Abstract
Background
The purpose of this study was to assess subclinical left ventricle (LV) myocardial dysfunction using global myocardial work (MW) in type 2 diabetes mellitus (T2DM) patients with preserved left ventricle ejection fraction (LVEF).
Methods
Sixty T2DM patients and 60 normal controls were enrolled in the study. Apical 4-, 3- and 2-chamber views were acquired by two-dimensional echocardiography. Peak systolic myocardial global longitudinal strain (GLS), global myocardial work index (GWI), global constructive work (GCW), global wasted work (GWW), and myocardial work efficiency (GWE) were determined by speckle-tracking echocardiography (STE).
Results
The GLS values in the T2DM patients were significantly lower than those in normal controls (p < 0.001). The GWW in T2DM patients was significantly greater than that in normal controls, while GWI, GCW and GWE was significantly lower (p < 0.001). Receiver operating characteristic (ROC) analysis showed there were no significant different difference between GWW, GWE and GLS in the area under the curves (AUCs). In T2DM patients, fasting plasma glucose was positively correlated with GWW but negatively correlated with GWE, and GLS was negatively correlated with GWI and GCW.
Conclusion
From the research, we found that global MW as new technique could detect the subclinical LV myocardial dysfunction and confirm that the impaired LV function in T2DM patients with preserved LV systolic function.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
The incidence of type 2 diabetes mellitus (T2DM) has increased worldwide in recent years. The development of coronary artery disease induced by T2DM has also increased. In the past few years, cardiovascular disease has become the major cause of morbidity and mortality for T2DM patients [1]. The pathological changes of diabetic-induced cardiomyopathy mainly include cardiomyocyte apoptosis, myocardial fibrosis and necrosis, ultimately leading to systolic and diastolic cardiac dysfunction and heart failure [2, 3]. Therefore, to protect cardiac function, early detection and intervention of the function of the left ventricle (LV) is essential to the prevention and management of diabetic cardiomyopathy.
Many techniques can be used to assess cardiac function, such as cardiovascular magnetic resonance T1 mapping [4], Tc-99 m MIBI gated single-photon emission-computed tomography myocardial perfusion imaging [5], tissue Doppler strain echocardiography [6], and two-dimensional speckle tracking echocardiography (2D-STE) [7, 8]. However, these techniques all have limitations. Like angle dependence in tissue Doppler strain echocardiography, long-term examination in cardiac magnetic resonance imaging and the radioactivity of cardiac radionuclide imaging, 2D-STE has a lower signal-to-noise ratio, weak acoustic windows, and through-plane motion artefacts [9, 10]. However, 2D-STE has become the leading reliable diagnostic technique for the assessment of cardiac function because of its noninvasiveness, convenience, and repeatability. In addition, our group previously reported that LV longitudinal myocardial function detected by longitudinal strain and rotation in T2DM patients with preserved LV ejection fraction (LVEF) was impaired when compared with that in healthy subjects [11]. However, global myocardial work (MW) is a new parameter for 2D-STE that takes into account deformation as well as afterload through interpretation of strain in relation to dynamic noninvasive LV pressure, potentially offering incremental value to myocardial function assessment.
The aim of the research was to explore the incremental value of global MW in the detection of subclinical LV myocardial dysfunction in T2DM patients with preserved LV systolic function.
Subjects and methods
Ethical statement
The study conducted according to the Principles of the Declaration of Helsinki and was approved by the human research and ethics committee of the affiliated Changzhou No. 2 people’s hospital with Nanjing Medical University. All of the patients had completed the informed consent forms.
Study population
Sixty T2DM patients (not well-treated, and it means poor blood glucose control in these T2DM patients before hospitalization) and 60 normal controls of similar age and sex were enrolled for this study and recruited from the hospital. The inclusion criteria for T2DM patients were clinically confirmed in accordance with the World Health Organization criteria [12] and without any history of heart disease (congenital heart disease, coronary artery disease, arterial hypertension, myocardial infarction, cardiomyopathy, valvular disease, atrial fibrillation, thyroid disease, neoplastic disease, or kidney failure), and also without obesity and dyslipidemia. All enrolled subjects were performed with coronary CT or coronary angiography to confirm that they have no coronary artery disease. All the T2DM patients had a LVEF > 55%. Normal controls were recruited from the physical examination in the hospital. In the normal controls, all of the physical and laboratory examination tests for cardiac function, electrocardiogram (ECG), and echocardiography were normal.
