Abstract
Background
The genus Bartonella includes fastidious, facultative intracellular bacteria mainly transmitted by arthropods and distributed among mammalian reservoirs. Bartonella spp. implicated as etiological agents of zoonoses are increasing. Apart from the classical Bartonella henselae, B. bacilliformis or B. quintana, other species (B. elizabethae, B. rochalimae, B. vinsonii arupensis and B. v. berkhoffii, B. tamiae or B. koehlerae, among others) have also been associated with human and/or animal diseases. Laboratory techniques for diagnosis (culture, PCR assays and serology) usually show lack of sensitivity. Since 2005, a method based on a liquid enrichment Bartonella alphaproteobacteria growth medium (BAPGM) followed by PCRs for the amplification of Bartonella spp. has been developed. We aimed to assess culture, molecular and serological prevalence of Bartonella infections in companion animal veterinary personnel from Spain.
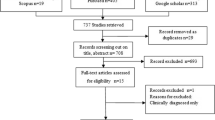
Methods
Each of 89 participants completed a questionnaire. Immunofluorescence assays (IFA) using B. vinsonii berkhoffii (genotypes I, II and III), B. henselae, B. quintana and B. koehlerae as antigens were performed. A cut-off of 1:64 was selected as a seroreactivity titer. Blood samples were inoculated into BAPGM and subcultured onto blood agar plates. Bartonella spp. was detected using conventional and quantitative real-time PCR assays and DNA sequencing.
Results
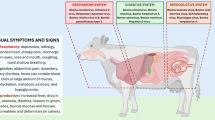
Among antigens corresponding to six Bartonella spp. or genotypes, the lowest seroreactivity was found against B. quintana (11.2%) and the highest, against B. v. berkhoffii genotype III (56%). A total of 27% of 89 individuals were not seroreactive to any test antigen. Bartonella spp. IFA seroreactivity was not associated with any clinical sign or symptom. DNA from Bartonella spp., including B. henselae (n = 2), B. v. berkhoffii genotypes I (n = 1) and III (n = 2), and B. quintana (n = 2) was detected in 7/89 veterinary personnel. PCR and DNA sequencing findings were not associated with clinical signs or symptoms. No co-infections were observed. One of the two B. henselae PCR-positive individuals was IFA seronegative to all tested antigens whereas the other one was not B. henselae seroreactive. The remaining PCR-positive individuals were seroreactive to multiple Bartonella spp. antigens.
Conclusions
High serological and molecular prevalences of exposure to, or infection with, Bartonella spp. were found in companion animal veterinary personnel from Spain. More studies using BAPGM enrichment blood culture and PCR are needed to clarify the finding of Bartonella PCR-positive individuals lacking clinical symptoms.
Similar content being viewed by others
Background
Bartonella spp. are fastidious, facultative intracellular, pleomorphic Gram-negative bacilli included in the class Alphaproteobacteria with at least 35 validated species and three subspecies (http://www.bacterio.net/bartonella.html). A wide range of animals are hosts and reservoirs of Bartonella spp., mainly transmitted by feces of fleas and lice, and bites of sand flies and potentially ticks [1].
Although not yet demonstrated, all Bartonella species and subspecies should be considered potentially zoonotic. An increasing number of Bartonella spp. has been associated with an expanding clinical spectrum in humans and animals [1,2,3]. Some species, such as Bartonella bacilliformis (Oroya fever, Verruga Peruana or Carrión’s disease) are confined to the highlands of Peru, Colombia and Ecuador, as the Lutzomyia sand fly vector is geographically limited. Bartonella quintana, responsible for trench fever during the first and second World Wars, has reemerged in homeless and alcoholic people with poor hygiene (e.g. refugee camps). B. quintana is also a known cause of bacillary angiomatosis and peliosis hepatis in HIV patients, chronic lymphadenopathy in immunocompromised or immunocompetent patients, and blood culture negative (BCN) endocarditis [1].
In 1992, a new bacterium, Bartonella henselae, the main agent of cat scratch disease (CSD) was described [4]. Subsequently, B. henselae has become the most representative species of the genus and the one most frequently reported as a human or animal pathogen [1]. Bartonella henselae is one of the main causes of subacute and chronic lymphadenopathy in children and young people, and also causes other severe infections such as endocarditis, hepatosplenic abscesses, retinopathy, uveitis, peliosis hepatis and bacillary angiomatosis, among others [5]. Other Bartonella spp. such as B. elizabethae, B. vinsonii (subsp. berkhoffii and subsp. arupensis), B. koehlerae and B. alsatica have been implicated in endocarditis cases; B. rochalimae has been associated with fever and bacteremia; B. tamiae, with febrile illness; and B. grahamii, with neuroretinitis [1, 6]. For all these reasons, Bartonella infections are considered emerging and re-emerging infections in humans.
