Abstract
Background
Diabetic gastroparesis is a severe diabetic complication refers to delayed gastric emptying in the absence of mechanical obstruction of the stomach. Vitamin B12 affects the dynamics of autonomic nervous system and its deficits has been linked to cardiovascular autonomic neuropathy therefore, vitamin B12 deficiency was hypothesized to be implicated in the development of diabetic gastroparesis. This study was conducted to explore the possible association between vitamin B12 deficiency and gastroparesis in patients with type 2 diabetes (T2D).
Methods
A total of 100 T2D patients with diabetes duration > 10 years and 50 healthy controls matched for age and sex were recruited for this study. T2D patients were divided into 2 groups: patients with gastroparesis and patients without gastroparesis. The diagnosis of gastroparesis was based on Gastroparesis Cardinal Symptom Index (GCSI) Score ≥ 1.9 and ultrasonographic findings including gastric emptying ˂ 35.67% and motility index ˂ 5.1. Anthropometric measurements, plasma glucose, glycosylated hemoglobin (HbA1c), lipids profile, vitamin B12 and transabdominal ultrasonography were assessed.
Results
The frequency of vitamin B12 deficiency in total patients with T2D was 35% (54.5% in patients with gastroparesis vs. 11.1% in patients without gastroparesis, P < 0. 001). Vitamin B12 level was negatively correlated with GCSI Score whereas, it was positively correlated with gastric emptying and motility index. Vitamin B12 deficiency was an independent predictor for gastroparesis in patients with T2D; it predicts gastroparesis at a cut off value of 189.5 pmol/L with 69.1% sensitivity and 64.4% specificity, P = 0.002.
Conclusions
Beside the known risk factors of diabetic gastroparesis, vitamin B12 deficiency is an independent predictor of diabetic gastroparesis in patients with T2D.
Similar content being viewed by others
Background
Diabetic gastroparesis is a clinical syndrome characterized by delayed gastric emptying in the absence of mechanical obstruction of the stomach [1]. The characteristic symptoms of gastroparesis are early satiety, nausea, vomiting, bloating and upper abdominal pain [2] however, diabetic gastroparesis is often asymptomatic [3, 4]. Diabetic gastroparesis is not uncommon disease [5]; the reported prevalence from the tertiary referral centers is 10–30% of patients with type 2 diabetes (T2D) [6,7,8] whereas, the community prevalence using strict diagnostic criteria is 1.1% of patients with T2D [9]. Autonomic neuropathy, enteropathy and hyperglycemia are the most frequently implicated risk factors of diabetic gastroparesis [2, 10, 11]. Delayed gastric emptying leads to poor glycemic control and increased risk of hypoglycemia [12]. Indeed, gastroparesis significantly impairs quality of life [9] and is associated with morbidity and mortality [5, 13].
Recently, vitamin B12 levels have been found to be inversely related to glucose intolerance [14]. Additionally, vitamin B12 affects the dynamics of autonomic nervous system [15] and its deficits has been linked to cardiovascular autonomic neuropathy [16]. Vitamin B12 deficiency may be also implicated in the development of diabetic gastroparesis however, this association has not been yet investigated. Therefore, the aim of the present study was to explore the possible association between vitamin B12 deficiency and diabetic gastroparesis in patients with T2D.
Methods
This study comprised 100 adult patients with T2D and 50 age- and sex-matched healthy controls. Patients with T2D were consecutively recruited from Diabetes Outpatient Clinic at Mansoura Specialized Medical Hospital, Mansoura University, Mansoura, Egypt. The inclusion criteria were patients with duration of T2D > 10 years and who had symptoms of gastroparesis [Gastroparesis Cardinal Symptom Index (GCSI) Score ≥ 1.9]. Patients with T2D were submitted for transabdominal ultrasonography accordingly, they divided into 2 groups: patients with gastroparesis (n = 55) and patients without gastroparesis (n = 45). Exclusion criteria were history of digestive tract surgery or prior gastric outlet obstruction, thyroid disease, liver & renal failure, neuropsychiatric disorder, connective tissue disorders, malignancies, pregnancy and participants taking vitamin B12 and alcohol. Drugs that could potentially interfere with gastrointestinal motility such as GLP-1 receptor agonists and the amylin analog, α glucosidase inhibitors, and opioid analgesic were also excluded. Healthy controls were recruited from the same geographic area with the same exclusion criteria.