Anthropometric and biochemistry
The sex, age, height, body weight, heart rate (HR) and blood pressure (systolic blood pressure: SBP, diastolic blood pressure: DBP) of all subjects were recorded at the time of the echocardiography examination. Fasting plasma glucose, glycated haemoglobin (HbA1c), total cholesterol (TCH), triglyceride (TG), high density lipoprotein (HDL) and low density lipoprotein (LDL) were measured when the patients were in hospital.
Conventional 2D Doppler echocardiography
Patients underwent conventional 2D transthoracic Doppler echocardiography with a Vivid E9 equipped with an M5S 3.5–5 MHz transducer (GE Vingmed Ultrasound, Horten, Norway) by an experienced cardiologist. All of the patients were connected to ECG leads. Apical 4-chamber, 2-chamber, and long-axis views of three consecutive cycles with a standard high frame rate (> 45 s−1) were stored for offline analysis. The examination of echocardiography and the measurement of fasting plasma glucose, HbA1c, TCH, TG, HDL and LDL were performed in the same day.
Echocardiographic parameters of left atrial diameter (LAd), interventricular septum thickness (IVSd), LV posterior wall thickness (LVPWd) and LV diameter (LVDd) in the end-diastole period, the peak early (E) and late (A) diastolic mitral annular velocities, LV end-diastole volume (LVEDV), LV end-systole volume (LVESV) and LVEF (modified biplane Simpson's method), and the peak early (e′) and late (a′) diastolic annular velocities (obtained by averaging the values at the septum and lateral wall by tissue Doppler imaging: TDI) were measured during the examination.
Two-dimensional STE
Global longitudinal strain and MW were measured by EchoPAC software (EchoPAC Version: 203, GE Vingmed Ultrasound, Norway).
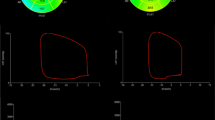
First, the aortic valve closure time was identified from the event timing of the aortic valve spectrum. Then, APLAX, A4C and A2C were used to analyse the apical long-axis, four-chamber and two-chamber views. The LV myocardium was divided into 18 segments, and the global longitudinal strain (GLS) was automatically measured by the software (Fig. 1A and B).
MW and related indices were calculated using a combination of echocardiographic strain data and a noninvasively estimated LV pressure curve. Blood pressure was input into the software, and “Advanced” was clicked. The software constructed a non-invasive LV pressure curve, then, MW and related indices were calculated using a combination of echocardiographic strain data and a noninvasively estimated LV pressure curve [13, 14]: (1) GWI: global myocardial work index, means the area within the global LV pressure-strain loop, calculated from mitral valve closure to mitral valve opening. (2) GCW: global constructive work, means work performed by the LV contributing to LV ejection during systole, estimated the work by the LV segments shortening during systole plus lengthening during isovolumic relaxation. (3) GWW: global wasted work, means work performed by the LV that does not contribute to LV ejection, estimated the work by the LV segments lengthening during systole plus shortening during the isovolumic relaxation phase. (4) GWE: myocardial work efficiency, GWE = GCW/(GCW + GWW) (Fig. 1 C–F).
Statistical analysis
All data analyses were performed using SPSS 25.0 software (SPSS, Chicago, IL, USA). The Shapiro–Wilk test or Kolmogorov–Smirnov test was used to detect the normality of all values. Differences between the T2DM patients and normal controls were compared with an independent Student′s t-test because the data distribution was normal. For variables with a nonnormal distribution, the nonparametric Mann–Whitney test was used. We defined GLS and global MW values in the normal controls as the normal state and considered the values of T2DM patients to be abnormal. These values in T2DM patients were determined from receiver operating characteristic (ROC) curve analysis by MedCalc software. Youden’s index was selected as the cut-off point that can give the best composite of specificity and sensitivity. Correlations among LVEF, fasting plasma glucose, HbA1c and GLS and global MW values were tested using Pearson or Spearman correlation tests as appropriate. The categorical variables are presented as frequencies and percentages. Data are presented as the mean ± standard deviation (SD) if normally distributed, and as medians and interquartile range boundaries otherwise. A p-value < 0.05 was considered significant in all tests.