Although Bartonella spp. can grow in axenic media, the sensitivity of culture is usually very low. In recent decades molecular tools have been used diagnostically in clinical practice to test certain samples such as adenopathies or cardiac valves for fastidious organisms. However, these techniques are not routinely available, and serological tests are usually the diagnostic modality offered by microbiological laboratories, although cross reactivity between Bartonella spp. may occur [7]. Since 2005, a new method for the diagnosis of Bartonella infections has been used for the study of animal and human diagnostic specimens. It is based on an enrichment growth medium for Bartonella culture that improves the yield of Bartonella spp. detection by subsequent molecular biology techniques (PCR and DNA sequencing), and it is called the Bartonella alpha-proteobacteria growth medium (BAPGM) enrichment blood culture/PCR platform [2, 8, 9].
We aimed to investigate culture, molecular and serological prevalence of Bartonella spp. infections in a group considered at risk (companion animal veterinary personnel) due to frequent exposure to pets and their associated arthropods.
Methods
A cross-sectional study was performed to determine the seroprevalence (detection of antibodies to six Bartonella spp./subspecies) and bacteremia using enrichment blood culture, PCR and DNA sequencing in companion animal veterinary personnel.
Subject recruitment
Based on a similar study, the expected prevalence of Bartonella DNA in veterinarians was 28% [10]. A minimum sample size of 77 individuals was calculated with a margin of error of 10% and a confidence level of 95%. A sample of 85 veterinarians and five veterinary technicians from different regions of Spain who worked with pets and other wild mammals and who attended the annual national small-animal veterinary congress ‘Vetmadrid 2016’ (2447 attendees) held in Madrid (Spain) in March 2016 were recruited. Before the congress, all attendees were notified about the opportunity to participate in the study. One veterinarian who had recently taken antimicrobials (in the last two months) was subsequently excluded from the study.
Data and specimen collection
A standardized questionnaire including demographic information, clinical symptoms experienced, occupational and non-occupational domestic and wild animal bites, scratch or exposures, and travel history, was completed. Exposure to, or bites by, different arthropods (i.e. lice, fleas, ticks, mites, bed bugs) was recorded. Persistent/chronic disease was defined in the questionnaire as longer than six months.
Approximately 10–12 ml of blood (5–6 ml in EDTA, 5–6 ml in a serum separator tube) was collected at the time of enrollment. Aseptic technique was used including chlorhexidine decontamination of the skin. An experienced nurse performed venipuncture.
Specimen processing and diagnostic testing
Refrigerated EDTA-anticoagulated blood and serum samples were transported in less than 48 h by car to the Center of Rickettsiosis and Arthropod-Borne Diseases at CIBIR (Logroño, La Rioja, Spain), where blood was centrifuged and sera stored to -80 °C until being prepared for shipping to Galaxy Diagnostics, Inc., Research Triangle Park, North Carolina, USA.
Bartonella IFA serological testing
To compare results across studies, we used culture, serological and enrichment blood culture/PCR techniques in this study, as were used in a previous study involving veterinary personnel [10]. Bartonella v. berkhoffii, B. henselae, and B. koehlerae antibodies were determined in the Intracellular Pathogens Research Laboratory (IPRL) at North Caroline State University (North Carolina, USA) using cell culture grown bacteria as antigens and following standard immunofluorescent antibody assay (IFA) techniques. Cell lines were determined Mycoplasma free by PCR testing. Canine isolates of B. v. berkhoffii genotype I (NCSU 93CO-01 Tumbleweed, ATCC type strain #51672), B. v. berkhoffii genotype II (NCSU 95CO-08, Winnie), and B. v. berkhoffii genotype III (NCSU 06CO-01 Klara) and feline isolates of B. henselae H-1 strain (NCSU 93FO-23 Cisco), B. henselae SA2 strain (NCSU 95FO-099, Missy), and B. koehlerae (NCSU 09FO-01, Trillium) colonies were passed from agar plate grown cultures into Bartonella-permissive cell lines, i.e. the DH82 (a canine monocytoid) cell line for strains B. henselae H-1 and SA2, B. v. berkhoffii I and B. koehlerae and Vero cells (a mammalian fibroblast cell line) for B. v. berkhoffii II and III to obtain antigens for IFA testing. For each antigen, heavily infected cell cultures were spotted onto 30-well Teflon-coated slides (Cel-Line/Thermo Scientific), air-dried, acetone-fixed, and stored frozen. Fluorescein conjugated goat anti-human IgG (Cappel, ICN) was used to detect bacteria within cells using a fluorescent microscope (Carl Zeiss Microscopy, LLC, Thornwood, NY).
Serum samples diluted in phosphate-buffered saline (PBS) solution containing normal goat serum, Tween-20, and powdered nonfat dry milk to block nonspecific antigen binding sites were first screened at dilutions of 1:16 to 1:64. All sera that were reactive at a titer of 64 were further tested with two-fold dilutions out to 1:8192. To avoid confusion with possible nonspecific binding found at low dilutions, a cut-off of 1:64 was selected as a seroreactive titer.
Growth medium
BAPGM enrichment blood culture/PCR was performed at Galaxy Diagnostics Inc., Research Triangle Park, North Carolina, USA, as previously described [8, 10, 11]. An aliquot of 1 ml of EDTA whole blood was inoculated into 10 ml of BAPGM, after which the cultures were maintained at 35 °C in a 5% CO2, water-saturated atmosphere. After 7, 14, and 21-day incubation periods, a 1-ml aliquot of the enrichment culture was inoculated onto blood agar plates and incubated at 35 °C. Plates were checked for colony formation at 7, 14, and 21 days after inoculation.