All participants were subjected to a thorough medical history and underwent a clinical examination. Anthropometric measurements including height, body weight, body mass index (BMI) (kg/m2), and waist circumference (WC) were obtained using standardized techniques. The diagnosis of diabetic gastroparesis was based on the symptom validated questionnaire GCSI Score ≥ 1.9 and ultrasonographic findings including gastric emptying ˂ 35.67% and motility index ˂ 5.1. The cut-off point of gastric emptying and motility index were calculated from our study healthy controls as mean—2SD.
The GCSI Score consists of 9 symptoms covering 3 areas; nausea/vomiting subscale (3 symptoms: nausea, vomiting and retching), postprandial fullness/early satiety subscale (4 symptoms: stomach fullness, early satiety, postprandial fullness and loss of appetite) and bloating subscale (2 symptoms: bloating and stomach distension). All symptoms are rated from 0 to 5 over the prior 2 weeks [no symptoms = 0, very mild = 1, mild = 2, moderate = 3, severe = 4, and very severe = 5]. GCSI Score was calculated as the average of the 3 symptom subscales [17]. The clinical severity of gastroparesis was graded on a scale originally proposed by Abell et al. [18]; grade 1: mild gastroparesis (symptoms are relatively easily controlled and weight and nutrition can be maintained with a regular diet); grade 2: compensated gastroparesis (symptoms are partially controlled with the use of daily medications and nutrition can be maintained with dietary adjustments); grade 3: gastroparesis with gastric failure (uncountable refractory symptoms with frequent hospitalizations and/or inability to maintain nutrition via an oral route).
Vitamin B12 deficiency was defined as vitamin B12 levels below 125 pmol/L [16]. Peripheral neuropathy was diagnosed based on neuropathy disability and symptom scores [19, 20]. Diabetic nephropathy was diagnosed according to Umanath & Lewis [21]. Diabetic retinopathy was assessed through fundus examination.
Laboratory assay
Fasting plasma glucose (FPG) and 2-h post prandial plasma glucose (PPG) were measured by commercially available kit, Cobas (Integra-400) supplied by Roche Diagnostics (Mannheim, Germany). Glycated hemoglobin (HbA1c) was estimated as an index of metabolic control on a DCA 2000 analyzer, fast ion exchange resin (Roche Diagnostic, Germany. Total cholesterol (TC), triglycerides (TGs) and high density lipoprotein cholesterol (HDL-C) were measured by commercially available kits (Cobas Integra-400). Low density lipoprotein cholesterol (LDL-C) was calculated according to Friedewald et al. [22]. Complete metabolic panel including ESR, complete blood count, renal, liver and thyroid function tests were also assessed. Serum vitamin B12 level was assayed by ELISA technique supplied by Bioassay technology.
Ultrasonography assessment of gastric motility
After an overnight fasting, patients sat in a chair, leaned slightly backwards and drank 400 ml meat soup (54.8 kcal, 0.38 g protein and 0.25 g fat). An ultrasound probe was positioned vertically to permit simultaneous visualization of the gastric antrum, superior mesenteric artery and abdominal aorta for evaluation of the antral contractions Fig 1. The examination was conducted by GE LOGIQ E9 ultrasound machine with a 5 MHz convex probe [23]. The gastric emptying (%) was estimated as: ([antral area at 1 min] – [antral area at 15 min]/antral area at 1 min) × 100. The motility index was estimated by calculating the mean amplitude x frequency of contractions. The amplitude of antral contractions is the difference between the relaxed and contracted areas during a 3-min interval, divided by the relaxed area. The frequency of antral contractions is the number of contractions during a 3-min interval beginning 2 min after ingestion of soup. Ultrasonography was assessed by the same operator to minimize variation in the examination procedure. Fasting blood glucose was less than 275 mg/dl on the day of testing and patients had stopped prokinetic drugs 7 days before the procedure.
