Abstract
Background
A high intake of phytoestrogens, found in soy, rye, and seeds, is associated with a reduced risk of a prostate cancer diagnosis. Previously, we found that the overall decreased risk of prostate cancer diagnosis in males with a high intake of phytoestrogens was strongly modified by a nucleotide sequence variant in the estrogen receptor-beta (ERβ) gene. However, we do not know if phytoestrogens can inhibit the growth of prostate cancer in males with established diseases. If there is an inhibition or a delay, there is reason to believe that different variants of the ERβ gene will modify the effect. Therefore, we designed an intervention study to investigate the effect of the addition of foods high in phytoestrogens and their interaction with the ERβ genotype on prostate tumor proliferation in patients with prostate cancer.
Method
The PRODICA trial is a randomized ongoing intervention study in patients with low- and intermediate-risk prostate cancer with a Gleason score < 8, prostate-specific antigen (PSA) < 20, and scheduled for radical prostatectomy. The study is conducted at Sahlgrenska University Hospital in Gothenburg, Sweden. The intervention consists of a daily intake of soybeans and flaxseeds (~ 200 mg of phytoestrogens) until the surgery, approximately 6 weeks. The aim is to recruit 200 participants. The primary outcome is the difference in the proliferation marker Ki-67 between the intervention and the control groups. The genotype of ERβ will be investigated as an effect-modifying factor. Secondary outcomes include, e.g., concentrations of PSA and steroid hormones in the blood.
Discussion
The results of the PRODICA trial will contribute important information on the relevance of increasing the intake of phytoestrogens in patients with prostate cancer who want to make dietary changes to improve the prognosis of their cancer. If genetic factors turn out to influence the effect of the intervention diet, dietary advice can be given to patients who most likely benefit from it. Dietary interventions are cost-effective, non-invasive, and result in few mild side effects. Lastly, the project will provide basic pathophysiological insights which could be relevant to the development of treatment strategies for patients with prostate cancer.
Trial registration.
ClinicalTrials.gov NCT02759380. Registered on 3 May 2016.
Similar content being viewed by others
Background
In the clinic, patients diagnosed with prostate cancer often request dietary advice to improve the prognosis of their cancer [1]. We do not know if dietary changes can reduce tumor proliferation in patients with prostate cancer [2]. However, a high intake of phytoestrogens has been associated with a reduced risk of prostate cancer diagnosis [3]. In a previous study, we found an inverse association between dietary intake of phytoestrogens and the risk of prostate cancer, especially among individuals with a particular genetic makeup of the estrogen receptor beta (ERβ) gene [4]. These data warrant a prospective study to investigate whether foods high in phytoestrogens can inhibit the growth of prostate tumors.
Since the 1970s, it has been well known that testosterone and estradiol are involved in the progression of prostate cancer [5]. Phytoestrogens, found in foods such as soy, rye, and seeds [6], are structurally similar to mammal estrogen and bind to ERβ with high affinity [7]. By interacting with ERβ, phytoestrogens could affect prostate cancer progression [8]. Testosterone and its metabolite 5α-dihydrotestosterone (DHT) cause the proliferation of prostate epithelium by binding to the androgen receptor (AR) [9]. In contrast, by binding to ERβ, 5α androstane-3β,17β-diol (3βAdiol), a metabolite of DHT, represses the expression of AR and thereby inhibits androgen-driven proliferation while promoting cell differentiation [10, 11]. In terms of proliferation, current data suggest a combined stimulatory role of estrogen receptor alpha (ERα) and AR in the prostate whereas ERβ inhibits proliferation and stimulates differentiation. Both ERα and ERβ have an affinity for estradiol whereas phytoestrogens and 3βAdiol selectively activate ERβ [10]. Phytoestrogens should, as a result, be able to restrict cancer growth by acting as a substitute for 3βAdiol [12,13,14,15].
Several studies have investigated the effect of phytoestrogens on proliferation markers and steroid hormones in patients diagnosed with prostate cancer, but the results have been inconsistent [16,17,18,19,20,21,22,23,24,25,26,27]. The reason may be that the results have been diluted due to genetic interactions only having effects in some subgroups [4]. Various studies also had few participants, short follow-ups, and varying methods with different doses and sources of phytoestrogens studied [16,17,18,19,20,21,22,23,24,25,26,27]. The PRODICA (impact of DIet and individual genetic factors on tumor proliferation rate in males with PROstate CAncer) trial was initiated to investigate the effect of dietary phytoestrogens and their interaction with ERβ genotype on prostate tumor proliferation. Our hypotheses in the study are as follows:
-
1)
In males diagnosed with low- and intermediate-risk prostate cancer, the daily addition of phytoestrogen-rich foods (~200 mg phytoestrogens) to the diet for 6 weeks reduces prostate tumor proliferation compared to no addition of phytoestrogen-rich foods to the diet during the same period.
-
2)
If the effect of phytoestrogens on prostate-tumor proliferation exists, it is modified by males’ polymorphisms in the promoter region of the ERβ gene.
In addition, we will identify the pathways for how a diet high in phytoestrogens may influence the growth of prostate cancer. To determine this, we will identify RNA expression of the ERβ, ERα, and the AR in tumor tissue, as well as steroid hormone concentrations in blood, and compare this between males with a diet high and low in phytoestrogens or between different genotypes of the ERβ gene. We will also evaluate the effect of the intervention diet on phytoestrogen concentrations in the blood depending on the genotype of ERβ.
Methods and design
The PRODICA study is a randomized controlled dietary intervention trial with patients diagnosed with low- and intermediate-risk prostate cancer, scheduled for radical prostatectomy.
Study design
Recruitment
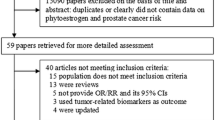
Participants are recruited at the outpatient urological department at Sahlgrenska University Hospital in Gothenburg, Sweden. The treating physician or the contact nurse asks eligible patients of interest to participate in the study (Fig. 1). The inclusion criteria are patients with prostate cancer T1–T2, Gleason score < 8, prostate-specific antigen (PSA) < 20, and scheduled for radical prostatectomy. The exclusion criteria are ongoing hormone therapy, other difficult physical or psychological conditions or diminished cognitive function, or allergy or intolerance to the intervention foods. A dietitian from the coordinating center contacts the patients that are interested to participate by phone; they will receive initial oral information about the study and can ask questions. An inclusion meeting is scheduled if the patient agrees to participate in the study.