Conventional and quantitative real-time PCR analysis
Using standard operating procedures, DNA was extracted from EDTA anticoagulated blood, enrichment liquid blood culture, and from blood agar plate colony isolates if obtained after subculture of the previously enriched blood samples for Bartonella spp. PCR [11]. Bartonella spp. moreover, strain classification was performed using primers designed to amplify two consensus sequences in the Bartonella 16S-23S internal transcribed spacer (ITS) region as described previously with minor modifications [11, 12]. Amplicon size obtained from the 16S-23S ITS region is species dependent, allowing preliminary species identification based on amplicon size. Two sets of oligonucleotides, 325s and 1100as were used as forward and reverse primers for conventional PCR. Meanwhile primers 325s and 538as were used as forward and reverse primers for quantitative PCR along with TaqMan probe 438 (Table 1). Additionally, as previously reported [13], PCR screening for B. koehlerae was performed using species-specific oligonucleotides Bkoehl-1s and Bkoehl1125as forward and reverse primers, respectively. Amplification of the ITS region at both genus and species (B. koehlerae) levels by conventional PCR was performed in a 25 μl final volume reaction containing 12.5 μl of MyTaq HS Red Mix 2× (Bioline), 0.2 μl of 100 μM of each forward and reverse primer (IDT-DNA Technology), 7.3 μl of molecular-grade water, and 5 μl of DNA from each sample tested. PCR negative controls were prepared using 5 μl of dH2O (when testing isolates from plates), 5 μl of DNA from the blood of a healthy dog, or 5 μl of DNA extracted from un-inoculated BAPGM-negative controls (when testing BAPGM enrichment cultures). Positive controls for PCR were prepared by serial dilution (using dog blood DNA) of genomic DNA from B. henselae (Houston I strain type) down to 0.001 pg/μl (equivalent to 0.5 bacteria/μL). Conventional PCR was performed in an Eppendorf Mastercycler EP gradient under the following conditions: a single hot-start cycle at 95 °C for 3 min followed by 55 cycles of denaturing at 94 °C for 15 s, annealing at 66 °C for 15 s, and extension at 72 °C for 18 s. Amplification was completed by an additional cycle at 72 °C for 1 min, and products were analyzed by 2% agarose gel electrophoresis with detection using ethidium bromide under ultraviolet light. Amplicon products were sequenced to determine the Bartonella sp. and ITS strain type. Quantitative real-time PCR was also performed in a 25 μl final volume reaction containing 12.5 μl of SsoAdvanced Universal Probes supermix (Bio-Rad, Hercules, USA), 0.2 μl of 100 μM of each forward and reverse primer (IDT-DNA Technology, Coralville, USA), 0.2 μl of 100 μM of TaqMan probe, and 7.3 μl of molecular-grade water. Positive and negative controls used were as described above. qPCR was performed in a CFX96 Real-time System (Bio-Rad) under the following conditions: a single hot-start cycle at 95 °C for 3 min followed by 44 cycles of denaturing at 94 °C for 10 s, annealing at 66 °C for 10 s, and extension at 72 °C for 10 s. Fluorescence at channel one was detected during the extension cycle. As in conventional PCR, all amplicon products were sequenced to determine the Bartonella sp. and ITS strain type. All PCR and un-inoculated BAPGM enrichment controls remained negative throughout the study period.
Sequencing analysis
PCR amplicon sequence analysis was performed using a commercial company (Genewiz, Research Triangle Park, NC). Chromatogram evaluation and sequence alignment were performed using Contig-Express and AlignX software (Vector NTI Suite 10.1, Invitrogen Corp., Carlsbad, CA). Bacteria species and strain were defined by comparing similarities with other sequences deposited in the GenBank database using the Basic Local Alignment Search Tool (Blast v. 2.0), and an in-house curated database.
Data analysis
Questionnaire data for the study were collected on paper forms, entered into a Microsoft Excel database, and validated comparing the electronic records with the information on the forms. Associations of demographic, risk factor, symptoms and exposure variables were assessed with means and medians for continuous variables, and with counts and percentages in contingency tables for categorical data. Group comparisons were performed. The Fisher's exact test for categorical variables and the Mann-Whitney U-test for numerical variables were used. Data processing was carried out with the R software [14], version 3.3.1 for Windows.
Results
Individuals studied
A total of 89 veterinary personnel from different regions of Spain (Madrid: 40; Catalonia: 10; Basque Country: 7; Andalusia: 6; Castilla y León: 6; Valencian Community: 5; Canary Islands: 5; Castilla La Mancha: 4; Galicia: 2; Aragon: 1; Asturias: 1; Navarra 1; and La Rioja: 1) were enrolled in the study and a total of 178 samples (EDTA-blood and sera) and the accompanying questionnaires were used to generate data reported in the study. The main characteristics of the study population (exposures and demographics) are listed in Additional file 1: Table S1. A high percentage of the participants reported having chronic/ persistent non-specific symptoms such as headache, insomnia, fatigue or memory problems.
