with over a 5 log10 reduction compared to carrier control (Table 1). In Fig. 1B, daptomycin showed activity, although non-bactericidal, at all time points for 0.98 and 9.8 mg/ml and at 4 and 8 h with 0.098 mg/ml (P < 0.0495). In Fig. 1C, the combination of daptomycin (0.098 mg/ml) and exebacase (0.098 mg/ml) also showed significant biofilm reduction compared to carrier control (up to 5.29 log10 cfu/K-wire; P < 0.0201). The use of daptomycin in addition to exebacase did not provide a significant benefit over the bactericidal activity demonstrated for exebacase alone.
Discussion
Lytic agents such as exebacase offer a potential novel mechanism to reduce the infectious burden and possibly potentiate activities of the immune system and traditional antibiotics. Previously, it was shown that exebacase reduces bacterial load when administered systemically, especially in combination with traditional antibiotics [8, 14,15,16]. Schuch et al. (2014) showed in vitro synergy with exebacase (referred to as CF-301) and daptomycin or vancomycin and that exebacase and daptomycin activity increased survival in a mouse S. aureus bacteremia model [8]. In a rat MRSA osteomyelitis model, the addition of exebacase administered systemically improved treatment outcome versus daptomycin alone [15].
This work provides a demonstration of bactericidal activity elicited by exebacase against MRSA biofilm on stainless steel orthopedic K-wires. These results are similar to previous work showing bactericidal activity against the same strain on titanium orthopedic cortex screws [17], suggesting that exebacase could be used for infections associated with several orthopedic implant types. We have also shown that local administration of exebacase into rabbit tibiae with implanted MRSA seeded screws reduced bacterial burden [17]. Results of this study provide support for further evaluation of local administration of exebacase as a potential treatment for orthopedic implant infections.
Limitations
The current study was limited in the number of replicates and timepoints performed and testing of a single bacterial species and S. aureus strain. In addition, the study was limited to one antibiotic and one implant type. Emergence of antibiotic/lysin resistance was also not tested.
Data Availability
Data is available from the corresponding author upon request.
Abbreviations
- cfu:
-
Colony forming unit
- DAP:
-
Daptomycin
- EXE:
-
Exebacase
- K-wire:
-
Kirschner wire
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
References
Masters EA, Trombetta RP, de Mesy Bentley KL, Boyce BF, Gill AL, Gill SR, Nishitani K, Ishikawa M, Morita Y, Ito H. Evolving concepts in bone infection: redefining “biofilm”, “acute vs. chronic osteomyelitis”, “the immune proteome” and “local antibiotic therapy”. Bone Res. 2019;7(1):1–18.
Muthukrishnan G, Masters EA, Daiss JL, Schwarz EM. Mechanisms of immune evasion and bone tissue colonization that make Staphylococcus aureus the primary pathogen in osteomyelitis. Curr Osteopor Rep. 2019;17(6):395–404.
Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR. Executive summary: diagnosis and management of prosthetic joint infection: clinical practice guidelines by the infectious Diseases Society of America. Clin Infect Dis. 2013;56(1):1–10.
Fowler VG, Das AF, Lipka-Diamond J, Schuch R, Pomerantz R, Jáuregui-Peredo L, Bressler A, Evans D, Moran GJ, Rupp ME. Exebacase for patients with Staphylococcus aureus bloodstream infection and endocarditis. J Clin Invest. 2020;130(7):3750–60.
Kebriaei R, Stamper KC, Lev KL, Morrisette T, Abdul-Mutakabbir JC, Schuch R, Lehoux D, Rybak MJ. Exebacase, in addition to daptomycin against MRSA. Antimicrob Agents Chemother. 2021;65(11):00128–21.
Oh JT, Cassino C, Schuch R. Postantibiotic and sub-MIC effects of exebacase (lysin CF-301) enhance antimicrobial activity against Staphylococcus aureus. Antimicrob Agents Chemother. 2019;63(6):e02616–18.
Schuch R, Khan BK, Raz A, Rotolo JA, Wittekind M. Bacteriophage lysin CF-301: a potent anti-staphylococcal biofilm agent. Antimicrob Agents Chemother. 2017;61(7):02666–16.
Schuch R, Lee HM, Schneider BC, Sauve KL, Law C, Khan BK, Rotolo JA, Horiuchi Y, Couto DE, Raz A, Fischetti V, Huang DB, Nowinski RC, Wittekind M. Combination therapy with lysin CF-301 and antibiotic is superior to antibiotic alone for treating methicillin-resistant Staphylococcus aureus–induced murine bacteremia. J Infect Dis. 2014;209(9):1469–78.