Design of the PRODICA* trial. Eligible patients are identified at Sahlgrenska University Hospital in Gothenburg, Sweden. An inclusion meeting is scheduled with patients who agree to participate. At the inclusion meeting, participants are randomized to an intervention or a control group, they fill out a questionnaire including a food frequency questionnaire, and blood samples are collected. A 24-h dietary recall is performed with participants about halfway through the study to measure compliance with the intervention. Endpoint blood samples are collected, and participants fill out a similar questionnaire again near the time of the surgery. In immediate adjacency to the surgery, biopsies of cancer and benign prostate tissue are sampled for the study, and the prostate is thereafter handled according to clinical routines. *Impact of DIet and individual genetic factors on tumor proliferation rate in males with PROstate Cancer
Inclusion meeting, randomization, and dietary intervention
At the inclusion meeting with the coordinating center dietitian, participants receive additional oral and written information and sign informed consent. Thereafter, participants fill out a questionnaire online or on paper, including a food frequency questionnaire (FFQ) together with questions about, e.g., meal patterns, physical activity, intake of nutritional supplements, tobacco use, use of medications including antibiotics, socio-economic parameters, anthropometric measurements, and family history of prostate cancer [28]. Participants are randomized to an intervention or a control group by drawing 1 of 26 folded notes from an envelope where half of the notes are labeled intervention and the other half control. Drawn notes are put in another envelope and the notes are reused when all notes are drawn. This procedure is done to achieve an equal number of participants in the two groups. No placebo is used in the control group, but participants in the control group are blinded regarding what intervention foods the intervention group is provided with. Besides the intervention foods, the groups are treated equally, and all participants receive standard care.
During the inclusion meeting, baseline blood samples are collected, and body weight and height are measured. Height is measured using a wall-mounted stadiometer to the nearest 0.1 cm. Participants are instructed to remove heavy objects from their pockets. Participants wear indoor clothing; 1 kg is subtracted from the measured weight to account for their clothes. Both body weight and height are measured without shoes.
All participants receive a brochure with dietary recommendations from the Swedish National Food Agency [29], and the dietitian orally goes through the advice with each patient. The intervention group receive, at the inclusion meeting, fresh frozen green soybeans, roasted yellow soybeans, and flaxseeds in amounts that are estimated to last until the surgery. The intervention foods are purchased from ordinary food suppliers. Participants receive a schedule on how to gradually increase the amounts of the intervention foods during the first 9 days, starting on the day of the inclusion meeting (Additional file 1). Thereafter, they are instructed to eat 47 g of green soybeans, 28 g of roasted yellow soybeans, and 28 g of flaxseeds daily. These amounts are estimated to equal approximately 200 mg of phytoestrogens [30, 31]. Participants also receive serving suggestions and recipes for the intervention foods. We intended to use crushed flaxseeds, but during the study, we had to replace these with whole flaxseeds. In 2017, the Swedish Food Agency dissuaded the intake of crushed flaxseeds due to the formation of hydrogen cyanide from cyanogenic glycosides [32, 33]. During the study, participants are not given any dietary restrictions except for instructions to avoid nutritional supplements.
Follow-up and endpoint
A 24-h dietary recall is performed by phone with participants about halfway through the study period. During a clinical visit about 1 week before the surgery, or on the day of the surgery, endpoint blood samples are collected. Participants receive instructions to fill out a similar questionnaire as at baseline, 1 to 2 days before the surgery. Participants receive reminders for both the endpoint blood sample and the endpoint questionnaire. At the surgery, the surgeon collects biopsies, and the radical prostatectomy tissue is handled according to clinical routines.
Evaluation of the protocol and preparatory analyses
We intended that the intervention should last at least 6 weeks. However, as the time to surgery sometimes was shorter than 6 weeks and few patients wanted to postpone their surgery, the inclusion rate became too slow. We, therefore, decided to include all patients with at least 2 weeks to scheduled surgery. We also aimed to have the prostate biopsies to measure the primary outcome and compare it with patients’ diagnostic biopsies. However, to enable measuring different areas of the tumor and avoid missing data, we choose to use prostatectomy specimens to measure our primary outcome.
When ten participants had been included in the study, we evaluated the study protocol and found that all practical arrangements and established collaborations worked satisfactorily. To test compliance, daily dietary intake was measured with the 24-h dietary recall and the questionnaire, among 13 and 12 participants in the intervention and control groups, respectively. We found no differences between the groups in background characteristics or dietary intake at baseline. The intervention group increased their intake of the intervention foods, and thus the intake of phytoestrogens, while the control group did not change their dietary habits during the study period.
Dietary assessment
Food frequency questionnaire
Intake of energy and nutrients has been validated in the FFQ using urine alkylresorcinol metabolites as markers of dietary whole-grain intake and by comparing intakes with 4-day estimated food records in 30 males with prostate cancer and 31 males without prostate cancer [28]. The FFQ includes 184 food items and complex dishes and is divided into twelve food categories. The participants first answer how many times per day, week, or month they consume the food or the dish. Thereafter, they distribute the sum of ten ingredients that the dish could be made of or specific food items included in the food group. The FFQ at baseline reflects the dietary intake during the past 3 months, and the FFQ at endpoint reflects the time during the study. Standard portions together with the content of energy and nutrients are based on information from the Swedish National Food Agency [34]. We are using an in-house developed database to calculate the estimated intake of phytoestrogens; the database is described elsewhere [30, 31]. After participants have completed the questionnaire, the coordinating center dietitian reviews the questionnaire for eventual errors and contacts the study participant if needed.
