Abstract
Background
Osteoprotegerin (OPG), a soluble member of the tumor necrosis factor receptor superfamily that inhibits bone resorption, has been suggested as a potential marker of cardiovascular risk. This study aimed to assess the relationship between insulin resistance, lipid profile and OPG levels in obese and non-obese sub-Saharan African women.
Methods
Sixty obese (44) and non-obese (16) volunteer women aged 18 to 40 years were recruited in this cross-sectional study. Their clinical (age, height, weight, waist circumference, systolic and diastolic blood pressures) and biochemical parameters (fasting blood glucose, total cholesterol, high density lipoprotein-cholesterol (HDL-C)) were measured using standard methods. Insulin levels were measured using an electrochemiluminescence immunoassay, while OPG levels were measured using the ELISA technique. Low density lipoprotein-cholesterol (LDL-C), body mass index (BMI) and Homeostasis Model Assessment of Insulin Resistance (HOMA-IR) were calculated using standard methods. Abdominal obesity was defined as a waist circumference ≥ 80 cm.
Results
OPG levels were higher in obese than in normal subjects, though the difference was not significant (p = 0.9). BMI, waist circumference, percent body fat and systolic blood pressure were significantly higher in obese than in non-obese subjects (p < 0.05). In these subjects, only age significantly correlated with OPG levels (r = 0.831, p = 0.003), while none of the anthropometric nor metabolic parameter did, even after adjustment for age. In obese subjects, OPG levels fairly correlated with HDL-C (r = 0.298, p = 0.058), and significantly correlated with HOMA-IR (r = −0.438, p = 0.018). After adjustment for age, OPG levels remained negatively correlated to HOMA-IR (r = −0.516, p = 0.020) and LDL-C (r = −0.535, p = 0.015) and positively correlated to HDL-C (r = 0.615, p = 0.004). In multiple linear regression analysis, age was a main determinant of OPG levels in non-obese (β = 0.647, p = 0.006) and obese (β = 0.356, p = 0.044) women. HDL-C was also associated to OPG levels in obese women (β = 0.535, p = 0.009).
Conclusion
The positive correlation of OPG with HDL-C and HOMA-IR, and its negative correlation with LDL-C suggest that it may be a marker of insulin sensitivity/resistance and atherogenic risk in obese African women.
Similar content being viewed by others
Background
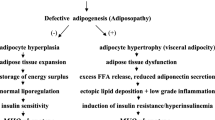
Osteoprotegerin (OPG) is a soluble glycoprotein that belongs to the tumor necrosis factor receptor super-family [1]. It acts as a decoy soluble receptor for the receptor activator of nuclear factor kB ligand (RANKL) [2], thus preventing RANKL from binding its receptor on osteoclasts, thereby inhibiting osteoclastogenesis [3]. Some studies showed that OPG may modulate vascular calcification, endothelial dysfunction and left ventricular dysfunction [4–7]. OPG was also found associated to ischemic heart disease, stroke and all-cause mortality in patients with heart failure [4, 8–10]. Furthermore, a relation between OPG and insulin sensitivity was seen in an ageing male population, and in obese and non-obese individuals [11, 12]. There is therefore a need to further investigate the potential of OPG as a marker of cardiovascular risk in diverse ethnic populations. This study aimed to assess the relationship between insulin resistance, lipid profile and OPG levels in obese and non-obese sub-Saharan African women.