Statistical analysis
This study was a pilot study with an initial sample size of 20 T2D patients who were excluded from the full scale study. The final calculated sample size was 97. Data entry and analysis were done by the SPSS statistical package (version 22, Armonk, NY: IBM Corp). The data were expressed as mean ± SD for continuous data, number and percent for categorical data and median (minimum–maximum) for skewed data. Student’s t and Mann–Whitney U tests were used to compare the 2 studied groups for parametric and non-parametric data, respectively. The chi-square and Fischer exact tests were performed to compare 2 or more groups of qualitative variables. The correlations of GCSI Score, gastric emptying and motility index with all other studied variables were analyzed by the Pearson and Spearman correlations analysis. Binary stepwise logistic regression analysis was used to predict the independent variables of binary outcome; the significant predictors in the univariate analysis were entered into the regression model. Receiver operating characteristic (ROC) curve was done to detect the level of vitamin B12 associated with gastroparesis in patients with T2D. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), area under the curve (AUC) and 95% CI were evaluated. P ≤ 0.05 was considered as significant.
Results
Patients with T2D had significantly higher BMI, WC, systolic & diastolic blood pressures (SBP & DBP), FPG, 2 h PPG, HbA1c, TC, TGs, LDL-C and lower HDL-C than did healthy controls. Among the studied participants with T2D, the median age of diabetes duration was 17 years, 63% had hypertension, 32% had retinopathy, 24% had diabetic nephropathy and 43% had neuropathy (18% moderate, 25% severe). With regard to anti-diabetic medications, 40% received insulin, 37% received oral anti-diabetic drugs and 23% received combined oral anti-diabetic drugs and insulin. Vitamin B12 was significantly lower in patients with T2D than in healthy controls, the frequency of vitamin B12 deficiency was 35% Table 1.
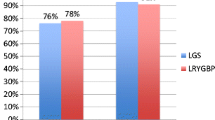
T2D patients with gastroparesis had significantly longer diabetes duration, higher BMI, WC, SBP, DBP, FPG, HbA1c, TC, TGs and LDL-C compared with those without gastroparesis. The frequency of hypertension, proliferative retinopathy, nephropathy and peripheral neuropathy were significantly higher in patients with gastroparesis than in those without gastroparesis. Vitamin B12 level was significantly lower in patients with gastroparesis than in those without gastroparesis. The frequency of vitamin B12 deficiency was 54.5% in patients with gastroparesis and 11.1% in patients without gastroparesis, P = 0.001. The grade of gastroparesis in T2D patients was distributed as 78.2% for grade 1, 21.8% for grade 2 with no reported cases in grade 3. Gastric emptying and motility index were significantly lower in T2D patients with gastroparesis than in those without gastroparesis. With regard to GCSI Score, there was no significant difference between patients with and without gastroparesis, Table 2.
GCSI Score was positively correlated with female sex, duration of T2D, BMI, SBP, DBP, retinopathy, nephropathy, neuropathy, FPG, HbA1c and grade of gastroparesis. Gastric emptying and motility index were negatively correlated with female sex, duration of T2D, BMI, SPB, DBP, retinopathy, nephropathy, neuropathy, FPG, HbA1c, TC, TGs and grade of gastroparesis. Table 3 Vitamin B12 levels were negatively correlated with GCSI Score and positively correlated with gastric emptying and motility index Figs 2, 3 and 4.
Female sex, duration of T2D, BMI, retinopathy, neuropathy, nephropathy, FPG, HbA1c, TC, TGs and vitamin B12 deficiency were significant positive predictors of gastroparesis in patients with T2D Table 4. The cutoff value of vitamin B12 level associated with gastroparesis was 189.5 pmol/I with 69.1% sensitivity, 64.4% specificity, 70.4% PPV and 63% NPV, AUC was 0.678, 95% CI (0.586–0.788), P = 0.002 Fig 5.