Twenty-four-hour dietary recall
The 24-h dietary recall is performed by telephone according to a template (Additional file 2) by the coordinating center dietician. First, a simple list of yesterday’s food intake is assessed. Second, a list of foods that might be forgotten is checked (Additional file 2). Third, the time of meals and food details including brand, fat content, cooking methods, and estimated quantities are investigated. Finally, the listed foods are read out for the participant to see if something was forgotten. The 24-h dietary recall is performed to promote and control compliance and measure the total intake of phytoestrogens in the groups. During the phone call, participants in the intervention group can report adverse effects, e.g., flatulence and bloating, of the intervention foods; thus, the amounts of the intervention foods can be regulated based on the information given. Any reason for discontinuation of the intervention foods is not a reason for withdrawal from the study.
Concentrations of phytoestrogens in blood
In a proportion of participants, plasma concentrations of different phytoestrogens (daidzein, enterodiol, enterolactone, equol, genistein, glycitein, lariciresinol, and secoisolariciresinol) will be analyzed at Aarhus University in Denmark using LC–MS/MS measurements performed on microLC 200 series (Eksigent/AB Sciex, Redwood City, CA, USA) and QTrap 5500 mass spectrometer (AB Sciex, Framingham, MA, USA) [35, 36].
Dietary compliance
Compliance is controlled at two time points by the question of remaining intervention foods: during the phone call when the 24-h dietary recall is performed and at the end of the intervention. The total reported intake of phytoestrogens at the 24-h dietary recall will also be calculated in both groups.
Blood and biopsy collection
Blood samples are collected by ordinary venipuncture according to laboratory routines by experienced healthcare professionals: in serum, lithium-heparin, and EDTA collection tubes. Serum and EDTA collection tubes are stored at room temperature for at least 30 min; thereafter, the serum tubes are centrifuged, and the EDTA tubes are refrigerated. Lithium-heparin tubes are centrifuged within 30 min. The serum and lithium-heparin collection tubes are centrifuged at 2000 g for 10 min. The samples are pipetted into microtubes, frozen at − 20 °C the same day as the sampling, and stored at − 80 °C before they will be sent for analysis in batches. All samples are stored in the biorepository of “Biobank Väst,” registration number 890.
In immediate adjacency to the surgery, the surgeon collects four median-needle biopsies from the fresh prostate specimen, two from the tumor site and two from healthy prostate tissue, based on the previous results from the diagnostic biopsies and magnetic resonance imaging. The time of sampling and refrigeration is recorded. One of the benign and one of the cancer biopsies are put in RNAlater overnight; the RNAlater is thereafter removed. When the RNAlater has been removed, the biopsies are frozen at − 20 °C and stored at − 80 °C before they will be sent for analysis. The two other extra biopsies are sent for ordinary clinical pathological analysis to confirm that they were obtained from benign and cancer tissue. The radical prostatectomy tissues are formalin-fixed paraffin-embedded according to clinical routine.
Other collection
Total PSA concentrations at diagnosis and concentrations that are missing at endpoint, Gleason score, tertiary Gleason grade, T-stage, number of prostate biopsies, number of prostate biopsies with cancer, and prostate volume are collected at different time points from the National Prostate Cancer Register of Sweden [37]. The prostate tumor volume will be collected by using the pathological-anatomical information established after the surgery. PSA density will be calculated from total PSA concentrations and prostate volume. Information on the possible use of Finasteride, a 5α-reductase inhibitor, will be collected from medical records.
Outcome measures
Primary outcome
The primary outcome is tumor proliferation measured with Ki-67 in prostatectomy specimens. Ki-67 is a common marker of tumor proliferation, it can predict survival in localized prostate cancer, and it is based on cellular expression during the cell cycle [38]. Ki-67 will be assessed with an immunohistochemical method (CONFIRM anti-Ki-67 [30–9] Rabbit Monoclonal Primary Antibody; 790–4286; Ventana/Roche), which is described elsewhere [39]. ULTRA Cell Conditioning Solution (Ventana) will be used in the processing of the tissue samples as a pretreatment step. UltraView Universal DAB Detection Kit A will be used to detect antibodies, and the staining process is run in Benchmark Ultra (Ventana). A pathologist will evaluate the Ki-67 index by evaluating five different randomly selected areas of the largest and dominating tumor from the formalin-fixed paraffin-embedded radical prostatectomy tissue. At least 100 cells per area and 500 cells per tumor will be evaluated. The Ki-67 index will be the ratio of immunohistochemically positive prostate cancer nuclei divided by the total number of tumor cells evaluated × 100.
Secondary outcomes
Secondary outcomes include (1) blood-based changes of total and free PSA and selected hormones (mentioned below), (2) mRNA expression of genes involved in tumor proliferation and ER signal pathways, and (3) protein expression of androgen, ERβ, and ERα receptors in prostate biopsies.
PSA and hormones
Concentrations of total and free PSA, testosterone, estradiol, sex hormone-binding globulin (SHBG), and insulin-like growth factor 1 (IGF-1) will be analyzed in the serum at the Department of Clinical Chemistry (Halland Hospital, Halmstad and Varberg, Sweden), and the ratio between free and total PSA along with ratio between testosterone and SHBG is calculated. PSA and SHBG will be analyzed by sandwich assay on a Cobas 8000 analyzer series (Roche). Testosterone and estradiol will be analyzed using electrochemiluminescence immunoassay (ECLIA) on Cobas 8000 analyzer series (Roche), and IGF-1 will be analyzed by using sandwich enzyme-linked immunosorbent assay (ELISA).
Genotyping of estrogen receptor beta
In whole blood samples, the single nucleotide polymorphism rs2987983-13,950 T/C, described in detail elsewhere [4], will be genotyped in the ERβ gene using the PCR-based method KASP™ [40]. The genotyping takes place at Umeå University. Participants will be divided into two subgroups, i.e., alleles of TT or TC/CC.
Receptors
Receptor expression will be analyzed in the biopsies by using RNeasy plus Universal Mini Kits (QIAGEN) and real-time PCR at the Department of Bioscience and Nutrition, Karolinska Institute. ERα, ERβ, and AR mRNA expression will be determined using TaqMan assay [41, 42].