Souche A, Kolenda C, Teoli J, Schuch R, Ferry T, Laurent F, Josse J. Activity of exebacase (CF-301) against biofilms formed by Staphylococcus epidermidis strains isolated from prosthetic joint infections. Antimicrob Agents Chemother. 2022;66(8):e00588–22.
Swift SM, Sauve K, Cassino C, Schuch R. Exebacase is active in vitro in pulmonary surfactant and is efficacious alone and synergistic with daptomycin in a mouse model of lethal Staphylococcus aureus lung infection. Antimicrob Agents Chemother. 2021;65(9):e02723–20.
Traczewski M, Oh J, Cassino C, Schuch R. Vitro activity of exebacase (CF-301) against clinical Staphylococcus aureus surveillance isolates from the United States, Europe, and Latin America, 2015–2017. Diagn Microbiol Infect Dis. 2019;95(4):114879.
Watson A, Oh JT, Sauve K, Bradford PA, Cassino C, Schuch R. Antimicrobial activity of exebacase (lysin CF-301) against the most common causes of infective endocarditis. Antimicrob Agents Chemother. 2019;63(10):e01078–19.
Watson A, Sauve K, Cassino C, Schuch R. Exebacase demonstrates in vitro synergy with a broad range of antibiotics against both methicillin-resistant and methicillin-susceptible Staphylococcus aureus. Antimicrob Agents Chemother. 2020;64(2):e01885–19.
Asempa TE, Abdelraouf K, Carabeo T, Schuch R, Nicolau DP. Synergistic activity of exebacase (CF-301) in addition to daptomycin against Staphylococcus aureus in a neutropenic murine thigh infection model. Antimicrob Agents Chemother. 2019;64(3):e02176–19.
Karau MJ, Schmidt-Malan SM, Yan Q, Greenwood-Quaintance KE, Mandrekar J, Lehoux D, Schuch R, Cassino C, Patel R. Exebacase in addition to daptomycin is more active than daptomycin or exebacase alone in methicillin-resistant Staphylococcus aureus osteomyelitis in rats. Antimicrob Agents Chemother. 2019;63(10):e01235–19.
Shah SU, Xiong YQ, Abdelhady W, Iwaz J, Pak Y, Schuch R, Cassino C, Lehoux D, Bayer AS. Effect of the lysin exebacase on cardiac vegetation progression in a rabbit model of methicillin-resistant Staphylococcus aureus endocarditis as determined by echocardiography. Antimicrob Agents Chemother. 2020;64(7):e00482–20.
Karau M, Schmidt-Malan S, Mandrekar J, Lehoux D, Schuch R, Cassino C, Patel R. Locally delivered antistaphylococcal lysin exebacase or CF-296 is active in methicillin-resistant Staphylococcus aureus implant-associated osteomyelitis. J Bone Joint Infect. 2022;7(4):169–75.
Funding
Funding provided by ContraFect Corporation through a grant from the Assistant Secretary of Defense for Health Affairs, through the Military Infectious Diseases Research Program-Broad Agency Announcement for Extramural Medical Research (grant no. W81XWH-19-l-0139).
Author information
Authors and Affiliations
Contributions
MJ, DL and RP designed the study. MJ performed the study, analyzed the data, and prepared the figures and manuscript. JM provided statistical support. All authors reviewed the data and the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Mayo Clinic Institutional Review Board approved the use (IRB #1770-00) of clinical isolate MRSA IDRL-6169 for use in this study.
Consent for publication
Not applicable.
Competing interests
RS, CC and DL were employed at Contrafect Corporation at the time the work was being completed. DL assisted in designing the study. RS, CC and DL reviewed the data and approved the final manuscript. MK and JM have no interests to declare. RP reports grants from ContraFect, TenNor Therapeutics Limited, and BioFire; is a consultant to PhAST, Torus Biosystems, Day Zero Diagnostics, Mammoth Biosciences, and HealthTrackRx with monies paid to Mayo Clinic. RP has research supported by Adaptive Phage Therapeutics, is a consultant to Netflix, Abbott Laboratories, and CARB-X and has a patent on Bordetella pertussis/parapertussis PCR issued, on a device/method for sonication with royalties paid by Samsung to Mayo Clinic, and on an anti-biofilm substance. RP receives honoraria from the NBME, Up-to-Date and the Infectious Diseases Board Review Course.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Karau, M.J., Mandrekar, J., Lehoux, D. et al. In vitro activity of exebacase against methicillin-resistant Staphylococcus aureus biofilms on orthopedic Kirschner wires. BMC Res Notes 16, 209 (2023). https://doi.org/10.1186/s13104-023-06468-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-023-06468-y