Reproducibility and repeatability
Intraobserver and interobserver variability for GLS and global MW values were determined by repeating measurements in 25 patients randomly selected from among all enrolled patients.
Results
Patient characteristics
A total of 120 patients met the baseline inclusion criteria. Nineteen patients were excluded from the strain and MW analyses because of inadequate image quality (n = 12), tachycardia (n = 7) or irregular heartbeat (n = 3). A total of 98 patients were therefore evaluated in the study and were initially divided into two groups: normal controls (n = 50, mean age, 50.38 ± 15.27 years, 25 men) and T2DM patients (n = 48, mean age, 53.79 ± 11.24 years, 25 men).
Comparison of the patient characteristics and conventional echocardiographic parameters of normal controls and T2DM patients (Table 1)
The values of SBP, fasting plasma glucose and HbA1c were significantly higher in the T2DM patients than in normal controls (p < 0.05). There were no significant differences in age, BMI, HR, sex, DBP, TCH, TG, HDL and LDL between the normal controls and T2DM patients (P > 0.05).
The values of LAd, IVSd, LVPWd, a′ and E/e′ in the T2DM patients were significantly higher than those in normal controls (p < 0.05), however, the LVEF, E and e′ values in the T2DM patients were significantly lower than those in normal controls (p < 0.05). There were no significant differences in levels of LVDd, LVEDV, LVESV, A or E/A between the normal controls and T2DM patients (p > 0.05).
LV GLS and global MW in normal controls and T2DM patients (Table 2 and Fig. 2)
The values of LV GLS in T2DM patients were significantly lower than those in normal controls (p < 0.001). The GWW value was significantly higher in T2DM patients than in normal controls, however, the GWI, GCW and GWE value was significantly lower in T2DM patients than in normal controls (p < 0.001).
ROC analysis (Table 3 and Fig. 3)
ROC curve analysis was used to discriminate whether global MW parameters and GLS were able to predict subclinical LV myocardial dysfunction in T2DM patients. According to the ROC analysis, the area under the curve (AUC) of GLS was 0.840, the cut-off value was − 21.1%, with a sensitivity of 75% and specificity of 80%. The AUC of GWI was 0.689, the cut-off value was 2024 mmHg%, with a sensitivity of 50% and specificity of 82%. The AUC of GCW was 0.683, the cut-off value was 2467 mmHg%, with a sensitivity of 58% and specificity of 74%. The AUC of GWW was 0.734, the cut-off value was 46 mmHg%, with a sensitivity of 96% and specificity of 46%, and the AUC of GWE was 0.784, the cut-off value was 97%, with a sensitivity of 94% and specificity of 54%. The comparation of AUCs showed that there was no significant difference between GWW, GWE and GLS (p > 0.05).
Correlation tests among LVEF, fasting plasma glucose, HbA1c, GLS and MW in T2DM patients (Table 4 and Figs. 4 and 5)
In T2DM patients, fasting plasma glucose was positively correlated with GWW but negatively correlated with GWE. GLS was negatively correlated with GWI and GCW.
Intra- and interobserver variability (Table 5)
Intra- and interobserver variabilities were assessed via the intraclass correlation coefficients (ICCs) for the measurements. GLS and global MW parameters showed excellent intra- and interobserver correlations, with ICC values > 0.85.
Discussion
The main finding of the study was that subclinical LV myocardial dysfunction was detected by global MW in T2DM patients with preserved LV systolic function.