Bartonella detection
Serology
Seroreactivity among the six Bartonella spp. or genotypes ranged between 11.2–56.2%, with the lowest percentage reactivity (11.2%) to B. quintana (Table 2). Only 24 of 89 (27%) participants were not seroreactive to any test antigen, whereas 13, 13, 14, 14, 9, and 2 participants were seroreactive to 1, 2, 3, 4, 5, or 6 antigens, respectively. Seroreactivity to B. henselae, B. v. berkhoffii genotypes I, II and III, and B. koehlerae ranged between 28 and 56%.
Among individual study participants, seroreactivity patterns varied among the six Bartonella spp. or genotypes used for IFA testing (Table 2). Bartonella spp. IFA seroreactivity was not statistically associated with any clinical sign or symptom (all P-values > 0.05).
BAPGM enrichment blood culture PCR
Six veterinarians and one veterinary technician (7.9%) had a positive BAPGM enrichment blood culture/PCR result (Table 3). There were no significant differences found between these two groups (P = 0.343). For PCR-positive participants, B. quintana was amplified and sequenced from 14 or 21-day BAPGM enrichment blood cultures (two veterinarians), B. v. berkhoffii genotype I from 7 and 14-day cultures (one veterinarian), B. v. berkhoffii genotype III from blood or a 7-day BAPGM enrichment blood culture (one veterinarian and veterinary technician), and B. henselae from seven and 14 days BAPGM enrichment blood cultures (two veterinarians). Blood agar plate subculture isolates were not obtained from any participant. No individual was found to be co-infected with more than one Bartonella spp. BAPGM enrichment blood culture/PCR positivity was not statistically associated with clinical signs or symptoms (all P-values > 0.05; Additional file 1: Table S1). Corticosteroid intake, demographics, and arthropod or animal exposures were not statistically associated with BAPGM enrichment blood culture/PCR positivity (P-values > 0.05; Additional file 1: Table S1). Information about exposures, demographics and clinical features of the individuals with BAPGM enrichment blood culture/PCR positivity are summarized in Additional file 2: Table S2.
Assays associations (serology and BAPGM-PCR)
One B. henselae PCR-positive individual was IFA seronegative to all test antigens, and another one was not seroreactive to B. henselae. The remaining five PCR-positive individuals were seroreactive to multiple Bartonella spp. antigens (Table 4).
Discussion
The study presented here documented a high serological (65/89 participants; 73.0%) and molecular (7/89; 7.9%) prevalence of Bartonella spp. in Veterinary workers from Spain.
Clinically, the diagnostic interpretation of these serological and molecular test results supporting Bartonella exposure or infection, respectively, in patients without typical clinical presentations or environmental epidemiological exposures is challenging. For example, the diagnosis of CSD in a patient with lymphadenopathy after being bitten or scratched by a mammal (cat or dog) is straightforward and microbiological assays are unnecessary in most instances to confirm the clinical diagnosis. In contrast, syndromes or illnesses caused by Bartonella spp. such as endocarditis, peliosis, angiomatosis, fever of unknown origin, isolated hepatosplenic abscesses, uveitis, and others are clinically challenging, diagnostically problematic, and require microbiological confirmation of diagnosis. In addition, specifically defining the infecting Bartonella sp. as the etiological agent of illness is necessary to determine disease epidemiology and to facilitate disease surveillance among various populations (humans, animals and vectors). However, implicating a Bartonella sp. as the causative agent of an atypical clinical presentation can be difficult when using serology, and even if the bacterial DNA is amplified from blood or enrichment blood cultures or if the organism is cultivated from the blood. Recently, B. henselae and B. clarridgeiae have been isolated from the blood of human donors in Brazil using BAPGM enrichment culture/PCR, indicating that asymptomatic bacteremia can occur in healthy humans [9]. Moreover, long standing B. quintana bacteremia has been reported in homeless and in immunosuppressed patients [15]. Thus, it is possible that Bartonella spp. can induce long standing intra-erythrocytic and endothelial cell infections in healthy individuals without causing pathology or long standing bacteremia may lead to chronic, slowly progressive vascular injury in an otherwise immunocompetent individual [16]. Data in support of either alternative is minimal. Regardless, Bartonella serological or molecular microbiological blood culture results in this study and patients without a medically defined clinical syndrome must be cautiously interpreted.