Discussion
In the current study, the diagnosis of diabetic gastroparesis was based on GCSI Score and transabdominal ultrasonography. Although gastric scintigraphy is the gold standard for diagnosis of gastroparesis [24, 25], ultrasonography is a radiation-free, readily available and a valid reliable imaging approach [26,27,28]. With transabdominal ultrasonography, gastric emptying and motility index were negatively correlated with female sex, duration of T2D, BMI, SPB, DBP, retinopathy, neuropathy, nephropathy, FPG, HbA1c, TC, TGs and grade of gastroparesis whereas, gastric emptying and motility index were not significantly correlated with GCSI Score. In line, Sogabe et al. [29] showed that gastric emptying and motility index values were significantly correlated with FPG. Authors concluded that the achievement of glycemic control improves both of gastric motility and gastrointestinal symptoms in patients with diabetic gastroparesis. Consistent with our results, Steinsvik et al. [30] found no significant associations between symptoms of gastroparesis and measurements of ultrasonography in patients with diabetic gastroparesis. In contrast, Darwiche et al. [31] found no significant associations between gastric emptying and the duration of diabetes, HbA1c, age or BMI; these incompatible findings are probably due to their small sample size.
In the present study, vitamin B12 level was significantly lower in patients with T2D than in healthy controls moreover, it was significantly lower in T2D patients with gastroparesis than in those without gastroparesis. Of interest, vitamin B12 was negatively correlated with GCSI Score whereas, it was positively correlated with gastric emptying and motility index. Additionally, vitamin B12 deficiency was an independent predictor for gastroparesis in patients with T2D. Vitamin B12 predicts gastroparesis at a cutoff value of 189.5 pmol/L with 69.1% sensitivity, 64.4% specificity, 70.4% PPV and 63% NPV, P = 0.002.
In the current study, the frequency of vitamin B12 deficiency in total patients with T2D was 35% (54.5% in patients with gastroparesis and 11.1% in patients without gastroparesis). However, our findings are much higher than estimates from a study conducted by Amjad et al. [32] where vitamin B12 deficiency was detected in 17.5% of patients with gastroparesis either diabetic or non-diabetic. The definition of vitamin B12 deficiency varies between studies; the cutoff point used in this study was 125 pmol/L which is comparable with Hansen et al. [16] however, it is low compared with what is used in other studies [33, 34]. The variability of cutoff limit for vitamin B12 could be explained by heterogeneity in age and race in the study populations.
Vitamin B12 deficiency is a major public health problem caused by age, consumption of vegetarian diets, malabsorption and drugs such as chronic use of omeprazole and metformin [35,36,37,38]. An adequate vitamin B12 is essential for the proper functioning of the nervous system through maintenance of the myelin nerve sheaths [39, 40] therefore, vitamin B12 deficiency induces neurological disorders such as peripheral neuropathy [41, 42]. Moreover, vitamin B12 is used in the treatment of peripheral neuropathy [43]. Furthermore, vitamin B12 affects the dynamics of autonomic nervous system [15] and a significant association between vitamin B12 deficiency and cardiovascular autonomic neuropathy has been recently reported [16]. In the light of these findings, we hypothesized that vitamin B12 deficiency may be also implicated in the development of diabetic gastroparesis. To our knowledge, this is the first study to indicate the independent association between vitamin B12 and diabetic gastroparesis.
In our study participants, the independent predictors of gastroparesis other than vitamin B12 deficiency were female sex, duration of diabetes, BMI, diabetic microvasascular complications, FPG, HbA1c, TGs and TC which are consistent with the existing literature [44,45,46].
In the current study, we did not observe an association between metformin treatment and diabetic gastroparesis. The increased frequency of vitamin B12 deficiency among patients with T2D taking metformin has been previously reported [47, 48], however this association depends on both the dose and the duration of treatment [49, 50]. It is believed that metformin induces vitamin B12 deficiency 5–10 years after treatment initiation due to late depletion of body storages [50]. In our study population, the duration of treatment was less than 5 years which may explain our finding.
Finally, in addition to sex, duration of diabetes, BMI, diabetic microvasascular complications, FPG, HbA1c, TGs and TC, vitamin B12 deficiency was an independent predictor of diabetic gastroparesis. From the previous discussion 2 raising questions arise which needs further studies. First, whether gastroparesis leads to vitamin B12 deficiency therefore, vitamin B12 may be a cause and a consequence of diabetic gastroparesis. Second, whether vitamin B12 supplementation can improve diabetic gastroparesis.