Gene expression
The expression of genes involved in proliferation and ER signal pathways and cell cycle progression (CCP) gene expression will be analyzed in prostatectomy specimens to identify the expression of genes involved in tumorigenesis by whole transcriptomic profiling. Total RNA will be extracted from formalin-fixed paraffin-embedded sections of tumors and benign tissues using the global transcriptome-wide expression array Clariom™ D (Thermo Fisher). For the analysis of the CCP score, gene expression of the genes involved in CCP is based on the Prolaris® gene panel [43] and the Decipher Score [44]. The genes for the ER signal pathways are based on the genes found to be ER-associated in a study by Thakkar et al. [45] in breast cancer and also found to be up- and downregulated in other studies (ESR1, GATA3, XBP1, NAT1, FOXA1, IL1R2, SLC39A6, CALU, ID1, ICA1, PFKP, SCUBE2, PLAT, CDC2, S100A6, SLPI, SLC2A3).
Statistical analysis
Sample size calculation
Calculation using the primary outcome (Ki-67) for a study group consisting of 118 patients provides an 80% power for a two-sided test with a level of significance of 0.05 and an effect size of 0.5 [21]. Earlier, we found that approximately 42% of the male population is heterozygous or homozygous for the variant allele (TC/CC) of the ERβ promoter region single-nucleotide polymorphism (SNP) and 58% homozygous for the wild-type allele (TT) [4]. We expect the effect of the intervention would decrease the Ki-67 score in the experimental arm with the variant genotype and have no effect among those with the common genotype. Thus, we arrived at a total sample size of 118/58% = 203 patients.
Data analysis and statistical methods
In the design and data collection, we have testing of drugs as the template (randomization, placebo, blinding, no attrition, no differential measuring errors, correct analysis); for the deviations from the perfect situation, we are using epidemiological theory [46] for guiding the analyses and interpreting the results. Statistical analyses will be performed following a statistical analysis plan that is set up a priori. The analysis plan is available at ClinicalTrials.gov. Interim analyses will be performed by an independent statistician when about half of the participants have been recruited. Thereafter, a data monitoring committee (DMC) is consulted, and the principal investigator decides whether to continue or terminate the study.
Analyses, based on means and standard deviations or medians and interquartile ranges will be provided to describe the baseline characteristics and outcomes. Differences between the intervention and the control groups will be assessed by using independent t-tests or the Mann–Whitney U test. The distribution of the data will be studied to apply to statistical tests and model fitting, and both P-values and 95% confidence intervals (CI) will be produced. If needed, appropriate transformations will be applied to improve symmetry and normality.
The dietary intake reported from the 24-h dietary recall and the questionnaires will be calculated and presented as descriptive data. The analyzed concentrations of phytoestrogens in the blood will be compared to the reported intake of phytoestrogens from the 24-h dietary recall and the questionnaires using linear regression analyses and kappa statistics. The median, mean, and maximum values from the five areas of Ki-67 will be calculated for each participant even if the median values will be used as the primary outcome. In the primary analyses, Ki-67 values will be dichotomized according to the median value in the study population. The difference between PSA concentrations at endpoint and baseline will be calculated, both for total concentrations and the ratio of free and total. In the primary analyses, the difference in PSA concentrations will be dichotomized into decreased/unchanged and increased concentrations. For hormone concentrations, the difference between endpoint and baseline and the ratio between testosterone and estradiol will be calculated. The association between phytoestrogen intake and cancer proliferation will be evaluated by generalized linear models, which will provide estimates of the risk difference (RDs) and corresponding 95% CIs, stratified by ERβ genotypes. Interactions between phytoestrogen intake and ERβ SNPs on proliferation will be evaluated considering additive effect scales. The group of phytoestrogen intake is included as a continuous variable, and each SNP is represented by an indicator variable (variant or not). The interaction will be assessed in a linear odds model by the product term between the covariates representing phytoestrogen intake and SNP genotypes.
Causal factors of the outcome, not equally distributed between the two groups (possible confounding factors), will be added to fitted models. Potential confounders will be based on previous subject matter knowledge and with the help of directed acyclic graphs. Missing data on potential confounding factors will be handled with multiple imputations using chained equations [47]. Subgroup analyses will be performed with compliant participants calculated from the endpoint FFQ and the 24-h dietary recall. In the intervention group, compliance will be considered as ≥ 80% of the recommended intake of 200 mg of phytoestrogens, which is equal to ≥ 160 mg. In the control group, intakes below 160 mg of phytoestrogens will be considered compliant.
Discussion
The PRODICA trial aims to evaluate if adding foods high in phytoestrogens to the diet can reduce the prostate-proliferation rate in patients with low- and intermediate-risk prostate cancer over a period as short as 6 weeks. Patients with prostate cancer often make dietary changes following their diagnosis [48], and the use of nutritional supplements is also common in patients with prostate cancer [49, 50]. Hence, it can be assumed that these patients are motivated to participate in a diet study and will have high compliance with the intervention.
We chose to use soybeans and flaxseeds as the source of phytoestrogens. Soybeans contain a high amount of isoflavones, and flaxseeds contain a high amount of lignans [51]. Unlike several other dietary sources, soybeans and flaxseeds do not need any preparation before eating, and adding them to the habitual diet does not require any major dietary changes, which could increase compliance with an intervention. In in-depth interviews with randomly selected prostate cancer patients (not included in this study), we investigated their attitudes toward participation in an intervention study eating soybeans and flaxseeds and found that patients were generally positive to eat the intervention foods. A major increased intake of beans could result in adverse effects of gastrointestinal discomfort, e.g., flatulence and bloating [52]. To handle this, we made a schedule for how to gradually increase the intake of the intervention foods during the first days of the intervention. Participants can also report gastrointestinal effects during the phone call when the 24-h dietary recall is performed, which enables individual regulation of the study foods.
We decided to give all participants dietary advice according to Swedish nutritional recommendations to treat the groups as equally as possible. The advice to avoid nutritional supplements is given due to potential confounding effects [53]. We chose a proliferation marker as the primary outcome instead of PSA since PSA could be affected by other factors than tumor proliferation [54]. Two other studies used Ki-67 to measure proliferation and found positive effects on this marker with flaxseed supplementation [21, 55].