In most clinical microbiology laboratories the diagnosis of Bartonella infections is based on serological assays, with current techniques lacking sensitivity, specificity or both. Moreover, conventional cultures (gold standard) are not routinely used due to the overall poor sensitivity in isolating Bartonella spp. In recent years, molecular assays have been used for clinical diagnosis and epidemiological studies in vectors (e.g. fleas) [5, 17,18,19]. However, the sensitivity of these assays is low when testing clinical specimens, such as blood, joint or cerebrospinal fluid or certain tissues. In this study, a very high prevalence of Bartonella spp. antibodies was found using in-house IFA assays and six different species and genotypes and strains. As veterinary personnel have frequent contact with reservoir hosts (cats, dogs, wild and production animals) and with Bartonella vectors (fleas, ticks, lice, mites), it is likely that these individuals are repeatedly exposed to these bacteria throughout their careers. Although cross reactivity occurs when IFA is used, exposure to more than one Bartonella spp. is also possible in veterinary personnel and others with frequent animal and arthropod exposures. For unknown reasons, the highest seroreactivity in the studied population was observed against B. v. berkhoffii genotype II, whereas only genotypes I and III were detected by enrichment blood culture/PCR. Bartonella koehlerae seroprevalence was also high among veterinary personnel (41.6%), although neither culture nor molecular amplification of this species was obtained in this study, despite testing with B. koehlerae-specific PCR primers. The presence of B. koehlerae has been reported from the Americas, Europe, Asia and Australia [20,21,22,23,24,25]. Cats appear to be the primary reservoir hosts for B. koehlerae, and this species has been associated with disease in dogs [20,21,22], with a case of human endocarditis [23] and with a young woman with a longstanding history of hallucinations, sensory neuropathy, and peripheral visual deficits [24]. By serology, B. koehlerae was implicated diagnostically in a veterinarian with complex regional pain syndrome type I [25] and as a potential cause or cofactor in the development of arthritis, peripheral neuropathies or tachyarrhythmias [13].
As expected, a high B. henselae seroprevalence was found in this veterinary worker population (37.1%). This Bartonella has a worldwide distribution, cats are the main reservoirs and vectors, and fleas (Ctenocephalides felis and C. canis) are considered the primary arthropod vectors for infecting cats and other animals. B. henselae is the primary or sole causative agent of CSD and induces other clinical syndromes in humans [1]. Documentation of human Bartonella infections is scarce in Spain. Nevertheless, clinical descriptions [5, 17, 26] and seroepidemiological studies about the prevalence of B. henselae/B. quintana [27,28,29] have been reported. In our previous studies carried out in La Rioja (North of Spain), B. henselae seroprevalences in cat owners, HIV-infected patients and blood donors were 28.9%, 17.3% and 5.9%, respectively, using a commercial kit [30, 31]. These lower percentages most likely reflect differences in the antigens used for testing, and exposure risks among the study populations, with veterinary personnel, most likely having the highest exposure risk. As previously reported, serological tests may not reliably distinguish between antibody responses to Bartonella spp. moreover, other infectious agents [32]. Contact with cats and their fleas are the main epidemiological risk factors that contribute to acquiring B. henselae infection, and this species has also been involved in disease in dogs from Spain [33]. In a molecular study carried out in fleas from La Rioja, 3.4% and 6.8% C. felis were infected with B. henselae and B. clarridgeiae, respectively [18]. Importantly, cats and dogs are frequently infested with numerous fleas, rather than a single or few fleas. Both B. henselae and B. clarridgeiae have been isolated from healthy human blood donors in Brazil [9, 34]. To our knowledge, no studies have attempted to culture Bartonella from the blood of healthy humans in Spain. Although a study from the United States found a statistical association between Bartonella spp. bacteremia and symptomatology [35], that study, the study presented here, and the Brazilian blood donor study indicate that B. henselae bacteremia can be documented in asymptomatic individuals.
Serology can only imply that the investigated population has been exposed to one or more Bartonella spp., whereas PCR amplification and DNA sequence confirmation of bacterial DNA from blood or cultures supports infection at the time of sampling. PCR and DNA sequencing confirmed the infection with B. henselae, B. quintana, and two B. v. berkhoffii genotypes (I and III, respectively). Four out of seven infected individuals were asymptomatic at the time of sample collection and the remaining three reported historical symptoms such as insomnia, memory problems and fatigue. B. v. berkhoffii genotype III has been recently documented as a cause of endocarditis and myocarditis in dogs [36], and genotype II was isolated from a boy with epitheliod hemangioendothelioma [37]. Bartonella v. berkhoffii has been involved in at least one human case of endocarditis [38], and it has also been found in patients with neurological disorders [39] and rheumatic symptoms [40]. A case of perinatal transmission of both B. henselae and B. v. berkhoffii has also been reported [41]. Although canines are the primary reservoir hosts for B. v. berkhoffii, the vector(s) responsible for transmission of this infection are unknown [42, 43].
Unexpectedly, two asymptomatic veterinarians were enrichment blood culture/PCR-positive to B. quintana, the agent of trench fever and other diseases. It is known that, outside of the context of HIV, B. quintana has been isolated from afebrile homeless and alcoholic patients from North America and small European clusters [15], but to our knowledge never before from a healthy individual. The mode of B. quintana acquisition in these two individuals is unresolved, as none of the study subjects recalled exposure to body lice (Pediculus humanus corporis), considered the sole primary vectors of B. quintana. These arthropods are common under poor hygiene conditions, which was not the case of the participants of our study. Apart from body lice, B. quintana DNA has been amplified from cat fleas and bed bugs (Cimex lectularius) [44, 45]. B. quintana endocarditis has been documented in dogs from New Zealand and the United States [46], and bites or scratches from a feral cat were implicated as the source of B. quintana transmission to a previously healthy, bacteremic human [47]. Collectively, these findings suggest that other arthropods, cats, dogs, or other animals could have been the source of B. quintana infections since the individuals reported exposure to fleas, head lice (Pediculus humanus capitis) and a variety of animals.