In conclusion
Beside the known risk factors of diabetic gastroparesis, vitamin B12 deficiency is an independent predictor of diabetic gastroparesis in patients with T2D.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Parkman HP, Hasler WL, Fisher RS. American gastroenterological association medical position statement: diagnosis and treatment of gastroparesis. Gastroenterology. 2004;127(5):1589–91.
Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L. Clinical guideline: management of gastroparesis. Am J Gastroenterol. 2013;108(1):18–37.
Camilleri M, Bharucha AE, Farrugia G. Epidemiology, mechanisms, and management of diabetic gastroparesis. Clin Gastroenterol Hepatol. 2011;9(1):5–12.
Bharucha AE, Kudva Y, Basu A, Camilleri M, Low PA, Vella A, et al. Relationship between glycemic control and gastric emptying in poorly controlled type 2 diabetes. Clin Gastroenterol Hepatol. 2015;13(3):466-76.e1.
Jung HK, Choung RS, Locke GR 3rd, Schleck CD, Zinsmeister AR, Szarka LA, et al. The incidence, prevalence, and outcomes of patients with gastroparesis in Olmsted County, Minnesota, from 1996 to 2006. Gastroenterology. 2009;136(4):1225–33.
Horowitz M, Harding PE, Maddox AF, Wishart JM, Akkermans LM, Chatterton BE, et al. Gastric and oesophageal emptying in patients with type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia. 1989;32(3):151–9.
Intagliata N, Koch KL. Gastroparesis in type 2 diabetes mellitus: prevalence, etiology, diagnosis, and treatment. Curr Gastroenterol Rep. 2007;9(4):270–9.
Koch KL, Calles-Escandón J. Diabetic gastroparesis. Gastroenterol Clin North Am. 2015;44(1):39–57.
Choung RS, Locke GR 3rd, Schleck CD, Zinsmeister AR, Melton LJ 3rd, Talley NJ. Risk of gastroparesis in subjects with type 1 and 2 diabetes in the general population. Am J Gastroenterol. 2012;107(1):82–8.
Bharucha AE, Camilleri M, Low PA, Zinsmeister AR. Autonomic dysfunction in gastrointestinal motility disorders. Gut. 1993;34(3):397–401.
Rayner CK, Samsom M, Jones KL, Horowitz M. Relationships of upper gastrointestinal motor and sensory function with glycemic control. Diabetes Care. 2001;24(2):371–81.
Kashyap P, Farrugia G. Diabetic gastroparesis: what we have learned and had to unlearn in the past 5 years. Gut. 2010;59(12):1716–26.
Hyett B, Martinez FJ, Gill BM, Mehra S, Lembo A, Kelly CP, et al. Delayed radionucleotide gastric emptying studies predict morbidity in diabetics with symptoms of gastroparesis. Gastroenterology. 2009;137(2):445–52.
Jayashri R, Venkatesan U, Rohan M, Gokulakrishnan K, Shanthi Rani CS, Deepa M, et al. Prevalence of vitamin B12 deficiency in South Indians with different grades of glucose tolerance. Acta Diabetol. 2018;55(12):1283–93.
Karnaze DS, Carmel R. Neurologic and evoked potential abnormalities in subtle cobalamin deficiency states, including deficiency without anemia and with normal absorption of free cobalamin. Arch Neurol. 1990;47(9):1008–12.
Hansen CS, Jensen JS, Ridderstråle M, Vistisen D, Jørgensen ME, Fleischer J. Vitamin B12 deficiency is associated with cardiovascular autonomic neuropathy in patients with type 2 diabetes. J Diabetes Compl. 2017;31(1):202–8.
Revicki DA, Rentz AM, Dubois D, Kahrilas P, Stanghellini V, Talley NJ, et al. Gastroparesis cardinal symptom index (GCSI): development and validation of a patient reported assessment of severity of gastroparesis symptoms. Qual Life Res. 2004;13(4):833–44.
Abell TL, Bernstein RK, Cutts T, Farrugia G, Forster J, Hasler WL, et al. Treatment of gastroparesis: a multidisciplinary clinical review. Neurogastroenterol Motil. 2006;18(4):263–83.