A limitation of the PRODICA study is that we had to change from crushed to whole flaxseeds during the study inclusion. This will result in a decreased uptake of lignans due to decreased bioavailability [56]. However, continuing to provide patients with crushed flaxseeds would not have been ethical when the authority is dissuading intake of it. According to the European Food Safety Authority, whole flaxseeds are expected to have low uptake of cyanide after consumption [32]. Another limitation is that we have to shorten our intended 6-week intervention for some patients, due to shorter surgery queues. A longer intervention would have been more optimal to discover the potential effects of the intervention. However, we cannot influence the que of surgery, and it would not have been ethical to prolong patients’ waiting time for surgery without their permission. To date, only four participants (intervention n = 2, control n = 2) with ≤ 2 weeks inclusion to surgery have been included. To measure outcomes in, e.g., blood samples, we are using standardized analytical methods. These methods may result in measurement errors like non-differential misclassification, which can dilute our results [57].
Strengths of the PRODICA study include the hypothesis-driven design, the substantial number of participants we intend to include, and the randomization. Providing participants with soybeans and flaxseeds simplifies intake and eliminates purchasing costs for participants. Furthermore, even if participants may have low compliance with the intervention or drop out of the study, we still can collect our primary outcome from the prostate which is stored in the pathology clinic. We will only have missing data for the primary outcome for those who have not undergone surgery (approximately 2%), and this will probably not affect the interpretation of our results. Other strengths include our developed in-house phytoestrogen database, which covers the foods that contain phytoestrogens in a regular Swedish diet, and our previous research. This includes an interview study of dietary habits in patients with prostate cancer, a validation study of the FFQ including face-to-face interviews, evaluations of the protocol, and preparatory analyses of compliance.
The results of the PRODICA study will contribute important information on the relevance of increasing the intake of foods high in phytoestrogens in patients with prostate cancer who want to make dietary changes to improve the prognosis of their cancer. If genetic factors turn out to influence the effect of the intervention diet, dietary advice can be given to patients who most likely benefit from it. Dietary interventions are cost-effective, non-invasive, and result in few mild side effects. Moreover, soybeans and flaxseeds are besides phytoestrogens also high in dietary fiber, which has several positive health effects [58]. Lastly, the project will provide basic pathophysiological insights which could be relevant to the development of treatment strategies for patients with prostate cancer.
Trial status
The recruitment to the pilot study was started in February 2016. Some administrative changes were done to promote study participation and decrease the risk of dropouts, but no major changes were made to the study protocol. The main recruitment was started on 20 May 2016 and is expected to be finalized by the end of 2024. The study was published at ClinicalTrials.gov on 3 May 2016. Protocol version: 4, 2022–08-30. If any major amendments to the current protocol will be done, this will be submitted to the Swedish Ethical Review Authority for approval and will then be updated on ClinicalTrials.gov.
Roles and responsibilities
The coordinating center is located in Gothenburg. An inclusion group consists of clinical-based personnel who are responsible to ask patients of interest to participate and report the interested patients to the coordinating center. The coordinating center mainly consists of dietitians and is responsible to contact interested patients, conducting inclusion meetings and 24-h dietary recalls, and handling collected centrifuged blood samples and collected biopsies. The coordinating center also occasionally contacts the inclusion group about the inclusion rate and, if necessary, a meeting is held with the two groups. The blood samples are collected as usual clinical samples according to sampling referrals.
A trial steering committee designed the study, has overall responsibility, and supervises the coordinating center. The trial steering committee decided on the study endpoints in consultation with experienced urological clinicians. A monthly follow-up meeting is held with the trial steering committee and the coordinating center. A surgery group, with surgeons and a responsible surgery nurse, is responsible for the collection of prostate biopsies; collection kits are received from the coordinating center. A data management team consists of the principal investigator, researchers, PhD students, and a statistician. The DMC has an advisory role and consists of three researchers active in urology or oncology, they will take part in how the data collection progresses and be given access to the interim analyses. After this, the group will communicate its advice in writing to the research group. The DMC members are independent of the sponsor and investigators and do not state any competing interests.
Availability of data and materials
The data are manually entered, but the ranges will be checked to be plausible. All study-related information will be stored securely at the study site in areas with limited access. The data are coded with an identification number, and the code key is stored separately from the data. Data are handled confidentially and are collected for research purposes only. The coordinating center is unblinded and all caregivers are blinded to which group the participants are allocated to. We do not anticipate any requirement for unblinding. All executors of the analyses will receive coded samples and will be blinded to whether the samples belong to the intervention or the control groups. The data from the questionnaires are stored in a secure server located in the DC13 in the data center park owned by Hetzner GmbH. The principal investigator and the research group at Sahlgrenska Academy, University of Gothenburg, will have access to the final dataset. The study results will be presented in publications of international scientific journals and at national and/or international conferences. In upcoming manuscripts, the Vancouver criteria for authorship will be followed. The datasets analyzed during the current study and statistical code are available from the corresponding author upon reasonable request, as is the full protocol.
Change history
13 March 2023
A Correction to this paper has been published: https://doi.org/10.1186/s13063-023-07219-x
Abbreviations
- PRODICA:
-
Impact of DIet and individual genetic factors on tumor proliferation rate in males with PROstate CAncer
- ERβ:
-
Estrogen receptor beta
- PSA:
-
Prostate-specific antigen
- DHT:
-
5α-Dihydrotestosterone
- AR:
-
Androgen receptor
- 3βAdiol:
-
5α Androstane-3β,17β-diol
- ERα:
-
Estrogen receptor alpha
- FFQ:
-
Food frequency questionnaire
- SHBG:
-
Sex hormone-binding globulin
- IGF-1:
-
Insulin-like growth factor 1
- CCP:
-
Cell-cycle progression
- DMC:
-
Data monitoring committee
- CI:
-
Confidence interval
References
Loeb S, Curnyn C, Fagerlin A, et al. Informational needs during active surveillance for prostate cancer: a qualitative study. Patient Educ Couns. 2018;101(2):241–7.