To a substantial degree, the current re-emergence or rediscovery of Bartonella spp. evolved as a result of the detection of B. quintana and B. henselae infections in HIV patients with bacillary angiomatosis or peliosis hepatis. Thus, infection in severely immunocompromised individuals was required before the worldwide clinical emergence of the genus Bartonella became recognized. During the ensuing decades, there have been continuous and substantial changes in our understanding of the epidemiology, pathophysiology and vector biology associated with these bacteria.
Conclusions
This study documented high serological and molecular prevalence of Bartonella in veterinary personnel. Future research is required to clarify the duration of and potential relationship to Bartonella spp. bacteremia and non-specific symptoms or subtle pathology in immunocompetent individuals.
Abbreviations
- ATCC:
-
American Type Culture Collection
- B. henselae H1:
-
Bartonella henselae Houston 1 strain
- B. henselae SA2:
-
Bartonella henselae San Antonio 2 strain
- BAPGM:
-
Bartonella alphaproteobacteria growth medium
- BCN:
-
Blood culture negative
- CSD:
-
Cat scratch disease
- DH82:
-
A canine monocytoid cell line
- EDTA:
-
Ethylenediaminetetraacetic acid
- HIV:
-
Human immunodeficiency virus
- IFA:
-
Immunofluorescence antibody assay
- IgG:
-
Immunoglobulin class G
- ITS:
-
Internal transcribed spacer
- PBS:
-
Phosphate-buffered saline
References
Gandhi TN, Slater LN, Welch DF, Koehler JE. Bartonella, including cat-scratch disease. In: Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett's principles and practice of infectious diseases. 8th ed. Philadelphia: Elsevier Saunders; 2015.
Vayssier-Taussat M, Moutailler S, Féménia F, Raymond P, Croce O, La Scola B, et al. Identification of novel zoonotic activity of Bartonella spp., France. Emerg Infect Dis. 2016;22:457–62.
Breitschwerdt EB. Bartonellosis: One Health and all creatures great and small. Vet Dermatol. 2017;28:96–e21.
Welch DF, Pickett DA, Slater LN, Steigerwalt AG, Brenner DJ. Rochalimaea henselae sp. nov., a cause of septicemia, bacillary angiomatosis, and parenchymal bacillary peliosis. J Clin Microbiol. 1992;30:275–80.
García JC, Núñez MJ, Castro B, Fernández JM, López A, Portillo A, et al. Hepatosplenic cat scratch disease in immunocompetent adults: report of 3 cases and review of the literature. Medicine (Baltimore). 2014;93:267–79.
Kerkhoff FT, Bergmans AM, van Der Zee A, Rothova A. Demonstration of Bartonella grahamii DNA in ocular fluids of a patient with neuroretinitis. J Clin Microbiol. 1999;37:4034–8.
Gutiérrez R, Vayssier-Taussat M, Buffet JP, Harrus S. Guidelines for the isolation, molecular detection, and characterization of Bartonella species. Vector Borne Zoonotic Dis. 2017;17:42–50.
Maggi RG, Duncan AW, Breitschwerdt EB. Novel chemically modified liquid medium that will support the growth of seven Bartonella species. J Clin Microbiol. 2005;43:2651–5.
Pitassi LH, de Paiva Diniz PP, Scorpio DG, Drummond MR, Lania BG, Barjas-Castro ML, et al. Bartonella spp. bacteremia in blood donors from Campinas, Brazil. PLoS Negl Trop Dis. 2015;9:e0003467.
Lantos PM, Maggi RG, Ferguson B, Varkey J, Park LP, Breitschwerdt EB, et al. Detection of Bartonella species in the blood of veterinarians and veterinary technicians: a newly recognized occupational hazard? Vector Borne Zoonotic Dis. 2014;14:563–70.
Maggi RG, Mascarelli PE, Pultorak EL, Hegarty BC, Bradley JM, Mozayeni BR, et al. Bartonella spp. bacteremia in high-risk immunocompetent patients. Diagn Microbiol Infect Dis. 2011;71:430–7.
Maggi RG, Breitschwerdt E. Potential limitations of the 16S-23S rRNA intergenic region for molecular detection of Bartonella species. J Clin Microbiol. 2005;43:1171–6.
Breitschwerdt EB, Maggi RG, Robert Mozayeni B, Hegarty BC, Bradley JM, Mascarelli PEPCR. Amplification of Bartonella koehlerae from human blood and enrichment blood cultures. Parasit Vectors. 2010;3:76.
Core Team R. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2016. URL http://www.R-project.org/
Brouqui P, Lascola B, Roux V, Raoult D. Chronic Bartonella quintana bacteremia in homeless patients. N Engl J Med. 1999;340:184–9.
Picascia A, Pagliuca C, Sommese L, Colicchio R, Casamassimi A, Labonia F, et al. Seroprevalence of Bartonella henselae in patients awaiting heart transplant in southern Italy. J Microbiol Immunol Infect. 2017;50:239–44.