Kisozi T, Mutebi E, Kisekka M, Lhatoo S, Sajatovic M, Kaddumukasa M, et al. Prevalence, severity and factors associated with peripheral neuropathy among newly diagnosed diabetic patients attending Mulago hospital: a cross-sectional study. Afr Health Sci. 2017;17(2):463–73.
Meijer JW, Smit AJ, Sonderen EV, Groothoff JW, Eisma WH, Links TP. Symptom scoring systems to diagnose distal polyneuropathy in diabetes: the diabetic neuropathy symptom score. Diabet Med. 2002;19(11):962–5.
Umanath K, Lewis JB. Update on diabetic nephropathy: core curriculum 2018. Am J Kidney Dis. 2018;71(6):884–95.
Friedewald WT, Levy RT, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol without the use of preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502.
Fujimura J, Haruma K, Hata J, Yamanaka H, Sumii K, Kajiyama G. Quantitation of duodenogastric reflux and antral motility by color Doppler ultrasonography. Study in healthy volunteers and patients with gastric ulcer. Scand J Gastroenterol. 1994;29(10):897–902.
Abell TL, Camilleri M, Donohoe K, Hasler WL, Lin HC, Maurer AH, et al. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American neurogastroenterology and motility society and the society of nuclear medicine. Am J Gastroenterol. 2008;103(3):753–63.
Orthey P, Yu D, Van Natta ML, Ramsey FV, Diaz JR, Bennett PA, et al. Intragastric meal distribution during gastric emptying scintigraphy for assessment of fundic accommodation: correlation with symptoms of gastroparesis. J Nucl Med. 2018;59(4):691–7.
Irvine EJ, Tougas G, Lappalainen R, Bathurst NC. Reliability and interobserver variability of ultrasonographic measurement of gastric emptying rate. Dig Dis Sci. 1993;38(5):803–10.
Szarka LA, Camilleri M. Gastric emptying. Clin Gastroenterol Hepatol. 2009;7(8):823–7.
Muresan C, Surdea Blaga T, Muresan L, Dumitrascu DL. Abdominal ultrasound for the evaluation of gastric emptying revisited. J Gastrointestin Liver Dis. 2015;24(3):329–38.
Sogabe M, Okahisa T, Tsujigami K, Okita Y, Hayashi H, Taniki T, et al. Ultrasonographic assessment of gastric motility in diabetic gastroparesis before and after attaining glycemic control. J Gastroenterol. 2005;40(6):583–90.
Steinsvik EK, Sangnes DA, Søfteland E, Biermann M, Assmus J, Dimcevski G, et al. Gastric function in diabetic gastroparesis assessed by ultrasound and scintigraphy. Neurogastroenterol Motil. 2022;34(4): e14235.
Darwiche G, Mohammed SK, Aldawi N, Skaria S, Tesfa Y. Gastroparesis among type 1 and type 2 diabetic patients in the United Arab emirates. J Diabetes Mellitus. 2014;4(2):96–106.
Amjad W, Qureshi W, Singh RR, Richter S. Nutritional deficiencies and predictors of mortality in diabetic and nondiabetic gastroparesis. Ann Gastroenterol. 2021;34(6):788–95.
Hannibal L, Lysne V, Bjørke-Monsen AL, Behringer S, Grünert SC, Spiekerkoetter U, et al. Biomarkers and algorithms for the diagnosis of vitamin B12 deficiency. Front Mol Biosci. 2016;3:27.
Aparicio-Ugarriza R, Palacios G, Alder M, González-Gross M. A review of the cut-off points for the diagnosis of vitamin B12 deficiency in the general population. CCLM. 2015;53(8):1149–59.
Vidal-Alaball J, Butler C, Cannings-John R, Goringe A, Hood K, McCaddon A, et al. Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency. Cochrane Database Syst Rev. 2005;20(3):CD004655.
Surendran S, Adaikalakoteswari A, Saravanan P, Shatwaan IA, Lovegrove JA, Vimaleswaran KS. An update on vitamin B12-related gene polymorphisms and B12 status. Genes Nutr. 2018;13:2.