Rinninella E, Mele MC, Cintoni M, et al. The facts about food after cancer diagnosis: a systematic review of prospective cohort studies. Nutrients 2020;12(8). https://doi.org/10.3390/nu12082345 [published Online First: 20200805]
Zhang Q, Feng H, Qluwakemi B, et al. Phytoestrogens and risk of prostate cancer: an updated meta-analysis of epidemiologic studies. Int J Food Sci Nutr. 2017;68(1):28–42. https://doi.org/10.1080/09637486.2016.1216525. [publishedOnlineFirst:2016/10/01]
Hedelin M, Bälter KA, Chang ET, et al. Dietary intake of phytoestrogens, estrogen receptor-beta polymorphisms and the risk of prostate cancer. Prostate. 2006;66(14):1512–20. https://doi.org/10.1002/pros.20487.
Huggins C, Hodges CV. Studies on prostatic cancer. I. The effect of castration, of estrogen and androgen injection on serum phosphatases in metastatic carcinoma of the prostate. CA Cancer J Clin. 1972;22(4):232–40. https://doi.org/10.3322/canjclin.22.4.232. ([published Online First: 1972/07/01]).
Kurzer MS, Xu X. Dietary phytoestrogens. Annu Rev Nutr. 1997;17:353–81. https://doi.org/10.1146/annurev.nutr.17.1.353. ([publishedOnlineFirst:1997/01/01]).
Kuiper GG, Lemmen JG, Carlsson B, et al. Interaction of estrogenic chemicals and phytoestrogens with estrogen receptor beta. Endocrinology. 1998;139(10):4252–63. https://doi.org/10.1210/endo.139.10.6216.
McPherson SJ, Ellem SJ, Simpson ER, et al. Essential role for estrogen receptor β in stromal-epithelial regulation of prostatic hyperplasia. Endocrinology. 2007;148(2):566–74. https://doi.org/10.1210/en.2006-0906.
Chokkalingam AP, Stanczyk FZ, Reichardt J, et al. Molecular epidemiology of prostate cancer: hormone-related genetic loci. Front Biosci. 2007;12:3436–60. https://doi.org/10.2741/2325.
Weihua Z, Lathe R, Warner M, et al. An endocrine pathway in the prostate, ERbeta, AR, 5alpha-androstane-3beta,17beta-diol, and CYP7B1, regulates prostate growth. Proc Natl Acad Sci U S A. 2002;99(21):13589–94. https://doi.org/10.1073/pnas.162477299. ([publishedOnlineFirst:20021007]).
Imamov O, Lopatkin NA, Gustafsson JA. Estrogen receptor beta in prostate cancer. N Engl J Med. 2004;351(26):2773–4. https://doi.org/10.1056/nejm200412233512622.
Hartman J, Strom A, Gustafsson JA. Current concepts and significance of estrogen receptor beta in prostate cancer. Steroids. 2012;77(12):1262–6. https://doi.org/10.1016/j.steroids.2012.07.002. ([publishedOnlineFirst:2012/07/25]).
Fritz WA, Wang J, Eltoum IE, et al. Dietary genistein down-regulates androgen and estrogen receptor expression in the rat prostate. Mol Cell Endocrinol. 2002;186(1):89–99. https://doi.org/10.1016/s0303-7207(01)00663-3.
Bektic J, Berger AP, Pfeil K, et al. Androgen receptor regulation by physiological concentrations of the isoflavonoid genistein in androgen-dependent LNCaP cells is mediated by estrogen receptor beta. Eur Urol. 2004;45(2):245–51. https://doi.org/10.1016/j.eururo.2003.09.001.
Lund TD, Munson DJ, Adlercreutz H, et al. Androgen receptor expression in the rat prostate is down-regulated by dietary phytoestrogens. Reprod Biol Endocrinol. 2004;2:5. https://doi.org/10.1186/1477-7827-2-5. ([publishedOnlineFirst:20040116]).
Bosland MC, Kato I, Zeleniuch-Jacquotte A, et al. Effect of soy protein isolate supplementation on biochemical recurrence of prostate cancer after radical prostatectomy: a randomized trial. JAMA. 2013;310(2):170–8. https://doi.org/10.1001/jama.2013.7842.
Hamilton-Reeves JM, Banerjee S, Banerjee SK, et al. Short-term soy isoflavone intervention in patients with localized prostate cancer: a randomized, double-blind, placebo-controlled trial. PLoS ONE. 2013;8(7):e68331. https://doi.org/10.1371/journal.pone.0068331. ([publishedOnlineFirst:2013/07/23]).
deVere White RW, Tsodikov A, Stapp EC, et al. Effects of a high dose, aglycone-rich soy extract on prostate-specific antigen and serum isoflavone concentrations in men with localized prostate cancer. Nutr Cancer. 2010;62(8):1036–43. https://doi.org/10.1080/01635581.2010.492085.
Landberg R, Andersson S-O, Zhang J-X, et al. Rye whole grain and bran intake compared with refined wheat decreases urinary C-peptide, plasma insulin, and prostate specific antigen in men with prostate cancer–3. J Nutr. 2010;140(12):2180–6. https://doi.org/10.3945/jn.110.127688.
Kumar NB, Kang L, Pow-Sang J, et al. Results of a randomized phase I dose-finding trial of several doses of isoflavones in men with localized prostate cancer: administration prior to radical prostatectomy. Journal of the Society for Integrative Oncology. 2010;8(1):3–13 ([published Online First: 2010/03/09]).
Demark-Wahnefried W, Polascik TJ, George SL, et al. Flaxseed supplementation (not dietary fat restriction) reduces prostate cancer proliferation rates in men presurgery. Cancer Epidemiology and Prevention Biomarkers. 2008;17(12):3577–87. https://doi.org/10.1158/1055-9965.EPI-08-0008.
Pendleton JM, Tan WW, Anai S, et al. Phase II trial of isoflavone in prostate-specific antigen recurrent prostate cancer after previous local therapy. BMC Cancer. 2008;8:132. https://doi.org/10.1186/1471-2407-8-132. ([publishedOnlineFirst:2008/05/13]).