Cardiac impairment by T2DM includes microvascular impairment, metabolic disturbance, subcellular component abnormalities, cardiac autonomic dysfunction, and a maladaptive immune response. Eventually, functional and structural changes in myocardium without coronary artery disease are caused by T2DM, and this is called diabetic cardiomyopathy [15]. Diabetic cardiomyopathy may first induce diastolic dysfunction and then systolic dysfunction. Finally, clinical heart failure may occur. With the development of imaging examinations, the detection of cardiac function has become increasingly easy. Echocardiography for measuring MW is considered the newest tool for the assessment of LV systolic dysfunction. Billig et al. [16] evaluated left and right ventricular structure, function and myocardial work by transoesophageal echocardiography (TEE) in swine and found that myocardial contractility and mechanics could be reliably evaluated with noninvasive GWI derived from echocardiography without additional invasive measures. Galli et al. [17] provided reference values for GWI, GCW, GWW and GWE in a group of healthy volunteers controlling for age and sex and found that assessment of MW was feasible in normal subjects. The presented referral ranges of GWI, GCW, GWW and GWE were not affected by age. According to previous studies, MW has been reported in many diseases, including coronary heart disease [14], hypertension, cardiac resynchronization therapy (CRT), percutaneous coronary intervention (PCI) [18], aortic stenosis [19], transcatheter aortic valve replacement (TAVR) [20], dilated cardiomyopathy [21], hypertrophic cardiomyopathy [22], chronic kidney disease [23], and cardiac amyloidosis [24]. However, there has been little research about LV systolic function in T2DM patients with MW.
Liu et al. [25] examined the prognostic value of GLS in T2DM patients and found that in T2DM patients without any history of cardiovascular disease, impaired GLS was associated with cardiovascular events. Our research was consistent with this research, and we found that LV GLS was decreased in the T2DM patients compared with normal controls. MW analysis showed that the GWW value was significantly higher in T2DM patients than in normal controls and that the GWI, GCW and GWE value was significantly lower in T2DM patients than in normal controls. The results may indicate that subclinical LV myocardial dysfunction was present in T2DM patients, although LV systolic function was normal. We considered that the results were related to the pathological changes of the LV myocardium in T2DM. In T2DM, persistent hyperglycaemia causes molecular and metabolic changes in cardiomyocytes and damages the coronary microvasculature. Hypoxia of cardiomyocytes and ischaemia results in myocardial hypertrophy, perivascular and fibrosis, LV stiffness, and systolic and diastole dysfunction in T2DM [15]. Normal myocardial fibres consist of longitudinal and circumferential myocardial fibres. Almost 70% of the myocardial fibre is longitudinal, and 30% is circumferential. If cardiomyocyte apoptosis, myocardial fibrosis and necrosis occur in T2DM, the sequence of the myocardium may change, eventually leading to damage to myocardial systolic function.
ROC analysis showed that GWW and GWE had the same diagnostic efficacy with GLS. The results may indicate global MW can evaluate the subclinical LV dysfunction in T2DM patients accurately.
In T2DM patients, fasting plasma glucose was positively correlated with GWW but negatively correlated with GWE, and GLS was negatively correlated with GWI and GCW. However, the correlations were not strong (0.3–0.6) and they could not accurately predict the subclinical LV myocardial dysfunction in T2DM patients.
Conclusion
From the research, we found that global MW as new technique could detect the subclinical LV myocardial dysfunction and confirm that the impaired LV function in T2DM patients with preserved LV systolic function.
Limitations
First, the number of enrolled subjects in this study was small and it is also a single center study, in the future research, we will expand the sample size to makes the research more reliable. Second, 2D-STE has the shortcoming of the speckle “out of plane motion”, if the speckles move out of plane during contraction, the software cannot be tracked successfully. Third, patients with COPD were insufficient and excluded for the analysis.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- LV:
-
Left ventricle
- LVEF:
-
Left ventricle ejection fraction
- T2DM:
-
Type 2 diabetes mellitus
- GLS:
-
Global longitudinal strain
- MW:
-
Myocardial work
- PSL:
-
Pressure-strain loops
- GMW:
-
Global myocardial work
- GWI:
-
Global myocardial work index
- GCW:
-
Global constructive work
- GWW:
-
Global wasted work
- GWE:
-
Myocardial work efficiency
- STE:
-
Speckle-tracking echocardiography
- TDI:
-
Tissue Doppler imaging
- HR:
-
Heart rate
- BMI:
-
Body mass index
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- TCH:
-
Total cholesterol
- TG:
-
Triglyceride
- HDL:
-
High density lipoprotein
- LDL:
-
Low density lipoprotein
- LAD:
-
Left atrial diameter
- IVSd:
-
Interventricular septal thickness in end-diastolic period
- LVPWd:
-
Left ventricular posterior wall thickness in end-diastolic period. LVDd: LV diameter in end-diastole period
- LVEDV:
-
Left ventricular end-diastolic volume
- LVESV:
-
Left ventricular end-systolic volume
- HbA1c:
-
Glycated haemoglobin
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- ICCs:
-
Intraclass correlation coefficients
- CRT:
-
Cardiac resynchronization therapy
- PCI:
-
Percutaneous coronary intervention
- TAVR:
-
Transcatheter aortic valve replacement
References
Low Wang CC, Hess CN, Hiatt WR, Goldfine AB. Clinical update: cardiovascular disease in diabetes mellitus: atherosclerotic cardiovascular disease and heart failure in type 2 diabetes mellitus—mechanisms, management, and clinical considerations. Circulation. 2016;133:2459–502.