Ortiz-Guerrero G, Amador-Munoz D, Calderon-Ospina CA, LopezFuentes D, Nava Mesa MO. Proton pump inhibitors and dementia: physiopathological mechanisms and clinical consequences. Neural Plast. 2018;2018:5257285.
Kim J, Ahn CW, Fang S, Lee HS, Park JS. Association between metformin dose and vitamin B12 deficiency in patients with type 2 diabetes. Medicine. 2019;98(46): e17918.
Reynolds E. Vitamin B12, folic acid, and the nervous system. Lancet Neurol. 2006;5(11):949–60.
Calderon-Ospina CA, Nava-Mesa MO. B Vitamins in the nervous system: current knowledge of the biochemical modes of action and synergies of thiamine, pyridoxine, and cobalamin. CNS Neurosci Ther. 2020;26(1):5–13.
McCombe PA, McLeod JG. The peripheral neuropathy of vitamin B12 deficiency. J Neurol Sci. 1984;66(1):117–26.
Healton EB, Savage DG, Brust JC, Garrett TJ, Lindenbaum J. Neurologic aspects of cobalamin deficiency. Medicine. 1991;70(4):229–45.
Hakim M, Kurniani N, Pinzon RT, Tugasworo D, Basuki M, Haddani H, et al. Management of peripheral neuropathy symptoms with a fixed dose combination of high-dose vitamin B1, B6 and B12: a 12-week prospective non-interventional study in Indonesia. Asian J Med Sci. 2018;9(1):32–40.
Parkman HP, Wilson LA, Farrugia G, Koch KL, Hasler WL, Nguyen LA, Gastroparesis Clinical Research Consortium, et al. Delayed gastric emptying associates with diabetic complications in diabetic patients with symptoms of gastroparesis. Am J Gastroenterol. 2019;114(11):1778–94.
Almogbel RA, Alhussan FA, Alnasser SA, Algeffari MA. Prevalence and risk factors of gastroparesis-related symptoms among patients with type 2 diabetes. Int J Health Sci (Qassim). 2016;10(3):397–404.
Adar T, Lysy J. Pseudodyslipidemia: are we over-treating dyslipidemia in diabetic patients with undiagnosed gastroparesis? Endocrine. 2014;45(1):26–7.
Nervo M, Lubini A, Raimundo FV, Faulhaber GA, Leite C, Fischer LM, et al. Vitamin B12 in metformin-treated diabetic patients: a cross-sectional study in Brazil. Rev Assoc Med Bras. 2011;57(1):46–9.
de Groot-Kamphuis DM, van Dijk PR, Groenier KH, Houweling ST, Bilo HJ, Kleefstra N. Vitamin B12 deficiency and the lack of its consequences in type 2 diabetes patients using metformin. Neth J Med. 2013;71(7):386–90.
Ting RZ, Szeto CC, Chan MH, Ma KK, Chow KM. Risk factors of vitamin B (12) deficiency in patients receiving metformin. Arch Intern Med. 2006;166(18):1975–9.
Andres E, Noel E, Goichot B. Metformin-associated vitamin B12 deficiency. Arch Intern Med. 2002;162(19):2251–2.
Acknowledgements
The authors thank all sample donors for their contribution to this study and all members of the Endocrinology Unit, Specialized Medical Hospital, Mansoura, Egypt. This paper has not been published in any other peer-reviewed media or currently under review elsewhere.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research did not receive any specific Grant from any funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Contributions
SSA, HAA, ETE and MME wrote the manuscript text and prepared the figures, MM carried out the ultrasonography assessment, AAE carried out the laboratory studies. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in the study were in accordance with Mansoura university institution and the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study complies with current research ethics standards and was approved by the Institutional Research Ethics Board of the Faculty of Medicine, Mansoura University, Egypt (Approval No: MD.19.05.178). A written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ahmed, S.S., El-Hafez, H.A.A., Mohsen, M. et al. Is vitamin B12 deficiency a risk factor for gastroparesis in patients with type 2 diabetes?. Diabetol Metab Syndr 15, 33 (2023). https://doi.org/10.1186/s13098-023-01005-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-023-01005-0