Kumar NB, Krischer JP, Allen K, et al. A phase II randomized, placebo-controlled clinical trial of purified isoflavones in modulating steroid hormones in men diagnosed with localized prostate cancer. Nutr Cancer. 2007;59(2):163–8. https://doi.org/10.1080/01635580701432678.
Kranse R, Dagnelie PC, van Kemenade MC, et al. Dietary intervention in prostate cancer patients: PSA response in a randomized double-blind placebo-controlled study. Int J Cancer. 2005;113(5):835–40. https://doi.org/10.1002/ijc.20653.
Schröder FH, Roobol MJ, Boevé ER, et al. Randomized, double-blind, placebo-controlled crossover study in men with prostate cancer and rising PSA: effectiveness of a dietary supplement. Eur Urol. 2005;48(6):922–31. https://doi.org/10.1016/j.eururo.2005.08.005.
Dalais FS, Meliala A, Wattanapenpaiboon N, et al. Effects of a diet rich in phytoestrogens on prostate-specific antigen and sex hormones in men diagnosed with prostate cancer. Urology. 2004;64(3):510–5. https://doi.org/10.1016/j.urology.2004.04.009.
Bylund A, Lundin E, Zhang J-X, et al. Randomised controlled short-term intervention pilot study on rye bran bread in prostate cancer. Eur J Cancer Prev. 2003;12(5):407–15. https://doi.org/10.1097/00008469-200310000-00010.
Nybacka S, Forslund HB, Hedelin M. Validity of a web-based dietary questionnaire designed especially to measure the intake of phyto-oestrogens. J Nutrl Sci. 2016;5. https://doi.org/10.1017/jns.2016.28
Swedish Food Agency. Find your way to eat greener, not too much and be active 2015. Available from: https://www.livsmedelsverket.se/globalassets/publikationsdatabas/andra-sprak/kostraden/kostrad-eng.pdf. Accessed 28 Apr 2021.
Hedelin M, Löf M, Andersson TM, et al. Dietary phytoestrogens and the risk of ovarian cancer in the women’s lifestyle and health cohort study. Cancer Epidemiol Biomarkers Prev. 2011;20(2):308–17. https://doi.org/10.1158/1055-9965.Epi-10-0752. ([publishedOnlineFirst:2010/11/26]).
Hedelin M, Klint A, Chang ET, et al. Dietary phytoestrogen, serum enterolactone and risk of prostate cancer: the cancer prostate Sweden study (Sweden). Cancer causes & control : CCC. 2006;17(2):169–80. https://doi.org/10.1007/s10552-005-0342-2. ([publishedOnlineFirst:2006/01/21]).
Chain EPoCitF, Schrenk D, Bignami M, et al. Evaluation of the health risks related to the presence of cyanogenic glycosides in foods other than raw apricot kernels. EFSA J. 2019;17(4):e05662. https://doi.org/10.2903/j.efsa.2019.5662.
Swedish Food Agency. Linfrön (Flaxseeds). Available from: https://www.livsmedelsverket.se/livsmedel-och-innehall/mat-och-dryck/notter-och-froer/linfro. Accessed 28 Apr 2022.
Swedish Food Agency. Sök näringsinnehåll (Search for nutrients). Available from: https://www7.slv.se/SokNaringsinnehall/ Accessed 28 Apr 2022.
Nørskov NP, Givens I, Purup S, et al. Concentrations of phytoestrogens in conventional, organic and free-range retail milk in England. Food Chem. 2019;295:1–9. https://doi.org/10.1016/j.foodchem.2019.05.081. ([publishedOnlineFirst:2019/06/09]).
Nørskov NP, Olsen A, Tjønneland A, et al. Targeted LC-MS/MS method for the quantitation of plant lignans and enterolignans in biofluids from humans and pigs. J Agric Food Chem. 2015;63(27):6283–92. https://doi.org/10.1021/acs.jafc.5b01275. ([publishedOnlineFirst:2015/06/17]).
Tomic K, Sandin F, Wigertz A, et al. Evaluation of data quality in the National Prostate Cancer Register of Sweden. Eur J Cancer. 2015;51(1):101–11. https://doi.org/10.1016/j.ejca.2014.10.025. ([publishedOnlineFirst:2014/12/04]).
Berlin A, Castro-Mesta JF, Rodriguez-Romo L, et al. Prognostic role of Ki-67 score in localized prostate cancer: a systematic review and meta-analysis. Urol Oncol. 2017;35(8):499–506. https://doi.org/10.1016/j.urolonc.2017.05.004. ([publishedOnlineFirst:20170623]).
Josefsson A, Wikström P, Egevad L, et al. Low endoglin vascular density and Ki67 index in Gleason score 6 tumours may identify prostate cancer patients suitable for surveillance. Scand J Urol Nephrol. 2012;46(4):247–57. https://doi.org/10.3109/00365599.2012.669791.
LGC Biosearch Technologies™. KASP genotyping technology. Available from: http://www.lgcgroup.com/LGCGroup/media/PDFs/Products/Genotyping/KASP-brochure.pdf?ext=.pdf. Accessed 28 Apr 2022.
Heid CA, Stevens J, Livak KJ, et al. Real time quantitative PCR. Genome Res. 1996;6(10):986–94. https://doi.org/10.1101/gr.6.10.986.
McKenzie SE, Mansfield E, Rappaport E, et al. Parallel molecular genetic analysis. Eur J Hum Genet. 1998;6(5):417–29. https://doi.org/10.1038/sj.ejhg.5200218.
Ebell MH. Prolaris test for prostate cancer risk assessment. Am Fam Physician. 2019;100(5):311–2 ([published Online First: 2019/09/04]).
Dalela D, Loppenberg B, Sood A, et al. Contemporary role of the Decipher® test in prostate cancer management: current practice and future perspectives. Rev Urol. 2016;18(1):1–9. [published Online First: 2016/05/11]
Thakkar AD, Raj H, Chakrabarti D, et al. Identification of gene expression signature in estrogen receptor positive breast carcinoma. Biomark Cancer. 2010;2:1–15. https://doi.org/10.4137/BIC.S3793. ([publishedOnlineFirst:2010/01/01]).