Bugger H, Abel ED. Molecular mechanisms of diabetic cardiomyopathy. Diabetologia. 2014;57:660–71.
Aneja A, Tang WH, Bansilal S, Garcia MJ, Farkouh ME. Diabetic cardiomyopathy: insights into pathogenesis, diagnostic challenges, and therapeutic options. Am J Med. 2008;121:748–57.
Cao Y, Zeng W, Cui Y, Kong X, Wang M, Yu J, et al. Increased myocardial extracellular volume assessed by cardiovascular magnetic resonance T1 mapping and its determinants in type 2 diabetes mellitus patients with normal myocardial systolic strain. Cardiovasc Diabetol. 2018;17:7.
Deepti S, Roy A, Patel CD, Tandon N, Naik N, Singh S, et al. Assessment of asymptomatic ischemic heart disease using stress myocardial perfusion imaging in patients with type 2 diabetes mellitus. Indian Heart J. 2018;70(Suppl 3):S157–60.
Galderisi M, de Simone G, Innelli P, Turco A, Turco S, Capaldo B, et al. Impaired inotropic response in type 2 diabetes mellitus: a strain rate imaging study. Am J Hypertens. 2007;20:548–55.
Ernande L, Bergerot C, Girerd N, Thibault H, Davidsen ES, Gautier Pignon-Blanc P, et al. Longitudinal myocardial strain alteration is associated with left ventricular remodeling in asymptomatic patients with type 2 diabetes mellitus. J Am Soc Echocardiogr. 2014;27:479–88.
Ng AC, Delgado V, Bertini M, van der Meer RW, Rijzewijk LJ, Hooi Ewe S, et al. Myocardial steatosis and biventricular strain and strain rate imaging in patients with type 2 diabetes mellitus. Circulation. 2010;122:2538–44.
Pedrizzetti G, Claus P, Kilner PJ, Nagel E. Principles of cardiovascular magnetic resonance feature tracking and echocardiographic speckle tracking for informed clinical use. J Cardiovasc Magn Reson. 2016;18:51.
Scatteia A, Baritussio A, Bucciarelli-Ducci C. Strain imaging using cardiac magnetic resonance. Heart Fail Rev. 2017;22:465–76.
Huang J, Hu HL, Yan ZN, Fan L, Rui YF, Shen D, et al. Peak systolic longitudinal rotation: a new tool for detecting left ventricular systolic function in patients with type 2 diabetes mellitus by two-dimensional speckle tracking echocardiography. BMC Cardiovasc Disord. 2019;19:137.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–53.
Chan J, Edwards NFA, Khandheria BK, Shiino K, Sabapathy S, Anderson B, et al. A new approach to assess myocardial work by non-invasive left ventricular pressure-strain relations in hypertension and dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2019;20:31–9.
Edwards NFA, Scalia GM, Shiino K, Sabapathy S, Anderson B, Chamberlain R, et al. Global myocardial work is superior to global longitudinal strain to predict significant coronary artery disease in patients with normal left ventricular function and wall motion. J Am Soc Echocardiogr. 2019;32:947–57.