Oteo JA, Castilla A, Arosey A, Blanco JR, Ibarra V, Morano LE. Endocarditis due to Bartonella spp. three new clinical cases and Spanish literature review. Enferm Infecc Microbiol Clin. 2006;24:297–301.
Blanco JR, Pérez-Martínez L, Vallejo M, Santibáñez S, Portillo A, Oteo JA. Prevalence of Rickettsia felis-like and Bartonella spp. in Ctenocephalides felis and Ctenocephalides canis from La Rioja (northern Spain). Ann N Y Acad Sci. 2006;1078:270–4.
Pérez-Martínez L, Venzal JM, González-Acuña D, Portillo A, Blanco JR, Oteo JA. Bartonella rochalimae and other Bartonella spp. in fleas, Chile. Emerg Infect Dis. 2009;15:1150–2.
Ohad DG, Morick D, Avidor B, Harrus S. Molecular detection of Bartonella henselae and Bartonella koehlerae from aortic valves of boxer dogs with infective endocarditis. Vet Microbiol. 2010;141:182–5.
Pérez C, Maggi RG, Diniz PP, Breitschwerdt EB. Molecular and serological diagnosis of Bartonella infection in 61 dogs from the United States. J Vet Intern Med. 2011;25:805–10.
Tabar MD, Altet L, Maggi RG, Altimira J, Roura X. First description of Bartonella koehlerae infection in a Spanish dog with infective endocarditis. Parasit Vectors. 2017;10:247.
Avidor B, Graidy M, Efrat G, Leibowitz C, Shapira G, Schattner A, et al. Bartonella koehlerae, a new cat-associated agent of culture-negative human endocarditis. J Clin Microbiol. 2004;42:3462–8.
Breitschwerdt EB, Mascarelli PE, Schweickert LA, Maggi RG, Hegarty BC, Bradley JM, et al. Hallucinations, sensory neuropathy, and peripheral visual deficits in a young woman infected with Bartonella koehlerae. J Clin Microbiol. 2011;49:3415–7.
Vera CP, Maggi RG, Woods CW, Mascarelli PE, Breitschwerdt EB. Spontaneous onset of complex regional pain syndrome type I in a woman infected with Bartonella koehlerae. Med Microbiol Immunol. 2014;203:101–7.
García JC, Núñez MJ, Portillo A, Oteo JA. Cat-scratch disease presenting as parotid gland abscess and aseptic meningitis. Enferm Infecc Microbiol Clin. 2017;35:58–9.
Garcia-Garcia JA, Baquerizo R, Vargas J, Mira JA, Merchante N, Macías J, et al. Prevalencia de anticuerpos séricos frente a Bartonella spp. en una población sana del área del sur de la provincia de Sevilla. Rev Clin Esp. 2005;11:541–4.
Pons I, Sanfeliu I, Cardeñosa N, Nogueras MM, Font B, Segura F. Serological evidence of Bartonella henselae infection in healthy people in Catalonia, Spain. Epidemiol Infect. 2008a;136:1712–6.
Pons I, Sanfeliu I, Nogueras MM, Sala M, Cervantes M, Amengual MJ, et al. Seroprevalence of Bartonella spp. infection in HIV patients in Catalonia, Spain. BMC Infect Dis. 2008b;8:58.
Blanco Ramos JR, Oteo Revuelta JA, Martínez de Artola V, Ramalle Gómara E, García Pineda A, Ibarra Cucalón V. Seroepidemiology of Bartonella henselae infection in a risk group. Rev Clin Esp. 1998;198:805–9.
Blanco JR, Oteo JA, Martínez V, Ramalle E, García A, Ibarra V, et al. Seroepidemiology of Bartonella henselae infection in HIV-infected patients. Enferm Infecc Microbiol Clin. 1999;17:434–8.
La Scola B, Raoult D. Serological cross reactions between Bartonella quintana, Bartonella henselae, and Coxiella burnetii. J Clin Microbiol. 1996;34:2270–4.
Tabar MD, Maggi RG, Altet L, Vilafranca M, Francino O, Roura X. Gammopathy in a Spanish dog infected with Bartonella henselae. J Small Anim Pract. 2011;52:209–12.
Vieira-Damiani G, Diniz PP, Pitassi LH, Sowy S, Scorpio DG, Lania BG, et al. Bartonella clarridgeiae bacteremia detected in an asymptomatic blood donor. J Clin Microbiol. 2015;53:352–6.
Breitschwerdt EB, Maggi RG, Nicholson WL, Cherry NA, Woods CW. Bartonella sp. bacteremia in patients with neurological and neurocognitive dysfunction. J Clin Microbiol. 2008;46:2856–61.
Shelnutt LM, Balakrishnan N, DeVanna J, Batey KL, Breitschwerdt EB. Death of military working dogs due to Bartonella vinsonii subspecies berkhoffii genotype III endocarditis and myocarditis. Mil Med. 2017;182:e1864–9.
Breitschwerdt EB, Maggi RG, Varanat M, Linder KE, Weinberg G. Isolation of Bartonella vinsonii subsp. berkhoffii genotype II from a boy with epithelioid hemangioendothelioma and a dog with hemangiopericytoma. J Clin Microbiol. 2009;47:1957–60.