Methods
This was a cross-sectional study. Sixty women aged 18 to 40 years, of which 44 obese and 16 non obese were recruited within the general population of Edéa, Cameroon. For each participant we measured height, waist circumference to the nearest 0.5 cm, and weight in light clothes to the nearest 0.1 kg, and we then calculated the body mass index (BMI) as weight in kg/height2 in m2. We measured resting blood pressures using standardized procedures with an automatic sphygmomanometer Omron HEM-705 CP (Omron Corporation, Tokyo, Japan). Fasting blood glucose was obtained with the Accu-Chek® Compact Plus glucometer (F. Hoffmann-La Roche AG, Basel, Switzerland). Serum cholesterol (cholesterol oxidase phenol4-amino antipyrene peroxidase method), serum triglycerides (glycerol phosphatase oxidase-phenol4-amino antipyrene peroxidase method), and high-density lipoprotein (HDL)-cholesterol (cholesterol oxidase phenol4-amino antipyrene peroxidase method) were measured on a spectrophotometer (UV Mini 1240) using Chronolab kits (Chronolab Systems, Barcelona, Spain). Low-density lipoprotein (LDL)-cholesterol was calculated using the Friedwald’s formula [13]. Insulin levels were measured using an electrochemiluminescence immunoassay (Roche Diagnostics, Indianapolis, USA), while OPG levels were measured using Osteoprotegerin ELISA kit (Immunodiagnostic systems, Fontain Hill, USA). Homeostasis Model Assessment of Insulin Resistance (HOMA-IR) calculated as HOMA ‐ IR = (Fasting insulin × Fasting blood glucose) ÷ 22.5. Abdominal obesity was defined as a waist circumference ≥ 80 cm.
Data were coded, entered and analyzed using the Statistical Package for Social Science (SPSS) version 20.0 for Windows (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.). Variables were expressed as mean with standard deviation (SD). The Student t-test was used to compare the obese and non-obese groups with respect to clinical and biological parameters. Pearson’s correlation and partial correlation were used to determine unadjusted and adjusted correlates of OPG levels in obese women. Multiple stepwise linear regression analyses were performed to determine the metabolic correlates of OPG levels in obese and non-obese women. A p value < 0.05 was considered statistically significant.
The study was approved by the National Ethical Review Board of the Cameroon Ministry of Public Health. Written informed consent was obtained from all the participants. The study was conducted in accordance with the Helsinki Declaration.
Results
Sixty women (44 obese and 16 non-obese) were recruited. Obese women were significantly older than non-obese (mean age: 31.86 ± 5.23 vs 27.44 ± 6.07; p = 0.012). BMI, waist circumference, systolic blood pressure and percent body fat levels were significantly higher in obese than in non-obese subjects (p<0.05). OPG levels were comparable among both groups (Table 1).
In non-obese subjects, only age significantly correlated with OPG levels (r = 0.831, p = 0.003), while none of the anthropometric nor metabolic parameters did, even after adjustment for age. As shown in Table 2, in obese subjects, OPG levels were almost correlated with HDL-C (r = 0.298, p = 0.058), and were significantly correlated with HOMA-IR (r = −0.438, p = 0.018). After adjustment for age, OPG levels remained negatively correlated to HOMA-IR (r = −0.516, p = 0.020) and LDL-C (r = −0.535, p = 0.015) and positively correlated to HDL-C (r = 0.615, p = 0.004).
In multiple stepwise regression analysis (Table 3), age was a main determinant of OPG levels in non-obese (β =0.647, p = 0.006) and obese (β =0.356, p = 0.044) women. HDL-C was also associated to OPG levels in obese women (β = 0.535, p = 0.009).
Discussion
The aim of this study was to assess the relationship between insulin resistance, lipid profile and OPG levels in obese and non-obese sub-Saharan African women. Age significantly correlated with OPG levels in both groups. After adjustment for age, only HDL-C levels, LDL-C levels, and HOMA-IR correlated with OPG levels in obese, but not non-obese women.
OPG levels have been associated with a high risk of cardiovascular disease in humans [14, 15]. This result has long been a matter of controversy in the literature, possibly because of different sizes of the study populations and of different methodologies [4]. Even in our previous study carried out on an older population made up of both sexes, HDL-C levels did not correlate with OPG levels [16]. Some observational studies showed an association between elevated serum OPG levels and clinical cardiovascular disease [11, 12, 17, 18]. Unlike these studies, we found that HDL-C which has a protective effect on heart and vessels in humans [19], was positively correlated with OPG levels. Additionally, LDL-C which carries a proatherogenic profile was negatively correlated to OPG. These findings are consistent with evidence from many animals studies that found a protective role for OPG on the vasculature [20].