Steineck G, Hunt H, Adolfsson JJAO. A hierarchical step-model for causation of bias-evaluating cancer treatment with epidemiological methods. Acta Oncol. 2006;45(4):421–9. https://doi.org/10.1080/02841860600649293.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–99.
Avery KN, Donovan JL, Gilbert R, et al. Men with prostate cancer make positive dietary changes following diagnosis and treatment. Cancer Causes Control. 2013;24(6):1119–28. https://doi.org/10.1007/s10552-013-0189-x.
Wilkinson S, Farrelly S, Low J, et al. The use of complementary therapy by men with prostate cancer in the UK. Eur J Cancer Care. 2008;17(5):492–9. https://doi.org/10.1111/j.1365-2354.2007.00904.x.
Westerlund A, Steineck G, Bälter K, et al. Dietary supplement use patterns in men with prostate cancer: the Cancer Prostate Sweden study. Ann Oncol. 2011;22(4):967–72. https://doi.org/10.1093/annonc/mdq456.
Fletcher RJ. Food sources of phyto-oestrogens and their precursors in Europe. Br J Nutr. 2003;89(Suppl 1):S39-43. https://doi.org/10.1079/bjn2002795. ([publishedOnlineFirst:2003/05/03]).
Winham DM, Hutchins AM. Perceptions of flatulence from bean consumption among adults in 3 feeding studies. Nutr J. 2011;10:128. https://doi.org/10.1186/1475-2891-10-128. ([publishedOnlineFirst:2011/11/23]).
Harvie M. Nutritional supplements and cancer: potential benefits and proven harms. Am Soc Clin Oncol Educ Book 2014:e478–86. https://doi.org/10.14694/EdBook_AM.2014.34.e478
Hernández J, Thompson IM. Prostate-specific antigen: a review of the validation of the most commonly used cancer biomarker. Cancer. 2004;101(5):894–904. https://doi.org/10.1002/cncr.20480[publishedOnlineFirst:2004/08/27].
Azrad M, Vollmer RT, Madden J, et al. Flaxseed-derived enterolactone is inversely associated with tumor cell proliferation in men with localized prostate cancer. J Med Food. 2013;16(4):357–60. https://doi.org/10.1089/jmf.2012.0159. ([publishedOnlineFirst:2013/04/10]).
Kuijsten A, Arts IC, van’t Veer P, et al. The relative bioavailability of enterolignans in humans is enhanced by milling and crushing of flaxseed. J Nutr. 2005;135(12):2812–6. https://doi.org/10.1093/jn/135.12.2812.
Rothman KJ, Poole C. A strengthening programme for weak associations. Int J Epidemiol. 1988;17(4):955–9. https://doi.org/10.1093/ije/17.4.955. [publishedOnlineFirst:1988/12/01]
Anderson JW, Baird P, Davis RH Jr, et al. Health benefits of dietary fiber. Nutr Rev. 2009;67(4):188–205. https://doi.org/10.1111/j.1753-4887.2009.00189.x.
Acknowledgements
We gratefully want to thank all patients participating in the study and the professional caregivers at the Urological Department at Sahlgrenska University Hospital who recruit the patients to the study.
Patient and public involvement
In the in-depth interviews, we also investigated prostate patients’ attitudes and possible barriers to research participation, information that became the basis of the study design. Neither the patients nor the public were involved in the design and will not be involved in the conduct, reporting, or dissemination plans of this research. Participants will, if they wish, receive a summary of the main study findings at the end of the trial.
Funding
Open access funding provided by University of Gothenburg. This work was supported by Dr. P. Håkansson’s Foundation, Eslöv, Sweden, grant number Maria Hedelin 2014; Lions Cancerfond Väst, grant number 2013;10; Patientföreningen för prostatacancer ProLiv Väst, King Gustav V Jubilee Clinic Research Foundation at Sahlgrenska University Hospital, grant numbers 2021:353, 2020:320, 2019:262, 2018:206, 2017:145, and 2016:76; The LUA/ALF agreement in West of Sweden health care region, grant number ALFGBG-727821 and ALFGBG-966360; and Knut and Alice Wallenberg Foundation, grant number KAW 2015.0114. The sponsor organization is the Region of Västra Götaland (Sahlgrenska University Hospital; 413 45 Gothenburg). The funding agencies nor the sponsor organization did play any part in designing the study, and they will not have any impact on the data collection, data analysis, interpretation of the data, or publications.
Author information
Authors and Affiliations
Contributions
RA wrote the first draft of the manuscript. MH is the principal investigator of this trial. MH along with SN, AJ, JS, and GS contributed to the research question, study design, and implementation of the study protocol. MH, AJ, and GS obtained the funding. JS contributed to the recruitment of patients and collection of material. RA, SN, JS, AJ, GS, and MH contributed to the critical revision and final approval of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Swedish Ethical Review Board (registration number 410–14; amendments T124-15; 2020–02471; 2021–03320, 2021–05878-02). The participants receive information on what data is collected about them, that the data will be analyzed and coded, and that no unauthorized person will have access to the data. The information also includes that participants’ samples only are used in a way for which participants have given consent. The samples can only become relevant in new research projects if the participant gives new consent and/or approval from the Ethical Review Authority. Written, informed consent to participate will be obtained from all participants. Patients can withdraw their consent at any time during the study without any explanation. They can also request that their biological samples are destroyed or de-identified (untraceable to any person). The participants are offered compensation for extra travel related to the study. There is no anticipated harm or other compensation for trial participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been updated to correct a typo in the background section.
Supplementary Information
Additional file 1.
Schedule on intake of the intervention foods. A schedule on how the participants should gradually increase the amounts of the intervention foods.
Additional file 2.
Template 24-h dietary recall. A template of how 24-h dietary recall is performed by the dietitian.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ahlin, R., Nybacka, S., Josefsson, A. et al. The effect of a phytoestrogen intervention and impact of genetic factors on tumor proliferation markers among Swedish patients with prostate cancer: study protocol for the randomized controlled PRODICA trial. Trials 23, 1041 (2022). https://doi.org/10.1186/s13063-022-06995-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-022-06995-2