Roux V, Eykyn SJ, Wyllie S, Raoult D. Bartonella vinsonii subsp. berkhoffii as an agent of afebrile blood culture-negative endocarditis in a human. J Clin Microbiol. 2000;38:1698–700.
Breitschwerdt EB, Maggi RG, Lantos PM, Woods CW, Hegarty BC, Bradley JM. Bartonella vinsonii subsp. berkhoffii and Bartonella henselae bacteremia in a father and daughter with neurological disease. Parasit Vectors. 2010;3:29.
Maggi RG, Mozayeni BR, Pultorak EL, Hegarty BC, Bradley JM, Correa M, et al. Bartonella spp. bacteremia and rheumatic symptoms in patients from Lyme disease-endemic region. Emerg Infect Dis. 2012;18:783–91.
Breitschwerdt EB, Maggi RG, Farmer P, Mascarelli PE. Molecular evidence of perinatal transmission of Bartonella vinsonii subsp. berkhoffii and Bartonella henselae to a child. J Clin Microbiol. 2010;48:2289–93.
Chomel BB, Boulouis HJ, Breitschwerdt EB, Kasten RW, Vayssier-Taussat M, Birtles RJ, et al. Ecological fitness and strategies of adaptation of Bartonella species to their hosts and vectors. Vet Res. 2009;40:29.
Yore K, DiGangi B, Brewer M, Balakrishnan N, Breitschwerdt EB, Lappin M. Flea species infesting dogs in Florida and Bartonella spp. prevalence rates. Vet Parasitol. 2014;199:225–9.
Kernif T, Leulmi H, Socolovschi C, Berenger JM, Lepidi H, Bitam I, et al. Acquisition and excretion of Bartonella quintana by the cat flea, Ctenocephalides felis felis. Mol Ecol. 2014;23:1204–12.
Leulmi H, Bitam I, Berenger JM, Lepidi H, Rolain JM, Almeras L, et al. Competence of Cimex lectularius bed bugs for the transmission of Bartonella quintana, the agent of trench fever. PLoS Negl Trop Dis. 2015;9:e0003789.
Kelly P, Rolain JM, Maggi R, Sontakke S, Keene B, Hunter S, et al. Bartonella quintana endocarditis in dogs. Emerg Infect Dis. 2006;12:1869–72.
Breitschwerdt EB, Maggi RG, Sigmon B, Nicholson WL. Isolation of Bartonella quintana from a woman and a cat following putative bite transmission. J Clin Microbiol. 2007;45:270–2.
Acknowledgements
The publication of this paper has been sponsored by Bayer Animal Health in the framework of the 12th CVBD World Forum Symposium. We are grateful to Amanda Elam (Galaxy Diagnostics Inc., North Carolina, USA) for administrative support for testing. We acknowledge Maria de Lourdes Mottier, Annette Boegel and Markus Edingloh (Bayer Animal Health GmbH, Leverkusen, Germany), Alejandra M. González, Montserrat Tarancón and Gemma Mascaró (Bayer Hispania, S.L., Barcelona, Spain), Beatriz Pérez (IFEMA, Madrid, Spain) and Raúl Martín (Trauma Assistance, S.L., Madrid, Spain) for facilitating the study. We are also grateful to Rosario López Gómez (Center for Biomedical Research from La Rioja, Logroño, Spain) for help with the inclusion of data.
Funding
We appreciate the support from Bayer Animal Health GmbH (Leverkusen, Germany) for funding the study (No. 2111116219).
Availability of data and materials
Data supporting the conclusions of this article are included in the article and its additional files. To assure participant confidentiality, please contact JO or EB for questions relative to the raw data.
Author information
Authors and Affiliations
Contributions
EB, JAO, RGM and AP designed the study. LGA, JAO and XR collected samples. RGM, NC and JB processed samples and analyzed sequences. MSM performed statistical analysis. JAO, AP, EB and RGM analyzed the data. JAO, AP, EB and RGM wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional review board approval for this study was received from the Ethical Committee of Clinical Research from La Rioja (CEICLAR) on January 29, 2016 (Ref. CEICLAR PI-209).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests. This study was presented in part at the 12th Symposium of the Canine Vector Borne Disease (CVBD) World Forum, Athens, Greece, March 13–16, 2017 (oral presentation), and in the XXI Congreso de la Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica (SEIMC), Málaga (Spain), May 11–13, 2017 (oral presentations 071 and 072).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1: Table S1.
Exposures and demographics of veterinary subjects, tests statistics and P-values for the differences between Bartonella PCR-positive and PCR-negative individuals. (DOCX 20 kb)
Additional file 2: Table S2.
Exposures, demographics and clinical features, if any, of bacteremic veterinary personnel based upon BAPGM enrichment blood culture/PCR positivity. (DOCX 17 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Oteo, J.A., Maggi, R., Portillo, A. et al. Prevalence of Bartonella spp. by culture, PCR and serology, in veterinary personnel from Spain. Parasites Vectors 10, 553 (2017). https://doi.org/10.1186/s13071-017-2483-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13071-017-2483-z