We found that HOMA-IR was negatively correlated with OPG levels in obese women, indicating that elevated OPG levels may be suggestive of high insulin sensitivity. Contrariwise, in a study among Caucasian obese, HOMA-IR was positively correlated to OPG levels [10]. Although our findings along with those of previous studies suggest that serum OPG may be a marker of insulin sensitivity/resistance in obese individuals [10, 12], whether elevated serum OPG levels reflect insulin sensitivity or resistance in this particular population remains controversial. Differences in ethnic background, metabolic conditions and diagnostic criteria of insulin sensitivity using HOMA-IR in the populations studied may partly explain this inconsistency. Indeed, it has been shown that cut-off values of HOMA-IR are defined by population-based percentiles criteria. Furthermore, these cut-off values are different according to ethnicity, clinical methods of estimation, and metabolic conditions of populations studied [21]. To the best of our knowledge, there is no reference values for HOMA-IR that have been validated in our population. However, we conducted a study that showed that the performance of fasting insulin sensitivity indices in predicting insulin sensitivity among Black Africans are not optimal [22]. Overall, discrepancy between our results and some previous reports in Caucasians regarding the relationship between OPG levels and lipid profile and HOMA-IR [10, 12] stresses the need for further investigation with an emphasis on ethnic differences.
The main limitation of this study is its small sample size which hampered definitive inferences and drawing relevant conclusions. Thus, our findings need to be verified in further large population studies.
Conclusion
The positive correlation of OPG with HDL-C and HOMA-IR, and its negative correlation with LDL-C suggest that it maybe a marker of insulin sensitivity/resistance and atherogenic risk in obese African women. Further large studies are needed to verify these findings.
References
Hofbauer LC, Heufelder AE. Clinical review 114: hot topic. The role of receptor activator of nuclear factor-kappaB ligand and osteoprotegerin in the pathogenesis and treatment of metabolic bone diseases. J Clin Endocrinol Metab. 2000;85:2355–63.
Lacey DL, Timms E, Tan HL, Kelley MJ, Dunstan CR, Burgess T, et al. Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell. 1998;1998(93):165–76.
Kwon BS, Wang S, Udagawa N, Haridas V, Lee ZH, Kim KK, et al. TR1, a new member of the tumor necrosis factor receptor superfamily, induces fibroblast proliferation and inhibits osteoclastogenesis and bone resorption. FASEB J. 1998;12:845–54.
Morony S, Tintut Y, Zhang Z, Cattley RC, Van G, Dwyer D, et al. Osteoprotegerin inhibits vascular calcification without affecting atherosclerosis in ldlr(−/−) mice. Circulation. 2008;117(3):411–20.
Moldovan D, Kacso IM, Rusu C, Potra A, Bondor CI, Moldovan I, et al. Role of osteoprotegerin in vascular disorders of the end-stage renal disease patients. Biomarkers. 2015;15:1–7.
Delgado-Frías E, López-Mejias R, Genre F, Ubilla B, Gómez Rodríguez-Bethencourt MA, González-Díaz A, et al. Relationship between endothelial dysfunction and osteoprotegerin, Vitamin D, and bone mineral density in patients with rheumatoid arthritis. Clin Exp Rheumatol. 2015. [Epub ahead of print].
Kalaycıoğlu E, Gökdeniz T, Aykan AÇ, Hatem E, Gürsoy MO, Ören A, et al. Osteoprotegerin is associated with subclinical left ventricular systolic dysfunction in diabetic hypertensive patients: a speckle tracking study. Can J Cardiol. 2014;30(12):1529–34.
Ueland T, Dahl CP, Kjekshus J, Hulthe J, Böhm M, Mach F, et al. Osteoprotegerin predicts progression of chronic heart failure: results from CORONA. Circulation. 2011;4(2):145–52.
Aramburu-Bodas O, García-Casado B, Salamanca-Bautista P, Guisado-Espartero ME, Arias-Jiménez JL, Barco-Sánchez A, et al. Relationship between osteoprotegerin and mortality in decompensated heart failure with preserved ejection fraction. J Cardiovasc Med (Hagerstown). 2014. [Epub ahead of print].