Lee WS, Kim J. Diabetic cardiomyopathy: where we are and where we are going. Korean J Intern Med. 2017;32:404–21.
Billig S, Zayat R, Ebeling A, Steffen H, Nix C, Hatam N, et al. Transesophageal echocardiography in swine: evaluation of left and right ventricular structure, function and myocardial work. Int J Cardiovasc Imaging. 2020. https://doi.org/10.1007/s10554-020-02053-7.
Galli E, John-Matthwes B, Rousseau C, Schnell F, Leclercq C, Donal E. Echocardiographic reference ranges for myocardial work in healthy subjects: a preliminary study. Echocardiography. 2019;36:1814–24.
Meimoun P, Abdani S, Stracchi V, Elmkies F, Boulanger J, Botoro T, et al. Usefulness of noninvasive myocardial work to predict left ventricular recovery and acute complications after acute anterior myocardial infarction treated by percutaneous coronary intervention. J Am Soc Echocardiogr. 2020;33:1180–90.
Fortuni F, Butcher SC, van der Kley F, Lustosa RP, Karalis I, de Weger A, et al. Left ventricular myocardial work in patients with severe aortic stenosis. J Am Soc Echocardiogr. 2020. https://doi.org/10.1016/j.echo.2020.10.014.
Jain R, Bajwa T, Roemer S, Huisheree H, Allaqaband SQ, Kroboth S, et al. Myocardial work assessment in severe aortic stenosis undergoing transcatheter aortic valve replacement. Eur Heart J Cardiovasc Imaging. 2020. https://doi.org/10.1093/ehjci/jeaa257.
Cui C, Liu L, Li Y, Liu Y, Huang D, Hu Y, et al. Left ventricular pressure-strain loop-based quantitative examination of the global and regional myocardial work of patients with dilated cardiomyopathy. Ultrasound Med Biol. 2020;46:2834–45.
Hiemstra YL, van der Bijl P, El Mahdiui M, Bax JJ, Delgado V, Marsan NA. Myocardial work in nonobstructive hypertrophic cardiomyopathy: implications for outcome. J Am Soc Echocardiogr. 2020;33:1201–8.
Ke QQ, Xu HB, Bai J, Xiong L, Li MM. Evaluation of global and regional left ventricular myocardial work by echocardiography in patients with chronic kidney disease. Echocardiography. 2020. https://doi.org/10.1111/echo.14864.
Clemmensen TS, Eiskjaer H, Ladefoged B, Mikkelsen F, Sorensen J, Granstam SO, et al. Prognostic implications of left ventricular myocardial work indices in cardiac amyloidosis. Eur Heart J Cardiovasc Imaging. 2020. https://doi.org/10.1093/ehjci/jeaa097.
Liu JH, Chen Y, Yuen M, Zhen Z, Chan CW, Lam KS, et al. Incremental prognostic value of global longitudinal strain in patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2016;15:22.
Acknowledgements
We would like to thank the department of Echocardiography and radiology, the Affiliated Changzhou No. 2 People’s Hospital with Nanjing Medical University.
Funding
This study was funded by Young Talent Development Plan of Changzhou Health Commission (No.: CZQM2020061), Talent Development Plan of Changzhou No. 2 People’s hospital (No.: YJRC202031) and Changzhou Science and Technique Program (Grant No.: CJ20190098).
Author information
Authors and Affiliations
Contributions
JH and TW designed the study and carried out the study, data collection and analysis, TW wrote the manuscript and JH revised the manuscript. LF designed part of the experiments, and collected the T2DM patients and normal controls. LL performed the statistical analysis. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study complied with the Declaration of Helsinki and was reviewed and approved by the Human Subjects Committee of Changzhou No. 2 People’s Hospital. Written informed consent was obtained from each couple enrolled in the study.
Consent to publication
This manuscript does not include any individual person’s data.
Competing interests
The authors declared no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, T., Li, L., Huang, J. et al. Assessment of subclinical left ventricle myocardial dysfunction using global myocardial work in type 2 diabetes mellitus patients with preserved left ventricle ejection fraction. Diabetol Metab Syndr 14, 17 (2022). https://doi.org/10.1186/s13098-021-00781-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-021-00781-x