Gannage-Yared MH, Yaghi C, Habre B, Khalife S, Noun R, Germanos-Haddad M, et al. Osteoprotegerin in relation to body weight, lipid parameters insulin sensitivity, adipocytokines, and C-reactive protein in obese and non-obese young individuals: results from both cross-sectional and interventional study. Eur J Endocrinol. 2008;158(3):353–9.
López-Mejias R, Ubilla B, Genre F, Corrales A, Hernández JL, Ferraz-Amaro I, et al. Osteoprotegerin concentrations relate independently to established cardiovascular disease in rheumatoid arthritis. J Rheumatol. 2015;42(1):39–45.
Gannage-Yared MH, Fares F, Semaan M, Khalife S, Jambart S. Circulating osteoprotegerin is correlated with lipid profile, insulin sensitivity, adiponectin and sex steroids in an ageing male population. Clin Endocrinol (Oxf). 2006;64:652–8.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Bjerre M. Osteoprotegerin (OPG) as a biomarker for diabetic cardiovascular complications. Springerplus. 2013;2:658.
Park JS, Cho MH, Ji NS, Yoo JS, Ahn CVV, Cha BS, et al. Effect of pioglitazone on serum concentrations of osteoprotegerin in patients with type 2 diabetes mellitus. Eur J Endocrinol. 2011;164:69–74.
Ayina Ayina CN, Boudou P, Fidaa I, Balti EV, Sobngwi E, Etoundi Ngoa LS, et al. Osteoprotegerin is not a determinant of Metabolic syndrom in sub-Saharan Africans after age-adjustment. Ann Endocrinol (Paris). 2014;75(3):165–70.
Van Campenhout A, Golledge J. Osteoprotegerin, vascular calcification and atherosclerosis. Atherosclerosis. 2009;204(2):321–9.
Kiechl S, Werner P, Knoflach M, Furtner M, Willeit J, Schett G. The osteoprotegerin/RANK/RANKL system: a bone key to vascular disease. Expert Rev Cardiovasc Ther. 2006;4:801–11.
Gotto Jr AM. Jeremiah Metzger Lecture: cholesterol, inflammation and atherosclerotic cardiovascular disease: is it all LDL? Trans Am Clin Clim Assoc. 2011;122:256–89.
Bennett BJ, Scatena M, Kirk EA, Rattazzi M, Varon RM, Averill M, et al. Osteoprotegerin inactivation accelerates advanced atherosclerotic lesion progression and calcification in older ApoE−/− mice. Arterioscler Thromb Vasc Biol. 2006;26:2117–24.
Antuna-Puente B, Disse E, Rabasa-Lhoret R, Laville M, Capeau J, Bastard JP. How can we measure insulin sensitivity/resistance? Diabetes Metab. 2011;37:179–88.
Sobngwi E, Kengne AP, Echouffo-Tcheugui JB, Choukem S, Sobngwi-Tambekou J, Balti EV, et al. Fasting insulin sensitivity indices are not better than routine clinical variables at predicting insulin sensitivity among Black Africans: a clamp study in sub-Saharan Africans. BMC Endocr Disord. 2014;14:65.
Acknowledgements
We are grateful to all the patients and volunteers who participated in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interest
The authors declare that they have no competing interest.
Authors’ contributions
Study conception and design: CNAA, ES, PB, LSEN, JFG. Data collection: CNAA, ES. Statistical analysis and interpretation: CNAA, ES. Drafting: CNAA, ME, JJNN. Critical discussion and manuscript revision: CNAA, ME, JJNN, ES, PB, LSEN, JFG. All authors read and approved the final version of the manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ayina Ayina, C.N., Sobngwi, E., Essouma, M. et al. Osteoprotegerin in relation to insulin resistance and blood lipids in sub-Saharan African women with and without abdominal obesity. Diabetol Metab Syndr 7, 47 (2015). https://doi.org/10.1186/s13098-015-0042-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-015-0042-3